Acid-Base Physiology
advertisement

Acid-Base Physiology
pH Review
• pH = - log [H+]
• H+ is really a proton!!
• Range is from 0 – 14
• If [H+] is high, the solution is acidic; pH < 7
• If [H+] is low, the solution is basic or alkaline ; pH > 7
2
How Can You Actually
Determine the pH of a Solution?
• Use a pH meter.
• Litmus paper – acidic or alkaline.
• Use pH paper (color patterns indicate pH).
• Titrate the solution with precise amounts of base or acid in
conjunction with a soluble dye, like Phenolphthalein, whose color
changes when a specific pH is reached.
8
4
pH scale – to express hydrogen ion concentration.
The [H+] of ECF is very low (0.00004 mEq/L = 40 nmoles/L).
Normal variations are are markably small 3-5 nEq/L. It is
customary to express these very small numbers using the
logarithmic pH scale.
pH = - log10 [H+] or
pH = log 1 / [H+] log to the base 10 of the
reciprocal of hydrogen-ion concentration.
1) Because [H+] is in the denominator,
A high [H+] low pH and
A low [H+] high pH.
2) pH unit change of 1 = 10X change in [H+]
The Conceptual Problem with pH
• Because it’s a logarithmic scale, it doesn’t make
“sense” to our brains.
• EASY TO REMEMBER FACTS :• Every factor of 10 difference in [H+] represents 1.0 pH units,
• Every factor of 2 difference in [H+] represents 0.3 pH units.
• Therefore, even numerically small differences in pH,
can have profound biological effects…
6
[H+] M
100
A strong acid
10-1
10-2
10-3
10-4
10-5
10-6
10-7
10-8
10-9
10-10
10-11
10-12
10-13
10-14
A strong base
7
ACIDS
• Acids are H+ donors.
• Acids can be:
• Strong – dissociate completely in solution
• HCl
• Weak – dissociate only partially in solution
• Lactic acid, carbonic acid
8
Volatile and Fixed Acids
• VOLATILE ACIDS :- carbonic acid
• Nearly 20,000 mEq of carbonic acid /day
• FIXED ACID :- lactate , keto acids, sulphuric acid, phosphoric acid
• Nearly60-80mEq of fixed acids/day
• 1 mol of glucose 2 moles of lactate
• 3g Sulphuric acid and 3g Phosphoric acid /day
9
BASES
• Bases are acceptors of H+(protons) or give up OH- in
solution
• Bases can be:-
• Strong – dissociate completely in solution
-NaOH
• Weak – dissociate only partially in solution
• NaHCO3
10
Weak acids thus are in equilibrium with their
ionized species:
Governed by the Law of Mass Action, and
characterized by an equilibrium constant:
HA
H+
+
[H ][A ]
+A
-
Ka = [HA]
, pKa = -log Ka
Derivation of the Henderson-Hasselbalch equation
• Ka = [H+] [A-]
[HA]
• so [H+] = Ka [HA]
[A-]
• TAKING THE NEGATIVE LOG OF BOTH SIDES
• As pH = - log [ H+],
• pH = -log Ka [HA]
[A-])
• pH = -log(Ka)-log([HA]
[A-])
• pH = pKa + log([A-]/[HA])
The Henderson Hasselbalch Equation
pH = pKa + log
[A ]
[HA]
L J HENDERSON
K A HASSELBALCH
13
Simplified form……
• pH = pKa + log ([A-]
[HA])
• pH = pKa + log(Conjugate base
Conjugate acid)
• pH = pKa + log(Proton acceptor
Proton donor )
Importance Of Maintenance Of pH Between 7.35 - 7.45(7.4)
Acidosis pH<7.35 and AlkalosispH>7.45.
Death occurs if Ph falls outside the range of 6.8 to 8.0
• Altered [H+] results in changes in protein structure
(Enzymes, Receptors and ligands, Ion
channels,Transporters,Structural proteins)
• Function of excitable tissues
• Acidosis: hypoexcitability, CNS depression
• Alkalosis: hyperexcitability, tetany
• Affects K+ levels in the body.
