ST Vincent lectures
advertisement

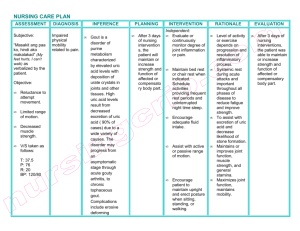
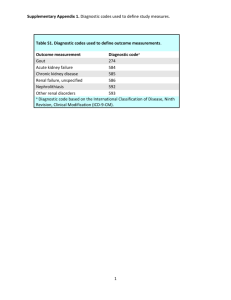
Case 3 - Acute L Ankle COMPLAINT 56 yr. old white woman complains of new onset left ankle pain and swelling for 6 days. Case 3 - Acute L Ankle HISTORY Complains of difficulty walking and warmth over the ankle. Self-treated with rest, elevation and taking "6 aspirins daily". Denies trauma, fever, or prior episodes joint swelling. Past history: NIDDM, coronary artery disease, and CHF. Medications: Digoxin, furosemide, KCL, glyburide and aspirin. Case 3 - Acute L Ankle EXAMINATION All joints were normal, except the left ankle. Left ankle - moderate warmth, erythema, tenderness and swelling present. Case 3 - Acute L Ankle INVESTIGATIONS Glucose = 244 mg/dl Creatinine = 2.4 mg/dl Uric acid = 6.7 mg/dl WBC = 13,000/mm3 ESR = 88 mm/hr. Case 3 - Acute L Ankle What diagnostic test(s) are warranted? Joint aspiration Radiographs of ankles and feet MR image of the lumbosacral spine Rheumatoid factor Repeat serum uric acid None of the above Case 3 - Acute L Ankle ADDITIONAL INVESTIGATIONS Synovial Fluid Analysis Amount aspirated: 10 ml Appearance: Cloudy, yellow WBC count: 34,000 cells/mm3 (89% PMNs) Gram stain/Culture: negative Crystals: negatively birefringent MSU crystals Gout Disorder of urate metabolism, results in deposition of monosodium urate (MSU) crystals in joints and soft tissues. 1st described 5th century BC – Hippocrates described gout as “the king of diseases and the disease of kings” Burden: In 1981, 37 million lost work days in US* 2003 Kim et al estimates the annual cost of Acute Gout is $27,378,494 in the USA (underestimate: women excluded & not all indirect and intangible costs included) * Roubenoff et al Gout Primary gout: from purine metabolism abnormalities (HGPRT defic. or PRPP synthetase) or from idiopathic decreased renal excretion of urate. Secondary gout: neoplasms, Alcohol, lymphoproliferative disease, chronic renal failure, psoriasis, or drug therapy (eg, diuretics, ethanol, cytotoxics). Most patients are Underexcreters rather than Overproducers Gout Epidemiology Men: onset is 40-50 yrs (most common inflammatory arthritis in men) Women: peak onset is post-menopausal Less than have 15% onset prior to menopause Prevalence influenced by hormonal, geographic, racial, genetic, dietary, background conditions: Males > Females. Estrogen is uricosuric Populations: Maori, Tokelauan migrants, Filipinos, Taiwan males, etc (genetics or dietary) renal transplant (2-13%); HTN (RR 2.7+) Seasonal:Gout more often in spring (possibly summer) Is the frequency of gout increasing over time? Is the Frequency Increasing? Author NHIS Population Self-report (prevalence) Rochester Arromdee MN Wallace Wortmann USA Managed Care 1st Era Incidence rate 2nd Era Incidence rate 1969 5/1000 1996 9.4/1000 1977-78 45/100,000 1995-96 62.3/100,00 1990 2.9/1000 1999 5.2/1000 Testing? Increasing life-span? Insulin resistance? Obesity? Prevalence of Gout Age (years) 20-29 Men 3.4 Million Population % 0.2 Women 1.7 Mill Population % 0.6 30-39 2.1 0.1 40-49 2.2 0.6 50-59 5.7 2.3 60-69 9.1 3.5 70-79 10.8 4.7 >80 8.6 5.6 •NHANES III 1988-94 Serum Uric Acid & Incidence of Gout* Serum Urate mg/dl Gout Incidence/yr/1000 5 year cummulative < 7.0 0.8 5 7.0 – 7.9 0.9 6 8.0 – 8.9 4.1 9.8 > 9.0 49 (4.9%) 220 (22%) *Campion EW et al (1963-87) Am J Med 82:421-26, 1987 NHANES III 1988-94 (5.6%) •National (2.7%) Health Intv Survey (&PE) = 