Integumentary
advertisement

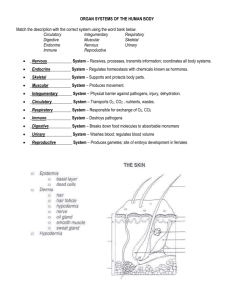
Integumentary System (ch 6) Medical Mystery: no fingerprints 1. What causes dermatopathia pigmentosa reticularis? 2. What treatments are available? 3. List something you thought was interesting about the article. 4. What is something you would like to know more about regarding the article or integumentary system. Why hairy? Read article on p170. • Why are we hairy? • Explain hypertrichosis. • What theories do scientists have about why we have hair in the places we do? • Is there an evolutionary relationship? Explain. • The integument is the largest system of the body is 16% of body weight and 1.5 to 2 m2 in area. • First line of defense • Observed by physicians for health analysis – – – – Color temperature Elasticity sensitivity Parts of the Integument • The integument is made up of 2 parts: 1. cutaneous membrane (skin) 2. accessory structures 3. Sub-Q (subcutaneous) • The integument is the largest system of the body is 16% of body weight and 1.5 to 2 m2 in area. Accessory Structures • Originate in the dermis • Extend through the epidermis to skin surface: – – – – hair nails multicellular exocrine glands Receptors Connections • Circulatory system: – blood vessels in the dermis • Nervous system: – sensory receptors for pain, touch, & temperature The Subcutaneous Layer • Subcutaneous layer (superficial fascia or hypodermis): loose connective tissue, below the dermis, location of hypodermic injections Functions of Skin? • Protects underlying tissues and organs • Excretes salts, water, and organic wastes (glands) • Maintains body temperature (insulation and evaporation) • Synthesizes vitamin D3 • Stores lipids • Detects touch, pressure, pain, and temperature by sensory receptors located in dermis • Characteristics of epidermis: – Avascular, stratified squamous epithelium • How are these cells nourished? – Nutrients and oxygen diffuse from capillaries in the dermis Cells of the Epidermis • Keratinocytes: – contain large amounts of keratin – the most abundant cells in the epidermis – Assist in immune fxn by producing hormone-like substance that stimulates dev of certain WBC. – Thick Skin • Covers the palms of the hands and soles of the feet • Has 5 layers of keratinocytes – Thin Skin • Covers most of the body • Has 4 layers of keratinocytes How do cells of the skin replace themselves? keritization • The formation of a layer of dead, protective cells filled with keratin • Cells begin to harden when tough fibrous waterproof keratin proteins are synthesized and stored within cell. • Occurs on all exposed skin surfaces except eyes Layers of the Epidermis • From basal lamina to free surface: – – – – – stratum stratum stratum stratum stratum germinativum/basale spinosum granulosum lucidum corneum Figure 5–3 Stratum Germinativum • The “germinative layer”: – has many (3-5 cells thick) germinative (stem) cells or basal cells – is attached to basal lamina by hemidesmosomes – forms a strong bond between epidermis and dermis • Structures of Stratum Germinativum – Epidermal ridges (e.g., fingerprints) – Dermal papillae (tiny mounds): • increase the area of basal lamina • strengthen attachment between epidermis and dermis • Cells of Stratum Germinativum – Merkel cells: • found in hairless skin • respond to touch (trigger nervous system) – Melanocytes: • contain the pigment melanin • scattered throughout stratum germinativum Stratum Spinosum • The “spiny layer”: – produced by division of stratum germinosum – 8–10 layers of keratinocytes bound by desmosomes – cells shrink until cytoskeletons stick out (spiny) • Cells of Stratum Spinosum – Continue to divide, increasing thickness of epithelium – Contain Langerhans cells, active in immune response (against pathogens and skin cancers) Stratum Granulosum • The “grainy layer” • Stops dividing, starts producing: – keratin: • a tough, fibrous protein • makes up hair and nails – keratohyalin • dense granules • cross-link keratin fibers • Cells of Stratum Granulosum – Produce protein fibers – Dehydrate and die – Create