Relationship of pH with K +
• When H+ increases in extracellular fluid it is exchanged with K+
• Metabolic acidosis Hyperkalemia
• Metabolic alkalosis Hypokalemia
• RENAL TUBULAR ACIDOSIS FAILURE TO EXCRETE H+ K+ IS LOST IN URINE
HYPOKALEMIA
• Rem :- SUDDEN HYPOKALEMIA MAY DEVELOP IN CORRECTION OF ACIDOSIS AS IN
DKA WITH INSULIN THERAPY
16
The body produces more acids than bases
• Acids taken with foods…
• Lime juice , Most fruit juices, Colas….
• Acids produced by metabolism of lipids and proteins.
• Cellular metabolism produces CO2.
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3-
17
Continuous addition of H+ ions to the body fluids and
3 Lines Of Defense Against pH Changes due to this:
•
Buffering
•
Changes in ventilation
•
Changes in renal handling of H+
and HCO3-
The Body and pH
• Homeostasis of pH is tightly controlled
• Extracellular fluid = 7.4
• Blood = 7.35 – 7.45
• < 6.8 or > 8.0 death occurs
• Acidosis (acidemia) below 7.35
• Alkalosis (alkalemia) above 7.45
19
20
Mechanisms of Regulation of pH
• FIRST LINE OF DEFENSE : BLOOD BUFFERS
• SECOND LINE OF DEFENSE :- RESPIRATORY REGULATION
• THIRD LINE OF DEFENSE :RENAL REGULATION
21
Three major mechanisms
1. Buffer systems. Buffers act quickly to temporarily
bind H+ removing the highly reactive, excess H+ from
solution. Buffers thus raise pH of body fluids but do
not remove H+ from the body.
2. Exhalation of carbon dioxide. By increasing the rate
and depth of breathing, more carbon dioxide can be
exhaled. Within minutes this reduces the level of
carbonic acid in blood, which raises the blood pH
(reduces blood H+ level).
3. Kidney excretion of H ion. The slowest mechanism,
but the only way to eliminate acids other than
carbonic acid, is through their excretion in urine.
Rates of correction
• Buffers function almost instantaneously
• Respiratory mechanisms take several minutes to hours
• Renal mechanisms may take several hours to days
23
Buffers
• Defn:- Solutions which can resist changes in pH when
acid or alkali is added.
• COMPOSITION OF A BUFFER :• A) Mixture of weak acids with their salt with a strong base
• Mixtures of weak bases with their salt with a strong acid.eg
• H2CO3/NaHCO3 ( BICARBONATE BUFFER)
• CH3COOH/CH3COONa (ACETATE BUFFER)
• NaHPO4/NaH2PO4 ( PHOSPHATE BUFFER)
•
24
BUFFER SYSTEMS IN THE BODY
• FIRST LINE OF DEFENSE.
• THEY ARE EFFECTIVE AS LONG AS THE ACID LOAD IS NOT VERY
HIGH .
• THE BODY’S ALKALI RESERVE SHOULD NOT BE EXHAUSTEDTHIS HAS TO BE REPLENISHED ONCE EXHAUSTED.
25
Buffering of hydrogen Ions in the body fluids
•
•
•
•
Bicarbonate buffer system
Intracellular protein
Hemoglobin Buffer system.
Phosphate buffer system
Buffers Are The1st Line Of Defense. They
Minimize (But Do Not Prevent) Changes In
pH.
Buffer + H+ ↔ Hbuffer
Bicarbonate Buffer
• The most important buffer in plasma.
• 65% of buffering capacity.
• BASE CONSTITUENT :- (HCO3-) Renal Regulation
• ACID CONSTITUENT :- (H2CO3) Respiratory Regulation
28
Bicarbonate buffer
CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3• Sodium Bicarbonate (NaHCO3) and carbonic acid (H2CO3)
• Maintain a 20:1 ratio : HCO3- : H2CO3
HCl + NaHCO3 ↔ H2CO3 + NaCl ; {excess H2CO3 , excess CO2}
NaOH + H2CO3 ↔ NaHCO3 + H2O; { decre H2CO3 ,dec CO2}
29
• Normal bicarbonate level of plasma is 24mmol/L
• The normal pCO2 is 40mm Hg
• The normal carbonic acid concentration is 1.2 mmol/L
Remember these values!!