17,030 men/women Diet and Gout Low Purine Diet High Purine Diet Cereals, bread, pasta Milk, dairy products, eggs Sugar, gelatin Butter, margarine, fats Fruit, peanut butter Lettuce, tomato, greens All Meats, Anchovies Seafood, herring, sardines Yeast, beer, alcohol, sweetbreads Beans, peas, lentils, oatmeal, spinach, asparagus, cauliflower, mushrooms Survey of 47150 males over 12 yrs. (w/ no hx Gout). Identified 730 new cases of gout Comparing highest and lowest quintiles: RR • Meat intake 1.41 (1.07-1.86) • Seafood intake 1.51 (1.17 – 1.95) • Dairy products 0.56 (0.42-0.74) • Purine Vegetables and protein intake were not associated with increased risk of gout Choy HK. NEJM 350:1093, 2004 Alcohol and Gout Choy HK. Lancet 363:1277-81, 2004 Surveys of 47150 males over 12 yrs( w/ no hx Gout) Identified 730 incident cases RR Relative Risk: 10-15 g/d 1.32 15-30 g/d 1.49 30-50g/d 1.96 >50g/d 2.53 Beer 1.49 per 12oz serving Wine 1.04 per 4 oz serving Gout Epidemiology Associations: Precipitants: Hypertension Alcohol Obesity Hospitalization (fever,Poly) Diabetes Surgery: joint replacement, Renal insufficiency carpal tunnel release Diuretics/congestive heart Drugs: Diuretics, ASA, IV failure NTG, PZA, GCSF, CyA Alcohol consumption Total parenteral nutrition Lead exposure Septic arthritis, reactive Family history arthritis, lupus, elderly Saturnine Gout Saturnine gout: gout due to chronic lead intoxication, either from occult or occupational exposure or the ingestion of moonshine. This account for <5% of cases and is due to lead induced tubulointerstitial renal damage. Saturnine gout should be expected when the magnitude of hyperuricemia exceeds the reduction in glomerular filtration. Gout Acute: intermittent/recurrent, LE, ascending, inflammatory mono/oligoarthritis, “Podagra” Atypical Gout: affects elderly women w/ OA Intercritical (interval) gout: between attacks Tophaceous gout: chronic, accumulation of MSU crystals as “tophi” (may look like RA) Asymptomatic hyperuricema: elevated uric acid without evidence of gout, nephrolithiasis. Higher levels increase risk of these diseases Renal: nephrolithiasis, gouty nephropathy, uric acid nephropathy Acute (Classic) Gout Precipitants: stress, trauma, excess alcohol, infection, surgery, drugs Acute, severe onset of pain, warmth, inflammation, Limited motion cant walk, cant put sheet on it. Podagra (50-90%): pain, swelling warmth in 1st MTP Joints: MTP, tarsus, ankle, knee Assoc. w/ fever, leukocytosis, high ESR or CRP Initially monarthritis (80-90%) and with repeated attacks ascends from the lower extremity (initially a polyarthritis: in elderly, women, myeloproliferative disorders, CyA) Chronology: untreated attacks last 7-14 days. Acute gout risk of repeat attack estimated to be 78% w/in 2 yrs Natural Hx of Acute Attack Bellamy N, et al. Br J Clin Pharmacol 24:33-6, 1987 11 volunteers with acute podagra studied 2 withdrew on day 4 for severe pain 9 remaining showed improvement • Pain by day 5 • Swelling by day 7 • Tenderness improved in 7/9 by day 7 (2 persisted) • But only 3 noted resolution of pain during 7d study Implications for clinical trial endpoints? Pain improvement/resolution by day 3-5 Resolution of symptoms, return to normal activity Comparison of Gout Forms CLASSIC GOUT Any age Mostly Men Acute onset Monarthritis Asymmetric Lower extremity Rarely tophi 1st seen Mis-Dx cellulitis, Septic jt ATYPICAL GOUT Elderly patients Women > Men Insidious, chronic