(and contraction).
advertisement

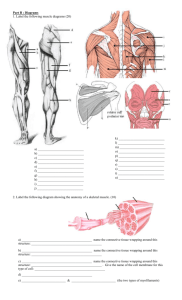
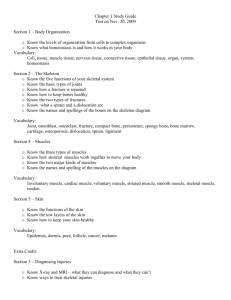
Skeletal Muscle 骨骼肌 Qiang XIA (夏强), PhD Department of Physiology Room C518, Block C, Research Building, School of Medicine Tel: 88206417, 88208252 Email: xiaqiang@zju.edu.cn Muscle Types of muscle: Skeletal muscle骨骼肌 Cardiac muscle 心肌 Smooth muscle平滑肌 Striated muscle 横纹肌 Muscle (cont.) • The sliding filament mechanism(肌丝滑行机制), in which myosin(肌凝蛋白) filaments bind to and move actin (肌纤 蛋白)filaments, is the basis for shortening of stimulated skeletal, smooth, and cardiac muscles. • In all three types of muscle, myosin and actin interactions are regulated by the availability of calcium ions. • Changes in the membrane potential of muscles are linked to internal changes in calcium release (and contraction). Muscle (cont.) • Neuronal influences on the contraction of muscles is affected when neural activity causes changes in the membrane potential of muscles. • Smooth muscles operate in a wide variety of involuntary functions such as regulation of blood pressure and movement of materials in the gut. Structure of skeletal muscle Skeletal muscles are attached to the skeleton by tendons. Skeletal muscles typically contain many, many muscle fibers. The sarcomere(肌小节) is composed of: thick filaments called myosin, anchored in place by titin fibers, and thin filaments called actin, anchored to Z-lines . A cross section through a sarcomere shows that: • each myosin can interact with 6 actin filaments, and • each actin can interact with 3 myosin filaments. Sarcomere structures in an electron micrograph. Filaments Myosin filament (thick filament)粗肌丝 Myosin肌凝蛋白 Actin filament (thin filament)细肌丝 Actin肌纤蛋白 Tropomyosin原肌凝蛋白 Troponin肌钙蛋白 Titin肌联蛋白 Sarcotubular system (1) Transverse Tubule横管 (2) Longitudinal Tubule纵管 Sarcoplasmic reticulum肌浆网 Molecular mechanisms of contraction Sliding-filament mechanism Contraction (shortening): myosin binds to actin, and slides it, pulling the Z-lines closer together, and reducing the width of the I-bands. Note that filament lengths have not changed. Contraction: myosin’s cross-bridges(横桥) bind to actin; the crossbridges then flex to slide actin. Click here to play the Sarcomere Shortening Flash Animation The thick filament called myosin is actually a polymer of myosin molecules, each of which has a flexible cross-bridge that binds ATP and actin. The cross-bridge cycle requires ATP 1. The myosin-binding site on actin becomes available, so the energized cross-bridge binds. 2. 4. Partial hydrolysis of the bound ATP energizes or “re-cocks” the bridge. 3. The full hydrolysis and departure of ADP + Pi causes the flexing of the bound cross-bridge. Binding of a “new” ATP to the cross-bridge uncouples the bridge. 1. The myosin-binding site on actin becomes available, so the energized cross-bridge binds. 2. The full hydrolysis and departure of ADP + Pi causes the flexing of the bound cross-bridge. 3. Binding of a “new” ATP to the cross-bridge uncouples the bridge. 4. Partial hydrolysis of the bound ATP energizes or “re-cocks” the bridge. The cross-bridge cycle requires ATP 1. The myosin-binding site on actin becomes available, so the energized cross-bridge binds. 2. 4. Partial hydrolysis of the bound ATP energizes or “re-cocks” the bridge. 3. The full hydrolysis and departure of ADP + Pi causes the flexing of the bound cross-bridge. Binding of a “new” ATP to the cross-bridge uncouples the bridge. Click here to play the Cross-bridge cycle Flash Animation Roles of troponin, tropomyosin, and calcium in contraction In relaxed skeletal muscle, tropomyosin blocks the cross-bridge binding site on actin. Contraction occurs when calcium ions bind to troponin; this complex then pulls tropomyosin away from the cross-bridge binding site. Interaction of myosin and actin Excitation-contraction coupling 兴奋-收缩偶联 Transmission of action potential (AP) along T tubules Calcium release caused by T tubule AP Contraction initiated by calcium ions The latent period between excitation and development of tension in a skeletal muscle includes the time needed to release Ca++ from sarcoplasmic reticulum, move tropomyosin, and cycle the cross-bridges. The transverse tubules bring action potentials into the interior of the skeletal muscle fibers, so that the wave of depolarization passes close to the sarcoplasmic reticulum, stimulating the release of calcium ions. The extensive meshwork of sarcoplasmic reticulum assures that when it releases calcium ions they can readily diffuse to all of the troponin sites. Passage of an action potential along the transverse tubule opens nearby voltage-gated calcium channels, the “ryanodine receptor,” located on the sarcoplasmic reticulum, and calcium ions released into the cytosol