30
• pKa for carbonic acid is 6.1
• So, applying Henderson –Hasselbalch’s equation
pH= pKa + log [HCO3- ]
[H2CO3]
= 6.1 + log 24
1.2
= 6.1 + log 20
= 6.1 +1.3
= 7.4
31
Relationship between (H+) and the members of a
buffer pair is expresses using-HendersonHasselbalch Equation
pH = pKa + log[HCO3-] / s*[PCO2 ]
pKa = 6.1(dissociation constant)
What Is The Central Message Of HendersonHasselbalch?
pH = pKa +
log(HCO3
/ s.PCO2)
Plasma pH is a simple function of the HCO3- : PCO2
ratio
HCO3- : PCO2 ↑ = pH ↑ (ALKALOSIS) :
Could occur due to either HCO3- ↑(Metabolic alkalosis)
or PCO2 ↓ (respiratory alkalosis)
HCO3- : PCO2 ↓ = pH ↓( ACIDOSIS) :
Could occur either HCO3- ↓(metabolic acidosis)
or PCO2 ↑ (respiratory acidosis)
Davenport diagram showing the relationships among
HCO3-, pH, and PCO2. A shows the normal buffer line
BAC
pH 7.2, HCO3- 15 mM and PCO2 40 mm Hg ?
metabolic acidosis
Davenport diagram showing the relationships among HCO3, pH, and PCO2. .
B shows the changes/compensation occurring in respiratory and metabolic acidosis
and alkalosis
Phosphate buffer:
• Major intracellular buffer
• The main elements of the phosphate buffer system are H2PO4–
and HPO4=.
• H+ + HPO42- ↔ H2PO4• OH- + H2PO4- ↔ H2O + H2PO42-
37
INTRACELLULAR BUFFERS ARE VERY IMPORTANT
11
BUFFERS
TISSUE CELLS
RBC
40
52
BICARBONATE BUFFER
PHOSPHATE
BUFFER(EXTRACELLULAR )
PROTEIN
(EXTRACELLULAR)
6
38
Protein Buffers
• Buffering capacity of protein dependson the pKa
value of the ionizable side chains.
• Includes hemoglobin
• In general ,
• Carboxyl group gives up H+
• Amino Group accepts H+
• Side chains that can buffer H+ are present on amino acids.
39
Protein Buffer System
• The free carboxyl group at one end of a protein acts like an
acid by releasing H+ when pH rises; it dissociates as follows:
ACTION OF HEMOGLOBIN
• GENERATES BICARBONATE BY CARBONIC ANHYDRASE
• In tissues :CO2 + H2O Carbonic Anhydrase
H2CO3
HCO3- + H+
H+ + HbHHb
H2CO3
41
• In THE LUNGS :HHb + O2 HbO2 + H+
HCO3 - + H+ H2CO3
H2CO3 H2O + CO2
THE ACTIVITY OF CARBONIC ANHYDRASE ACTIVITY ALSO
INCREASES IN ACIDOSIS AND DECREASES WITH DECREASED
H+.
42
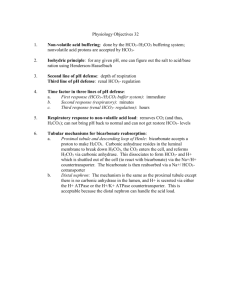
2. Respiratory mechanisms
• 2nd Line of Defence
• Exhalation of carbon dioxide
• Powerful, but only works with volatile acids
• Doesn’t affect fixed acids like lactic acid
• CO2 + H2O ↔ H2CO3 ↔ H+ + HCO3• Body pH can be adjusted by changing rate and depth of breathing
43
Respiratory System is the Second Line of
Defense
The peripheral chemoreceptors
↑
↓
also respond to pH changes
caused by PCO2 changes,
however they directly monitor
changes in the arterial blood, not
the cerebrospinal fluid as the
central chemoreceptors do.
