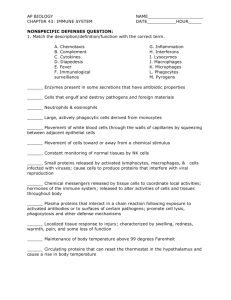
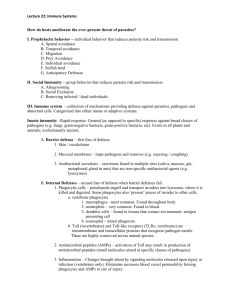
Lecture #12 * Animal Immune Systems
advertisement

Lecture #12 – Animal Immune Systems 1 Key Concepts: • Innate immunity provides broad-spectrum defense against many pathogens • Acquired immunity is very specific, develops over time, and relies on B and T cells • Antigen recognition properties of B and T cells • B and T cell binding sites develop randomly! • Integrated B and T cell function • When the immune system goes wrong… 2 Some definitions…. Generates Pathology • Pathogen = anything that causes disease Microbes (bacteria, protozoans), viruses, fungal spores, pollen, dust mites, etc Secretions (venoms, animal saliva) Non-self tissue cells (transplant rejections) Generates Some cancer cells Antibodies • Antigens = cell surface proteins and other molecules that the body recognizes as nonself Pathogens have Antigens 3 The immune system is spread diffusely throughout the body – a system of organs, nodes and lymph vessels Schematic of the human immune system 4 Remember, the white blood cells are the defenders Diagram of the blood cells 5 Some WBC’s circulate though the lymph, the blood and the interstitial fluid Some are permanently housed in lymph nodes, thymus gland, spleen, appendix and a few other glands 6 Defense is step-wise • 90% of pathogens are neutralized by innate immunity Multiple strategies to destroy pathogens • Any remaining pathogens are normally attacked by the acquired immune system Table showing the stages of defense 7 Innate Immunity – you are born with it • Pathogens are ubiquitous • Innate immunity includes both external and internal systems to eliminate pathogens • Any and all pathogens are targeted • This system does not recognize specific pathogens – it goes after any non-self cell or molecule 8 Innate Immunity – external defenses • Skin – vital barrier • Mucous membranes – trap, cilia evacuate • Secretions – skin and mucous membranes secrete anti-microbial proteins; stomach secretes acids 9 Sweeping cilia in trachea Innate Immunity – internal defenses • Sometimes pathogens get past the barriers and into the tissues • Non-specific WBC’s attack Neutrophils Monocytes macrophages Dendritic cells Eosinophils Basophils 10 Innate Immunity – internal defenses • Phagocytic WBC’s cells ingest and destroy microbes in the tissues Neutrophils – the most abundant, but short-lived Macrophages develop from monocytes – large and longlived, also stimulate acquired Dendritic cells – mostly function to stimulate the acquired immune system 11 Model of a macrophage ingesting a fungal spore 12 Micrograph of macrophage ingesting bacteria 13 Innate Immunity – internal defenses • Eosinophils destroy multicellular parasites by releasing toxic enzymes Also contribute to allergic responses • Basophils contribute to inflammatory and allergic responses 14 Schistosoma mansoni Additional Internal Defenses • Antimicrobial proteins Lysosymes work in macrophages; also found in saliva, tears and mucous Complement proteins result in lysis; also help trigger inflammation and activate acquired immunity Interferons limit intra-cellular spread of viruses Defensins are secreted by macrophages, attack pathogens • Natural killer cells attack virus-infected cells and cancer cells 15 • The inflammatory response Complement Protein Function: these proteins complement other immune system processes Diagram showing complement protein function 16 Additional Internal Defenses • Antimicrobial proteins Lysosymes work in macrophages; also found in saliva, tears and mucous Complement proteins result in lysis; also help trigger inflammation and activate acquired immunity Interferons limit intra-cellular spread of viruses Defensins are secreted by macrophages, attack pathogens • Natural killer cells attack virus-infected cells and cancer cells 17 • The inflammatory response Interferons initiate production of proteins that inhibit viral reproduction Diagram of interferon activity 18 Additional Internal Defenses • Antimicrobial proteins Lysosymes work in macrophages; also found in saliva, tears and mucous Complement proteins result in lysis; also help trigger inflammation and activate acquired immunity Interferons limit intra-cellular spread of viruses Defensins are secreted by macrophages, attack pathogens • Natural killer cells attack virus-infected cells and cancer cells 19 • The inflammatory response Additional Internal Defenses • Antimicrobial proteins Lysosymes work in macrophages; also found in saliva, tears and mucous Complement proteins result in lysis; also help trigger inflammation and activate acquired immunity Interferons limit intra-cellular spread of viruses Defensins are secreted by macrophages, attack pathogens • Natural killer cells attack virus-infected cells and cancer cells 20 • The inflammatory response A natural killer cell (yellow) attacking a cancer cell (red). 