bind to troponin. The calcium-troponin complex “pulls” tropomyosin off the myosin-binding site of actin, thus allowing the binding of the cross-bridge, followed by its flexing to slide the actin filament. Which of these following proteins contains the binding sites for Ca2+ that initiates contraction? A Myosin B Troponin I C Tropomyosin D Troponin C E Troponin T General process of excitation and contraction in skeletal muscle Neuromuscular transmission Excitation-contraction coupling Muscle contraction A single motor unit(运动单位) consists of a motor neuron and all of the muscle fibers it controls. The neuromuscular junction( 神经肌接头)is the point of synaptic contact between the axon terminal of a motor neuron and the muscle fiber it controls. Action potentials in the motor neuron cause Acetylcholine(乙酰胆碱) release into the neuromuscular junction. Muscle contraction follows the delivery of acetylcholine to the muscle fiber. 1. The exocytosis of acetylcholine from the axon terminal occurs when the acetylcholine vesicles merge into the membrane covering the terminal. 2. On the membrane of the muscle fiber, the receptors for acetylcholine respond to its binding by increasing Na+ entry into the fiber, causing a graded depolarization. 3. The graded depolarization typically exceeds threshold for the nearby voltage-gate Na+ and K+ channels, so an action potential occurs on the muscle fiber. Nicotinic acetylcholine receptor 烟碱型乙酰胆碱受体 Acetylcholinesterase 乙酰胆碱酯酶 End plate potential (EPP) 终板电位 Miniature end plate potential 微终板电位 Small fluctuations (typically 0.5 mV) in the resting potential of postsynaptic cells. They are the same shape as, but much smaller than, the end plate potentials caused by stimulation of the presynaptic cell. Miniature end plate potentials are considered as evidence for the quantal release of neurotransmitters at chemical synapses, a single miniature end plate potential resulting from the release of the contents of a single synaptic vesicle. Click here to play the Neuromuscular Junction Flash Animation Click here to play the Action Potentials and Muscle Contraction Flash Animation A woman comes to your clinic and explains that she is noting gradually worsening fatigue/weakness in her legs when she goes for her walk. She also mentions a droopy right eyelid, and wonders if this is a normal aging process.You examine her and find the following: overall decreased muscle strength, trace reflexes throughout, and weakness of eyelid closure bilaterally.The rest of the exam is unremarkable. What would you administer to treat the likely condition? A Muscarinic blockers B Nicotinic blockers C Acetylcholinesterase blockers D Alpha blockers E Beta blockers A woman comes to your clinic and explains that she is noting gradually worsening fatigue/weakness in her legs when she goes for her walk. She also mentions a droopy right eyelid, and wonders if this is a normal aging process.You examine her and find the following: overall decreased muscle strength, trace reflexes throughout, and weakness of eyelid closure bilaterally.The rest of the exam is unremarkable. What would you administer to treat the likely condition? A Muscarinic blockers B Nicotinic blockers C Acetylcholinesterase blockers D Alpha blockers E Beta blockers Neuromuscular transmission A Is caused by the release of acetylcholine from the muscle side of the junction B Shows a permeability change to Na+ and K+ at the receptor site during the endplate potential (EPP) C May be facilitated by curare in myasthenia gravis D Is blocked by curare because it competes with the Na+ entry during the muscle action potential E Is solely an electronic function Neuromuscular transmission A Is caused by the release of acetylcholine from the muscle side of the junction B Shows a permeability change to Na+ and K+ at the receptor site during the endplate potential (EPP) C May be facilitated by curare in myasthenia gravis D Is blocked by curare because it competes with the Na+ entry during the muscle action potential E Is solely an electronic function A miniature end-plate potential is A Not related to changes in ionic permeability B A reduced action potential in the motor endplate C Produced by spontaneous release of acetylcholine D Responsible for weak muscular contractions E An afterdischarge at the neuromuscular junction A miniature end-plate potential is A Not related to changes in ionic permeability B A reduced action potential in the motor endplate C Produced by spontaneous release of acetylcholine D Responsible for weak muscular contractions E An afterdischarge at the neuromuscular junction The action of acetylcholine at the neuromuscular junction is terminated primarily by A Enzymatic breakdown by choline acetylase B Enzymatic breakdown by acetylcholinesterase C