The peripheral
chemoreceptors also
respond to acids such as
lactic acid, which is produced
during strenuous exercise
↑
↑
↑
↑
↑
↑
↓
↑
Central Chemoreceptors: Effect of PCO2 IN REGULATING VENTILATION
↑CO2
CO2 + H2 0
H2 CO3
H+ + HCO-3
↑ H+
Breath
holding
↓pH
central
chemoreceptors
respiratory
centers
in the medulla
capillary
Ventricle
Blood
brain Barrier
• As carbon dioxide increases, so does the number of hydrogen ions, which in turn lowers the pH. The
central chemoreceptors actually respond to this pH change caused by the blood PCO2.
Cellular Respiration Produces CO2 And
“Metabolic Acids”
ECF
Food
Cells
Buffering
metabolic acid
consumes ECF HC0-
H+ + HC03-
3
CO2
CO2
CO2
Lung
• Rate of respiration is controlled by chemoreceptors in the
respiratory centre– sensitive to pH changes in blood.
•
•
FALL in pH of plasma
HYPERVENTILATION
•
•
•
MORE CO2 ELIMINATED
H2CO3 REMOVED
pH increased)
Increasing Alveolar Ventilation Decreases
Extracellular Fluid Hydrogen Ion Concentration
and Raises pH
Increased Hydrogen Ion Concentration Stimulates
Alveolar Ventilation
The Renal System Is The 3rd Line Of
Defense. Changes Are Slow But Powerful
1. Regulation of plasma HCO32. Excretion of fixed (metabolic) acid load
…..Most of the time the urine is acidic to balance metabolic acid
production
RENAL REGULATION
• Can eliminate large amounts of acid.
• Can also excrete base .
• Can conserve and produce bicarb ions
• MOST EFFECTIVE REGULATOR OF pH
• If kidneys fail, pH balance fails
51
Normal Urine(freshly passed) has a pH around 6,i.e
lower than plasma ; ACIDIFICATION OF URINE
52
MAJOR MECHANISMS OF RENAL REGULATION
1. SECRETION OF H+
2. RECOVERY OF HCO3- BY REABSORPTION
3. BICARBONATE IONS ARE “TITRATED” AGAINST HYDROGEN IONS
4.
COMBINATION OF EXCESS HYDROGEN IONS WITH PHOSPHATE AND
AMMONIA BUFFERS IN THE TUBULE—A MECHANISM FOR GENERATING
“NEW” BICARBONATE IONS
5. PRIMARY ACTIVE SECRETION OF HYDROGEN IONS IN THE INTERCALATED
CELLS OF LATE DISTAL AND COLLECTING TUBULES
53
SECRETION OF H+ IN PROXIMAL CONVOLUTED TUBULE
AND RECOVERY OF HCO3- BY REABSORPTION
BLOOD
PCT –CELL
Na+
HCO3-
Alkali is
recovered
TUBULAR LUMEN
Na+
Na+
HCO3- + H+
H+
H2CO3
CARBONIC
ANHYDRASE
H2O + CO2
54
Bicarbonate Ions Are “Titrated” Against
Hydrogen Ions in the Tubules
BLOOD
TUBULAR CELL
TUBULAR LUMEN
NaHCO3
Na+
HCO3-
Alkali is
recovered
Na+
Na+
HCO3- + H+
H2CO3
CARBONIC
ANHYDRASE
H2O + CO2
HCO3-
H+
H2CO3
CARBONIC
ANHYDRASE
H2O + CO2
55
Acid Secretion In The Proximal Tubule
Recovers Filtered HCO3
Lumen
Blood
filtration
Na+
3Na+
NHE3
HCO3H+
2K+
H2CO3
CA
H2O + CO2
H2O
+
CO2
H2CO3
Na+
NBC
HCO3-
CA
CA = carbonic anhydrase
VERY LITTLE ACID EXCRETION OCCURS.