21 Additional Internal Defenses • Antimicrobial proteins Lysosymes work in macrophages; also found in saliva, tears and mucous Complement proteins result in lysis; also help trigger inflammation and activate acquired immunity Interferons limit intra-cellular spread of viruses Defensins are secreted by macrophages, attack pathogens • Natural killer cells attack virus-infected cells and cancer cells 22 • The inflammatory response The Inflammatory Response • Usually localized, in response to tissue injury • Cascade of events • May also be systemic – increased WBC release from bone marrow; fever Diagram of the inflammatory response 23 Critical Thinking • Why do tissues swell near a cut??? 24 Critical Thinking • Why do tissues swell near a cut??? • Notice the dilation of the capillary Dilation results from chemical signals released by wounded tissues • Plasma leaks out, along with macrophages and other WBC’s 25 Invertebrates Also Have Innate Defense Systems • Amoeboid cells ingest by phagocytosis in echinoderms • Insect exoskeleton acts as a barrier similar to skin • Hemocytes in insect hemolymph function similarly to vertebrate innate internal defenses • Research indicates little immune system memory Little capacity for acquired immunity as seen in 26 vertebrates Defense is step-wise • 90% of pathogens are neutralized by innate immunity – both external and internal • Any remaining pathogens are normally attacked by the acquired immune system Same diagram of step-wise immune system function 27 Acquired Immunity • Develops over time, in response to exposure to pathogens • Highly specific – lymphocytes develop that match each incoming pathogen B cells and T cells Some circulate in tissues; some are permanently located in lymph nodes, the spleen and other lymph system structures • Pathogen contact with lymphocytes, phagocytes, and other triggers initiates rapid immune responses 28 Remember – the lymph system is closely tied to the circulatory system • Lymph vessels absorb excess fluids in capillary beds • Pathogens in the blood are rapidly exposed to the phagocytes and lymphocytes in the lymph system Every heart beat pushes blood, and any pathogens it carries, past the immune system structures 29 The next 3 slides show the relationship between the capillary beds and the lymph vessels 30 31 Lymph fluid is returned to blood at shoulder ducts Diagram of lymphatic system 32 Remember – the lymph system is closely tied to the circulatory system • Lymph vessels absorb excess fluids in capillary beds • Pathogens in the blood are rapidly exposed to the phagocytes and lymphocytes in the lymph system Every heart beat pushes blood, and any pathogens it carries, past the immune system structures 33 Antigen Recognition by B and T Cells • Remember, antigens are the non-self molecules that initiate the immune response • Mostly cell surface proteins, other cell surface molecules, or toxins dissolved in fluid (venoms and other secretions) • Most pathogens have several different kinds of antigens Because of this, there are usually several different lymphocytes that recognize and respond to the pathogen • Antigens have specific binding sites 34 Membranes are complex, with many surface molecules Diagram showing structure of the cell membrane 35 Antigen Recognition by B and T Cells • Remember, antigens are the non-self molecules that initiate the immune response • Mostly cell surface proteins, other cell surface molecules, or toxins dissolved in fluid (venoms and other secretions) • Most pathogens have several different kinds of antigens Because of this, there are usually several different lymphocytes that recognize and respond to the pathogen • Antigens have specific binding sites 36 Epitopes are the specific binding sites found on all antigens Diagram showing epitope structure 37 Lymphocytes – B and T Cells • Remember, lymphocytes are one of the categories of white blood cells • Each B or T cell has ~100,000 antigen receptors – all of the exact same type Each B or T cell recognizes a single antigen • The receptor molecules and recognition process are different for B cells vs. T cells Both types of receptors are protein-based Both have both constant and variable regions 38 Diagram showing development of all the blood cells and how lymphocytes have a separate origin from other white blood cells. 