Important Facts
advertisement

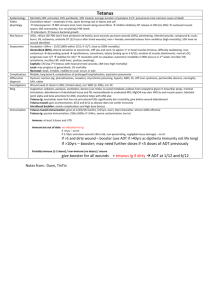
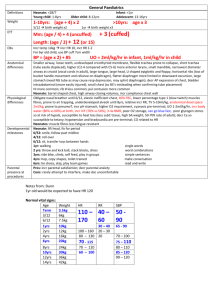
ACRONYMS Lactic acidosis LLTIPS Inhibitors Inducers L eukaemia L ymphoma T hiamine def I nfection P ancreatitis S mall bowel syndrome S odium valproate I soniazid C holamphenicol K etoconazole F luconazole A lcohol binge C iprofloxacin E rythromycin S ulphonamides C imetidine O meprazole M etronidazole + warfarin C arbemazepine R ifampicin A lcoholism P henytoin G riseofluvin P henobarb S ulphonylureas + folic acid Causes of DIC = VHOTMISS V ascular H epatic O bstetric T rauma M alignancy I mmune S epsis S hock / snakes Vasculitis, large aneurysm Failure Amn fl emb, HELLP, abruption, septic abortion Burns, rhabdo, thermia, fat emb, brain inj, decr O2 AdenoCa, lymphoma, promyelocytic Transfusion, anaphylaxis Gram –ive, viral haemorrhagic ARDS, pancreatitis Causes of ARDS = VHOTMAST V ascular H epatic O bstetric T rauma M OF A ltitude S epsis T ox fat, clot, air embolism Failure Amniotic fluid embolism, eclampsia Severe HI, multiple #, >8iu blood transfusion in a day ARF, DIC HAPE Pneumonia, pancreatitis, G-ives Smoke, metals, NO, NH3, chlorine, SO2, aspirin, HC, paraquat, opioids, cocaine, nitrofurantoin Causes of pancreatitis: GETSMASHED G allstones (35-40%) E TOH T rauma S corpian bite / toxin M umps, EBV, HIV, coxsackie, parasitic A utoimmune (SLE, Sjogrens, vasculitis) S teroids H yperCa / lipids E RCP (5% risk) D rugs (5%; sulphonamides, thiazides, valproate) TTP = FARTN F ever A anemia (haemolytic) R enal failure T hrombocytopenia N euro Sx Enhanced elimination = PAM PACAAT PALAAT Urinary alkalinisation P henobarb A spirin M ethotrexate MDAC P henobarb A spirin C olchicine (DECONTAMINATION > RESUS) A nticonvulsants (carbamazepine, phenytoin, Na valproate) A mitrip A manita mushroom HaemoD T heophylline P henobarb A spirin L ithium Anticonvulsants (Na valproate, carbamaz) A lcohol T heophylline CI for thrombolysis = ABC CHAMP Absolute CI A ortic dissection / active bleeding B errycarditis C NS (ICH ever / ischaemic CVA in past 6m / OT in past 2m) Relative CI C oagulopathy / cavitatory lung disease / CPR H TN (>180 / >110) A llergy, age >80yrs M ajor trauma in past 2m P regnancy / PUD / procedures in past 3w Simple febrile convulsion = FATGIDS AGMA: CATMUDPILERS F ever >38.5 A ge 6m – 5yrs T ime <15mins G eneralised 1Y I ntracranial pathology absent D eficit absent S ingle seizure per episode of fever C O, cyanide A lcoholic ketoacidosis T oulene M etformin, methanol U reaemia D KA P araldehyde, paracetamol OD I soniazid, iron L actic acidosis A Tissue hypoxia B1 Systemic disorders B2 Drugs/toxins C Hereditary metabolic E thylene glycol, ETOH XS R habo S alicylates, starvation NAGMA: USEDCARP U reterostomy S mall bowel fistula E xtra Cl D iarrhoea KA (resolving) Iuretics C arbonic anhydrase inhibitors A ddisons R TA P ancreatic fistula Metabolic alkalosis: GRORORE Cl insensitive Cl sensitive Normal BP High BP Prolonged QRS and QTC: PAACCTT A ntihistamines A ntimalarials T ype Ia/c T CA C ocaine C arbamazepine P henothiazines Prolonged QRS only: PLAT P ropanolol LA A mantadine T ype IV Prolonged QTc only: LMAO AT SS L ithium M ethadone A ntipsychotics O ‘s A ntibiotics T ype III / IV S umatriptan S SRI And ethylene glycol! Incr K May incr K Incr K Incr K with type 4 G I losses R enal losses O ther Post-diuretic Contraction alkalosis Post-hypercapnia CF R enal losses Bartter, Gitelman, diuretic efeeding alklosis O verdose of base Milk alkalki, NaHCO3 ther Severe hypoK/Mg R enal losses Liddle, diuretic, RAS, CRF E ndocrine Conns, Cushings, steroids Diphenhydramine Quinine, chloroquine Procainamide, quinidine Chlorprom, stemetil Diltiazem, verapamil HaloP, risperidone, quetiapine, droperidol OP’s, ondansetron, omeprazole Erythromycin, clarithromycin, tetracycline Amiodarone, sotalol, Ca ant Amitriptyline IMPORTANT TRIALS CV ISIS2: 1988; 17,000; aspirin vs SK vs aspirin + SK vs placebo in MI Aspirin+SK > aspirin / SK Aspirin = SK Aspirin alone + SK alone > placebo 3% decr AR mortality, 25% decr RR mortality ISIS1 + 3: beta-blockers in MI 50% decr infarct size, reinfarct, mortality 30% decr ICH Decr short term mortality with TL; decr cardiac rupture Worsens Sx with large infarct / LVF CLARITY-TIMI / COMMIT: clopidogrel in MI Improved hospital and 30/7 outcome CURE: clopidogrel + aspirin vs aspirin in MI 20% decr death / MI / CVA in 3-12/12 in clopidogrel+aspirin vs aspirin alone 1% incr bleeding rate SYNERGY: heparin + aspirin vs aspirin in MI Decr reinfarct / mortality by 33% in heparin+aspirin vs aspirin alone GUSTO: thrombolysis in MI 5% decr AR mortality PIOPED: investigation of PE diagnosis Clinical assessment and VQ scan established diagnosis in only minority of patients CTPA: 83% sens, 96% spec, 92-96% PPV, 10% inconclusive VQ: 98% sens, 10% spec, >50% inconclusive +ive (13%) 88% likelihood of PE; 96% PPV if mod/high pre-test prob Intermediate 15-30% likelihood Low prob 4-12% likelihood -ive (14%) <5% likelihood; NPV 96% NS NINDS: tPA vs placebo for NIHSS scores / mortality / probability of favourable outcome in CVA 600 patients; multiple centre RCT; industry sponsored; poorly matched 50% treated <90mins; no control over post-TL trt improved outcome at 3-12/12 13% absolute increase in minimal / no disability 3% decr mortality: 17% mortality tPA (21% placebo) 6% ICH tPA (0.6% placebo) – 50% were fatal ECASS: tPA vs placebo for TL <6hrs 600 patients; multiple centre RCT; industry sponsored; post-hoc analysis; well matched tPA no significant improvement in outcomes; increased mortality 27% ICH tPA (17% placebo) ECASS II: tPA vs placebo for TL <6hrs 800 patients; multiple centre RCT; industry sponsored No statistically significant change in outcome; increased ICH ECASS III: tPA vs placebo for TL 3-4.5hrs Multiple centre RCT; industry sponsored Better NIHSS score at 90/7 tPA and decr mortality; but incr ICH CAST + IST: aspirin in CVA prevention post-TIA 20-30% decr risk of CVA TOX Salt Lake Study: HBO in CO poisoning Good study; high FU Low no. suicides, high no. chronic exposure Poorly matched groups, corrected for in analysis 20% decr cognitive sequelae at 6/52 and 6/12 (25 vs 45%, 20 vs 38%) Alfred Study: HBO vs 48hrs 100% O2 in CO poisoning 50% lost to FU; only severely poisoned studied, poor methods No benefit ID Early goal directed therapy (Rivers et al, NEJM, 2001): RCT; severe sepsis Improved survival 16% compared to control May not be applicable to Australasia as have lower mortality rates than USA Endpoint: CVP 8-12 CVO2 >70% MAP 65-90 UO >0.5ml/kg/hr If low MAP / CVP 500ml (10ml/kg) N saline Q5-10minly + watch for improved / worsened CV status If MAP not achieved Commence NAD + insert CVL/AL Endpoint: PWP 15-18 MAP 90-110 HR 80-120 If CO not achieved (ie. CVO2 <70%, UO low, incr lactate) - CONTROVERSIAL Commence dobutamine (controversial; may decr BP and incr HR) Aim HCt >30% (transfuse; controversial) Aim Hb >7 APC in sepsis: 6% decr mortality (controversial) Use if severe sepsis with dysfunction of >2 organ systems / APACHE >25 24mcg/kg/hr INF for 96hrs CORTICUS (NEJM, 2008): hydrocortisone in septic shock No improved survival or reversal of shock, but did speed up reversal of shock in those who did survive 11% decr mortality if relative adrenal insufficiency Controversial – recommended if septic shock requiring vasopressors 200-300mg hydrocortisone per day SAFE study (NEJM 2004): saline vs albumin in ICU in critically ill patients RCT, double blinded No significant difference in mortality, survival time, organ dysfunction, duration of mechanical ventilation / dialysis, hospital / ICU LOS Decr mortality in albumin in severe sepsis (statistically insignificant) Incr mortality in albumin in trauma Dopamine vs NAD in shock (NEJM, 2010) No significant difference in outcome Dopamine: Incr adverse events, incr mortality in cardiogenic shock Low dose dopamine for renal protection (Lancet, 2000) Not recommended NAD + dobutamine vs adrenaline in septic shock (Lancet, 2007): No difference RS BiPAP in COPD (Bronchard et al): Decr mortality; NNT 10 Decr ETT; NNT 5 Decr hospital and ICU LOS (no effect on mortality when CPAP for CCF) RESUS CRASH-2 trial ( 2010, The Lancet): tranexamic acid 1g Large RCT trial of effects of tranexamic acid on death and transfusion requirement in trauma patients with, or at risk of, significant haemorrhage Decr death if given <3hrs of trauma (incr risk if given after >3hrs) CONTROL trial: factor VIIa in blunt trauma Incr mortality No improvement of any clinically significant outcomes 5% incr VTE Only as last resort after control of bleeding obtained Permissive hypotension: if uncontrolled haem and early intervention can control bleeding Aim: SBP 60-80, MAP 40 CI: Controlled haem, evidence of end organ failure (eg. MI), HI Unclear effects on mortality and organ failure in long term ARDS-net: TV 6ml/kg (decr mortality rate 10%, from 40% 30%) Permissive hypercapnia (aim pH >7.2 and adequate PaO2) RR 18-22 PIP <30 Allow mod hypercapnia Titrate PEEP to FiO2 Elevate head of bed 45deg Prone ventilation improves oxygenation but no survival benefit NEJM, 2002 HACA (Hypothermia after Cardiac Arrest, ) Cooled for 24hrs At 6/12 Favourable neuro 55% vs 40% Ability to live independently and work parttime Death 40% vs 55% Trend to sepsis, bleeding and pneumonia in hypothermia group NNT 6-7 Melbourne Study (Bernard et al, NEJM 2002) Cooled for 12hrs Good neuro outcome 50% vs 25% Mortality 50% vs 70% ILCOR Recommendations (2002) Discharge to home or rehab If unconscious (absent response to verbal commands; GCS <6; motor <4) Initial rhythm VF Out of hospital ROSC within <60mins TESTS AND SCORES Trauma Score <12 = serious GCS RR SBP Revised Trauma Score GCS RR Low score = bad Cons: poorly predictive of mortality SBP CRAMS Score Circ Resp Abdo <8 = bad Pros: good for pre-hospital triage Motor CRT Resp effort Speech Injury Severity Score Head+neck Abdo+pelvis Chest Face