Integumentary System Notes (All)

Unit 3
Integumentary and Skeletal Systems
Part 1:
Integumentary System
Integumentary System
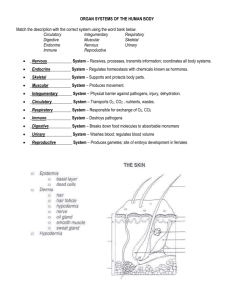
The integumentary system consists of the skin , hair , nails , and glands .
Functions:
1.
protection of internal structures (from abrasion & UV light)
2.
prevention of infectious agent entry
3.
regulation of temperature
4.
production of vitamin D
5.
prevention of water loss
6.
detection of stimuli such as touch, pain, and temperature
Integumentary System
Hypodermis:
also called subcutaneous tissue or superficial fascia
It is not part of the skin, but usually is considered with it because it attaches the skin to underlying muscle, bone, or other connective tissue
loose connective tissue that contains collagen and elastic fibers
contains about half of the body's stored fat
important for padding and insulation
responsible for some of the differences in appearance between men & women & between individuals of the same sex.
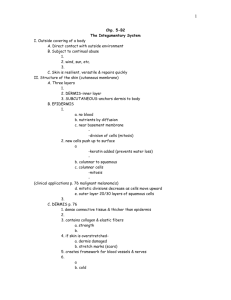
Integumentary System (Skin)
Epidermis
(stratified squamous epithelium)
Skin
Two major tissue layers:
Epidermis
(stratified squamous epithelium)
Dermis
(dense connective tissue)
Dermis
(dense connective tissue)
Integumentary System (Dermis)
Dermis
dense, irregular connective tissue
responsible for most of the structural strength of the skin
Common use of the dermis: leather (tanned animal dermis)
consists of collagen and elastic fibers
contains fibroblasts, fat cells, and macrophages
On the upper part, has dermal papillae (projections which extend toward the epidermis)
Contains many blood vessels that supply the epidermis with nutrients, removes waste products, & aids in regulating body temperature
The dermal papillae in the palms of the hands, soles of the feet, & tips of the fingers are in parallel, curving ridges that shape the overlying epidermis into fingerprints & footprints. (The ridges increase friction
& improve the grip of the hands & feet.
Integumentary System (Dermis)
There are two layers of the dermis:
The reticular layer is the main fibrous layer and consists mostly of collagen. It is the deeper layer and blends into the hypodermis.
The papillary layer is well supplied with capillaries. It is the more superficial layer and derives its name from projections called dermal papillae that extend into the epidermis.
If the skin is overstretched for any reason, the dermis can be damaged, leaving lines that are visible through the epidermis. These lines, called striae or stretch marks .
Integumentary System (Epidermis)
Characteristics of the Epidermis (“ upon + skin
”):
stratified squamous epithelium separated from the dermis by a basement membrane
It is avascular - contains no blood vessels and derives nourishment by diffusion from capillaries of the papillary layer
cells are produced in the deepest layers by mitosis (FYI: your skin is replaced approximately every 40-56 days!)
as new cells are formed, they push older cells to the surface, where they slough (flake) off - did you know that you will lose approximately 8 pounds just in dead skin cells in one year?
during migration from “deep” to “superficial” cells change in shape and chemical composition
thick skin is found on the palms of the hands, souls of the feet, and tips of the digits
Integumentary System (Epidermis)
Keratinization:
process that epidermal cells undergo as they move to the surface
produces cells filled with protein (keratin)
gives the stratum corneum its structural strength
produces an outer layer of epidermal cells that resist abrasion & acts as a permeability barrier
Epidermis divided into regions or strata
(from deep to superficial) :
stratum basale or germinativum (SG)
stratum spinosum (SS)
stratum granulosum (SGR)
stratum lucidum (absent in thin skin)
stratum corneum (SC)
"Before Signing, Get Legal Counsel"
(Mnemonics to learn deep to superficial)
Layers of the Epidermis
Cells Types of the Epidermis
The cell type that makes up the majority of the epidermis is a
KERATINOCYTE
Produces the protein keratin which is waterproof & strong.