39 Lymphocytes – B and T Cells • Remember, lymphocytes are one of the categories of white blood cells • Each B or T cell has ~100,000 antigen receptors – all of the exact same type Each B or T cell recognizes a single antigen • The receptor molecules and recognition process are different for B cells vs. T cells Both types of receptors are protein-based Both have both constant and variable regions 40 Constant regions have stable amino acid sequences from cell to cell; Variable regions have different amino acid sequences from cell to cell Diagram showing the receptor molecules in B cells and T cells. This diagram is used several times in the next sequence of slides. 41 Antigen Recognition – B Cells • B cell receptors are Y-shaped • Each branch of the “Y” has 2 parts, called chains Inner, heavy chain makes the full “Y” Outer, light chain is located on the branches of the “Y” Both chains are proteins Chains are linked by chemical bonds • The bottom of the “Y” is anchored in the B cell membrane 42 B Cell Receptor Structure 43 The protein structure of a B cell receptor 44 Antigen Recognition – B Cells • The bottom regions of both chains have constant amino acid sequences • The outer branches of both chains have variable amino acid sequences These variable ends are the antigen binding sites They bind directly to the epitopes B cells recognize unaltered antigens! 45 B Cell Receptor Structure 46 Antigen Recognition – T Cells • • • • T cell receptors are unbranched α chain and β chain are chemically linked Both are anchored in the membrane Both have basal constant regions and terminal variable regions • A single antigen binding site is at the terminus 47 T cell receptor structure 48 T Cells DO NOT recognize intact antigens on intact pathogens • T cells recognize antigen fragments that have been bound to a self-cell protein called a major histocompatibility molecule MHC major histocompatibility complex of genes codes for these molecules • MHC molecules bind to antigen fragments inside a self-cell, and present the fragments at the surface of the cell • T cells detect the presented antigen+MHC complex 49 MHC – self-cell proteins Diagram showing the production of MHC molecules, how they become attached to antigen fragments, and how the complex is presented at the cell surface. This diagram is used repeatedly in the next sequence of slides. 50 T Cells DO NOT recognize intact antigens on intact pathogens • T cells recognize antigen fragments that have been bound to a self-cell protein called a major histocompatibility molecule MHC major histocompatibility complex of genes codes for these molecules • MHC molecules bind to antigen fragments inside a self-cell, and present the fragments at the surface of the cell • T cells detect the presented antigen+MHC complex 51 Development of MHC Variation • MHC alleles are numerous Many more than just the 2 alleles common for most genes (ie: not just dominant vs. recessive) As a result, MHC molecules are the most polymorphic proteins known • Because of the high degree of variation, it is very rare for any two individuals to have the exact same set of MHC molecules MHC molecules are unique to the “self” Help to distinguish “self” from “non-self” cells 52 Development of MHC Variation • MHC alleles are numerous Many more than just the 2 alleles common for most genes (ie: not just dominant vs. recessive) As a result, MHC molecules are the most polymorphic proteins known • Because of the high degree of variation, it is very rare for any two individuals to have the exact same set of MHC molecules MHC molecules are unique to the “self” Help to distinguish “self” from “non-self” cells 53 T Cells DO NOT recognize intact antigens on intact pathogens • T cells recognize antigen fragments that have been bound to a self-cell protein called a major histocompatibility molecule MHC major histocompatibility complex of genes codes for these molecules • MHC molecules bind to antigen fragments inside a self-cell, and present the fragments at the surface of the cell • T cells detect the presented antigen+MHC complex 54 Two classes