Extremities <9 = minor >25 = severe >35 = very severe Cons: doesn’t account for age / co-morbidities; retrospective; bad for penetrating New Injury Severity Score Pros: better mortality prediction Just 3 worst injuries of above External CHADS2: >75yrs 1 for CCF / HTN / Age / DM 2 for CVA / TIA / thromboembolism 0 = aspirin = 2% risk/yr of CVA 1 = aspirin / warfarin 2 = warfarin = 3% risk = 4% risk 1.5%/yr ARR 1Y prevention; 2.5%/yr ARR 2Y 20% decr risk CVA 60% RRR 2.5%/yr ARR 1Y prevention, 8.5%/yr ARR 2Y 1%/yr =haemorrhage 3 4 5 6 = 6% = 8% = 12% = 18% ABCD2 score: 1 for >60yrs BP: >140/90 Clinical: speech disturbance Duration: 10-60mins Age: 2 for: unilateral weakness >60mins DM 0-3 = 1% 2/7 risk = 15% 1/52 risk 4-5 = 4% 2/7 risk = 20-25% 1/52 risk 6-7 = 8% 2/7 risk = 25-30% 1/52 rsik = do CT head and carotid USS within 48-72hrs; OP FU = admit Stroke screening tools: ROSIER scale, FAST, CPSS, LAPSS, MASS Stroke assessment scale: NIH: correlates with infarct vol, weighted to ant circulation, allows comparison over time, measures level of impairment TIMI risk score 0-1 2 3 4 5 6-7 >0.5mm ST deviation >2 angina in past day >3 cardiac RF >50% prev stenosis >65yrs Aspirin in past week Incr cardiac markers = 5% risk death / MI / urgent revasc at 2/52 = 8% = 13% Intermediate Early invasive therapy good = 20% = 25% High = 40% Pros: not dependent on physiology; validated; applicable to all Cons: doesn’t weight RF’s; 0 score still has 2% risk Grace Score ST changes Age Biomarkers HR Estimate of in-hospital and 6/12 mortality SBP Cr Killip class Cardiac arrest Pros: more precise Cons: more difficult; RF’s not involved Duke Criteria 2 major 2x +ive blood culture of typical MO >12hrs apart Intracardiac mass Periannular abscess Partial dehiscence of prosthetic valve New regurg on echo Staph aureus, strep bovis Strep viridians, enterococcus HACEK 1major, 3 minor IVDU / congenital heart disease 5 minor T >38 Vascular phenomena (organ emboli, mycotic aneurysm, splinter haem, Janeway) Immunological phenomena (GN, Osler’s nodes, Roth spots) +ive blood culture / echo not fitting major criteria Modified Jones Criteria 2 major Carditis / new murmur Chorea Migratory polyarthritis Erythema marginatum Subcutaneous nodules 1 major, 2 minor PMH RF T >38 Incr titre of antistrep ab Incr ESR / CRP >30 Long PR Arthralgia 66% 10-30% 60-70% 10% Uncommon SMART-COP S BP <90 M ultilobar A lb <35 RR T achy >125 C onfusion O2 P H <7.35 Predicts deterioration, need for ICU/vasopressors 0-2 = low risk 3-4 = mod risk 5-6 = high risk (33%) >7 = high risk (50%) 92% sens, 62% spec CORB C onfusion O 2 <90% R R >30 B P <95 Predicts deterioration, need for ICU/vasopressors >1 = severe 80% sens, 68% spec CURB-65 C onfusion U r >7 R R >30 B P <90 >65yrs Predicts 30/7 mortality / ICU admission 0 = 0% 0 – 1: can send home 1 = 1% 2: borderline 2 = 7.5% 3 = 20% 4 = 40% 5 = 60% Pneumonia Severity Index History NH res, CCF/CVA/CRF, Ca, liver OE T, HR >125, RR >30, BP <90 Ix BSL >14, Hct <30, PaO2 <60, Ur >11, Na <130, pH <7.35 Pleural effusion Predicts mortality; class I – V; admit class III and over; 30% mortality class V NYHA CCF: I II III IV Sx on abnormal exertion Sx on ordinary exertion Sx on less than ordinary exertion Sx at rest 10%/yr mortality 20%/yr mortality 40-50%/yr mortality Killip Classification I II III IV 5% mortality 15-20% mortality 40% mortality 80% mortality Brugada’s VT criteria Absent RS in any precordial lead RS >100 in any precordial lead AV dissociation (<25% sens) Wellen’s VT criteria RBBB LBBB Other VT criteria Well’s Criteria for DVT No CCF Bibasal rales + S3 Frank pul oedema Cardiogenic shock V1 V6 V1 V6 L sided incr rabbit ear in V1 RS ratio <1 QS wave RS >60ms R wave >30ms RS ratio <1 Any Q wave QRS >120-140 RBBB + QRS >140 LBBB + QRS >160 Concordance of QRS LAD/RAD 1 for -2 for 100% spec >95% spec Notched QRS (40% sens, >75% spec) Fusion beats Capture beats Notched downslope of S 20% sens, 90% spec RF’s Ca <6/12 Recent POP / decr movement Bedridden >3/7 / major OT <4/52 Leg Tender veins Entire leg swollen Calf swelling >3cm compared to opposite Pitting oedema Collateral superficial veins alternative diagnosis more likely 0-2 = low risk >2 = high risk Well’s Criteria for PE 1 for haemoptysis Ca 1.5 for HR >100 Bedridden >3/7 / PMH PE / 3 for Sx of DVT PE most likely diagnosis RED = in PERC OT <4/52 DVT 0-1 = 3-4% risk 2-6 = 20% risk 7+ = >60% risk Subjective; extensively validated Revised Geneva Score 1 for 2 for >65yrs haemoptysis; OT/leg # in 1/12; active Ca 3 for 4 for 5 for HR 75-94; unilat leg pain; prev DVT/PE Leg pain on palpation / unilat oedema HR >95 0-2 = 8% risk 4-10 = 28% risk 11+ = 74% risk More objective; less validated PERC Criteria EpiD Age <50yrs History No haemoptysis No OT / trauma in 1/12 PMH No PMH PE/DVT DH No OCP OE HR <100 SaO2 >95% No unilateral leg swelling Sens 97.5% Spec 22% SADPERSONS PSYCH EXAM ADDMIS A ppearance D isorders of thought D isorders of perception M ood and affect I nsight S Cognitision ASA CLASS: 1 = healthy, no medical problems 2 = mild systemic disease 3 = severe systemic disease, but no incapacitating 4 = severe systemic disease that is constant threat to life 5 = moribund, expected to live <24hrs irrespective of operation E = emergency SAN FRAN SYNCOPE RULE History PMH OE Investigation SOB PMH CCF SBP <90 at triage Not in SR New ECG changes Hct <30 1 = 12% serious outcome <1/52; 95% sens, 60% spec; similar to physician judgement but 10% more sens MMSE 10 points 9 points 5 points 3 points 3 points Orientation Language (objects, if and but, paper, close eyes, sentence, pentameter) Attention + calculation (serial 7’s / world) Recall (recall registration words) Registration (3 words, rpt back) >25 = normal 21-25 = mild <20 = cognitive impairment GCS Eye 1 2 3 4 Verbal 1 None To pain To voice Open spontaneously None <9 = severe Motor 2 3 4 5 1 2 3 4 5 6 Sounds Inappropriate words Disorientated Appropriate None Decerebrate (extension) Decorticate (flexion) Withdraws Localises Obeys commands SGARBOSSA CRITERIA Concordant STE >1mm Discordant STE >5mm Concordant STD >1mm OTTAWA ANKLE RULES Pain near malleoli Pons Midbrain Forebrain Up Up Up Down Down Down + inability to WB 4 steps immediately and in ED Tender post / inf lat / medial malleolus 100% sens, 40% spec; decr XR by 30% OTTAWA FOOT RULES Pain in mid-foot + inability to WB 4 steps immediately and in ED Tender base 5th MT and navicular Pain in knee + inability to WB 4 steps immediately and in ED >55yrs Tender head of fibula / patella Active knee flexion <90deg 100% sens, 80% spec OTTAWA KNEE RULES 100% sens fo significant #, 50% spec; decr XR by 25% NEXUS CRITERIA Neuro deficit ETOH Xtra injuries Unconsciouns / decr LOC Sore on palpation CANADIAN C SPINE High risk: Low risk: CANADIAN CT HEAD High risk: Med risk: Rule Of Nines Leg Sens 99.6% OLD >65yrs NEURO SX Paraesthesia MECHANISM: fall >1m / >5 steps / axial load / >100kmph / rollover / ejection / >55kmph / death at scene / bike collision / motorized rec vehicle INJURIES: sig closed HI, neuro Sx, pelvic #, multiple limb # Rear ended Sitting in ED Ambulatory at any time Delayed neck pain No tenderness OLD NEURO SX >65yrs GCS <15 2hrs post Vomiting >2x INJURIES Open / depressed skull # BSF MECHANISM: fall >1m / >5 steps / car v ped / ejection Amnesia >30mins Adult 18% each Child 1yr old 13.5% (+0.5% per yr each) Ranson’s Criteria Arm Torso Head Perineum Neck 9% each 18% front, 18% back 9% 1% 1% On arrival A ge >55yrs Same Same 19% (- 1% per yr) A ST >250 @ 48hrs L DH >350-700 B SL >10 W BC >16 P aO2 <60 H ct drop >10% <2 Ca U r rise >5 B E >4 E stimated fluid sequestration >6L 0-2 = 1% mortality 3-4 = 15% mortality Glasgow Scoring System 4-5 = 40% mortality 6-7 = 100% mortality A ST >200 A lb <32 L DH >600 B SL >10 W BC >15 P aO2 <60 C a <2 U r >15 >3 = severe Apache Score Age Physiology T, MAP, HR, GCS pH, Na, K, Cr, AA gradient, PaO2 WBC, Hct Chronic Health Chronic organ insufficiency Immune compromise ARF Done at admission only >7 = severe = 11-18% mortality 65% sens, 76% spec Light’s Criteria: 1+ of Pleural chol : serum chol Pleural protein : serum protein Pleural LDH : serum LDH Pleural chol Serum alb - pleural alb Pleural LDH Protein WBC Exudate >30 High >0.3 >0.5 99% sens for exudate >0.6 65-85% spec >1.1 >1.2 >2/3 upper limit of normal for serum LDH Transudate <30 Low Complicated parapneumonic effusion/empyema: pH <7.2 or 0.15-0.3 less than serum Glu <2.5 LDH >1000 Loculated Ongoing sepsis despite ABx Empyema Turbid with WCC >1000 MO on gram stain Transudate Increased hydrostatic pressure CHF Constrictive pericarditis SVC obstruction Decreased oncotic pressure Cirrhosis Nephrotic syndrome Hypoalbuminemia Iatrogenic / other Peritoneal dialysis Exudate Malignancy – primary or metastatic; 38% lung, 17% breast Infection Pneumonia Viral, fungal, mycobacterial, parasitic Contiguous infection PE (80%) Connective tissue diseases SLE, RA Inflammation Uremia Pancreatitis Sarcoidosis Hemothorax Iatrogenic / other Post-cardiac surgery Post-radiotherapy Drugs – amiodarone “Classic” exudates that can be transudates Malignancy PE (20%) Sarcoidosis Hypothyroidism Severity of Asthma Severity of COPD Mild PEFR, FEV1 >75% Mod PEFR, FEV1 >50-75% Severe PEFR, FEV1 <50% Extremis Can’t do SaO2 >95% SaO2 90-95% SaO2 <90% SaO2 <90% Mild FEV1 <80% Mod FEV1 <60% Severe FEV1 <40% DRUG DOSES I FORGET O+G Tocolysis: Salbutamol 100mcg/hr and increase until contractions stop Nifedipine 20mg stat rpt Q30min if ongoing 20mg TDS MgSO4 20mmol over 30mins GTN CI: >34/40, fetal distress, placental abruption, infection, pre-eclampsia Delay delivery by 24-48hrs in 80% HR 100-120 HR >120 HR >140/low Phrases Words Can’t do Betamethasone 11.4mg IM Q24h x2; if <34/40; decr risk of ARDS by 50% AntiD: 250iu if <13/40, 625iu IM if >13/40 Oxytoxcin 10iu IV stat 40iu over 4hrs or Ergometrine 250-500mcg IV/IM Misoprostol 500-1000mcg PR or Intramyometrial 250-500mcg PGF2a PPH MgSO4 in eclampsia: 40mmol over 