tightly interlocked layer of keratin surrounded by keratohyalin Stratum Lucidum • The “clear layer”: – found only in thick skin – covers stratum granulosum • Cells of Stratum Lucida – Flat – Dense – Filled with keratin Stratum Corneum • The “horn layer”: – – – – exposed surface of skin 15 to 30 layers of keratinized cells water resistant shed and replaced every 2 weeks What are the structures & functions of the dermis? The Dermis • Is located between epidermis & subcutaneous layer • Fxns to nourish epidermis and house accessory organs of skin • Has 2 components: – outer papillary layer – deep reticular layer Reticular layer • Consists of dense irregular connective tissue • Contains larger blood vessels, lymph vessels, and nerve fibers • Contains collagen and elastic fibers • Houses sensory neurons: pacinian corpuscle: detects deep pressure and vibration The Papillary Layer • Consists of areolar tissue • Contains smaller capillaries, lymphatic vessels, and sensory neurons • Sensory neurons: meissner’s corpuscle: detects ligh touch What are the structures & functions of the subcutaneous layer? The Hypodermis • The subcutaneous layer or hypodermis: – lies below the integument – stabilizes the skin – allows separate movement – made of elastic areolar and adipose tissues – connected to the reticular layer of integument by connective tissue fibers – has few capillaries and no vital organs – is the site of subcutaneous injections using hypodermic needles Adipose Tissue • Deposits of subcutaneous fat: – have distribution pattern determined by hormones – are reduced by cosmetic liposuction Water Loss Through Skin • Dehydration results: – from damage to stratum corneum, e.g., burns and blisters (insensible perspiration) – from immersion in hypertonic solution, e.g., seawater (osmosis) Water Gain Through Skin • Hydration: (skin is water resistant, not water proof) – results from immersion in hypotonic solution, e.g., freshwater (osmosis) – causes stretching and wrinkling skin Perspiration • Insensible perspiration: – interstitial fluid lost by evaporation through the stratum corneum • Sensible perspiration: – water excreted by sweat glands What causes different skin colors? Skin Color • Skin color depends on: – blood circulation (red cells) – the pigments carotene and melanin • Melanin – – – – Yellow-brown or black pigment Produced by melanocytes in stratum germinativum Stored in transport vesicles (melanosomes) Transferred to keratinocytes • Carotene – – – – Orange-yellow pigment Found in orange vegetables Accumulates in epidermal cells and fatty tissues of the dermis Can be converted to vitamin A Function of Melanocytes • Melanin protects skin from sun damage • Skin color depends on melanin production, not number of melanocytes • Ultraviolet (UV) radiation: – causes DNA mutations and burns which lead to cancer and wrinkles Capillaries and Skin Color • Oxygenated red blood contributes to skin color: – blood vessels dilate from heat, skin reddens – blood flow decreases, skin pales • Cyanosis – Bluish skin tint – Caused by severe reduction in blood flow or oxygenation • Jaundice: – buildup of bile produced by liver – yellow color • Addison’s disease: – and other diseases of pituitary gland – skin darkening • Vitiglio: – loss of melanocytes – loss of color Skin Damage • Sagging and wrinkles (reduced skin elasticity) are caused by: – – – – dehydration age hormonal changes UV exposure • Stretch Marks – Thickened tissue resulting from: • excessive stretching of skin due to: – Pregnancy – weight gain Vitamin D • Epidermal cells produce cholecalciferol (vitamin D3): – in the presence of UV radiation • Liver and kidneys convert vitamin D into calcitriol: – to aid absorption of calcium and phosphorus • Insufficient vitamin D: – can cause rickets Epidermal Growth Factor (EGF) • Is a powerful peptide growth factor • Is produced by glands (salivary and duodenum) • Is used in laboratories to grow skin grafts • • • • Functions of EGF Promotes division of germinative cells Accelerates keratin production Stimulates epidermal repair Stimulates