Blood
advertisement

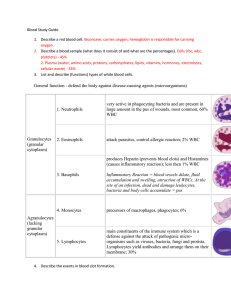
Blood Functions 1. Transport gases 2. Regulates pH by removing acids generated in tissues 3. Protection – Clotting factors to prevent fluid loss – WBC and Antibodies to fight pathogens – Stabilizes body temp Blood Volume and Composition • Blood volume is 8% of body weight • Average adult has 5 liters of blood • Blood is 45% cells – hematocrit or packed cell volume – 99% are red blood cells, remainder white blood cells and blood platelets • Blood is 55% plasma – water, amino acids, proteins, carbohydrates, lipids, vitamins, hormones, electrolytes, wastes Blood Plasma • Clear, straw colored liquid portion of blood where proteins and platelets are suspended • Components – – – – – 92% water Plasma proteins Gases and nutrients Nonprotein nitrogen substances amino acids, urea, uric acid, creatine, creatinine • Plasma electrolytes – sodium, potassium, calcium, magnesium, chloride, bicarbonate, phosphate, sulfate Plasma Proteins • Globulins – 36% of plasma proteins – alpha, beta, gamma globulins • Fibrinogen – 4% of plasma proteins – primary role in blood clotting Figure 14.3 Red Blood Cells • Erythrocytes – Life span of 120 days • Small, biconcave discs • Cells are 1/3 hemoglobin • Mature cells lack nuclei, cannot divide or synthesize proteins • Red blood cells lack mitochondria and produce ATP through glycolysis only Red Blood Cell Destruction • Damaged or worn cells rupture in the spleen or liver. • Macrophages phagocytize and destroy cells. • Hemoglobin is broken down into globin and heme which decomposes into biliverdin. • Biliverdin is converted to bilirubin and excreted in bile. • Iron is carried on transferrin and store in the liver as ferritin. Figure 14.5 Erythropoiesis • Erythrocytes are produced in the red bone marrow. • Average life span is 120 days. • Erythropoietin operates in a negative feedback mechanism to maintain red blood cell homeostasis. • When oxygen concentrations in the blood are low, erythropoietin is released. Anemia Sickle cell anemia Sickle Cell anemia • Herediatry disease of RBC where there is an incorrect AA incorperated in hemoglobin • Causing the cell to “sickle” • Blocks circulation in small vessels and 0xygen is not carried efficiently • Results…joint pain, organ damage Dietary Factors • Vitamin B12 – required for DNA synthesis – intrinsic factor necessary for absorption • Folic acid – required for DNA synthesis • Iron – required for hemoglobin synthesis • Vitamin C – increases absorption of iron White Blood Cells • • • • Leukocytes 5,000-9,000 cubic mm of blood Protect against disease Granulocytes – granular cytoplasm – neutrophils, eosinophils, basophils • Agranulocytes – lack cytoplasmic granules – monocytes, lymphocytes Neutrophils • Granules stain light purple in acid-base combination stains • First white blood cells at arrive at infection • ~70% of WBC Figure 14.9 • Nasal and oral cavity inflammation Eosinophils • Some mild allergic reactions • Defend against parasitic worm infection • 1-3% Figure 14.10 Basophils • Granules stain deep blue in basic stain • Nuclei have two lobes Figure 14.11 Basophils • Migrate to damaged tissue • Allergic rxns: Release histamine to promote inflammation and heparin to inhibit blood clotting • less than 1% of leukocytes Agranulocytes • Monocytes – largest cells – leave bloodstream and become macrophages – 3% to 9% of the leukocytes – FXN: phagocytosis Agranulocytes • Lymphocytes – Aka: T cells and B cells – important in immunity – Help prevent cancer – 35% to 33% of leukocytes Figure 14.13 Leukocytes • Protect against infection – phagocytize bacteria – produce proteins that destroy foreign particles • Diapedesis: leukocytes can squeeze between cells and leave the circulation Figure 14.14 Figure 14.15 Leukocytes • Positive chemotaxis: damaged cells release chemicals that attract leukocytes • Inflammation delays spread of microorganisms Blood Platelets • Thrombocytes • Arise from megakaryocytes