of MHC molecules: each found in a different type of antigen presenting cell 55 Class I MHC • Found in most nucleated cells • They bind antigen fragments if the cell has been infected, or is cancerous • Class I MHC+antigen complexes are recognized by cytotoxic T cells • Cytotoxic T cells then destroy the infected or cancerous cell 56 Antigen Presentation – Class I MHC molecules are presented on infected or cancerous cells 57 Class II MHC • Found in dendritic cells, macrophages and B cells • Present antigens from pathogens that have been engulfed by phagocytosis • Class II MHC+antigen complexes are recognized by helper T cells • Activated helper T cells begin a cascade of events that control the infection 58 Antigen Presentation – Class II MHC molecules are presented on phagocytic cells 59 In both cases, the T cell recognizes ONLY THE COMBINATION of antigen + self-protein 60 Review: B and T Cell Receptors B cell receptors bind directly to antigen on intact pathogen T cell receptors bind to MHC+antigen complex on self-cells 61 Review: B and T Cell Receptors Remember – both B and T cells have multiple receptors per cell (as many as 100,000), all identical 62 Lymphocyte (B & T cell) Development • Lymphocytes are all produced from stem cells in the bone marrow • Some mature in the bone marrow (B cells) • The rest mature in the thymus gland (T cells) 63 Lymphocyte (B & T cell) Development • Maturation = development of the B and T cell receptors • Once the cells are fully differentiated, they migrate into the rest of the body Some stay permanently in the organs of the lymph system Some circulate constantly through blood, lymph and interstitial fluids 64 Lymphocyte (B & T cell) Development • Step 1 – generation of diversity • Step 2 – testing and removal • Step 3 – clonal selection • Steps 1 and 2 occur during the development of the B and T cells • Step 3 occurs after exposure of the fully developed B and T cells to antigens 65 Lymphocyte (B & T cell) Development Step 1 – generation of diversity • The genes that code for the antigen receptors are randomly rearranged by enzymes during lymphocyte maturation These are the genes that code for the variable regions of the light and heavy chains of B cells • Ditto for the variable regions of the α and β chains of T cells These chains are then linked together to form the T cell receptor molecule 66 Example: gene re-alignment for the light chain of a B cell receptor. Diagram showing the development of diversity in the receptors of a B cell. This diagram is used repeatedly in the next sequence of slides. 67 68 The coding gene has 40 variable (V) segments and 5 joining (J) segments 69 During differentiation of each B cell, one V segment is snipped out and attached to one J segment. Recombinase enzymes randomly snip and join! 70 40 V regions x 5 J regions = 200 possible combinations of V and J in the functional gene. Each cell ends up with only one of these possible combinations for the light chain. 71 The V+J segment is attached via an intron to the C segment that codes for the constant region of the light chain. 72 This “new” gene is processed and translated into the protein that makes up the light chain 73 The DNA coding for the heavy chain goes through the same kind of random rearrangement process, but there are more V regions 74 The light and heavy chains form independently and are then linked Additional variation occurs during the linkage Thus the enormous number of possible receptors Many millions of different receptors are produced in B cells!!! 75 76 Lymphocyte (B & T cell) Development Step 1 – generation of diversity • The genes that code for the antigen receptors are randomly rearranged by enzymes during lymphocyte maturation These are the genes that code for the variable regions of the light and heavy chains of B cells • Ditto for the variable regions of the α and β chains of T cells These chains are then linked together to form the T cell receptor molecule 77 Lymphocyte (B & T cell) Development Step 2 – testing and removal • The rearrangement process is entirely random • Each new receptor is “tested” against selfcells – both during development and during migration into lymph system organs • Receptors that bind to self-cells or self-MHC molecules are eliminated or deactivated 78 Critical Thinking • Why would testing be so important??? 