Estrogens LH
advertisement

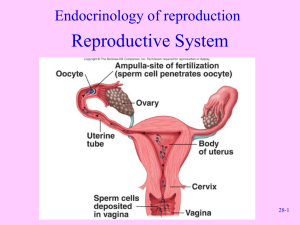
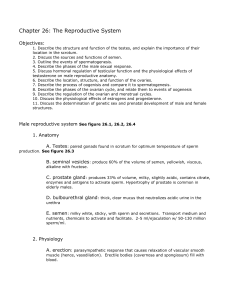
Exam 4 Review Reproductive and Mammary Systems AN S 214 Supplemental Instruction 4/24/13 Reproductive System Outline • • • • • • • • • • • • • • • Male Anatomy Heat Regulation of Testes Hypothalamic-Pituitary-Gonadal Axis Spermatogenesis and Spermiogenesis Female Anatomy Ovarian Cycle Uterine (Menstrual) Cycle Hypothalamic-Pituitary-Gonadal Axis Putting it All Together Fertilization and Development Pregnancy Duct Formation Abnormalities Estrous Cycle Seasonally Polyestrous Male Anatomy • • • • • • • • • Seminiferous Tubules Tubulus Rectus Rete Testis Efferent Ductules Epididymis (Head, Body, Tail) . Seminal Vesicle – Viscous alkaline seminal fluid – Fructose, ascorbic acid, coagulating enzyme, and prostaglandins – 70% of the volume of semen Ejaculatory Duct Prostate – Milky, slightly acid fluid – Contains citrate and enzymes Bulbourethral (Cowper's) gland – Prior to ejaculation-thick, clear mucus – Lubricates the glans penis – Neutralizes traces of acidic urine in the urethra Urethra Glans Penis • Seminal fluid + Sperm = Semen • • • Heat Regulation of Testes • Keeps testes 3 degrees Celsius cooler than body temperature • . – Countercurrent heat exchanger • Cools arterial blood, warm venous blood • . – Smooth muscle that wrinkles scrotal skin • . – Skeletal muscle that raises or lowers testes Hypothalamic-Pituitary-Gonadal Axis • Leydig/Interstitial Cells – – Stimulated by LH Secrete androgens • • • Testosterone Sertoli/Sustenacular Cells – – – – – – Stimulated by FSH Nourishment of developing spermatozoa Form blood-testes barrier Produce inhibin-represses FSH Secrete androgen-binding protein (ABP) Produce mullerian duct-inhibiting substance (MIS) – – – Exogenous testosterone Negative feedback on pituitary Results in infertility, testicular atrophy and impotence . Spermatogenesis and Spermiogenesis • • • • • • Spermatogonium-Most primitive cell – Mitosis Spermatogonium A – Mitosis Spermatogonium B – Mitosis Primary Spermatocytes – Meiosis I Secondary Spermatocytes – Meiosis II Spermatids Spermatogenesis Differentiation • Spermatozoa – Mature Sperm Spermiogenesis Female Anatomy • Path of Oocyte – Ovary – Oviduct • . • . • . – Uterus – Cervix – Vagina • External Genitalia – – – – Clitoris Labia minora Labia majora Accessory glands Ovarian Cycle • Follicular Phase – – Primordial Follicle Primary Follicle • – Secondary Follicle • – • Meiosis occurs Large antrum Ovulation – • Three layers of cells-One being granulosa cells, Two of thecal cells Antrum begins to form Dominant Follicle, Mature Follicle, Graffian Follicle, or Vesicular Follicle • • • Two layers of granulosa cells Tertiary Follicle, Late Secondary Follicle, or Antral Follicle • – One layer of granulosa cells Secondary oocyte expelled Luteal Phase – – – . • “Bloody Body” • “Yellow Body” • “White Body” . . Uterine (Menstrual) Cycle • . – Days 1-5 – Menstrual flow due to low hormone levels • . – Days 6-14 – Estrogen levels prompt new endometrium in uterus • . – Days 15-28 – Progesterone levels prompt further development of endometrium – Glandular secretions Hypothalamic-Pituitary-Gonadal Axis • FSH stimulates Granulosa (G) cells to produce Estrogens • LH stimulates Thecal (T) cells to produce androgens • Estrogen Production – Cholesterol Progesterone (G&T) Testosterone (T) – Aromatase (G)Estradiol (G) Putting it All Together Fertilization and Development • • • • • • • • • • • • • Aided by surface hyaluronidase enzymes, a sperm weaves its way past granulosa cells of the corona radiata Binding of the sperm to ZP3 molecules in the zona pellucida causes rise in calcium levels within the sperm, triggering the acrosomal reaction Acrosomal enzymes digest holes through the zona pellucida clearing a path to the oocyte membrane The sperm forms an acrosomal process, which binds to the oocyte’s sperm-binding receptors The sperm and oocyte plasma membranes fuse, allowing sperm contents to enter