CO2
• In Alkalosis
• there is an excess of HCO3–
over H+ in the tubular filterate,
the excess HCO3– cannot be
reabsorbed; therefore, the
excess HCO3– is left in the
tubules and eventually excreted
into the urine, which helps
correct the metabolic alkalosis.
• In Acidosis
• there is excess H+ relative to
HCO3–, causing complete
reabsorption of the bicarbonate;
the excess H+ passes into the
urine. The excess H+ is buffered
in the tubules by phosphate and
ammonia and eventually
excreted as salts.
Excretion Of “Titratable Acid” Also
Generates New HC03Lumen
filtration
Blood
Na+
3Na+
NHE3
HPO42-
H+
H2PO4-
2K+
H2O
+
CO2
H2CO3
CA
Proximal tubule cell
Na+
NBC
HCO3-
Phosphate Buffer System
BLOOD
(DT)TUBULAR CELL TUBULAR LUMEN
Na2HPO4
Na+
HCO3-
Alkali is
recovered
pH
7.4
Na+ NaHPO4-
Na+
HCO3- + H+
H2CO3
CARBONIC
ANHYDRASE
H2O + CO2
H+
H+
EXCRETED
NaH2PO4
pH
5.4
EXCRETED
59
• Phosphate Buffer System Carries
Excess Hydrogen Ions into the
Urine and Generates New
Bicarbonate
• Excretion of Excess Hydrogen
Ions and Generation of New
Bicarbonate by the Ammonia
Buffer System
Summary Of Renal Acid Base Handling
• Functions of the renal system in acid base balance
• Mechanisms for acid excretion, bicarbonate reabsorption and new
bicarbonate generation.
• Renal responses to acid base disorders
• Interactions between volume and potassium balance and acid-base
balance
PLEASE REMEMBER !!!
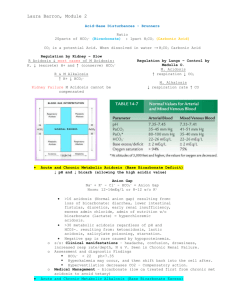
Normal Values
pH
7.35 – 7.45
Bicarbonate
22-26mmol/L
Chloride
96-106mmol/L
Potassium
3.5-5mmol/L
Sodium
136-145mmol/L
pO2
95(85-100) mmHg
pCO2
40(35-45) mmHg
66
COMA
CRAMPS
67
Acid-Base Imbalances
• pH< 7.35 acidosis
• pH > 7.45 alkalosis
• The body response to acid-base imbalance is called compensation
• May be complete if brought back within normal limits
• Partial compensation if range is still outside norms.
68
Acidosis
• Principal effect of acidosis is depression of the CNS through ↓
in synaptic transmission.
• Generalized weakness
• Deranged CNS function the greatest threat
• Severe acidosis causes
• Disorientation
• coma
• death
69
Alkalosis
• Alkalosis causes over excitability of the central and peripheral
nervous systems.
• Numbness
• Lightheadedness
• It can cause :
• Nervousness
• muscle spasms , cramps
• Convulsions
• Loss of consciousness
• Coma
• Death
70
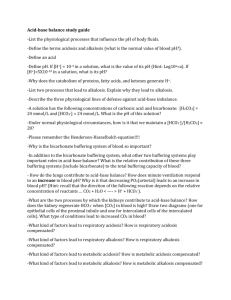
Primary Changes and Compensations in Simple Acid-Base Disorders
Primary
Disturbance
pH
HCO3−
Pco2
Prediction of Compensation
Metabolic
acidosis
< 7.35
Primary decrease
Compensat
ory
decrease
1.2 mm Hg decrease in Pco2 for every 1
mmol/L decrease in HCO3−
Metabolic
alkalosis
> 7.45
Primary increase
Compensat
ory
increase
0.6–0.75 mm Hg increase in Pco2 for
every 1 mmol/L increase in HCO3− (Pco2
should not rise above 55 mm Hg in
compensation)
Respiratory
acidosis
< 7.35
Compensatory
increase
Primary
increase
Acute: 1–2 mmol/L increase in HCO3− for
every 10 mm Hg increase in Pco2
Chronic: 3–4 mmol/L increase in HCO3−
for every 10 mm Hg increase in Pco2
Respiratory
alkalosis
> 7.45
Compensatory
decrease
Primary
decrease
Acute: 1–2 mmol/L decrease in HCO3− for
every 10 mm Hg decrease in Pco2
Chronic: 4–5 mmol/L decrease in HCO3−
for every 10 mm Hg decrease in Pco2
73
http://animalsbeingdicks.com/page/6
Clinical Definitions and Diagnostic Aids
• Respiratory acidosis = PaCO2 > 45 mmHg
• Respiratory alkalosis = PaCO2 < 35 mmHg
• Metabolic acidosis = HCO3- < 22 mmHg or Base
Deficit of < -2
• Metabolic alkalosis = HCO3- > 28 mmHg or Base
Excess of > +2
Acid - Base Diagnosis
PaCO2
< 35 or >45?