15mins 20mmol rpt x2 Q15min if seizing 10-30mmol/hr INF Monitor Mg levels and for SE’s (lethargy, decr reflexes, flushing) CaGlu is antidote BP: Hydralazine 5-10mg IV over 5-10mins rpt Q20min Nifedipine: 10mg PO rpt Q30min Labetalol 20mg 40mg 80mg to max 200mg Methylodopa: Nitroprusside: PID: Sexy: Ceftriaxone 250mg IM stat Azithromycin 1g PO single dose Metronidazole 400mg BD 2/52 Severe: Ampicillin 2g IV Q6h IV Gentamicin 5mg/kg OD IV Metronidazole 500mg BD IV OR 5-60mg/hr INF 10mg PO Q4hrly 1-2mg/hr INF 250mg PO Q6h 0.1-5mcg/kg/min INF (clinda if penicillin allergy) Doxycycline 100mg BD 2/52 (roxy if BF) TOX Toxic doses ACEi Can have 2-3x dose and it’s fine ETOH 2-5g/kg coma >4mmol/L 0 order kinetics Withdrawal: 5-10mg PO 10-20mg PO 5mg IV 6-8hrly 1-2hrly stat Rpt up to 20mg in 30mins Then Q30minly Thiamine 500mg IV Ethylene Meths Wernickes 1ml/kg lethal ETOH if >3mmol/L ETOH 1g/kg in 5% dex 150mg/kg/hr Aim ETOH 20-30mmol/L / 100-150mg/dL Haemodialysis if >4-8mmol/L (until <3mmol/L) CNS CV renal Pyridoxine 100mg IV Thiamine 100mg IV NaHCO3 0.5-1ml/kg lethal Most potent cause of incr OG ETOH as above until <6mmol/L Haemodialysis if >15mmol/L Pyridoxine and thiamine as above Iso + folate 50mg IV 4ml/kg coma Incr OG as above, but minimal AGMA despite high ketosis Haemodialysis if >65mmol/L ETOH not used Carbamazepine Delayed onset 2Y to anticholinergic Na blockade SO TREAT AS TCA OD Charcoal, MDAC, NaHCO3 (cardiotoxicity), haemodialysis Na val >200mg/kg coma Blood probs: decr plt/WBC (BM failure) decr BSL/Ca/phos incr NH/LFT (liver failure) incr Na/MetHb, AGMA Charcoal, MDAC, WBI if SR, haemodialysis (>1-1.5g/L) Phenytoin 100mg/kg risk of coma Na blockade (IV) Charcoal, MDAC Type I antihis Anticholinergic, anti adrenergic, anti serotonin, Na and K blockade NaHCO3, MgSO4, inotropes, benzos for seizures Olanzapine >300mg coma Anticholinergic, anti adrenergic Anticholinergic, seizures, agranulocytosis, myocarditis >3g severe Na and K blockade, seizures Anticholinergic, Na and K blockade, anti serotonin, EPSE Clozapine Quetiapine Risperidone Chlorprom Haloperidol Thioridazine Na channel >5g severe Anticholinergic, EPSE, seizures Na and K blockade, EPSE, seizures Anticholinergic, Na and K blockade (severe) Citalopram, venlafaxine Quetiapine, haloperidol Propanolol Risperidone, thioridazine Aspirin >300mg/kg severe >500mg/kg fatal Charcoal, MDAC, WBI if SR NaHCO3 if symptomatic / level > 2.2 / pH <7.1 HaemoD if can’t UA / UA doesn’t work / level >4 despite trt / level >4 chronic / level > 6 acute / severe Propanolol As per TCA Verapamil Nifedipine >15mg/kg toxic HyperG, hypoK, ketoacidosis, lactic acidosis, AGMA >2mg/kg toxic TCA >10mg/kg HypoG, hyperK Olanzapine 40-100mg mod Quetiapine Chlorprom Na valproate Carbamazepine 20-50mg/kg mod >300mg coma >3g severe >5g severe 400-1000mg/kg severe >50mg/kg severe Aspirin 150-300mg/kg mod >300mg/kg severe Colchicine Paraquat Isoniazid >0.5mg/kg mod >0.8mg/kg severe 20-40mg/kg death in 5/7-wks >40mg/kg death in 1-5/7 >50mg/kg death in <3/7 >10g Fe Li 20-60mg/kg mod >40mg/kg Ethylene glycol Meths Isopropanol 2ml/kg 30ml of 40% 2.5ml/kg of 70% Propanolol Digoxin Diltiazem Verapamil >1g >10mg (>4mg in children) 5mg/kg (>10tabs in adults, >2 tabs in children) 16mg/kg (>10tabs in adults, >2tabs in children) Theophylline >110mmol/l 60-120mg/kg severe >1g/kg MOF >15g fatal >120mg/kg lethal Trt: Syrup of ipecac 15-30ml Gastric lavage: 200ml (10ml/kg) warm water Charcoal: 25-50g (0.5-1g/kg) WBI: 2L/hr (25ml/kg/hr) Intralipid: 1ml/kg 20% over 1min 10ml/hr INF MDAC: 50g (1g/kg) PO 25g (0.5g/kg) Q2h Urinary alkalinisation: 1mmol/kg NaHCO3 IV bolus 2.5-25mmol/hr OP Pralidoxime 1-2g in 100ml N saline slow IV over 15mins 0.5-1g/hr Endpoint: plasma cholinesterase >10% Atropine 1-2mg double dose Q2-3min until dry secretions Fe Desferrioxamine 5-15mg/kg/hr (can cause hypotension) Indication: >90mmol/L, 60mmol/L + Sx, severe toxicity Endpoint: Sx gone, Fe normal, AGMA normal, urine normal Cy Hydroxycobalamin 5g in 100ml N saline over 15mins rpt if no improvement Endpoint: improved LOC, CV status, metabolic acidosis Safe Dicobalt EDTA 300mg in 20ml dex over 1-5mins rpt if no improvement Endpoint: as above Bad SE’s esp if not poisoned Amyl nitrite 300mg over 2-3mins INH Na thiosulphate 12.5g IV over 10mins rpt if needed Endpoint: as above Safe Lead Succimer 10mg/kg PO TDS Dimercaprol 3-4mg/kg IM Q4h Na Ca EDTA 25-75mg/kg Isoniazid Pyridoxime 5g IV over 3-5mins (or same dose as isoniazid) rpt Q15min until seizures Controlled Morphine Naloxone MetHb Methylene blue 1-2mg/kg IV over 5mins rpt at 1hr if needed Digibind: Acute: 2/3 of wake up dose INF per hour DOA 20-60mins mg ingested x 0.8 x 2 = no ampoules Chronic: (mmol/L level x kg) / 100 = no ampoules CaGlu in HFl poisoning: ?NG???? 60ml 10% IV if systemic 10ml 10% up to 40ml with KY TOP Q15min then 6x/day 0.5-1ml/cm 10% SC (not in hands / feet) – not diluted N saline 10ml 10% with 40ml + heparin IV regional - large 10ml 10% with 40ml N saline IA regional over 4hrs (gold standard) 1.5ml 2.5% in N saline NEB Ca antagonist poisoning: 60ml 10% CaGlu over 15mins 20ml/hr INF Endpoint: Ca >2 5mg glucagon stat 1-5mg/hr 1iu/kg actrapid in 50ml 50% dex 0.5-1iu/kg/hr actrapid in 10% dex 1ml/kg 20% intralipid over 1min 0.5ml/kg/min INF Dystonic reaction (EPSE) DB Benztropine 1-2mg IV rpt at 15mins if needed 1mg PO TDS SS SC Cyproheptadine 8mg PO TDS Chlorpromazine 50-100mg IV NMS NB Bromocriptine 2.5mg PO TDS Dantrolene MH MD Dantrolene 1mg/kg IV 1mg/kg QID IV Fe OD stages 0-3hrs 3-12hrs 12-48hrs 2-5/7 weeks GI Variceal haem: Octreotide: 50mcg stat IV 50mcg/hr INF for 48hrs Terlipressin: 2mg IV Q6h Gastro: Paedialyte 25ml/kg/hr for 4hrs Liver failure: Mannitol 0.3-0.4g/kg Lactulose 20g PO / 300ml PR Appendicitis 1g Ampicillin QID + 5mg/kg gentamicin OD + metronidazole Cholecystitis 1g ampicillin QID + 5mg/kg gentamicin OD (+ metronidazole if gallstones) Gastro Norfloxacin 400mg (10mg/kg) PO BD 5/7 – E coli, Yersinia, salmonella, shigella Doxycycline – cholera Metronidazole 400mg (10mg/kg) PO TID 7-10/7 – C diff, giardia Vancomycin 125-250mg PO QID 10/7 – severe C diff Erythromycin 500mg (10mg/kg) PO QID 5/7 – campylobacter H pylori Pantoprazole 40mg BD + amoxicillin 1g BD for 5/7 pantoprazole 40mg BD + amox + clarithromycin 500mg BD for 5/7 SBP Ceftriaxone 2g IV OD / cefotaxime 2g IV TDS Ceftazadime / cefazolin / vanc intraperitoneal RS Asthma Salbutamol MgSO4 AminoP 10mcg/kg (500mcg) over 2mins rpt at 10mins 1-20mcg/kg/min 25-50mg/kg IV over 20mins 6-10mg/kg (500mg) over 1hr 0.5-1mg/kg/hr infusion CV Esmolol 500mcg/kg bolus 50-100mcg/kg/min infusion (thyroid storm) HTN: GTN 1-20mcg/min titrated up 5mcg ever 5mins max 200mcg/min Labetalol 10-20mg 40mg 80mg 1-10mg/hr infusion Esmolol 500mcg/kg bolus 50mcg/kg/min titrated to max 300mcg/kg/min Na nitroprusside 0.1-10mcg/kg/min Hydralazine 5-10mg IV over 5-10mins 5mg/hr INF AF: Amiodarone 2-5mg/kg over 10mins Flecainide 2mg/kg over 30mins 200-300mg PO Digoxin 500mcg IV 250mcg Q4-6h up to 250mcg/day Verapamil 1mg rpt to 10mg IV Metoprolol 5-10mg over 2mins MI Aspirin: 300mg Clopidogrel: 300mg for TL, 600mg for PCI UFH: 60Iiu/kg 12iu/kg/hr INF aiming APTT 1.5-4x normal LMWH: 0.75-1mg/kg SC BD (give 30mg IV bolus if <75yrs) Metoprolol: 50mg PO BD Reteplase: 10iu IV over 2mins 2nd dose 30mins later SK: 1.5million IU over 1hr PE: UFH: 80iu/kg IV 18iu/kg/hr INF LMWH: 1mg/kg SC BD r-tPA: 10mg IV bolus 90mg IV over 2hrs SK: 250,000iu IV over 30mins 100,000iu/hr for 24hrs IE: ampicillin 2g IV Q4h Fluclox 2g IV Q4h (not needed if subacute) Gent 5mg/kg IV OD METHB CYANIDE 50% reversion in 24hrs, 90% in 48hrs 60% reversion in 3hrs, 80% in 8hrs If prosthetic / IVDU: ceftriaxone + vanc + gent RF: penicillin 10mg/kg BD for 10/7 SVT: adenosine 6, 12, 18 (0.1mg/kg, 0.2mg/kg, 0.3mg/kg); reverts 90%; 15% recur Verapamil 5mg IV slowly; 80% reversion, 95% with 10mg Flecainide 2mg/kg IV over 30-45mins TdP: 20mmol MgSO4 over 1-2mins 10-20mmol/hr VT: Amiodarone 150mg IV over 5-10mins 600mg/24hrs Procainamide 100mg IV 50mg/min until reversion Sotalol 1.5mg/kg over 3mins Lignocaine 1.5mg/kg IV over 5mins Product Dose Effect Rbc 2u (15ml/kg) Hb 20g/l, Hct 6% Plt (single) 1u (5ml/kg) Plt 50,000/mcl FFP 4u (15ml/kg) 1 unit = 3-5% Cryoppt 10u (1u/5kg) Fibrinogen 75mg/dL 30% effective in 1hr 75% effective 65% effective 20-30% effective NS Seizure: midaz 0.15mg/kg IV/IN/IM phenytoin 18mg/kg over 30mins Phenobarb 18mg/kg over 30mins Levetiracetam 20mg/kg Na valproate 20mg/kg over 3-5mins Thiopental 2-5mg/kg 2-5mg/kg/hr Migraine: paracetamol, nsaid, aspirin Maxalon, chlorprom, stemetil sumitrip chlorprom Stemetil Maxalon 1 Droperidol Sumitriptan 12.5-25mg IV Effective in 85% SE: decr BP, sedation 12.5mg IV Effective in 80% SE: phlebitis, akthesia 10mg IV 70-80% effective 2.5mg IV slow 80-100% effective SE: QT prolongation 100mg PO / 6mg SC 60-75% effective; use in mod-severe CI: vascular disease, preg, HTN, MAOI SE: MI, HTN, arrhythmia, chest pressure, dizziness Dihydroergotamine: 1mg IV over 3mins Q8h 85% effective CI: preg, sepsis, vascular disease, HTN SE: vasoC, ischaemia Lignocaine: Prilocaine: Bupivacaine: EMLA: AnGEL cream: TAC: LAT/ALA: DOA 40mins (2-5hrs with adrenaline) 5mg/kg plain, 7mg/kg with adrenaline Use phentolamine to reverse adrenaline effect Toxicity: dizziness, tinnitus, perioral tingling, decr LOC, agitation, nystagmus, muscle twitches, seizures, decr BP, arrhythmia 6mg/kg plain, 8mg/kg with adrenaline; 3mg/kg for Bier’s block DOA 6hrs 2mg/kg plain, 3mg/kg with adrenaline SE: most cardiotoxic prilocaine + lignocaine; onset 45mins; effective in 65% children SE: local allergy 5%; vasoC; CI <6/12 as systemic absorption + risk of MetHb amethocaine; onset 20mins SE: local reaction 15% tetracaine adrenaline cocaine SE: less effective <4yrs; CI’ed in places where adrenaline CI’ed; toxicity if used on MM’s (so use lower dose) lignocaine + adrenaline + tetracaine; cheap; as effective as TAC; less toxic; onset 