Uptake into the muscle D Uptake into the nerve ending E Diffusion into the surrounding extracellular fluid The action of acetylcholine at the neuromuscular junction is terminated primarily by A Enzymatic breakdown by choline acetylase B Enzymatic breakdown by acetylcholinesterase C Uptake into the muscle D Uptake into the nerve ending E Diffusion into the surrounding extracellular fluid The transmission of an action potential over the muscle fiber membrane causes the contraction of the fiber a few milliseconds later. Which of the following terms is used to describe that process? A Ratchet Theory of Muscle Contraction B Excitation Contraction Coupling C Membrane Potential D All-or -Nothing Law The transmission of an action potential over the muscle fiber membrane causes the contraction of the fiber a few milliseconds later. Which of the following terms is used to describe that process? A Ratchet Theory of Muscle Contraction B Excitation Contraction Coupling C Membrane Potential D All-or -Nothing Law Mechanics of single-fiber contraction Muscle tension 肌张力 – the force exerted on an object by a contracting muscle Load 负荷 – the force exerted on the muscle by an object (usually its weight) Isometric contraction 等长收缩 – a muscle develops tension but does not shorten (or lengthen) (constant length) Isotonic contraction 等张收缩 – the muscle shortens while the load on the muscle remains constant (constant tension) Twitch contraction 单收缩 The mechanical response of a single muscle fiber to a single action potential is know as a TWITCH iso = same tonic = tension metric = length Tension increases rapidly and dissipates slowly Shortening occurs slowly, only after taking up elastic tension; the relaxing muscle quickly returns to its resting length. All three are isotonic contractions. 1. 2. 3. 4. Latent period潜伏期 Velocity of shortening Duration of the twitch Distance shortened Load-velocity relation 长度-速度关系 Click here to play the Mechanisms of Single Fiber Contraction Flash Animation Answer the following question by referring to the attached chart. Which curve or line represents the total tension of the muscle? A Curve A B Curve B C Curve C D Curve D E Curve E Answer the following question by referring to the attached chart. Which curve or line represents the total tension of the muscle? A Curve A B Curve B C Curve C D Curve D E Curve E Frequency-tension relation频率-张力关系 Complete dissipation of elastic tension between subsequent stimuli. S3 occurred prior to the complete dissipation of elastic tension from S2. S3 occurred prior to the dissipation of ANY elastic tension from S2. T e m p o r a l s u m m a t i o n. Frequency-tension relation Unfused tetanus非融合性强直收缩: partial dissipation of Fused tetanus融合性强直收缩: elastic tension between no time for dissipation subsequent stimuli. of elastic tension between rapidly recurring stimuli. Mechanism for greater tetanic tension Successive action potentials result in a persistent elevation of cytosolic calcium concentration Length-tension relation Short sarcomere: actin filaments lack room to slide, so little tension can be developed. Optimal-length sarcomere: lots of actin-myosin overlap and plenty of room to slide. Long sarcomere: actin and myosin do not overlap much, so little tension can be developed. Optimal length Click here to play the Length-Tension Relation in Skeletal Muscles Flash Animation In skeletal muscle, ATP production via substrate phosphorylation is supplemented by the availability of creatine phosphate磷酸肌酸. Skeletal muscle’s capacity to produce ATP via oxidative phosphorylation is further supplemented by the availability of molecular oxygen bound to intracellular myoglobin. In skeletal muscle, repetitive stimulation leads to fatigue疲劳, evident as reduced tension. Rest overcomes fatigue, but fatigue will reoccur sooner if inadequate recovery time passes. Types of skeletal muscle fibers On the basis of maximal velocities of shortening Fast fibers快肌纤维 – containing myosin with high ATPase activity (type II fibers) Slow fibers慢肌纤维 -- containing myosin with low ATPase activity (type I fibers) On the basis of major pathway to form ATP Oxidative fibers氧化型肌纤维 – containing numerous mitochondria and having a high capacity for oxidative phosphorylation, also containing large amounts of myoglobin (red muscle fibers) Glycolytic fibers糖酵解型肌纤维 -- containing few mitochondria but possessing a high concentration of glycolytic enzymes and a large store of glycogen, and containing little myoglobin (white muscle fibers) Types of skeletal muscle fibers Slow-oxidative fibers – combine low myosinATPase activity with high oxidative capacity Fast-oxidative fibers -- combine high myosinATPase activity with high oxidative capacity and intermediate glycolytic capacity Fast-glycolytic fibers -- combine