No
No Ventilatory
Component
HCO3<21 or >28?
No
No Metabolic
Component
Yes
Metabolic
Alkalosis
HCO3<21?
Yes
Metabolic
Acidosis
Acidemia
Yes
pH
<7.35?
Yes
PaCO2
< 35?
Yes
Yes
Ventilatory
Alkalosis
HCO3>28?
No
PaCO2
>45?
No
Yes
Ventilatory
Acidosis
No
Normal pH
Alkalemia
No
Yes
pH
>7.45?
Diagram source unknown
Case #2
• 36 year old heroin addict found unresponsive with
needle in arm
• P = 102, BP = 110/80, T = 35.2 C
• ABG: PaO2 = 70, PaCO2 = 80,
• pH = 7.00, HCO3- = 23
Respiratory Acidosis
• Carbonic acid excess caused by blood levels of CO2 above 45 mm Hg.
• Hypercapnia – high levels of CO2 in blood
79
Causes
DECREASED FUNCTIONING OF
LUNGS
•
•
•
•
Pneumonia
Bronchitis
Asthma
Pneumothorax
• DEPRESSION OF THE
RESPIRATORY CENTRE
• Head Injury
• Anaesthetics, sedatives (morphine )
• COPD (Emphysema)
• ARDS- Adult Respiratory Distress Syndrome
• Motor neuron disease
80
Signs and Symptoms of Respiratory Acidosis
• Breathlessness
• Restlessness
• Lethargy and disorientation
• Tremors, convulsions, coma.
• Respiratory rate rapid, then gradually depressed.
• Skin warm and flushed due to vasodilation caused by
excess CO2
81
Compensation for Respiratory Acidosis
• Kidneys eliminate hydrogen ion and retain
bicarbonate ion
82
84
Treatment of Respiratory Acidosis
• IV lactate solution
• Treat underlying dysfunction or disease
85
Question :- Why is lactate used ??
86
Case #3
• 16 year old with closed head injury after a fall
from 15 feet
• P = 132, BP = 115/90,
• T = 37.2 C
• ABG: PaO2 = 110, PaCO2 = 26,
• pH = 7.52, HCO3- = 22
Respiratory Alkalosis
• Carbonic acid deficit
• pCO2 less than 35 mm Hg (hypocapnea)
• Most common acid-base imbalance
88
Causes
• Hyperventilation(most common )
• Anxiety, Hysteria etc
• Conditions that stimulate respiratory center:
• Oxygen deficiency at high altitudes
• Pulmonary disease and Congestive heart failure – caused
by hypoxia
• Acute anxiety
• Fever, anemia
• Meningitis
• Cirrhosis
• Gram-negative sepsis
89
Compensation of Respiratory Alkalosis
• Kidneys conserve hydrogen ion
• Excrete more bicarbonate ion( i.e less is resorbed)
90
92
Treatment of Respiratory Alkalosis
• Treat underlying cause
• Breathe into a paper bag
• IV Chloride containing solution – Clions replace lost bicarbonate ions
93
Case #4
• 22 year old diabetic found unresponsive
• P = 102, BP = 110/80,
• T = 36.2 C
• ABG: PaO2 = 90, PaCO2 = 36,
• pH = 7.12, HCO3- = 8
Metabolic Acidosis
• Bicarbonate deficit - blood concentrations of bicarb drop
below 22mEq/L
• Causes:
• Loss of bicarbonate through diarrhea or renal dysfunction
• Accumulation of acids (lactic acid or ketones)
• Failure of kidneys to excrete H+
95
Symptoms of Metabolic Acidosis
• Headache, lethargy
• Nausea, vomiting, diarrhea
• Coma
• Death
96
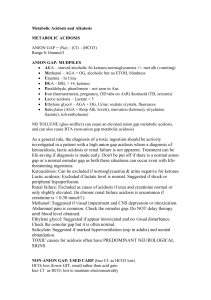
Anion gap; Difference b/w measured cations and measured anions .