Polyarthritis Symmetric or asymmetric Upper and lower extrem. Tophic common Mis-Dx: RA, OA, infx * Adapted from Rott KT, Agudelo CA. JAMA 289:2857, 2003 Gouty Tophi Incidence has decreased over last few decades Seen in 25-50% of untreated patients (after 10-20yrs) Location: Olecranon, bursae, digits, helix of ear Damages bone, periarticular structures and soft tissues Palpable measure of total body urate load Other: Renal manifestations Uric acid calculi (seen in10-15% of gout pts) Chronic urate nephropathy (in those with tophi) Acute uric acid nephropathy (in pts undergoing chemotherapy) Hypertensive renal disease is the most common cause of renal disease in gout Assessment of Gout Laboratory Findings Acute gout: 40-49% have normal uric acid levels >90% will be hyperuricemic during intercritical period Leukocytosis common ESR and CRP elevated No indices of chronic inflammatory disease (alb, Hgb) Measureable elevations in IL-6 and IL-1 Radiographic findings Soft tissue swelling (Opacities = tophi) Normal Joint space and Normal ossification Erosions: nonarticular, punched out, Sclerotic margins, overhanging edge Gout: Xray Changes •Soft tissue swelling •Opacities = tophi •Nl Joint space •Nl ossification •Erosions: punched out Sclerotic margins Overhanging edge Treatment Acute Gout NSAIDs Contraindicated? Renal insufficiency Peptic ulcer disease Congestive heart failure NSAID intolerance 1. NSAIDs Antiinflamatory doses no yes Are Corticosteroids Contraindicated? no 2.Corticosteroids yes # Joints Involved? 1 3.Oral Colchicine Intraarticular PO Steroid Lipsky PE, Alarcon GS, Bombardier C, Cush JJ, Ellrodt AG, Gibofsky A, Heudebert G, Kavanaugh AF, et al. Am J Med 103(6A):49S-85S, 1997 >1 Oral or Intraarticular Steroid NSAIDs in Acute Gout FDA approval:indomethacin, naproxen, sulindac Tested: etodolac, flurbiprofen, meclofenamic acid, indoprofen, carprofen, phenylbutazone, piroxicam, isoxicam, fentiazac, ketorolac, etoricoxib Benefits Faster onset of relief (compared with colchcine) • Within 2-4 hours for indomethacin Less toxic (when prescribed appropriately); better tolerated Widespread use and familiarity Cost Colchicine Serious Toxicity, Suidice, & Death Carr AA. Colchicine toxicity. Arch Int Med 115:29, 1965 Ellwood MG, Self poisoning with colchicine. Postgrad Med 47:129, 1971 Baum J, Colchicine use as a suicidal drug by females. J Rheumatol 7:124, 1980 Ferranini E, Marrow aplasia following colchicine in gout. Clin Exp Rheum 2:173,1984 Pasero G. Colchicine: should we still use it? Clin Exp Rheumatol 2:103-4, 1984 Roberts WN. Colchcine in acute gout: reasses risk/benefits. JAMA 257:1920-2, 1987 Wallace SL. Systemic toxicity assoc with the IV colchicine. J Rheum 15:495, 1988 Hoffman RS. Outpatient colchicine poisoning. Del Med J. 65: 257-60, 1993 Lee BI. Colchicine myopathy with cyclosporine. J Korean Med Sci 12:160, 1997 Dawson TM. Colchicine induced rhabdomyolysis. J Rheumatol 24:2045, 1997 Maldonado MA, IV colchicine:retro analysis hosp patient. Clin Exp Rheum 15:487, 1997 Mullins ME. Fatal CVS collapse after acute colchicine. J Toxicol Clin Tox 38:51, 2000 Goldbart A. Fatal colchicine intox in a child. Eur J Pediatr 159:895, 2000 Mullins ME. Troponin I cardiac toxicity w/ colchicine. Am J Emerg Med 18:743, 2000 Sanchez Munoz LA, Acute colchicine poisoning. An Med Intern 17:109, 2000 Dogukan A. Fatal colchicine intoxication w/ CAPD. Clin Nephrol 55:181, 2001 Dixon AJ. Colchicine neutropenia, not overdose. Ann