79 Critical Thinking • Why would testing be so important??? • Testing process ensures that the immune system can distinguish self from non-self 80 Differentiation and testing result in an enormous variety of B and T cells – each capable of recognizing a single antigen • ~ 1010 - 1014 different B cells!!!! • Similar numbers of different T cells • Usually no duplication – you start out with a single cell of each type • Clonal selection (the next step) builds a population of duplicate lymphocytes 81 Lymphocyte (B & T cell) Development Step 3 – clonal selection • Each B and T cell has receptors that are specific to a single antigen • Incoming pathogens typically display several antigens • Virtually always, there is a B or T cell receptor to match at least one of the pathogen’s antigens 82 Critical Thinking • How are incoming pathogens exposed to these myriad B and T cells??? 83 Critical Thinking • How are incoming pathogens exposed to these myriad B and T cells??? • Remember the way blood and lymph circulate • Incoming pathogens are rapidly exposed to the B and T cells because of the leaky capillaries and the lymph “vacuum system” 84 Lymphocyte (B & T cell) Development Step 3 – clonal selection • When a lymphocyte receptor encounters a matching antigen, the lymphocyte is activated • Activation = stimulation of the lymphocyte to begin mitotic cloning Diagram showing clonal expansion of selected B cell 85 Lymphocyte (B & T cell) Development Step 3 – clonal selection • Duplicate lymphocytes are rapidly produced • Two clonal populations form • Effector cells are short-lived and carry out the immune system response (varies based on type of lymphocyte – more later) • Memory cells are long-lived and “remember” the epitope Memory cells allow for rapid response to that same pathogen the next time it enters the body 86 Memory cells confer active immunity Clones divide into two populations: effector and memory Diagram showing clonal expansion of selected B cell 87 Lymphocyte (B & T cell) Development Step 3 – clonal selection • Duplicate lymphocytes are rapidly produced • Two clonal populations form • Effector cells are short-lived and carry out the immune system response (varies based on type of lymphocyte – more later) • Memory cells are long-lived and “remember” the epitope Memory cells allow for rapid response to that same pathogen the next time it enters the body 88 Memory cells confer active immunity Step 3 – clonal selection Memory cells accumulate over repeated exposure to the same pathogen EX is for B cells; T cells also accumulate Graph showing accumulation of memory cells after repeated exposures. 89 Critical thinking • If the immune system response is so rapidly initiated, why do we ever get sick??? 90 Critical thinking • If the immune system response is so rapidly initiated, why do we ever get sick??? • Note that the initial response takes about 2 weeks to peak • This is about how long we usually stay sick after first exposure to a new pathogen! • Future exposures are more rapidly attacked 91 Integrated B and T Cell Function Diagram showing how B cell and T cell functions are integrated 92 Simultaneous 93 Helper T Cell Function • Nearly all pathogens activate helper T cells • Dendritic phagocytes 1o activate naïve helper T cells Diagram of helper T cell binding to antigen presenting cell. Important in primary immune response • Macrophages 1o activate memory helper T cells Important in secondary immune response 94 Helper T Cell Function • Clones of active and memory T cells develop after exposure • Active helper T cells secrete proteins that stimulate cytotoxic T cells and B cells 95 Active helper T cells stimulate the rest of the immune system: both cytotoxic T cells and B cells Diagram showing activated helper T cell functions. 96 Cytotoxic T Cell Function • Activated cytotoxic T cells release proteins that perforate target cells & initiate apoptosis • The activated T cell releases, and moves on to target additional infected or cancer cells Diagram showing cytotoxic T cell function Class I MHC molecule 97 B Cell Function • Remember, B cells recognize and bind to specific intact pathogens • B cells also engulf some pathogens by phagocytosis Antigens are presented on the B cell surface These antigens are recognized by helper T cells Helper T cells activate the B cell • Only its one specific antigen can be presented by each type of B cell 98 Some B cells are activated directly by exposure to the antigen 99 B Cell Function • Remember, B cells recognize and bind to specific intact