in the red bone marrow • Platelets are small and lack a nucleus • Assists in blood clotting: Help repair broken blood vessels • Release serotonin Plasma Proteins • Albumins – 60% of plasma proteins – maintain osmotic pressure, bind and transport molecules Figure 14.16 Blood Gases and Nutrients • Blood gases – oxygen and carbon dioxide • Nutrients – amino acids, simple sugars, nucleotides, lipids – Lipids include triglycerides, phospholipids, cholesterol transported as lipoproteins • chylomicrons, VLDL, LDL, HDL Hemostasis • Stoppage of bleeding to prevent blood loss • Blood vessel spasm – vasospasm due to smooth muscle contraction – direct stimulation of vessel wall and pain reflexes Hemostasis • Platelet plug formation – platelets become spiny and sticky and plug the vascular break Figure 14.17 Blood Coagulation • • • • Complex cascade of events Utilizes clotting factors Vitamin K is necessary for clotting factors Major event is conversion of soluble plasma protein fibrinogen to insoluble treads of fibrin Extrinsic Clotting Mechanism • Triggered when blood contacts damaged blood vessel wall or tissue outside blood vessels • Damaged tissue releases thromboplastin • Thromboplastin activates clotting cascade • These reactions with calcium release prothrombin • Prothrombin is converted into thrombin • Thrombin converts fibrinogen to fibrin Extrinsic Clotting Mechanism • Fibrin threads stick to exposed damaged blood vessels. • Meshwork traps blood cells and platelets. • This produced a blood clot. • The amount of prothrombin activator is proportional to the degree of tissue damage. • Blood clotting is self-initiating, a positive feedback system. Clot Limitation • Blood flow keeps thrombin concentration low • Antithrombin limits thrombin formation • Thrombus: a clot abnormally forming in a vessel • Embolus: a dislodged clot carried by the bloodstream • Embolism: embolus blocking blood flow Intrinsic Clotting Mechanism • All components found in the blood • Activation of Hageman Factor initiates intrinsic clotting • Cascade of activation in the presence of calcium produces prothrombin activator • Prothrombin and fibrin are formed as in the extrinsic pathway Figure 14.19 Fate of Blood Clots • Blood clot retraction occurs pulling torn vessel ends together. • Serum is squeezed out. • Platelet-derived growth factor repairs wall. • Plasminogen is absorbed by fibrin. • Plasminogen activator converts plasminogen to plasmin. • Plasmin digests the clot. Prevention of Coagulation • Endothelial cells produce prostacyclin which inhibits platelet adherence. • Antithrombin inactivates thrombin. • Basophils and mast cells release heparin which interferes with the formation of prothrombin activator. Antigens and Antibodies • Blood cell compatibility is based on clumping or agglutination • Transfusion reaction: a reaction between red blood cell antigens or agglutinogens and protein antibodies or agglutinins in the plasma • Antigens include those of the ABO group and the Rh group Figure 14.22 ABO Blood Group • Based on red blood cell membrane antigen A and antigen B ABO Blood Group • Four possible combinations – Type A contains antigen A – Type B contains antigen B – Type AB contains antigens A and B – Type O contains no antigens Figure 14.21 ABO Blood Group • Anti-A and anti-B antibodies are produced when an antigen is absent from the cell membrane – Type A plasma contains anti-B antibodies – Type B plasma contains anti-A antibodies – Type AB plasma contains anti-A and anti-B antibodies, universal recipient – Type O plasma contains no antibodies, universal donor Rh Blood Group • Rh positive indicates presence of antigen D, one of the Rh antigens • Rh negative indicates absence of Antigen D Figure 14.23 Rh Blood Group • Rh antigens, like A and B antigens are inherited and present from birth • Anti-D antibodies and not produced until after an individual is sensitized to D antigen • http://nobelprize.org/educational_games/me dicine/landsteiner/