Blood

Blood
Accept no substitute
Artificial Blood?
• Yes it has been developed.
• Unfortunately, the oxygencarrying function, the primary function of blood is very difficult to replicate.
– Can you think of any advantages?
• Demand generally outweighs donations of blood.
• Blood supply is not safe everywhere (HIV, etc.)
• Trauma situations (battlefield, etc.)
Creatures of the Night?
• From Nosferatu (1922) to Daybreakers (2010), vampire just can’t seem to get their fix.
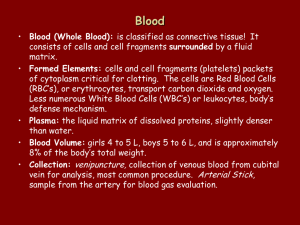
Blood
• Blood is a type of connective tissue whose cells are suspended in a liquid matrix.
• Its cells, formed mostly in bone marrow, include red blood cells, white blood cells, and platelets. These are the formed elements.
• The liquid portion of blood is called plasma.
Blood functions
• Transports nutrients and oxygen = primary function.
• Cellular metabolism
• Homeostasis of fluid volume
• Homeostasis of pH
• Homeostasis of T
• Defense
Blood Volume
• Blood is heavier and 3 x more viscous than water.
• Average adult has blood volume of about 5 liters.
• Men have more blood than women. Men have
1.5 gallons / women have
0.875 gallons.
• Effect of body fat – inversely proportional.
Blood Composition
• Blood is about 45% formed elements.
This is called the hematocrit (HCT).
• Blood plasma = 55%
– Water 92%
– Proteins 7%
– Other solutes 1%
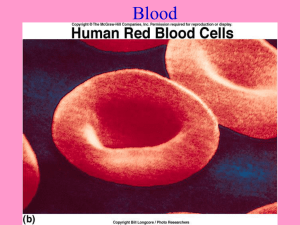
Red Blood Cells - Erythrocytes
• RBCs make up 99.9% of formed elements.
• 5.5 million per cubic mm in men; 4.8 in women
• Blood loss in women reduces their number.
Red Blood Cells - Erythrocytes
• Shape is concave disc.
• Lack nucleus, therefore live only 120 days.
• Shape is function which allows for increased surface area through which gases can diffuse.
• Also allows better transport of Hemoglobin.
Hemoglobin
• Hemoglobin is an oxygencarrying protein.
• It has four parts.
• Each part contains an iron carrying portion = heme and protein portion = globin.
• Fe will carry an oxygen molecule to form iron oxide
(rust) and give blood a red color
• Oxygen taken to cells while carbon dioxide removed
Formation of RBC -
Erythropoiesis
Erythropoiesis
• All blood cells start as stems cells in bone marrow - hemocytoblast.
• Controlled through negative feedback by hormone released from kidney: erythropoietin.
• Released in response to oxygen deficiency.
– Why would this be released when O
2 is low?
Anemia
• When red blood cells can’t carry enough oxygen it is termed anemia
• Normocytic – too few
• Macrocytic – large / less
• Microcytic – too small
• Sickle cell – cell folds on itself (sickles); gets stuck and can’t carry oxygen
• Related to malariaresistance.
RBC Death
• Macrophages are sent in to destroy damaged and old RBCs.
• Hemoglobin is broken down into its heme and globin portions.
• Heme decomposes into iron and biliverdin – a green pigment.
• Often the iron and globin are recycled.
• If not, the biliverdin is converted into bilirubin – an orange pigment.
– Jaundiced patients have ineffective bilirubin excretion.
Jaundice
• Occurs fairly often in newborns.
– Too many RBCs so too much bilirubin production.
• Result of malfunctioning liver or gallbladder with ineffective excretion of bilirubin.
• Here a Russian man has been the victim of bootleg alcohol containing medical disinfectant.
The White Blood Cells
The Armed Forces of the Human Body!
White Blood Cells - Leukocytes
• WBCs protect against disease.
• Develop from stem cells in response to hormones.
• Contain a nucleus.
• No hemoglobin – cannot carry oxygen.
• 5,000 – 9,000 / mm 3 .