Pharmacother 35:192, 2001 Bonnel RA. Deaths assoc w/ IV colchicine. J Emerg Med 22:385-7, 2002 Jones GR. LC-MS analysis of colchicine fatality. J Anal Toxicol 26:365-9, 2002 Maxwell MJ, Accidental colchicine overdose. Emerg Med J 19:265-7, 2002 Debie K, Colchcine induced rhatbomyolysis in CHF. Acta Cardiol 58: 561, 2003 Phanish MK, Colchicine induced rhabdomyolysis. Am J Med 114 (2) 2/1/03 Asuvdevan AR, Colchicine induced rhabdomyolysis. Am J Med 115 (3) 8/15/03 Deaths associated with IV Colchicine Since 1990, AERS reports 90 deaths associated with IV colchicine use (429 allopurinol) Bonnel RA, et al. J Emerg Med 22:385-7, 2002 20 deaths 1983-2000 (13 AERS, 7 literature) 8F:11M; 17 gout pts (ages 50-91 yrs), 2 FMF(21,31) All exceed rec. dose (2-4 mg). Range 5.5-19 mg Adverse effects: thrombocytopenia (8), leukopenia (8), pancytopenia (3), agranulocytosis (2), aplastic anemia (2), acute renal failure (6), and DIC (4) Death within 1-40 days; 80% showed BM depression 13 risk factors: age > 65 yrs, preexisting medical cond, concomitant NSAIDs, recent oral colchicine use Warnings, precautions, contraindications, dosing NOT followed or were misinterpreted Number of <2 Gouty Attacks per Year >2 yes Treatment of Interval Gout Can pt. Stop Alcohol, Diuretics, Weight Loss? no Hx of nephrolithiasis? yes Tophi present? Serum urate > 11? Serum Creat > 2.0? Uric acid >650mg/24h? Lipsky PE, Alarcon GS, Bombardier C, Cush JJ, Ellrodt AG, Gibofsky A, Heudebert G, Kavanaugh AF, et al. Am J Med 103(6A):49S-85S, 1997 no Uricosuric (Probenecid) Colchicine during initiation Observe Educate Rx Acute Attack yes Allopurinol Therapy (colchicine during Initiation) Gout: management Acute Rx: NSAIDs > steroids > colchicine (oral only) Steroids: PO, IM, intraarticular > 2-3 attacks/year > prophyllaxis? Chronic Rx:colchicine,probenecid,allopurinol Probenecid: uricosuric, promotes excretion Don’t use with CRI, nephrolithiasis or Tophaceous gout Colchicine: (diarrhea) decr. PMN motility Allopurinol: decrease formation- use w/ CRF, renal stones, Tophaceous gout, Uric acid > 11 * * Adjust dose for renal insufficiency Gout Review Demographics: males and postmenopausal females. Incidence rises when uric acid >9.0 Clinical: exquisite tenderness, red, warm, fever, attacks last 7-14 days Labs: High WBC, ESR, uric acid may be normal in 40% of acute attacks. Renal function? 24 hr. uric acid excretion Dx: Hx Plus synovial fluid (inflammatory) crystals (negatively birefringent) or ^uric acid or Xray proof. Differential Dx: septic arthritis, pseudogout, Reiters 55 yr. old “dude” with Oligoarthritis Acute onset (3 wks) of Oligoarthritis: knee and ankle Inflammatory Sxs? fever, 1 hr AM stiffness PMHx: EtOH abuse Exam: T=100.2F, Swollen/warm Left knee and ankle. 2+ L knee effusion. Differential Diagnosis? Tests? Procedures? 55 yr. old “dude” with Oligoarthritis Acute onset (3 wks) of Oligoarthritis: knee and ankle Inflammatory Sxs? fever, 1 hr AM stiffness PMHx: EtOH abuse Exam: T=100.2F, Swollen/warm Left knee and ankle. 