2030mins Thrombolysis for CVA: tPA 0.9mg/kg 10% as bolus, 90% over 60mins GBS IVIG 2g/kg for 5/7 MG Crisis Trt Edrophonium 1 1 2mg IV slow push Neostigmine 0.5-2mg IV Pyridostigmine 60-90mg PO Q4h Pred 100mg/day ENVIRONMENTAL AMS/HACE: HAPE: Acetazolamide 250mg PO BD Dexamethasone 8mg stat 4mg Q6h PO/IM/IV Nifedipine 10mg SL stat 20-30mg SR BD ORTHO Septic arthritis: 2g IV fluclox QID 1.2g IV penicillin QID + gent if <6yrs / IVDU Bier’s block 3mg/kg 0.5% prilocaine Inflate cuff 100mmHg over SBP ID Same dose prophylaxis 4mg PO BD for prophylaxis Same dose prophylaxis Ondansetron 0.15mg/kg IV/PO Decr LOS, IV use, vomiting, hospitalization No effect on readmission Herpes simplex: Acyclovir 200mg 5x/day for 5/7 or 400mg TDS Herpes zoster: Acyclovir 400mg 5x/day for 10/7 Neonatal / encephalitis: 10mg/kg IV TDS for 2/52 Kawasaki disease: IVIG 2g/kg over 12hrs Aspirin 30-50mg/kg/day until fever gone 3-5mg/kg OD for 6-8/52 OM Amox /aug 15-25mg/kg TDS PO Cefaclor 10mg/kg QID PO Epiglottitis Ceftriaxone 25mg/kg for 5/7 (+/- vanc) Ludwig’s angina Benpen 1.2g IV Q6hr or Clinda 450mg IV Q8h Metronidazole 500mg IV BD Nec fasc Meropenem 1g IV TDS + clindamycin Fournier’s Ceftriaxone 2g IV + metronidazole 500mg IV + gentamicin 5mg/kg IV Meningitis 10mg (0.2mg/kg) dexamethasone IV Q6h for 4/7 within 1hr of ABx halves incidence of audio/neuro complications decr risk mortality in adults Rifampicin 10mg/kg BD x4 for contact prophylaxis / ceftriaxone IM / cipro Brain abscess Fluclox 50mg/kg Q4h + cefotaxime 50mg/kg QID + metronidazole 7.5mg/kg TDS <3/12 Unknown source >3/12 Unknown source <3/12 Meningitis >3/12 Meningitis Adult Meningitis <3/12 Pneumonia >3/12 Amoxicillin 50mg/kg QID (covers listeria and Grp B strep in <3/12) + cefotaxime 100mg/kg stat 50mg/kg QID or ceftriaxone 100mg/kg IM if no IV access +/- 10-20mg/kg acyclovir TDS Cefotaxime 100mg/kg stat 50mg/kg QID Amoxicillin 50mg/kg QID + cefotaxime 100mg/kg stat 50mg/kg QID or ceftriaxone 100mg/kg IM if no IV access Cefotaxime 100mg/kg stat 50mg/kg QID If suspect pneumococcus: vancomycin 12.5mg/kg QID If suspect listeria: keep amoxicillin Ceftriaxone 2g + benpen 1.8g Amoxicillin 50mg/kg QID + cefotaxime 100mg/kg stat 50mg/kg QID or ceftriaxone 100mg/kg IM if no IV access Pneumonia Amoxicillin 30-50mg/kg TDS Well pneumoniae Amoxicillin 30mg/kg TDS PO 5-7/7 Complicated pneumonia Augmentin 30mg/kg TDS (or cefuroxime 30mg/kg TDS) Unwell pneumonia Fluclox 50mg/kg QID + cefotaxime 50mg/kg QID or clindamycin Atypical pneumonia Roxithromycin 4mg/kg PO BD <3/12 UTI >3/12 UTI Amoxicillin 50mg/kg QID + gentamicin 5-7.5mg/kg OD (if CNS not excluded, use cefotaxime) Gentamicin 5-7.5mg/kg OD (or cefuroxime) If well, ceftriaxone then discharge on augmentin Gastro Na <120 Na 120-150 Na 150-160 Na >160 Per stool Per vomit NG rehydration 3% saline at 1ml/kg/hr 0.45% saline + 2.5% dex over 24hrs 0.45% saline + 2.5% dex over 48hrs 0.45% saline + 2.5% dex over 72hrs 10ml/kg 2ml/kg 25ml/kg/hr (or 100ml/kg over 4hrs) or 5ml/min ENDOCRINE DKA 1L N saline 1L over 1hr 1L over 2hrs 1L over 4hrs 1L over 10hrs Change to 0.45% saline + 5% dex once BSL <15 Aim decr glu by 5/hr, osm by 1-2/hr Add KCl once K <5 and UO – 10mmol/hr if K 4-5, 30 if 3-4, 40 if <3 If BSL decreasing too fast, used 0.45% saline + 10% dex Actrapid 0.1iu/kg/hr (max 6iu/hr) 0.05iu/kg/hr once BSL <12 NaHCO3 if pH <7, HCO3 <5, severe hyperK 0.5-1g/kg mannitol if cerebral oedema 5-10ml/kg 3% saline over 30mins if cerebral oedema Thyroid storm Esmolol 500mcg/kg 50mcg/kg/min infusion (if concern of COPD/CCF) Propanolol 0.5-1mg/min to max 10mg Propylthiouracil 900-1200mg PO loading 300mg/day Hydrocortisone 100mg IV GU Priapism Terbutaline Pseudoephedrine Adrenaline 1:100,000 5-10mg PO 60-120mg PO 2-3ml 500mcg SC METABOLIC HyperK Salbutamol 5mg nebs rpt Ca resonium 15-30g PO Q4-6h 10iu actrapid in 50mls 50% dex NaHCO3 1mmol/kg over 15-3mins Ca Glu 10-20ml of 10% over 5mins Hypertonic (3%) saline Indication: Endpoint: Onset 15-30mins Onset 1-2hrs Onset 15-30mins Onset 5-30mins Onset 1-3mins DOA 2-4hrs DOA 4-6hrs DOA 2-4hr DOA 1-2hrs DOA 30-60mins 25-100ml/hr (1-2ml/kg/hr) via CVL Coma, seizure, decr LOC Na >125 / Sx resolved RESUS Cooling 32-34deg for 12-24hrs passively rewarm over 8hrs at 0.25-0.5deg/hr 30ml/kg 4deg N saline over 30mins Paeds resus Adrenaline Amiodarone MgSO4 NaHCO3 Atropine Sux Naloxone 10mcg/kg including in neonates 5mg/kg 0.1-0.2mmol/kg 1mmol/kg 20mcg/kg (min 100mcg, max 1mg) Neonate: 3mg/kg; child: 2mg/kg 0.1mg/kg NUMBERS I FORGET RESUS Cardiac arrest: no CPR: no long term survival if time to shock >8mins CPR: no long term survival if time to shock >12mins Defib: 95% success if <30secs; 25% success if 2mins Out of hospital: 35% survive to hospital, 5% survive to discharge In ED: 70% survival ETCO2 is 5 less than arterial; correlates well with coronary perfusion p and survival from cardiac arrest; if <10mmHg, survival unlikely Cardioversion: 0.8% risk of VF with sync cardioversion; 15% risk of asystole with VF Propofol Cons Pros Ketamine Cons CI Pros NO Cons CI Pros Sux CI Cons Thio Cons resp depression in 50-60% Apnoea in up to 20% Ventilation needed in 1.5% (intubation in 0.02%) SBP drop by >20 in 15% Pain on injection No analgesia Myoclonic jerks + hypertonicity (rare) Propofol-infusion syndrome (rare) Onset 20secs; offset 9mins Amnesia, bronchoD, anticonvulsant, antiemetic HTN, incr HR Salivation, bronchorrhoea, tearing Laryngospasm 1-2.5% Transient resp dep if rapid IV admin Vomiting 8% Incr ICP Movement; ataxia during recovery Dysphoric and emergence phenomena URTI, LRTI, CF, <3/12, incr ICP, glaucoma, penetrating eye inj, HTN , CCF, aneurysm, porphyria, thyrotoxicosis, IHD Catatonia, amnesia, analgesia Preserveation of resp and airway reflexes BronchoD Onset 40secs (8mins IM); offset 10mins (30mins IM) Little sedation Onset 5mins; rapid offset Vomiting 5-10% Dysphoria 1% Apnoea 1-2% children <2yrs – resolves when stop gas Dizziness Mild CV depressant, pul vasoC Pneumothorax, bowel obstruction, severe, HI, severe COPD, decompression illness, recent drive, FiO2 >0.5 needed; intoxicated; decr LOC; prolonged use in pregnancy No resp depression Anxiolysis; analgesia Burns (9-66 days from inj, if >20% TBSA) Neuro conditions (10/7 – 6/12 from SC inj, UMN lesion, peri nerve inj, peri neuropathy, tetanus, muscular dystrophy, CVA) Congenital neuropathy Crush inj Malignant hyperthermia Incr IGp, IOp, ICP Muscle fasciculations HyperK (3-5mins after injection; lasts 10-15mins; by <1) No analgesia Pros Etomidate Cons Pros Fentanyl Cons Pros Hypotension, arrhythmias Apnoea, trismus Phlebitis, emergence delirium Amnesia, anticonvulsant Onset 40secs; offset 10-30mins No analgesia Myoclonus in 20% Vomiting Pain on admin Resp depression Emergence phenomena Adrenocortical suppression and seizures if infusion No CV depression Onset 15secs, offset 10mins Chest wall rigidity if >5mcg/kg Hypotension if BP maintained by sympathetic tone Decr HR, resp depression Onset <1min; offset 30-60mins Less hypotensive as no histamine release Analgesia PAEDS Paediatric Formulae Weight (>1y) (Age + 4) x2 Weight (<1y) [Age (months) + 9] / 2 Age/4 + 4 Neonate 3mm ETT 6/12 3.5mm 12/12 4mm Age/2 + 12 to lips Age/2 + 15 to nose ETT length Neonate 10cm 6-12/12 12cm (Age x 2) + 85 BP Neonate = 60mmHg Infants 20/min Ventilation rate 1-8y 15/min >8y 12/min Defib 4J/kg Cardioversion 0.5J/kg, 1J/kg, 2J/kg NG and IDC 2 x ETT Chest tube 4 x ETT or 2 x NG Bronchiolitis RSV in 40-70% Adenovirus rare but causes more severe disease Rapid Ag test 85% sens, 99% spec 40% are admitted Croup Parainfluenza I 50% CHANGES IN ELDERLY 15% decr TBW, 40% decr ECF, decr CI, incr SVR, decr ability to incr HR Decr muscle, incr fat, decr plasma proteins, decr bone density Decr pul compliance, incr diaphragmatic breathing Decr GFR Decr 1st pass, decr p450, decr GI motility and gastric acid secretion Decr immunity STATISTICS Precision False negative False positive Sens Spec Accuracy PPV NPV Measure of accuracy of test FN = 1 – sens FP = 1 – spec TP / (TP + FN) TP rate = fraction of people known to have disease who test positive TN / (TN + FP) TN rate = fraction of people known to be disease free who test negative (TP + TN) / N Proportion of all test results that are correct (sens and spec) TP / (TP + FP) The probability a positive test actually signifies presence of disease TN / (TN + FP) The probability that a disease will not be present if the test is negative NS Reflexes: CVA: 75% C5-6 C7-8 C8 L3-4 L5-S1 S1 Biceps Triceps Finger Knee Ankle Plantar 50% unknown 80% anterior 25% lacunar 20% posterior 20% embolic 80% MCA territory 5% atherosclerotic 2% dissection (10-25% if young/middle aged) 10% mortality Thrombolysis <3hrs (<6-12hrs in MI) NIHSS 4-25 for TL; <1/3 MCA involvement; plt <100; PT <15; <80yrs 2% decr mortality if <90mins; benefits at 3-12/12; NNT 8 3% risk of death from TL BP >220/120 Trt (BP >185/110 if for TL) Aim 10-15% decr in 24hrs ICH: 25% 50% ICH, 50% SAH 80-90% 1Y: putamen > thalamus > pons > cerebellum, brainstem, BG; central on CT 10-20% 2Y: peripheral on CT 40% mortality OT if <1cm from surface + <60yrs Cerebellar haem >3cm Hydrocephalus / marked mass effect Endarterectomy if: >80% stenosis (50% decr RR disabling CVA / death) 70-80% stensosis (25% decr RR) BP >190/120 Trt Aim SAH: 160/90 / MAP 110 70% ruptured Berry aneurysm: <50% aneurysms rupture; <50% AVMs have symptoms 15% perimesencephalic 50% mortality from initial bleed; 33% good recovery; 33% severe neuro deficit Warning bleed in 50% LOC in 66% CT head 97.5% sens at 12hrs; 95% 12-24hrs; 85% 1-2/7; 75% 2-3/7; 50% >1/52 >100,000 RBC LP Rebleed 20% (50% mortality); vasospasm 30% (30% mortality) Trt Aim SBP >180/120 pre-haem BP / SBP 120 – 180 / MAP 110 CV Norms: CO 5.5L/min; SV 70ml; EF 65%; EDV 130ml Infective endo: AF: native: mortality 25%; worse acute; better subacute Staph aureus in normal (30% in normal, 66% in IVDU) Prosthetic: mortality 50% Strep viridans in abnormal (50-60%) Mitral