MERKEL CELLS: used as sensory receptors for the sense of light touch.
LANGERHANS CELLS: star-shaped cells arising from bone marrow that migrate to epidermis (macrophages) that aid in immune response in the skin
MELANOCYTES produce MELANIN (dark brown pigment)
Layers of the Epidermis
STRATUM BASALE
• The deepest layer of the epidermis where cells rapidly divide to create the upper layers (mitosis) – only at this layer
• Because of the rapid division, this layer is also called the Stratum
Germinativum
• One layer of cuboidal or columnar cells (80-85% keratinocytes, with other 15% made up of melanocytes, Merkel disks, and
Langerhans cells).
STRATUM SPINOSUM
• “spiny layer”
• - 8-10 rows of many sided cells with the appearance of prickly spines
• - melanin granules and Langerhans’ cell predominate
Layers of the Epidermis (continued)
STRATUM GRANULOSUM
• 3-5 rows of flattened cells
• nuclei of cells flatten out
• organelles disintegrate & cells eventually die as they are now too far from the needed nutrients found in the dermis.
STRATUM LUCIDUM
• 3-5 layers of clear, flat cells found only in the thickest skin (soles of feet, palms, & fingertips)
Layers of the Epidermis (continued)
STRATUM CORNEUM
• Layer has many rows of dead cells filled with keratin
• Continuously shed and replaced
• Acts as an effective barrier against light, heat and bacteria
• 20-30 cell layers thick
• Dandruff and flakes
• 40 lbs. of skin flakes in a lifetime (dust mites!)
Epidermal Cells and Layers of the Epidermis
Figure 5.3
Integumentary System (Skin Color)
Skin Color determined by:
pigments in the skin:
Melanin, a brown-to-black pigment, is produced by melanocytes in the stratum basale
Carotene – yellow pigment found in plants; it is lipid soluble, & when consumed, it accumulates in the stratum corneum & the fat cells of the dermis & hypodermis. This gives the skin a slight yellowish tint.
by blood circulating through the skin
by the thickness of the stratum corneum
Integumentary System (Skin Color)
melanin is transferred to other cells by melanocytes
melanin is present in large quantities in moles , freckles , the genitalia , and nipples
melanin production is genetically determined, but can be influenced by hormones and ultraviolet light
albinism a recessive genetic trait that causes a deficiency or absence of melanin
albinos have fair skin, white hair, and unpigmented irises in the eyes
Melanin Transfer from
Melanocyte to Epithelial Cells
Melanocytes make melanin, which is packaged into melanosomes & transferred to many epithelial cells.
Integumentary System (Skin Color)
Redness of the skin can occur from :
the inflammatory response
anger or blushing
exposure to heat
exposure to cold
Skin Conditions :
decreased blood flow causes a pale skin (shock)
decreased oxygen content in the blood results in a bluish color called cyanosis
a yellowish skin color, jaundice , can occur when the liver is damaged by a disease such as viral hepatitis
the disease scarlet fever results from a bacterial infection in the throat
the condition of age spots are caused by increased melanocytes
Integumentary System (Skin Color)
Birthmarks = congenital disorders of capillaries in the dermis
IV. Accessory Skin Structures
A. Hair
1. Characteristic of all mammals a. Thick hair = fur
2. Hair anatomy: a. Hair shaft = portion of hair above skin surface b. Hair root = portion of hair below skin surface c. Hair bulb = base of hair root d. Medulla = center of hair e. Cortex (bark) = surrounds the medulla f.
Cuticle (skin) = single layer of overlapping cells holding hair follicle g. Hair follicle = extension of epidermis deep into dermis i.
Plays role in tissue repair
3.
Hair growth: a.
Cyclic: growth stage + resting stage i.
Hair bulb produces hair; nourished by blood vessels ii.
Epithelial cells undergo keratinization in hair bulb; cells are added to base of hair – hair “growth” iii. Growth stops during resting stage iv.