high myosin-ATPase activity with high glycolytic capacity Fast-oxidative skeletal muscle responds quickly and to repetitive stimulation without becoming fatigued; muscles used in walking are examples. Fast-glycolytic skeletal muscle is used for quick bursts of strong activation, such as muscles used to jump or to run a short sprint. Most skeletal muscles include all three types. Slow-oxidative skeletal muscle responds well to repetitive stimulation without becoming fatigued; muscles of body posture are examples. Note: Because fast-glycolytic fibers have significant glycolytic capacity, they are sometimes called “fast oxidative-glycolytic [FOG] fibers. Muscles containing many type IIA fibers are called A Red muscles B Slow oxidative muscles C White muscles D Fast glycolytic muscles Muscles containing many type IIA fibers are called A Red muscles B Slow oxidative muscles C White muscles D Fast glycolytic muscles The to A B C D E store of glycogen in the muscle functions Attenuate blood glucose levels directly Provide energy for muscle contraction Provide a source of ketone bodies Provide structural integrity to muscle Inhibit muscle contraction The to A B C D E store of glycogen in the muscle functions Attenuate blood glucose levels directly Provide energy for muscle contraction Provide a source of ketone bodies Provide structural integrity to muscle Inhibit muscle contraction Whole-muscle contraction All three types of muscle fibers are represented in a typical skeletal muscle, Fastglycolytic Fast-oxidative Slow-oxidative and, under tetanic stimulation, make the predicted contributions to the development of muscle tension. Flexors(屈肌) and extensors( 伸肌) work in antagonistic sets to refine movement, and to allow force generation in two opposite directions. How can gastrocnemius contraction result in two different movements? The lever system of muscles and bones: Here, muscle contraction must generate 70 kg force to hold a 10 kg object that is 30 cm away from the site of muscle attachment. Muscle contraction that moves the attachment site on bone 1 cm results in a 7 cm movement of the object 30 cm away from the site; similar gains in movement velocity occur. Duchenne muscular dystrophy(Duchenne型肌营养不良) weakens the hip and trunk muscles, thus altering the lever-system relationships of the muscles and bones that are used to stand up. Case Duchenne muscular dystrophy is a devastating, progressive disease that occurs in boys; it is characterized by the progressive necrosis of skeletal muscle fibers and death at an average age of 16, usually from respiratory failure. It is the second most common genetic disorder in humans, and there is no specific treatment. The course of the disease includes slow muscular development, progressive weakness, and frequent contractures. The disease is usually recognized at ages 2 to 5, and the child is usually confined to a wheelchair by age 12. Laboratory observations show highly elevated serum concentrations of creatine kinase and other soluble sarcoplasmic enzymes. Both fast and slow muscle fibers are affected by fiber necrosis and phagocytosis, balanced by marked regeneration of cells in the early stages of the disease. The fibers resemble fetal muscles, in terms of their isoenzyme patterns, with marked dedifferentiation. Fiber death and replacement by fat and connective tissue gradually predominate. DNA analysis reveals that the disease is caused by the deficiency of a gene on the X chromosome. The product of the gene is a cytoskeletal protein called dystrophin that forms a network adjacent to the sarcolemma. Dystrophin is a very large protein (426 kDa). It is a minor constituent of muscle and links sarcomeres to the sarcolemma via association with a glycoprotein inserted into the membrane. Questions 1. Diseases affecting striated muscle cells are uncommon but are devastating and characteristically lethal. Why? 2. What is the significance of the elevated serum creatine kinase level? 3. Is elevated serum creatine kinase diagnostic for muscular dystrophy? 4. Some muscles are more affected than others. In fact, the muscles of the calves exhibit a characteristic hypertrophy, whereas the muscles of the upper legs are weakened. What factors may influence differential responses in a patient whose skeletal muscle cells lack a functional dystrophin gene? 5. Why is Duchenne muscular dystrophy progressive even though the genetic defect is present from conception? 6. Why don't girls develop Duchenne muscular dystrophy? 7. Exercise is a major component of the clinical management of Duchenne muscular dystrophy. What is the rationale? 8. Would the introduction of a functional allele of the dystrophin gene in the affected cells be a potential treatment that could cure the disease? Thank you!