in normal; triscuspid in IVDU 2/3 cardiovert within 24hrs 40% due to IHD 0.1% risk if lone AF <60yrs 1.5% if low risk and anticoagulated 4.5% if low risk and uncoagulated Post-cardioversion: 55% in SR @ 1yr 90% success <48hrs, 50% success >48hrs 1-5% risk of embolism 2.5%/yr ARR 1Y, 8.5%/yr ARR 2Y 60% RRR CVA 1%/yr haemorrhage 1.5%/yr ARR 1Y, 2.5%/yr ARR 2Y 20% decr risk CVA Warfarin: Aspirin: Syncope: MI: 1% ED visits; 5% hospital admissions; 2% incidence >80yrs 40% unknown 20% vasovagal 10% cardiac (exertional = HOCM, AS) 10% postural (abnormal = decr SBP >20mmHg, or SBP <90) situational carotid sinus sens (abnormal = decr SBP >50mmHg, or ventricular pause >3secs) pacemaker failure ECG finds cause in 5%; blood tests in 2.5% Prox LAD Ant-septal Lateral Inferior RV Mortality 70% Mortality 10% Mortality 5% Mortality 25-30% aVR V1 CHB, RBBB, Mobitz II Ventricular rupture RV in 1/3; CHB; papillary muscle rupture CHB Circulation balanced 60-65%; R dominant 20-25%; L dominant 10-15% 15-30% silent 15% with initial normal ECG’s develop criteria on serials 10% incr sens if RV and post leads 12% in hospital mortality Irreversible damage in 20-40mins 1/3 have no RF’s Risk stratification: 40% V low <2% chance of MI / death in 6/12 55% Low 2-10% chance 30% reclassified as high risk 5% High >10% chance Normal ECG + trop: 1% risk MI Normal ECG + trop + <40yrs, no PMH, no RF 0.1-0.2% risk MI Trop T Trop I Tot CK CKMB CKMB mass Reperfusion in general: PCI: 99% sens 95% sens 90% sens Higher 95% sens 75-90% spec 82-95% spec 90% spec Higher 99% spec Detectable 2-12hrs Detectable 2-12hrs Detectable 4-8hrs Detectable 4-8hrs Duration 14/7 Duration 7/7 Duration 4/7 Duration 2/7 2.5% decr AR mortality 47% decr RR mortality 5-10% incr improvement of LVEF 6-7% dec AR mortality, 90% reperfusion rate <1hr since Sx Available <60mins 1-2hr since Sx Available <90mins 3-12hr since Sx and offsite Available <120mins >12hrs If unstable Large infarct: anterior / RV / inferior plus significant ST depression / LBBB Cardiogenic shock / severe CCF (Killip >3) and <75yrs CI to thrombolysis As rescue therapy if TL fails Best if: >70yrs, late, large, anterior / RV, CCF, prev CABG TL: 5% decr AR mortality, 60-80% reperfusion rate Too late for PTCA / PTCA not available >30mins pre-hospital transfer time <6-12hrs since Sx (<3hrs in CVA) tPA best if: <75yrs; decr BP; indigenous; >4hrs delay; ant MI; CI to SK 2% decr AR mortality compared to SK Aspirin: 1Y prevention for AMI: 2Y prevention for AMI: In unstable angina: In MI (ISIS2): not recommended decr ARR serious vascular events 8% 6.7% decr ARR CVA 2.5% 2% decr ARR coronary evetns 5% 4% 50-70% decr MI / death 3% decr AR mortality same as reperfusion therapy 25% decr RR mortality Clopidogrel: In MI (CURE): 20% decr mortality (with aspirin) 1% incr bleeding rate Heparin: In MI: 33% decr mortality (with aspirin) GTN: In MI: 35% decr mortality BB: In MI: 50% decr mortality, infarct size, reinfarct rate 30% decr ICH Statins: 30% decr coronary events over 5yrs 15% decr CVA PE: 10% mortality rate 5x incr risk during pregnancy DVT in 30-50% patients 50% no RF’s, 15-30% trauma, 10-25% Ca, 5-15% immobilization SOB most common Sx D dimer ELISA 95% sens Qualitative 80-85% sens USS leg 60% sens, 93% spec TTE 60-70% sens, 90% spec TOE 80-97% sens, 88-100% spec Thoracic USS 75% snes, 95% spec CXR Abnormal in 70-85% ECG Abnormal in 70-90% Risk stratification High = massive 40-50% PA occluded Mod = submassive RV dysfx Low = non-massive No RV dysfx TL indications in PE: CV compromise / cardiac arrest likely 2Y to PE PE <5/7 >40% pul vascular occlusion RV dilation / hypokinesis / RVSP >40mmHg Significant co-morbidities: COPD, CCF, prev PE Floating thrombus HR:SBP >1 Incr trop ECG showing RV strain >15% short term mortality 3-15% short term mortality 3% short term mortality Severe hypoxia Pericardial tamponade: Pericarditis: 15-60ml normal 200ml tamponade 200-250ml must be present to be seen on CXR 2L can be tolerated if slow accumulation Pulsus paradoxicus = decr SBP >10-20mmHg on inspiration Cancer most common cause of chronic; SOB most common Sx Echo: >2cm effusion depth RA / RV / LA collapse Dilated IVC with lack of collapse 25% Idiopathic 25% Ca ECG abnormal in 90% Pericardial effusion in 40% Incr trop in 50% CCF: If Sx 2yr mortality 35%, 6yr mortality 65-80% ACEi: 40% decr mortality; decr re-hospitalisation BB: decr disease progression / hospitalization; incr survival / cardiac performance Morphine: 10% incr mortality, hospital LOS, need for ventilation CPAP: decr need for intubation / ICU No change in hospital mortality / LOS Diuretics: No study has ever shown benefit HTN: Mild Mod Severe Malignant Aim WPW: 95% orthodromic, 5% antidromic ECG changes 140-159 160-179 >180 >180 90-99 100-109 >110 >120 + evidence of end organ damage <110 or 25% reduction in 12-24hrs K >10 9 7-8 VF, asystole, sinus arrest, brady, CHB Sine wave Loss of P waves Wide QRS, S+T waves merge Idioventricular rhythm, BBB 6.5-7 Small P waves, ST depression Blocks 6-6.5 Long PR, long QT 5.5-6 Peaked T waves 3.5 – 5 Normal Decr Long PR, T wave flat/inverted, ST depression U waves (mimic long QTc) VF, VT, atrial arrhythmia Ca Incr Decr Short QT; peaked wide T waves; J waves Long QTc Mg Incr Long PR, wide QRS CHB Long QTc TdP, AF, SVT Decr dsd RS NIV: Decr need for intubation by 25% overall CPAP decr need for intubation by 90% in APO Incr survival to discharge Decr ICU LOS, intubation Less evidence in pneumonia, ARDS, asthma, children 25% don’t tolerate Indication: type II resp failure pH 7.25-7.35 paO2 <60 on FiO2 50% paCO2 >50 RR >24 Incr WOB Type I resp failure RR >30 CPAP Improved compliance, FRC, VQ Decr preload + afterload incr CO Decr intrapul shunting BiPAP Decr WOB, afterload Pneumothorax: 1Y: 50-85% re-expansion rate without intervention 0.1% risk non-smoker, 12% smoker 2Y: 30-65% re-expansion rate without intervention >70% smokers 30-50% recurrence rate; 20% recurrence within 1yr CXR 90-95% sens; sliding lung 95% sens, comet tail >95% sens O2 4x incr reabsorption Asthma CXR USS PaCO2 >40 = bad = likely if PEFR <200 / <30% predicted FEV1 <1L / <25% predicted Will detect 100-300ml fluid on PA/AP 75-100ml on lateral decubitus 800-1000ml on supine 100% sens for >100ml; can detect 5-50ml Decr pneumothorax from 15% to 5% when used to guide drainage Pleural effusion Removing >500ml/hr will cause re-expansion pul oedema if >1.5L removed Drain if deeper than 1cm on USS O+G Pre-eclampsia: >160/>110 x1 or >140/>90 x2 + >300g/24hrs + generalized oedema or other end organ damage In 5-7% pregnancies 30% recurrence in next pregnancy Fetal and maternal mortality 2% Trt >170/110 Aim <160/110 Eclampsia Fetal mortality up to 30% Beta-hCG: Urine: Blood: + >50% + <50% - <35% - >35% >20iu/L 95-100% sens; <1% false negatives >5iu/L Sens 100% in 2/7 suggests viable pregnancy (decr from 12/40 onwards) in 2/7 suggests ectopic in 2/7 suggests ectopic in 2/7 suggests miscarriage Fundus height: 12/40 16/40 20/40 Symphysis pubis Half way Umbilicus TVUS: 4.5-5/40 5.5-6/40 6/40 Bad Empty gestational sac with diameter >18-20mm Gestational sac >16mm / CRL >6mm without cardiac activity TVUS zone TAUS zone 1500-2400 3000-6000 Ectopic In 2% pregnancies 25-30% ectopic pregnancy rate in subsequent pregnancies 80% ampullary PID: Works from 5/40 If >6/40 and nothing seen TVUS 10% infertility after 1st episode, 20% after 2nd, >50% after 3rd Changes in preg CV Haem RS GI GU APH Gestational sac Yolk sac Fetal pole and cardiac activity Can lose 30% blood vol before decr BP Uterus decr CO 10-30% when compresses 40% incr CO; 15-20 incr HR by term; 10-15 decr BP and MAP in 2nd trimester but normalizes by 20/40; decr DBP>SBP; 20% decr SVR; 50% incr plasma vol; 100x incr uterine blood flow; split S1; loud S3; SM; LAD 20-30% incr RBC vol; 30% incr RBC mass; decr Hct; incr WBC 20-30% incr O2 consumption; 40% incr TV; 25% incr MV; 20% decr FRC; 25% decr RV; no change in VC / RR 2-3x incr ALP; decr alb 5 50% incr GFR and CrCl; glycosuria in >50% In 2-5% pregnancies 30% placenta preaevia Painless profuse PV bleeding Bright red Non-tender soft uterus Maternal shock (mortality 0.03%) Fetus OK USS 95% sens 20% placental abruption Painful PV bleeding or may be concealed (1-2L) Dark red blood Tender tense large uterus Maternal shock (<1% mortality) Fetal shock (15-35% mortality) USS 25% sens Uterine rupture PV bleeding Palpable fetal parts; small uterus High maternal morbidity High fetal morbidity Vasa praevia PPH 1Y 2Y Perimorbid CS Painless small amounts PV bleeding Mother OK 75% fetal mortality >500ml in 1st 24hrs / >1L after CS Massive = >50% circulating blood vol in <3hrs / >150ml/min 2-5% of SVD Tone, trauma, tissue, thrombin From 24hrs – 6/52 Immediate 10mins 20mins 70% survival 15% survival 2% survival with poor outcome RENAL / URO Renal stone: 90% opaque 70% CaPhos (O), 15% struvite; 10% urate (L); 1% cysteine (partially O) CTKUB: 97% sens and spec IVP: 80-85% sens, 95% spec USS: 65-93% sens, 90-95% spec AXR: 50% sens Renal failure Mild Mod Severe Failure CAPD >100 WBC >50% neutrophils Usually staph Na deficit H20 deficit (135 – Na) x 0.6 x kg ((Na – 140) / 140) x 0.6 x kg GFR 60-90ml/min GFR 30-60 GFR <30 GFR <15 GI Upper GI bleeding: PUD: 60% PUD (25% duodenal ulcer, 20% gastric ulcer, 25% gastritis) 20% Mallory Weiss tear 7-10% Variceal: most common cause of rebleed 30% duodenal, 15% gastric H pylori most common cause; ELISA IgG 85% sens, 80% spec; Urease 90-95% sens; Faecal Ag >90% sens and spec; trt success 85% NSAID’s 2nd (20% have Sx) Duodenal = 90-95% have H pylori Gastric = NSAID (70% have H pylori) H pylori: 10-20% get PUD bleeding stops spontenously in 80% 5-6% mortality 20% haemorrhage, 20% penetration, 5% perf, 2% GOO GORD: omeprazole help Sx in 80%; H2 better at helping Sx than omeprazole 20-50% have H pylori Varices: bleeding stops spontaneously in 20-30% 10-15% haemorrhage/yr 25-40% mortality (15-20% 6/52 mortailty) 20-30% recurrence (most common