97
• Actually the sum of CATIONS and ANIONS in ECF is
always equal.
• There is no gap whatsoever .
• The unmeasured anions constiute the anion gap .( 12± 5
mmol/L)
98
Anion Gap In Metabolic Acidosis
• Anion gap:
[Na+] - ([Cl-] + [HCO3-]) = 8-16 mmol/L
• If > 18, there are unmeasured anions, such as:
•
•
•
•
•
lactate
ketones
salicylate
ethanol
ethylene glycol (anti-freeze)
Explanation
• Say , 5mmol/L Lactic Acid has entered the
circulation Lactate + H+
• Buffered by HCO3• 5mmol/L Lactate + 5mmol/L H2CO3
• H2CO3 H2O + CO2 (LUNGS)
• Finally what has happened
• HCO3- LOWERED +5 mmol/L of UNMEASURED ANION
(LACTATE )
• NO CHANGES IN Na+/K+
• ELEVATED ANION GAP
100
So what does this mean?
• Lactic Acid + HCO3 ↔ lactate- + H2O + CO2
So increasing Lactic acid leads to lactate replacing HCO3
If anion gap is unchanged in metabolic acidosis suggest other reason
for acidosis (eg diarrhoea – loss of HCO3 but gain in Cl-
High Anion-Gap Acidosis
1. Ketoacidosis
•Diabetic ketoacidosis
•Starvation ketoacidosis
2. Lactic Acidosis
3. Renal Failure- Excretion of H+ and regeneration of HCO3- DEFICIENT
4. Toxins
•Ethylene glycol
•Methanol
•Salicylates
MUDPILES (methanol, uremia, diabetic
ketoacidosis, propylene glycol, isoniazid, lactic
acidosis, ethylene glycol, salicylates)
102
Normal Anion-Gap Acidosis
(Loss of both CATIONS AND ANIONS)
1. Renal Causes
•Renal tubular acidosis
•Carbonic anhydrase inhibitors
2. GIT Causes
•Severe diarrhoea
•Uretero-enterostomy or Obstructed ileal conduit
•Drainage of pancreatic or biliary secretions
•Small bowel fistula
3. Other Causes
•Addition of HCl, NH4Cl
103
Compensation for Metabolic Acidosis
• Increased ventilation- to decrease volatile acid
• Increased reapsorption of HCO3- by kidneys
• Renal excretion of hydrogen ions if possible
• K+ exchanges with excess H+ in ECF
• ( H+ into cells, K+ out of cells)
104
106
I.V NaHCO3 is kept as a last reserve !