2+ L knee effusion. ESR=112, Uric acid=7.5, negative RF & ANA XRAY L Knee: STS, Ca++ of Menisci, -erosion Procedures? RED FLAG CONDITIONS FRACTURE SEPTIC ARTHRITIS GOUT/PSEUDOGOUT CALCIUM PYROPHOSPHATE CRYSTAL DEPOSITION DISEASE (CPPD) Synonyms: Pseudogout, chondrocalcinosis, pyrophosphate arthropathy Chondrocalcinosis: calcification of articular cartilage. Chronic CPPD: damage associated with intraarticular deposition of CPPD crystals. Pseudogout: acute synovitis with intra-articular CPPD crystal deposition. Pseudogout is the most common form of CPPD. CALCIUM PYROPHOSPHATE CRYSTAL DEPOSITION DISEASE (CPPD) OA and aging. hyperparathyroidism hypophosphatasia hypomagnesemia hypothyroidism hypocalciuric hypercalcemia hemochromatosis hemosiderosis CPPD - Dx & Rx Pseudogout: self-limited acute monarticular attacks w/ swelling lasting from 1 day to 4 weeks . Knee>wrist > shoulder >ankle. Fever may occur Chronic CPPD: women. symmetric polyarthritis affecting the knees or hands Chondrocalcinosis:usually incidental radiographic finding. Labs: normal uric acid, high ESR & + WBC Diagnostic Tests: Synovial fluid inflammatory w/ intracellular crystals, weakly positive birefringence. Rx: NSAIDs Intraarticular steroids Colchicine prophyllaxis Synovial Fluid Analysis Visual inspection (color, clarity, hemorrhagic) Viscosity - incr w/ normal (noninflam) SF (long “string sign”) - decreased with inflammatory SF (loss of string sign) Place in tubes: EDTA (purple)-cell count.; Na heparin (green)-Crystals Cell Count and Differential noninflammatory: WBC < 2000/mm3 (PMNs < 75%) inflammatory: WBC = 2000 - 75,000/mm3 (PMNs > 75%) septic: WBC > 60,000/mm3 (PMNs >80%) • GC may have WBC from 30K - 75K Synovial Fluid Analysis Analyze SF immediately by “wet prep” • If cannot, refrigerate @ 4oC. • Delay will lower WBC counts and increase artifacts • MSU crystals will persist for days/weeks. CPPD crystals will decrease over time (days/weeks) Do not do protein or glucose - no predictive value No value to SF urate, RF, ANA, LE cells, complement, LDH Gram stain, c/s, Tbc, fungal, cryptococcal Ag as indicated Use Thayer-Martin media if gonococcal infx is suspected Low Yield Tap Visually inspect, assess viscosity, perform SF culture, do “wet prep” to assess the # and type of cell Indications for Arthrocentesis and Joint Injection Monarthritis (acute/chronic) Suspected infection or crystal-induced arthritis New monarthritis in old polyarthritis Joint effusion and trauma Intrarticular therapy Arthrography Uncertain diagnosis Osteoarthritis with pain RA - focal pain/swelling Acute gouty attack Acute bursitis (r/o septic) Tendinitis Early adhesive capsulitis Reflex sympathetic dystrophy Contraindications to Corticosteroid Injections Suspicion of infected joints or bursae Overlying cellulitis Neuropathic (Charcot) joints Referred pain Known bacteremia Thrombocytopenia (platelets < 50K) Coagulopathy - anticoagulant therapy Uncontrolled diabetes (?) Lack of response to previous injection Prosthetic joints Inaccessible joints (SI, hip, etc) Synovial Fluid Analysis Type I Type II Type III Type IV Noninflamatory Inflammatory Septic Hemorrhagic Appearance Straw Yellow Purulent Bloody Clarity Clear Cloudy Opaque Opaque Normal Decreased Decreased Variable Cell # 200 –2000 2000-75,000 > 60,000 RBC > WBC PMN% < 25% > 60% > 80% OA, Trauma, AVN, SLE RA, Gout, viral Reiters, Tbc Bacterial Crystal Viscosity Examples Trauma, FX, Hemophilia, PVS Leave needle in place, change syringes Knee Joint Injection A Moran – Cush Video Exclusive “I’ve seen the needle and the damage done...” - Neil Young “Harvest” 1972 Complications Allergic reactions: iodine, lidocaine adhesives Vasovagal episodes Local ecchymosis Corticosteroid crystal-induced synovitis Depigmentation of overlying skin Subcutaneous atrophy at injection site Rare: skin/joint infection, hemarthrosis, calcification or rupture of periarticular structures