cause of rebleed in upper GI bleeding) SB tube: 50% recurrence; controls bleed in 80%; 30% complication rate Sclerotherapy: 40% complication rate Ligation / sclero: stops bleeding in 80% Octreotide: stops bleeding in 80% TIPS: controls bleeding in 90% Lower GI bleed 20% bleeds; 5-10% mortality 80% stop spontaneously 60% due to diverticular disease; 10-20% no cause; 12% angiodysplasia; 2% Ca 90% GI FB’s pass sponteanously; 80% are paeds; cricopharyngeal narrowing at C6 most common site of obstruction in paeds, distal oesophagus most common in adult SBP: WCC >500-1000; neut >250; low glu; high protein; G stain and culture 70% sens Enterobacter (63%; eg. E coli (30%), klebsiella (10%)) > strep pneumonia, enterococci, anaerobes (5%), staph aureus (10%), pseudomonas (5%) 10% >1 MO 30% ascitic patients develop SBP in 1yr Ages for diseases: <1/12 <3/12 2-6/12 6-18/12 18-24/12 1-3yrs 1-7yrs 4-6yrs 5-8yrs Abdo USS: 90% sens for 250ml 96% sens for 500ml 95% spec Ascites: Transudate Exudate <30g/L protein >30g/L protein Blood >300 WBC Lactate Amylase Liver failure: Nec enterocolitis Volvulus / malrotation, feeding intolerance, incarcerated hernia, testicular torsion Pyloric stenosis Intussusception Kawasaki disease Croup (most 18m) Epiglottitis (most <2yrs) HSP Bacterial tracheitis CCF, cirrhosis, constrictive pericarditis Ca, infection, venous obstruction, pancreatitis, lymphatic Obstruction Ca ?infection SBP Pancreatitis Jaundice seen when bil >40 70% unconjugated = 2, 30% conjugated = direct Fulminant >75% mortality Onset of encephalopathy within 2/52 Acute Onset of encephalopathy within 8/52 Bad prognosis: Hep C/D/E, idiosyncratic drug reaction Good prognosis: Hep A, paracetamol Adults 50-70% paracetamol 20% no cause Paeds <1yrs Paeds >1yr 13% idiosyncratic drug reaction 8% Hep B (more in developing world) <5% Hep A 4% Hep C 40% metabolic 25% other 15% neonatal haemochromatosis 15% viral hepatitis 45% unknown 25% Hep C/D/E 10% Hep A 10% drug related 5% Hep B Appendicitis 20% fetal loss in preg 30% retrocaecal, 30% pelvic Anorexia most common Sx; pain migrates to RIF in 50% 50-75% have classical Sx McBurney’s point = 1/3 way from ASIS/umbilicus; appendix is medial and inf to point USS 80-90% sens, 90-100% spec – diameter >6cm, target sign, wall thickness >2mm CT + MRI 90-95% sens, 95% spec Acceptable negative laparotomy rate 10-20% Biliary Gallstones present in 10-20%; symptomatic in 20% Ca is most common cause of CBD obstruction Cholecystitis >90% gallstones, 10% acalculus (anaerobes and coliforms) Bacteria present in 50% cholecystitis (75% G-ive, 15% G+ive, anaerobes rare) Acalculus cholecystitis >50% mortality 70% cholesterol stones (radiolucent); 30% pigment stones (radio-opaque) Murphy’s sign 85-95% sens, 85% spec USS 90-95% sens, 95% spec for gallstones 90% sens, 80% spec for cholecystitis – GB >4x8cm, wall >4mm, CBD >10mm CT Lower sens Diverticulitis Occurs in 10-25% people with diverticular disease Usually anaerobes and G-ive rods Significant bleeding usually R sided; 5-15% bleed CT 97% sens, 100% spec Volvulis Sigmoid 2/3, elderly; sigmoidoscopy 90% success rate, but 90% recurrence Caecal 1/3, young; mortality 10-40% Obstruction SBO >2.5cm LBO >5cm >5 AF levels abnormal AXR 75-80% sens, 50% spec USS 95% sens and spec CT 90% sens, 95% spec Elderly AP 10% mortality; 40% initially misdiagnosed Cholecystitis most common cause Hernias Inguinal: Femoral: 75%; 2/3 indirect, 1/3 direct; 3%/mth strangulation; cough impulse above and medial to symphysis pubis; most common inc in women Indirect: lat to inf epiG art; frequent strangulation Direct: med to inf epiG art 20%/mth strangulation Med to inf epiG art; below and lat to pubic tubercle Ischaemic colitis >50% mortality Pancreatitis Mortality 2-10% ETOH most common cause; gallstones most common cause in women Bacteria present in 20% (50% in cholecystitis) CRP >150 at 48hrs is predictor of severity Lipase Incr earlier (in 4-8hrs), for longer (1-2/52) 95% sens and spec Does not correlate with severity Amylase Incr later (2-12hrs), for shorter (1/52) 80-90% sens (less sens with ETOH), 75% spec Does not correlate with severity CT 80-95% sens GU Renal colic 90% stones radio-opaque (25% gallstones) 90% pass spontaneously 70% Ca phos / oxalate (radio-opaque) 10-15% struvite – infective staghorn 10% urate (radiolucent) 1% cysteine (partially radio-opaque) Narrowest part is VUJ : 1-5mm 4mm = 90% pass 5mm = 80% pass 5-8mm = 15% pass >8mm = 5% pass Haematuria absent in 5-10%; gross haematuria in 30% CT KUB 97% sens and spec AXR 50% sens USS may miss if <5mm / mid-ureter ENT OM Incr cure rate by 10%, decr duration fever by 1/7 No effect on rate of complications Pharyngitis Decr duration Sx by 0.5 days, decr severity Sx, decr infectious period from 2/52 to 1/7 Decr risk RF by 70% Decr risk OM by 70% Decr risk quinsy by 85% Decr risk sinusitis by 50% No effect on risk of post-strep GN Ludwig’s angina 50% failure rate for RSI TOX Concerning doses Metformin >10g Digoxin >10mg (>4mg in children) Fe >60mg/kg Lithium Paracetamol >200mg/kg Aspirin >300mg/kg >60mmol/L (>90mmol/L is high risk) >2.2mmol/L for alkalinisation Decontamination Charcoal: 45% decr absorption at 30mins, 40% at 1hr, 15% at 2hrs Syrup of ipecac: decr absorption 30% if in 1st hr Gastric lavage: 25% decr absorption if at 30mins, 10% if at 1hr Fe OD Markers of toxicity: WCC >15, BSL >8, AGMA METABOLIC Na deficit (mmol/L) = (0.6 x kg) x (desired Na – actual Na) 90% DM is type II HONK: pH >7.3, HCO3 >15, AG normal, BSL >600, ketones +, osm >320 DKA: pH <7.3, HCO3 <15, AG high, BSL >250, ketones +++, variable osm HONK: N saline resus replace with 0.45% saline over 48-72hrs add 5% dex when BSL <15 DKA: N saline resus replace with N saline over 24hrs 0.45% saline + 5% dex when BSL <15 HONK: 0.05iu/kg/hr DKA: 0.1iu/kg/hr HONK mortality: 15-45% DKA mortality: 5-15% TRAUMA Hyphema: rebleeding in 3-5/7 in 30% FAST: 96% sens for >800ml FF 90% sens for >250ml FF 95% spec 100% sens, 96% spec for need for laparotomy in hypotensive patient insufficient sens to rule out significant inj in stable patient USS chest: 90% sens, 95% spec for haemothorax Sliding lung sign 95% sens, 90% spec Absent comet tails >95% sens, 60% spec USS AAA: ED doc 90-100% sens, >95% spec for >3cm USS IVC: normal 15-20mm with 5mm decr during insp Hypovolaemia: <14mm, with >40% collapse on inspiration Hypervolaemia: >20mm, without any insp collapse Burns: Minor Full <2% Partial <15% Burns unit >10% TBSA adult >5% TBSA child Mod 2-10% 15-25% Major >10% >25% (-5 if <10 / >50yrs) >5% full thickness Special areas Brooke-Parkland: 2-4ml/kg/% burn (+maintenance if child) 1st half in 8hrs, 2nd half in 16hrs Aim UO 0.5-1ml/kg/hr Penning’s criteria: Haemothorax Thoractomoty C1 C2 C3-4 C5+ 10mm 5mm 7mm 20mm Small Mod Large Massive <50% width C4 in children <350ml 350-1500ml >1500ml (>15ml/lg) >300ml/hr for 2hrs >600ml/6hrs >4ml/kg/hr Stable >200ml/hr for >2hrs >1500ml overall Unstable >100ml/hr for >2hrs >1000ml overall Compartment syndrome: 1-10mmHg <15mmHg 20-30mmHg >30mmHg Normal Safe Cause damage Emergency fasciotomy Boehler’s angle: <20deg = fracture DPL: 1L (10ml/kg) saline; 98% sens; 1% complication rate; 15% false +ive >20ml frank blood >100,000 RBC/ml if blunt >5000 RBC/ml if penetrating >500 WBC/ml if <3hrs since inj bile / food ORTHO Jt aspirate: Normal Inflamm Septic WCC <200, <25% PMN WCC 2000-50,000; >50% PMN WCC >25,000; >85% PMN Septic arthritis: 15% mortality 50% staph, 40% grp A strep in adults ENVIRONMENTAL Heat stroke T >40, altered LOC, anhydrosis, MOF Mortality 10-50% Decr T by… Incr T by… Blanket Ice packs Ice/warm water immersion Evaporative Humidified O2 Gastric lavage Peritoneal lavage Thoracic lavage Haemodialysis CPB 0.5-2deg / hr 0.04-0.08deg / min 0.15-0.25deg / min 0.3deg /min 4-10deg / hr 1-1.5deg / hr 0.5deg / min 2-4deg / hr 3-6deg / hr 2-3deg / hr 7-10deg / hr Hypothermia: Severe <28; mod 28-32; mild 32-35 check pulse for 60secs (instead of 10) 1x shock + drugs withhold until >30deg then 2x interval between drugs until 35 deg Heat IVF to 42 deg Use 5% dex as energy substrate Rapid rewarm to 30deg then slower 45% survive with normal function, 15% with severe brain inj 100% good outcome if GCS >8 at 2hrs >90% if GCS >3 at 2hrs Good prognosis: witnessed <5mins to retrieval <5mins submersion GCS >5 on scene <10mins to CPR <10mins to first resp effort = <10% significant neuro deficit <30mins to spontaneous breathing SaO2 >94% ROSC pre-hospital / no resp arrest Pupillary response / motor response to pain on arrival Cold water Bad prognosis: above + male <3yrs >10-25mins submersion >25mins resus Fixed dilated pupils at 6hrs GCS 5 on arrival = 80% risk death / severe deficit VT/VF on initial ECG / asystole Metabolic acidosis pH <7.1 on arrival Altitude High >1500m (4900ft) AMS begins >2500m HAPE begins >3500m Most can acclimitise up to 5500m Changes Incr RR, HCO3 diuresis, pul HTN, incr lung vol Incr SV, incr BP, incr CO, peri vasoC Incr RBC (days-wks), incr EPO (hrs), incr 23DPG Burns >20% fluid shifts, recommend IVF + IDC + NGT >40% recommend stress ulcer prophylaxis >50% potentially fatal >60% decr CO >80% full thickness unsurvivable 50deg 5mins 55deg 30secs 60deg 5secs 70deg 1sec Admit burns unit: AGE DCS Partial thickness >20% Partial thickness >15% if chemical Partial thickness >10% if <10yrs / >50yrs Full thickness >5% Other major burn criteria Occurs within 5-20mins of ascent, or in water 50% within 1hr, 90% within 6hrs Electrical >1000V = threshold for severe inj Vertical = 20% mortality Horizontal = 60% mortality Lightning = 10-30% mortality 1mAmp tingling 2-10mAmp pain 10mAmp paralysis / tetany 100mAmp – 1Amp VF, rest arrest, burns >10Amp asystole Low volt AC VF, rhabdo, ARF, deep tissue burns High volt AC / DC / lightning asystole, superficial burns ID Needlestick inj: Transmission: Hep B: E+ive, 40%; E-ive 5% (2-30% risk) Hep C: 2-10% (<2% risk) HIV: 0.3% Gloves decr by 50% Prophylaxis decr seroconversion by 