Neutrophils – The Marines
• Account for over 50% of the leukocytes in adult humans.
• First to arrive on the scene of infection.
• Phagocytic - engulfs small particles.
• Contains lysosomes, organelles that break down organic matter in captured bacteria.
• Release chemicals to kill bacteria (H2O2, defensins, leukotrienes)
Eosinophils – the Air Force
• Make up only 1-3 % of leukocytes.
• Kill certain parasites.
• Help control inflammation and allergic reactions by removing biochemicals associated with these reactions.
Examples of Human parasites
Basophils – the Navy
• Account for less than 1% of leukocytes.
• Help relieve inflammation.
• Releases histamine
(increases blood flow to injured tissue) and heparin (blood-clotinhibiting substance) therefore keeping things fluid.
Monocytes – the Army
• Largest blood cells – 3 x larger than RBCs.
• Make up less than 10% of leukocytes.
• Live for several weeks or months.
• Phagocytic – devour large bacterial cells
• Go directly to site and release chemicals to attract other WBC
• Attract fibroblasts which begin rebuilding process (scar tissue)
Lymphocytes – the Reserves
• Account for 25-33% of leukocytes.
• Live for many years (in the reserves).
• Most are in lymphatic system.
• Important in immunity – produce antibodies that attack specific foreign substances.
– T Cells – Coordinate immune response
– B Cells – Humoral immunity (antibodies)
– NK Cells (Natural killer cells)– Respond to tumors and viruses.
Check your Understanding
• 1. The most common type of blood cell is the
– A. Leukocyte.
– B. Erythrocyte.
– C. Monocyte.
• 2. The primary function of red blood cells is
– A. Immunity.
– B. Blood transport.
– C. Transport of oxygen.
• 3. The eosinophils are a type of white blood cell whose function it is to
– Help with allergic reactions.
– Attack tumors.
– Engulf large particles.
Platelets - Thrombocytes
• Incomplete cells from fragmented cells in bone marrow called megakaryocytes.
• Lacks nucleus – lives only about 10 days.
• Platelet count varies from 130,000 – 360,000 / mm 3 .
• Platelets help close breaks in damaged blood vessels and initiate formation of blood clots.
Blood Plasma
• Plasma – clear, straw-colored liquid portion of blood in which cells and platelets are suspended.
• Plasma proteins:
– Albumins – osmotic pressure
– Globulins – transport lipids
– Fibrinogens – help coagulation
Hemostasis
• Hemostasis – stoppage of bleeding.
• Coagulation – causes formation of a blood clot.
• Complex with many steps, utilizes many biochemicals called clotting factors.
• Results in scab.
FACTOR “X” – The Clotting Process
• Used to prevent bleeding to death
• Involves calcium ions and
11 plasma proteins
• Cascade of changes occur to make a clot
1. One protein converted to an enzyme that activates the next protein
2. Extrinsic pathway – begins outside bloodstream
3. Intrinsic pathway – inside bloodstream
4. Pathways converge with
Factor “X”
The Extrinsic Pathway
• Starts when a blood vessel is damaged, usually within 15 seconds
• Begins with the release of a lipoprotein, called tissue factor, by damaged cells
• Tissue factor combines with calcium ions and clotting protein called Factor VII
• Factor VII forms and enzyme able to activate
Factor X
The Intrinsic Pathway
• Begins with the activation of a clotting protein exposed to collagen fibers at site of injury
• Pathway assisted with platelet factor
• Along with Calcium and other clotting factors we get series of reactions that lead to Factor X
The Common Pathway
• Begins when intrinsic or extrinsic pathways make factor X
• Factor X changes to enzyme prothrombinase
• Prothrombinase changes prothrombin to thrombin
• Thrombin converts fibrinogen to fibrin
• Fibrin is stringy and catches platelets and cells for “scab”
When Good Clotting Goes Bad
Excessive Coagulation
• Embolus – drifting clot
• Thrombus – blood clot attached to vessel wall
* also known as plaque
Inadequate Coagulation
• Hemophilia – inherited disorder of missing factor
VIII
• Transfusion of plasma can restore clotting factors
• Increases risk of infection from AIDS and HepB
Blood weapons
Timber Rattlesnake (Crotalus horridus)
• Most rattlesnakes have hemotoxic venom.