the oocyte Entry of sperm contents causes a rise in the calcium levels in the oocyte’s cytoplasm, triggering the cortical reaction. The result is hardening of the zona pellucida and clipping off of sperm receptors (slow block to polyspermy) After the sperm penetrates the secondary oocyte, oocyte completes meiosis II forming ovum and second polar body Sperm and ovum nuclei swell, forming pronuclei Pronuclei approach each other and mitotic spindle forms between them Chromosomes of pronuclei intermix. Fertilization is accomplished (Zygote is formed). Then the DNA replicates in preparation for the first cleavage stage. 4 cell stage Morula Blastocyst – Implants roughly 7 days after ovulation Pregnancy • Hormones – Estrogen produced by corpus luteum and placenta • Causes uterine, mammary duct, and breast enlargement – Progesterone produced by corpus luteum and placenta • Prevents menstruation, thickens endometrium and breast development • Maternal recognition of pregnancy produced by blastocyst – – – – – Human- Human Chorionic Gonadotropin Sow- Estrogen Mare- Small Unknown Peptide Cow- Bovine Interferon tau Ewe- Ovine Interferon tau • Organ development in utero – ~8 week cutoff for major malformations Duct Formation • . – Sex-determining region on Y (SRY gene) – Male – Testosterone promotes development – Mullerian inhibiting substance (MIS) regresses mullerian ducts • Can cause freemartin in female twin • . – Female – Absence of testosterone, wolffian ducts regress – Absence of MIS, mullerian ducts develop Abnormalities • Male Pseudohermaphrodite – Genotype: XY – Phenotype: Testes inside body, female external genitalia – Caused by: Androgen Insensitivity Syndrome (AIS) • Female Pseudohermaphrodite – Genotype: XX – Phenotype: Have ovaries, male external genitalia – Caused by: Congenital Adrenal Hyperplasia • Adrenal glands overproduce testosterone Estrous Cycle • • Days in Cycle Stage of Cycle Phase Ovarian Structure Hormone Pattern 17-20 Proestrus Follicular Growing follicles Corpus albicans ↑Estrogen ↓Progesterone 0-1 Estrus Follicular Graffian follicle, Dominant follicle, Mature follicle, or Vesicular follicle Max. Estrogen Min. Progesterone 2-4 Metestrus Luteal Corpus hemorrhagicum ↓Estrogen ↑Progesterone 5-16 Diestrus Luteal Corpus luteum Min. Estrogen Max Progesterone . – Without cyclicity – – – Produced by endometrium when no pregnancy occurs Regress Corpus luteum Controls when the animal will cycle . Seasonally Polyestrous • Goal – Give birth in spring when food is abundant • . – – – – Sheep 5 month gestation Breed in the fall ↓Light ↑Melatonin ↑GnRH Cyclicity – – – – Horse 11 month gestation Breed in the spring ↑Light ↓Melatonin ↑GnRH Cyclicity • . Mammary System Outline • • • • Alveolus Lactation Phases Milk Synthesis and Letdown Milk Components Alveolus • Smallest unit of mammary • Composed of epithelial cells – Produce milk components – Polar in nature • Nucleus located near basal membrane • Golgi apparatus near lumen of alveolus • . • Many alveoli make a lobule, many lobules make a lobe Lactation Phases Phase of lactation Mammogenesis Lactogenesis Galactokinesis Galactopoiesis What is occurring… Preparation of breasts Important hormones Other details… Duct Growth: E2, GH, GC Breast development begins in utero Lobuloalveolar Growth: E2, GH, GC, P4, PRL Synthesis and secretion PRL PRL causes synthesis of of milk components milk components in epithelial cells Milk ejection Oxytocin Oxytocin causes contraction of myoepithelial cells Maintenance of lactation PRL PRL surge with suckling PRL inhibits GnRH rBST (GH) can sustain lactation Milk Synthesis and Letdown Negative Milk Components • • Water . – Least variable milk component – Mainly lactose – Lactose intolerance is when people lack lactase • . – Most variable milk component – Mainly Triglycerides • . – Between carbohydrates and fats for variability – Whey (20%) – Casein (80%) • • • • Precipitates from whey at pH 4.6 by chymosin or rennin Vitamins and Minerals Immunity Growth Factors