80% Full 4/52 course tolerated by 35% HIV transmission: 0.8% anal receptive 3-15% prev in homos 0.6% shared IVDU 1% prev in IVDU 0.3% needlestick 0.1% vag / insertive anal <0.1% prev in heteros <0.1% MM exposure Hep B transmission 15% sex Hep C transmission 15% sex HIV: PCP occurs in 60% Malaria Falciparum >90% within 2/12; more resistance Vivax 50% within 2/12; most common; can be delayed months Most common cause of fever in traveller Dengue 4-10/7 incubation Risk of SBI: <4w and well <5% <4w + ill 13-21% <4w + bronchiolitis: 3-10% so do septic screen <6w 15% overall Height of fever irrelevant this young 6w – 3m well <5% 6w – 3m ill 13-21% 4w – 2m + bronchiolitis: 3-5% so do urine 6w – 3m 6-10% overall if any fever UTI (paeds) 3m – 6m 6m – 2yrs Overall <2yrs <1% <1% (incr if higher fever) 3% Seizure + well Seizure + ill 0.3% SBI 15-18% SBI 3-8% with no source have UTI <3/12 30% systemic sepsis >3/12 5% systemic sepsis 85% E coli, 6% proteus Nitrites 40% sens, 99% spec WBC 50-90% sens and spec (dipstick 75% sens) Bacteria 50-90% sens, 10-90% spec MSSU >5-10 WCC Catheter >1-5 WCC SPA >0 WCC Meningitis (paeds) Meningitis CSF Bacterial Viral Partial Trt TB 5% mortality FND in 15% (30% pneumococcus) Decr LOC 15% (more pneumococcus) Seizures 30% 60% strep pneumonia 16% N meningitides 14% grp B strep WCC 200-10,000 WCC 100-700 WCC 200-5000 WCC 100-500 FND prominent PMN 100-10,000 PMN <100 PMN 10-100 PMN high early MMN <100 MMN >100 MMN >100 MMN high late Pro >1 N Either Pro >1 Glu low N Either Glu low late Protein incr 0.01 per 1000 RBC Opening p Adult 7-18cm 22-25G, 12cm 8-18yrs 7-20cm 22-25G, 6cm 1-8yrs 1-10cm 2cm SIRS = >2 of T <36 or >38 HR >90 RR > 20 or PaCO2 <32 WCC <4 or >12 or >10% bands Organ dysfx SBP <90 / 40 below normal / MAP <60 BE < -5 Lactate >2 UO <30ml/hr FiO2 >0.4 or PEEP >5 Cr >160 Decr LOC Severe sepsis = SIRS + organ dysfx HR >160 infants, HR 150 children RR >60 infants, RR >50 children Lactate good for risk stratification: >2 = 4% mortality, >4 = 28% mortality Incr mortality by 8%/hr for delay in ABx Septic shock = severe sepsis + uncorrectable hypotension Unknown source RS GI UTI Skin Fluclox + gent Ceftriaxone + azithromycin Ampicillin + gent + metronidazole Ampicillin + gent Fluclox Febrile convulsion 4% incidence; 35% recurrence 3% go on to epilepsy (same as general population) Nec fasc Mortality 25-35% Clostridium perfringens most common cause B fragilis and E coli in Fournier’s Kawasaki IVIG 2g/kg IV over 12hrs Aspirin 30-50mg/kg/day until fever gone 3-5mg/kg OD for 6-8/52 ENDOCRINE DM: Type I 10% DM 90% immune mediated; 10% unknown 50% concordance in twins >80% loss islet cells for features of DM Type II 80% DM 100% concordance in twins MODY 2-5% DM DKA Fetal mortality 30-50%; mortality 5-15% (1% in children); 70% mortality if cerebral oedema Acetoacetate on ketostix urine test B-HB on blood; more in alcoholic ketoacidosis B-HB converted to acetoacetate Acetone on breath test 5-10L fluid deficit; 5-10mmol/kg Na deficit; 3-5mmol/kg K deficit DERMATOLOGY EM minor EM major No MM involved 1MM involved SJS Epidermal detachment <10% BSA >1MM involved Mortality 10-15% TEN Epidermal detachment >30% BSA MM often involved Mortality 25-35% TSS Toxic Shock T >38.9 SBP <90 S SSSS Rash desquamation; involvement 3+ systems No MM involvement FACTS I FORGET DISCHARGE PLANNING Diagnostic certainty SH Predictors of early readmission – reliance on others, assistance needed Symptom control PO intake Mental state Test mobility Time of discharge Communication Check contact details Organise OP FU Discharge medication Statutory requirements (eg. Work certificate) Discharge info and letter Transportation DERMATOLOGY Kawasaki disease Fever >5/7 + 4/5 of MM involvement: cracked lips, strawberry tongue Bilat conjunctivitis with perilimbic sparing Polymorphous generalized rash Peripheral redness and oedema Cervical lymphadenopathy Do echo at 2/52 6/52 1yr MI is leading cause of death; mortality <1% Measles Fever >38 Rash – erythematous maculopapular 1 of: cough / coryza / conjunctivitis / Koplick spots Mortality 10-15%; 50% due to pneumonia ENVIRONMENTAL PIB Funnel web, mouse spider All snakes inc sea Cone shell Blue ringed octopus Redback 20% envenomation rate Female bite Severe pain (in mins/delayed), erythema, sweating, piloerection lactrodectism (severe pain, sweating, piloerection) maybe weakness, N+V+AP 2 vial AV IM (serum sickness 10-15% for all AV) 10-25% envenomation rate Male bite pain + fang marks within 30mins, autonomic storm NCPO, spasms, paralysis, coma PIB, 1 vial AV rpt <5% envenomation rate Mod local Non-specific general PIB, funnel web AV Local pain Blue ulcer necrotizing arachnidism, metHb Necrotising arachnidism Funnel web Mouse spider White tail Recluse spider Black house 100% 90% 80% 99% 85-95% 60-98% Box Jelly Carybdeid Blue bottle Blue ringed Stone fish Sea snake Brown snake Tiger snake Black snake Taipan Death adder Immediate severe pain Cardiotoxicity collapse in water cardiac arrest, arrhythmia, HTN /decr BP Muscle spasms + paralysis vinegar, 1-6 vials AV, MgSO4 Mild local Irukandji Syndrome on beach sympathetic storm HTN, CCF, NCPO, collapse Severe generalized pain vinegar, MgSO4, anti-HTN Severe local in water hot water Paralysis collapse on beach PIB Severe pain hot water, 1-3 vials AV, ABx, ADT Paralysis in 2-6hrs Myolysis + ARF PIB, 1-3 vials AV 60% snake deaths, 70% snake bites Cardiotoxicitiy early collapse Early severe coagulopathy Thrombotic microangiopathy ARF PIB, 2 vials AV 25% snake deaths Cardiotoxicity early collapse Early coagulopathy Late neurotoxicity, severe myolysis, ARF PIB, 2 vials AV Marked local Coagulopathy, neurotoxicity, myolysis, ARF PIB, 1 vial AV 10% snake deaths Early collapse, coagulopathy, neurotoxicity, myolysis PIB, 1-3 vials AV 5% snake deaths Early neurotoxicity PIB, 1 vial AV ID Live attenuated BCG MMR VZV Polio Notifiable disease Avoif if immunosuppressed Campylobacter, chlamydia, gonorrhea, hep A+E, flu, legionella, listeria, MMR, syphilis, salmonella, VZV TRAUMA Brown Sequard Ipsilateral motor, position, vibratory Contralateral pain, T Central Anterior Human bites: Staph aureus Upper > lower bilaterally Bilat motor weakness Eikenella Dog bites • Staphylococcus Streptococcus Haemophilus species • Eikenella Pasteurella Proteus Klebsiella species • Enterobacter species • Capnocytophaga canimorsus – overwhelming sepsis in immunocomp • Bacteroides Moraxella Corynebacterium Neisseria Fusobacterium • • • • • Prevotela Porphyromonas Cat bites – 60-80% get infected Staphylococcus Streptococcus Pasteurella Actinomyces Propionibacterium Bacteroides Fusobacterium Clostridium Wolinella Peptostreptococcus species Bartonella cat scratch disease regional lymphadenopathy after 7-12/7 Marine assoc Staph, strep G-ive rods esp Vibrio Tetanus Prophylaxis Hx Clean Dirty Td TIG Td TIG ✓ No ✓ ✓ ≤ 5y No No No No 5-10 y No No ✓ No >10 y ✓ No ✓ No <3 or unknown Immunised HBsAg+ HBsAg- Unknown Unvaccinated HBIg (400iu IM) + vacc Vacc Vacc Vacc + responder (anti-HBs >10) No Rx No Rx No Rx Vacc + non- responder (anti-HBs <10) HBIg (400iu IM) + vacc Booster If hi-risk, Rx as H Source Mx HIV - Nil else Likely/confirmed + PEP 4/52 (ideally <24-36h) 2 drugs standard 3 drugs if hi-risk Unknown O+G Safe in preg: Usually no PEP 2 drugs if hi-risk cephalosporins, azithromycin, nitrofurantoin, penicillins Maxalon, ondansetron, stemetil, promethazine Heparin Not safe in preg: fluroquinolones (ie. Ciprofloxacin), sulphonamides (eg. Cotrim), tetracyclines (eg. Doxy), gent, metronidazole Oral hypoglycaemics Warfarin, thrombolysis NSAIDs, aspirin Stemetil Phenytoin Amiodarone, ACEi, AII receptor antagonists Lithium Most common cause of vulvovaginitis: bacterial vaginosis GI H pylori: NSAIDS: PUD: PUD: Omeprazole: GI bleed: PUD: H2 antagonists: GORD: PUD: Misoprostol Sucralfate Bismuth cmpds Octreotide: Varices: Gastroscopy: SB tube: GI bleed: Varices: Banding/sclera: Varices: TIPS: Varices: Angio+embo: Complications: Varices: PUD: Hepatitis Acute IgM anti HAV HAV RNA IgM anti HBcAg HBsAg HBeAg HBV DNA A B C HCV RNA D HDV RNA PUD in 20%; most common cause; duodenal > gastric Symptoms in 20%; endoscopic evidence in 50%; 2 nd most common cause; gastric > duodenal Decr LOS, active bleeding at endoscopy, need for OT No effect on transfusion, recurrence, mortality Heal earlier Better at treating Sx than omeprazole Heals 85% duodenal in 4-8/52, 70% gastric in 8/52 80% relapse at 1yr if no maintenance For NSAID related disease Better in smokers For H pylori related disease Decr active bleeding; transfusion need by 33%; as effective as sclerotherapy Decr rebleeding by 60%, mortality by 45%, emergent OT by 65% Controls bleeding in 70-90% 50% recurrence; 25-30% complication rate stops bleeding in 80-90% 40% complication rate for sclerotherapy Stops bleeding in 90%; 25% decr 1yr mortality, 50% decr rebleeding Stops bleeding in 80% Haem 20% (most common), penetration 20%, perf 5%, GOO 2% Previous Chronic No Carrier No Immune IgG anti HAV . Anti HBsAg Anti HBeAg IgG anti HBcAg 5-10% HBsAg >6/12 HBeAg (phase 2) IgG anti HBcAg Anti HBeAg (phase 3) Hep B DNA 75-85% (less in kids) IgG anti HCV 5-10% co, 80% super 1-10% HBsAg IgG anti HBsAg . 