• Cause hemolysis (destroy RBCs)
• Cause organ degeneration and destroy tissue
• Cause coagulopathy (disrupted blood clotting)
• Why would disrupted blood clotting be an effective blood weapon?
Blood weapons
Hirudinea (Leeches)
• Many leeches are hematophagous but not all can bite. Some survive off decaying matter and already open wounds.
• Leeches secrete an anticoagulant, hirudin, which impairs blood clotting and allows the leech to acquire more blood from the wound.
• Derivatives of hirudin are used in some pharmaceuticals.
• Leeches in Medicine Video
Blood weapons
Vampire Bats (Desmodontinae)
• Vampire Bats Feeding Video
• Vampire bats are hematophagous and feed on the blood of mammals.
• A piece of skin is first removed, painlessly, with razor-sharp front incisors.
• Vampire bat saliva has an anticoagulant, allowing the blood to flow freely, which it then sucks up with its tongue and lower lip.
Blood weapons
Culcidae (Mosquitoes)
• Many female mosquitoes are hematophagous. They drink blood to supplement protein and iron for their developing eggs.
• Mosquito saliva inhibits vascular constriction, blood clotting, platelet aggregation, angiogenesis (growth of new blood vessels), and immunity.
• They are also vectors of many diseases.
• Mosquito Video
Blood weapons
Assassin Bug (Triatominae)
Assassin Bug VS Bat Video a.k.a. The Kissing Bug
• Most of the bugs in this family are hematophagous.
• Widespread in South
America, these insects are vectors for Chagas disease.
• This disease can cause cardiac, nervous, and digestive system damage.
Blood weapons
VS
Blood Groups and Transfusions.
• Early blood transfusions sometimes resulted in blood clumping.
• Agglutination is the clumping of red blood cells following a transfusion reaction.
• Antigens are red blood cell surface molecules.
Known as agglutinogens during clumping.
• Antibodies are proteins carried in the plasma.
They are called agglutinins when they react during clumping.
ABO Blood Group
• Blood groups are based on presence or absence of two major protein antigens on RBC membranes – antigen A and antigen B.
• Every person has four possible combinations of antigens on the surface of their RBCs:
– Only A = Type A Blood (41% of USA)
– Only B = Type B Blood (9% of USA)
– Both A and B = Type AB Blood (3% of USA)
– Neither A or B = Type O Blood (47% of USA)
ABO Blood Group
• 2 to 8 months after birth certain antibodies are produced. This is an inherited trait.
• If antigen A is absent, an antibody called anti-A is produced.
• If antigen B is absent, antibody anti-B is made.
– What antibodies do people with Type A, B, AB, and O blood have?
• An antibody of one type will react with an antigen of another type and clump RBCs.
– Which could be donated to which?
Rh Blood Group
• Named after rhesus monkey. Inherited trait.
• Includes several Rh antigens, main = antigen D
• If antigen D or any other RH antigens are present in the blood, blood is Rh-positive.
• If blood lacks antigens = Rh-negative
• Only 15% of the US has Rh-negataive blood.
• O- = Universal Donor
• AB+ = Universal Acceptor.
– Why?
Rh Blood Group
• If an Rh-negative person receives an Rhpositive transfusion, the Rh antigens began to produce anti-Rh antibodies.
• No effect first time, but now body is sensitized to Rh-positive blood and thus another transfusion of Rh-positive blood could cause the blood to agglutinate.
Rh Blood Group
• This can be a problem with pregnancy.
• If a woman who is Rh-negative conceives a child with an Rh-positive father, their child will be Rh-positive then this blood will enter the woman’s bloodstream.
• The woman’s body will now have antibodies that will attack a second child’s fetal red blood cells.
• Modern medicine can help the child.
Check Your Understanding
• 1. What antibodies does a person with type A blood produce?
– A. anti-A
– B. anti-B
– C. anti-A and anti-B
– D. none
• 2. A person with O- blood can safely receive blood from people with
– A. O- blood
– B. O+ blood
– C. AB+ blood