pathogens • B cells also engulf some pathogens by phagocytosis Antigens are presented on the B cell surface These antigens are recognized by helper T cells Helper T cells activate the B cell • Only its one specific antigen can be presented by each type of B cell 100 Most B cells are activated by proteins secreted from active helper T cells Diagram showing an activated helper T activating a B cell 101 B Cell Function • Remember, B cells recognize and bind to specific intact pathogens • B cells also engulf some pathogens by phagocytosis Antigens are presented on the B cell surface These antigens are recognized by helper T cells Helper T cells activate the B cell • Only its one specific antigen can be presented by each type of B cell 102 B Cell Function • Activated B cells form 2 clones – plasma cells and memory cells • Plasma cells release antibodies Diagram showing secretion of antibodies from activated B cell 103 Antibodies • Each activated B cells produces thousands of clones • Each clonal B cell releases nearly a billion antibodies Table of antibodies and their functions 2000 antibodies per second Each B cell has a 4 – 5 day life span 104 Antibodies • Five classes of antibodies are secreted • Each recognizes and attacks specific pathogens • Read through this table for understanding; don’t memorize 105 Antibodies • Only one antibody per type of B cell But remember, most pathogens have multiple antigens with multiple epitopes Many B cells are activated 106 Antibody Mediated Pathogen Disposal Diagram showing how antibodies work 107 Integrated B and T Cell Function • Responses to pathogens are coordinated and simultaneous, NOT mutually exclusive • All components of the immune system are activated • Positive feedback increases function 108 Active vs. Passive Immunity • Active immunity is generated when the acquired immune system is activated Memory cells are generated Exposure to pathogen OR vaccination with inactivated pathogen that still retains antigens Confers long-term protection (often, lifetime) • Passive immunity is generated when antibodies alone are transferred Does not generate memory cells Antibodies cross placenta; are injected Short-term protection 109 Critical Thinking • What would be the advantage of passive immunity??? 110 Critical Thinking • What would be the advantage of passive immunity??? • Rapid protection against very toxic pathogens – rabies virus, snake venoms 111 Immune System Failure • Allergic responses Hypersensitive response to allergenic antigens Antibody tails bind to mast cells Exposure causes massive histamine release • Autoimmune diseases Immune system fails to distinguish self-cells • Immunodeficiency diseases Immune system fails Can be genetic, developmental, or acquired 112 AIDS; also some cancers, chemotherapy, stress Allergic Responses • • • • • • Most generated by IgE antibodies Antibody tail binds to mast cells IgE accumulates on mast cell surface Eventually, allergen binds between 2 IgE This triggers massive release of histamine Histamine dilates blood vessels….. 113 Immune System Failure • Allergic responses Hypersensitive response to allergenic antigens Antibody tails bind to mast cells Exposure causes massive histamine release • Autoimmune diseases Immune system fails to distinguish self-cells • Immunodeficiency diseases Immune system fails Can be genetic, developmental, or acquired 114 AIDS; also some cancers, chemotherapy, stress Rheumatoid Arthritis 115 Diabetes 116 Multiple Sclerosis 117 Lupus 118 Immune System Failure • Allergic responses Hypersensitive response to allergenic antigens Antibody tails bind to mast cells Exposure causes massive histamine release • Autoimmune diseases Immune system fails to distinguish self-cells • Immunodeficiency diseases Immune system fails Can be genetic, developmental, or acquired 119 AIDS; also some cancers, chemotherapy, stress T Cell HIV 120 2007 – 40 million people are infected by HIV; 15 million children have been orphaned by AIDS Graph showing relationship between HIV concentration, antibody concentration and T cell concentration over time. 121 REVIEW – Key Concepts: • Innate immunity provides broad-spectrum defense against many pathogens • Acquired immunity is very specific, develops over time, and relies on B and T cells • Antigen recognition properties of B and T cells • B and T cell binding sites develop randomly! • Integrated B and T cell function • When the immune system goes wrong… 122