0.2-1% - Low - . IgM anti HDV HEV Ag IgM anti HEV E IgG anti HDV . No IgG anti HEV IgG anti HEV HAEMATOLOGY Clotting probs retroperitoneal bleeding, intra-articular bleeding, delayed bleeding Plt probs mucocutaneous bleeding = gum, petechiae, purpura, epistaxis, GI/GU bleed, menorrhagia, bruising DIC incr DD, decr plt (most common lab finding), incr INR, decr fib Absolute Relative Recent bleed <4/52 Surgery <3/52 Active bleeding or diathesis Active PUD Bleed Sig closed HI <3/12 Anticoagulant use Face trauma <3/12 Non-comp vasc punc site CPR >10min Prior ICH Severe/poorly controlled HT Ischemic CVA <3/12 HT >180/110 on presentation Cerebral vasc lesion Ischemic CVA >3/12 Malig lesion 1° or 2° Dementia ICH Aortic dissection Other Pregnancy Pericarditis TOXICOLOGY WBI: Intralipid: MDAC: SR preps Agents that don’t bind charcoal Fe (>60mg/kg) Li (>40mg/kg) Lead, arsenic, SR verapamil/diltiazem, SR KCl (>2.5mmol/kg), body packers, pharmacobezoars LA Propanolol, verapamil TCA Carbamazepine / phenobarb coma, phenytoin, valproate Aspirin Theophylline Quinine NaHCO3: Phenobarb coma Aspirin Methotrexate Haemodialysis: Carbamazepine / phenobarb, valproic acid Aspirin Theophylline Metformin, alcohols Lithium (>6mmol/L acute OD, >2.5mmol/L chronic) Charcoal haemP: Carbamazepine / phenobarb, phenytoin Aspirin, paracetamol Theophylline Amanita DRUGS NO BLOODS Ur Incr Decr Cr Incr Decr Ur:Cr Incr 50-100 Decr max 70:30; onset 4-5mins; MAC 1.02 (weak) Pros: analgesia, amnesia, no decr RR or airway reflexes Cons: diffusion hypoxia at high doses; mask intolerance; vomiting 5-10%; dysphoria 1%; apnoea 1-2% <2yrs, 1:300 otherwise CI: pneumothorax, bowel obstruction, gastric distension, severe HI; severe COPD, decompression illness, >50% O2 needed, decr LOC, pregnancy Renal failure, CCF, dehydration, catabolism, sepsis, OT, steroids, starvation, GI bleed Preg, severe liver disease, low protein diet, anabolism, Ur cycle defects Decr GFR, incr muscle mass, catabolism, muscle disease Elderly, decr muscle mass Prerenal, sepsis, GI bood, dehydration, CCF, RAS, steroids, tetracyclines Renal, acute Renal, chronic; hepatic failure, muscle trauma, preg, trimethoprim CV JVP Apex Heave Thrill S1 S2 Split S1 Split S2 S3 S4 Ejection click Raised Paradoxical Large a Absent a Systolic wave Tapping Prolonged Triple Large RV / LA Loud Soft Loud Soft Increased Fixed Reversed R heart failure, fluid overload, decr HR, SVC obstruction Cardiac tamponade, constrictive pericarditis Tricuspid stenosis, pul HTN, pul stenosis, CHB, flutter, HOCM, AS AF TR MS AS HOCM Severe AS MS, TS MR AS AR Tachy LBBB, 1st deg HB, MI HTN MI RBBB RBBB PS, MR, VSD ASD AS, coarctation LBBB Rapid diastolic filling; CCF, AR, MR, VSD, PDA, MI, maybe physiological Poorly compliant V; AS, PS, MR, pul HTN, HTN, MI AS Mid-systolic click Opening snap PSM ESM Late systolic Early diastolic Mid diastolic Continuous Inspiration Expiration HOCM AS AR MS MR MV prolapse MV prolapse MS MR, TR AS, PS MV prolapse AR, PR MS, TS VSD ASD PDA, coarctation, venous hum Incr R murmurs Incr L murmurs Incr by Valsalva and standing; decr by squatting, hand grip, leg elevation; SM Loud reverse split S2, S4, ejection click, ESM, large a wave, narrow pulse p, slow rising pulse, sustained displaced apex beat, thrill if severe, LVH on ECG Soft S2, S3, early diastolic murmur (+/- SM), Corrigan’s sign, Quinke’s sign, Traube’s sign, Duroziez’s sign, water hammer pulse, wide pulse p, Austin Flint murmur, displaced apex beat, LVH Loud S1, opening snap, mid diastolic murmur, tapping apex beat, small pulse p, thrill; RAD; RV strain; P mitrale, AF Soft S1, incr splitting S2, S3, S4, PSM, small vol pulse, RAD, LV strain, P mitrale, AF Mid-systolic click, late systolic murmur Anti-arrhythmics: IA IB IC II III IV Procainamide, quinidine, disopyramide Lignocaine, phenytoin Flecainide Beta-blockers Ca antagonists Wide QRS, QT Wide QRS, PR Long PR; HB Wide PR, QRS, QT Long PR OK in WPW: Flecainide, procainamide, verapamil (if narrow complex) Not OK in WPW: Adenosine, BB, Ca antagonists, dig Cyanotic heart disease TOF Total anomalous venous drainage TGA Truncus arteriosus Tricuspid atresia ECG Decr complex size; Osborn wave (esp II, III, aVF, precordial); HB’s; AF, VF, asystole, prolonged PR, long QRS and QT, STE Long QTc; AF, SVT, RBBB Hypothermia Hyperthermia RESPIRATORY Cavitating lung lesions: Cancer: SCC; Hodgkins Autoimmune: granulomatosis, sarcoidosis, Wegener’s, RA, progressive massive fibrosis Vascular: septic emboli, pul infarct Infectious: Staph aureus Klebsiella G-ives, anaerobes Fungi, aspiration, 2Y TB Infected bullae / cysts Trauma: traumatic cyst Young: bronchogenic cyst, laryngotracheal papillomatosis Abscess Staph aureus (esp if immunocompromised) Klebseilla G-ive, anaerobes (esp if immunocompetent) Fungi (aspergillus, cryptococcal), aspiration, 2Y TB Aspiration Staph aureus, strep pneumonia Klebsiella G-ives, anaerobes E coli, enterobacter, H influenza, pseudomonas CXR initially normal in 25%; 40% who aspirate get pneumonia Empyema/effusion Staph aureus, strep pneumonaie (esp effusion) Empyema Klebsiella Pseudomonas, nocardia, TB Effusion G-ives, anaerobes Mycoplasma, Hib CCF, trauma, PE, Ca (more likely if large), autoimmune, renal failure R = ovarian Ca L = pancreatitis, chylothorax, CCF Round pneumonia Strep pneumonia, staph Legionella Coxiella Interstitial lung disease: A-SHITFACED Diffuse, tiny, haze A typicals S arcoidosis H istiocytosis I diopathic Viral, atypicals, radiation T umour F ailure A utoimmune Mets, lymphangitis SLE, RA, scleroderma, granulomatosis C ollagen vascular disease E nvironmental D rugs Pul fibrosis Ground glass, reticular Linear and nodules Upper zone SETCARP Asbestosis, silicosis, coal, farmer Methotrexate, amiodarone S ilicosis, sarcoidosis E osinophilic pneumonia TB C oal, CF Dirty looking A spergillosis, ank R adiation spond P CP, pneumoconiosis Lower zone BADRASH B ronchiectasis A spiration D rugs RA Methotrexate, nitrofurantoin, hydralazine, amiodarone, paraquat, smoke inhalation A stebestos S cleroderma H amman Rich, histiocytosis Honeycomb BIGHIPS Pul nodules: CAVIE C ancer A utoimmune V ascular I nfection E nviro B leomycin I diopathic G ranulomas H istiocytosis I nterstitial pneumonia P neumoconiosis S arcoidosis Adenoma Neoplasia Mets Colon, breast, renal, testicular, melanoma, TCC AdenoCa Central SCC, small cell Peri Large cell, bronchoalveolar Granulomatosis, RA, Wegener’s, silicosis AVM, haemartoma, PE, infarct Round pneumonia Miliary TB Varicella pneumonia Fungal Histoplasmosis, aspergilloma Pleural plaques Pleural masses MALLETS M esothelioma A denoCa, asbestosis L ymphoma, leukaemia E mpysema T hymoma S plenosis NEUROLOGY MCA Contralat face+arm >leg hemiplegia + sensory loss Honomynous hemianopia Dom: aphasia, agnosia (Broca’s and Wernicke’s) Non-dom: spatial neglect, dressing apraxia ACA Contralat leg > arm hemiplegia + sensory loss Disorder of conjugate gaze Confusion, personality change Dom: aphasia Non-dom: neglect, confusion Opthalmic Amaurosis fugax PCA Ipsilat cranial nerve III deficit Contralat sensory loss Honomynous hemianopia, quadrantanopia VertebroB Ipsilat cranial nerve deficit Contralat body signs Cerebellar signs NO MOTOR LOSS Lat med S Ipsilat VII, IX, X Horner’s syndrome, ipsilat facial numbness, dysphagia, dysarthria Contralat loss pain and T in body NO MOTOR LOSS Disorder of conjugate gaze Cerebellar signs Wallenberg Ipsilat facial loss of pain and T, weakness Contralat loss pain and T in body, weakness Cerebellar signs Int capsule Contralat motor loss NO SENSORY LOSS Thalamus Contralat sensory loss NO MOTOR LOSS Wasting Tone Fasciculations Reflexes UMN acute None Decr No Incr UMN chronic Mild Incr No Incr LMN Severe Decr Yes Decr Plantar Up Up None Spinal cord NMJ Loss at level Incr below level Normal Fatiguable ILCOR changes Major 30 chest immediately Minor AED ASAP – now BLS skill Change op Q2min Annual BLS training Emphasis on signs of life rather than vital No finger sweep Chest compressions only OK Place hand over centre of chest Precordial thump de-emphasised Major No interruptions – push hard, push fast Compress charging Change Q2min No atropine ETCO2 Minor 100/min Drug IV/IO not ETT Single shocks 200J USS for checking heart activity Avoid hyperoxia Hypothermia for surivivors Precordial thump for witnessed collapse Angioplasty post ROSC CT head: Lat ventricle 3rd ventricle quadrigeminal cistern, suprasellar cistern 4th ventricle Ring enhancing lesions: Mets Radiation necrosis Tuberculoma Haematoma (resolving) Aneurysm Multiple sclerosis Primary brain tumour (glioblastoma, CNS lymphoma, cystic astrocytoma) Abscess toxoplasma, TB cryptococcus, candida Staph aureus, strep prevotella, pseudomonas anaerobes, bacteroides neurosyphilis A. Synovial Fluid Class 2 Class 3 Class 4 Inflammatory* Purulent Hemorrhagic Cloudy-opaque Cloudy-opaque Cloudy Dark yellow Dark yellow-green Pink-red Volume (ml) >3.5 >3.5 >3.5 Viscosity Low Low Variable 3000-100,000 >40,000 >2000 Wbc/L PMNs 30% 50% 75% Gram + culture Neg Usually positive Neg Glc:serum < << = Differentials Rheumatoid Pyogenic Trauma Gout S. aureus Fracture Pseudogout Gonococcus Bleeding Reiter’s (25% G+C only) diathesis Ank spond Hemophilia Psoriatic Neuropathic Sarcoid Hemangioma IBD Bleeding Scleroderma neoplasm Rh fever TB, viral *pseudogout = pos birefringence; gout = neg birefringence; RA = phagocytic PMN inclusions; Reiters = phagocytosis of leucs by macrophages Type of fluid Appearance Normal Normal Clear Light yellow <3.5 High <200 <25% Neg = N/A Class I Non-inflamm Clear Light yellow >3.5 High 200-2000 <25% Neg = Degenerative Trauma AVN Neuropathic HPOA Early inflamm B. CSF Parameter Pressure cmH2O Wcc/mm3 Predominant cell type Glucose Protein Normal 7-20 <5 neonates <30 Lymphocytes 0 PMNs 0.6 x serum 0.8 in neonates 15-45 mg/dl Bacterial Very high >200 up to 20,000 PMN (10% lymphocytes) Low 0.3 x serum High > 50 Viral N / slightly high <1000 TB / Fungal Very high in TB <1000 Lymphocytes (50% PMN initially) Normal or high Lymphocytes Normal or high High Low / N Organisms 90 in infants 0 80% +ve 60% if pretreated 0 80% +ve ZN 90% crypto Ag C. Abdominal Paracentesis Traditionally classified as transudate vs exudate More useful is serum-ascites albumin gradient (SAAG) SAAG Protein pH LDH Glucose WCC Causes Transudate High (>11g/l) < 30g/l > 7.3 Low Normal <1000 /l Portal HT present: Cirrhosis Heart failure Constrictive pericarditis Budd-Chiari or veno-occlusive disease Exudate Low (<11g/l) > 30g/l < 7.3 High Low > 1000 /l Non-portal HT etiology: Malignancy Inflammatory / Infection Pancreatitis Lymphatic obstruction Bacterial peritonitis likely if: (ADHB RMO Handbook 2005) Wcc > 500 x 106 / L Predominantly neutrophils