Next growth stage causes hair to fall out
Hair Type
Eyelash
Growth Stage Resting Stage
30 days 105 days
Scalp 3 years 1-2 years i.
Pattern baldness – permanent loss of hair
4.
Hair color determined by varying amounts & types of melanin a.
Melanin production decreases with age = gray/white
B.
Muscles
1.
Arrector pili (that which raises, hair) = contraction of these muscles cause hair to
“stand on end”… goosebumps
a.
Composed of smooth muscle b.
Evolutionary advantage in mammals – traps air (heat) for insulation, also look larger - intimidation
C. Glands
(Exocrine – secrete onto a suface)
1. Sebaceous glands a.
Simple, branched acinar/alveolar b. Produce sebum
– an oily white substance that lubricates hair & skin surface, preventing drying out & protection against some bacteria
C. Glands, continued…
2.
Sweat glands (two types): a.
Merocrine sweat glands i.
Simple, coiled tubular w/ ducts opening to skin surface ii.
Every part of skin, most abundant in palms/soles iii. Produces sweat: slightly salty water-based secretion
•
Evaporative cooling
• Emotional stress produces sweat in palms, soles, axillae (used in lie detector tests!) b.
Apocrine sweat glands i.
Simple, coiled tubular gland with ducts opening into hair follicles of the axillae & pubic region
•
Become active at puberty due to sex hormone influence ii.
Secretes thick organic substances
•
Broken down by bacteria = body odor
Sensory Receptors of the Skin
Perceive Touch:
Merkel’s Discs
Meissner’s
Corpuscles
Root Hair Plexus
Perceive Pressure:
Pacinian Corpuscle
Krause’s Corpuscle
(also heat)
Ruffini Corpuscle
(also cold)
D. Nails
1. Nail = thin, horny plate at end of fingers and toes, consisting of several layers of dead epithelial cells
(stratum corneum) containing a hard keratin
2. Nail anatomy: a. Nail body = visible part of nail b. Nail root = part of nail covered by skin c.
Eponychium or cuticle (upon + nail) = stratum corneum extending onto nail body d. Nail bed = nail root and nail body attach to this e.
Nail matrix = proximal portion of nail bed w/o nail root attached i.
Produces cells that result in nail growth ii. Nails grow continuously f.
Lunula = whitish, crescent-shape at base of nail
Fingertip & Nail
A.
Burns
1.
Partial-thickness burns – part of stratum basale viable a.
First-degree burns – involves epidermis, red, painful, edema i.
Sunburn, quick exposure to hot/cold ii.
No scarring, heals quickly b.
Second-degree burns – destruction of epidermis and dermis, recovery happens from edge of burn c.
Full-thickness or third-degree burns i.
Painless b/c nervous tissue destroyed ii.
May appear white, tan, brown, black, or deep cherry red iii. Scarring with disfiguration, extended healing time iv. Skin grafts (self, cadavers, pigs, lab-grown?)
First-degree
(epidermis only; redness)
Burns
Second-degree
(epidermis and dermis,with blistering)
Third-degree
(full thickness, destroying epidermis, dermis, often part of hypodermis)
Rule of Nines for Adults
The estimated extend of burns may be calculated using the rule of nines.
Totals:
Anterior & posterior head & neck = 9%
Anterior & posterior upper limbs = 18% (9% per arm)
Anterior & posterior trunk = 36%
Perineum = 1%
Anterior & posterior lower limbs = 36%
TOTAL 100%
Rule of Nines for Adults
Anterior head and neck 4 1 /
2
%
Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
4 1 /
2
% Anterior and posterior head and neck
9%
4 1 /
2
%
Posterior head and neck 4 1 /
2
%
Anterior upper extremities 9%
4 1 /
2
%
Anterior trunk
18%
4 1 /
2
%
Anterior and posterior upper extremities
18%
Anterior and posterior trunk
36%
4 1 /
2
%
Posterior trunk
18%
4 1 /
2
%
Posterior upper extremities 9%
Anterior lower extremities 18%
9% 9%
Perineum 1%
Anterior and posterior lower extremities
36%
33
100%
9% 9%
Posterior lower extremities 18%
Skin Disorders
Warts - nonmalignant epithelial growth caused by a virus
Cold sores (fever blisters)
small fluid-filled blisters around lips & mouth caused by a herpes simplex virus
Acne - inflammation of sebaceous glands
Impetigo - inflamed lesions caused by staphylococcus infection
Decubitus ulcers (bed sores) caused by irritation and inadequate circulation, especially in areas over bony projections such as hip bones, heels, etc. (occur most often in those who are bedridden or confined to a wheelchair.