•
•
•
•
Never give in Cl- losing situations e.g Vomiting
Never in congestive cardiac failure and renal insufficiency
Can cause hypernatremia especially dangerous in children
Celllulitis around the site of infusion
107
Case #5
• 6 week old infant is lethargic with history of
vomiting increasing for 1 week
• P = 122, BP = 85/60,
• T = 37.2 C
• ABG PaO2 = 90, PaCO2 = 44,
• pH = 7.62, HCO3- = 36,
Metabolic Alkalosis
• Bicarbonate excess - concentration in blood is greater than 26
mEq/L
• Causes:
•
•
•
•
•
•
Excess vomiting = loss of stomach acid
Excessive use of alkaline drugs
Certain diuretics
Endocrine disorders:Hyperaldosteronism
Heavy ingestion of antacids
Severe dehydration
109
Symptoms of Metabolic Alkalosis
• Respiration slow and shallow
• Hyperactive reflexes ; tetany
• Often related to depletion of electrolytes
• Atrial tachycardia
• Dysrhythmias
110
Compensation for Metabolic Alkalosis
• RENAL COMPENSATION – decreased reabsorption of HCO3• Kidneys conserve H+ ions
• Sometimes , Alkalosis occurs with renal dysfunction can’t count on kidneys
• Respiratory compensation difficult – hypoventilation limited by
hypoxia
111
112
Treatment of Metabolic Alkalosis
• Electrolytes to replace those lost
• IV chloride containing solution
• Treat underlying disorder
113
Diagnosis of Acid-Base Imbalances
1. Note whether the pH is low (acidosis) or high
(alkalosis)
2. Decide which value, pCO2 or HCO3- , is outside the
normal range and could be the cause of the
problem.
•
•
If the cause is a change in pCO2, the problem is respiratory.
If the cause is HCO3- the problem is metabolic.
114
3. Look at the value that doesn’t correspond to the
observed pH change.
If it is inside the normal range, there is no
compensation occurring.
If it is outside the normal range, the body is partially
compensating for the problem.
115
Example
• A patient is in intensive care because he suffered a severe myocardial
infarction 3 days ago. The lab reports the following values from an
arterial blood sample:
• pH 7.3
• HCO3- = 20 mEq / L ( 22 - 26)
• pCO2 = 32 mm Hg (35 - 45)
116
Diagnosis
• Metabolic acidosis
• With compensation
117
acid base condition
pH 7.58; Pa.CO2 23 mm Hg; [HCO3-] 18 mEq/L
1. Look at pH (is it acidosis or alkalosis?)
pH = 7.58 alkalosis
2. Look at HCO3- (is it metabolic alkalosis?)
HCO3- = 18 mEq/L (normal 22-30) not metabolic alkalosis
3. Look at Pa.CO2 (is it respiratory alkalosis?)
Pa.CO2 = 23 mmHg (normal 35-45) respiratory alkalosis
4. See if appropriate compensation has occurred:
compensation for respiratory alkalosis is HCO3- excretion
HCO3- = 18 mmHg (normal 22-30)
partially compensated respiratory alkalosis
118
Case F2: acid base condition
pH 7.29; Pa.CO2 26 mm Hg; [HCO3-] 12 mEq/L
1. Look at pH (is it acidosis or alkalosis?)
pH = 7.29 acidosis
2. Look at HCO3- (is it metabolic acidosis?)
HCO3- = 12 mEq/L (normal 22-30) metabolic acidosis
3. Look at Pa.CO2 (is it respiratory acidosis?)
Pa.CO2 = 26 mmHg (normal 35-45) not resp. acidosis
4. See if appropriate compensation has occurred:
compensation for metabolic acidosis is hyperventilation
Pa.CO2 = 26 mmHg (normal 35-45); partial compensation
120
Mixed disturbances
Here several problems of acid-base management are
colliding at the same time.
It’s definitely not just a matter of the body trying to
compensate for one such disorder.
a. An example would be a DIABETIC with KETOACIDOSIS, who
also happens to
have C.O.P.D, or develops a bad PNEUMONIA (and as a result
develops a respiratory acidosis.)
123
Siggard Andersen Normogram
124
125
Comments On Compensation…
• Recall HH – compensation aims to normalize pH by
restoring [HCO3]:PCO2 ratio towards normal.
• The “Primary” disturbance is the one that is
consistent with the pH
Mixed Acid-Base Disorders
• Most common acid-base disorders
• Multiple disorders
• Usually one acidosis and one alkalosis
• pH usually partially or completely corrected
Key Points
• Acid-base disorders are common and important clinical concerns
• Accurate diagnosis is essential to proper treatment
• Primary disorders are complicated by secondary disorders occurring
at a different time course