glandular secretion Dermatitis • An inflammation of the papillary layer • Caused by infection, radiation, mechanical irritation, or chemicals (e.g., poison ivy) • Characterized by itch or pain • Strong, due to collagen fibers • Elastic, due to elastic fibers • Flexible (skin turgor) Lines of Cleavage • Collagen and elastic fibers in the dermis: – are arranged in parallel bundles – resist force in a specific direction • Lines of cleavage establish important patterns: – a parallel cut remains shut, heals well – a cut across (right angle) pulls open and scars Lines of Cleavage Dermal Circulation Arteries • Cutaneous plexus: – a network of arteries along the reticular layer • Papillary plexus: – capillary network from small arteries in papillary layer Veins • Venous plexus: – capillary return deep to the papillary plexus • Contusion: – damage to blood vessels resulting in “black and blue” bruising Figure 5–8 What determines hair growth, texture,& color? Location of Hair • The human body is covered with hair, except palms, soles, lips, portions of external genitalia • Protects and insulates • Guards openings against particles and insects • Is sensitive to very light touch • Hair FollicleIs – located deep in dermis – Produces nonliving hairs – Is wrapped in a dense connective-tissue sheath – Base is surrounded by sensory nerves (root hair plexus) Accessory Structures of Hair • Arrector pili: – involuntary smooth muscle – causes hairs to stand up – produces “goose bumps” • Sebaceous glands: – lubricate the hair – control bacteria • Hair root: Regions of the Hair – lower part of the hair – attached to the integument • Hair shaft: – upper part of the hair – not attached to the integument How Hair Grows • Hair begins deep in the dermis: – the hair papilla contains capillaries and nerves – the hair bulb produces hair matrix Hair Matrix • A layer of dividing basal cells • Produce hair structure • Push hair up and out of skin Layers in a Hair • Medulla:the central core • Cortex:the middle layer • Cuticle:the surface layer Keratin • As hair is produced, it is keratinized: – medulla contains flexible soft keratin – cortex and cuticle contain stiff hard keratin Layers in the Follicle • Internal root sheath: – the inner layer – contacts the cuticle in lower hair root • External root sheath: – extends from skin surface to hair matrix • Glassy membrane: – a dense connective-tissue sheath – contacts connective tissues of dermis Hair Growth Cycle • Growing hair: – is firmly attached to matrix • Club hair: – is not growing – is attached to an inactive follicle • New hair growth cycle: – follicle becomes active – produces new hair – club hair is shed Types of Hairs • Vellus hairs: – soft, fine – cover body surface • Terminal hairs: – heavy, pigmented – head and eyebrows – other parts of body after puberty Hair Color • Produced by melanocytes at the hair papilla • Determined by genes What are the skin glands & secretions? Exocrine Glands • Sebaceous glands (oil glands): – Simple branched alveolar glands:associated with hair follicles – Sebaceous follicles:discharge directly onto skin surface – holocrine glands – secrete sebum • Contains lipids and other ingredients • Lubricates and protects the epidermis • Inhibits bacteria • Sweat Glands – Apocrine: • found in armpits, around nipples, and groin • Associated with hair follicles • Produce sticky, cloudy secretions • Break down and cause odors – Merocrine glands • widely distributed on body surface especially on palms and soles • Cools skin, flushes microorganisms and harmful chemicals from skin Other Integumentary Glands • Mammary glands: – produce milk • Ceruminous glands: – protect the eardrum – produce cerumen (earwax) What is the structure of nails, & how do they grow? • Nails protect fingers and toes: – made of dead cells packed with keratin – metabolic disorders can change nail structure – produced in a deep epidermal fold near the bone called the nail root • Nail body: – the visible portion of the nail – covers the nail bed • Lunula: – the pale crescent at the base of the nail