Metastasize
(Metastasis):
Spreading of cancer
Benign: A noncancerous tumor
Malignant: A cancerous tumor
Carcinoma: Cancer
Carcinogen: Cancercausing agent
Causes for Skin Cancer
1. Overexposure to UV light
2.
Frequent skin infections
3. Chemical exposure
4. Physical trauma
Basal Cell Carcinoma
Most common form of skin cancer
Least deadly
Stratum Germinativum cells are altered and the boundary between the dermis and epidermis is destroyed
Occurs most commonly on sun exposed areas (face)
Basal Cell Carcinoma (continued)
Signs and symptoms
New growth or sore that will not heal
Waxy, smooth, red, pale, flat, or lumpy
May or may not bleed
approx. 30% of caucasians will develop this
99% cure rate
24-38
Squamous Cell Carcinoma
Less common than basal cell carcinoma
Scaly keratinized elevation that arises from Stratum
Spinosum
Found most commonly on scalp, ears, back of hands, and lower lip.
Can metastasize to the lymph nodes
Believed to be sun induced
Good chance of complete cure
Malignant Melanoma
From melanocytes, usually in a pre-existing mole
Appear on trunk, head, neck of men
Appear on arms and legs of women
Itches or bleeds
Metastasizes quickly to lymph and blood vessels.
Treatment
Surgery and biopsy
Removal of lymph nodes
Chemotherapy and radiation therapy
Immunotherapy
Survival is helped by early detection
24-40
Malignant melanoma
Irregular growths with variety of pigmentation
(brown, gray, black, or blue)
Occur in all age groups, usually in people who sunburn easily
More common in people who get short intense exposure to sunlight .
Survival rate is low.
Malignant Melanoma
ABCD’s of Skin Cancer
ABCD Rule
A - Asymmetry
B - Border irregularity
C - Color
D - Diameter
Skin Cancer
Sqaumous cell carcinoma
Basal cell carcinoma Melanoma
Reduce your risk of skin cancer:
Here are some ways to play it safe in the sun:
Avoid the sun between 10 a.m. and 4 p.m.
Seek shade: Look for shade, especially in the middle of the day when the sun’s rays are strongest. Practice the shadow rule and teach it to children. If your shadow is shorter than you, the sun’s rays are at their strongest.
Slip on a shirt: Cover up with protective clothing to guard as much skin as possible when you are out in the sun. Choose comfortable clothes made of tightly woven fabrics that you cannot see through when held up to a light.
Slop on sunscreen: Use sunscreen and lip balm with a sun protection factor (SPF) of
30 or higher. Apply a generous amount of sunscreen (about a palmful) and reapply every 2 hours and after swimming, toweling dry, or sweating. Use sunscreen even on hazy or overcast days.
Slap on a hat: Cover your head with a wide-brimmed hat, shading your face, ears, and neck. If you choose a baseball cap, remember to protect your ears and neck with sunscreen.
Wrap on sunglasses: Wear sunglasses with 99% to 100% UV absorption to provide optimal protection for the eyes and the surrounding skin.
Follow these practices to protect your skin even on cloudy or overcast days. UV rays travel through clouds.
Avoid other sources of UV light. Tanning beds and sun lamps are dangerous. They also damage your skin in other ways.
Go to this web address on your Photon Browser and go through the tutorial and check your skills on identifying skin cancer:
http://sciencenetlinks.com/interactives/skindeep/interactive/base
.html