Integumentary system
advertisement

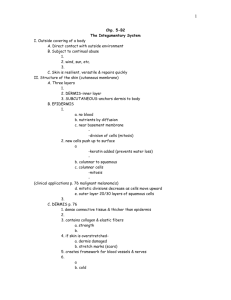
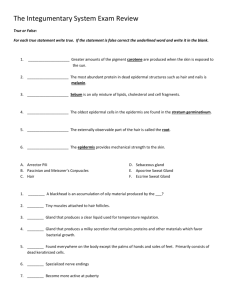
Honors Anatomy & Physiology INTEGUMENTARY SYSTEM ESSENTIAL QUESTION What are the ways skin protects the body? INTEGUMENTARY SYSTEM functions: 1. protecting the body 2. helping to regulate body temperature 3. allows you to sense stimuli in your environment 4. stores blood 5. synthesis of vit. D 6. excretion & absorption of materials STRUCTURE OF THE SKIN skin = cutaneous membrane largest organ of body in adults: covers ~ 2 m² & weighs ~ 4.5 – 5 kg (10 – 11 lb) 2 parts: 1. epidermis 2. dermis 3. sub Q below dermis & not technically part of skin: contains fat (insulation), & blood vessels, nerves that supply the skin LAYERS OF THE EPIDERMIS EPIDERMIS keratinzed stratified squamous epithelium 4 main cell types: 1. keratinocytes 2. melanocytes 3. Langerhans cells 4. Merkel cells KERATINOCYTES ~ 90% of all epidermal cells produce fibrous protein: keratin: protects heat skin & underlying tissue from microbes chemicals also release a water-repellant sealant from lamellar granules decreases water entry/loss inhibits entry of foreign materials KERATINOCYTES MELANOCYTES ~8% of epidermal cells produce melanin keratinocytes pigment (yellow-red to brown-black) that contributes to skin color * absorbs UV radiation “covers” nucleus in keratinocyte LANGERHANS CELLS arise in red bone marrow then migrate to epidermis easily damaged by UV radiation function: immune response vs. microbes that invade MERKEL CELLS least numerous of epidermal cells (>1%) deep in epidermis in contact with Merkel disc (tactile disc) together detect different aspects of touch THIN SKIN covers most of body 4 layers: 1. stratum basale 2. stratum spinosum 3. stratum granulosum 4. stratum corneum THICK SKIN found in areas where exposure to friction is the greatest “thick” because has 1 extra layer: stratum lucidum (between stratgum granulosa & a thicker stratum corneum) PSORIASIS common & chronic skin disorder in which keratinocytes divide & move more quickly than normal from stratum basale stratum corneum make abnl keratin flaky, silvery scales @ skin surface most often over knees, elbows, or scalp DERMIS 2nd, deeper layer of skin composed mostly of CT 2 regions: 1. papillary region 2. reticular region PAPILLARY REGION OF DERMIS ~ 1/5th of total dermis surface area greatly increased by fingerlike structures: dermal papillae that project into epidermis contain: capillary loops tactile receptors: Meissner corpuscles free nerve endings (temp, pain, tickle, itch) EPIDERMAL RIDGES develop during 3rd month of fetal development pattern is genetically determined & unique to individuals (x identical twins) on finger tips ridges deeper finger prints allow you to grasp things by increasing surface area RETICULAR REGION OF DERMIS attached to subcutaneous layer beneath contains: dense irregular CT hair follicles sebaceous glands sudoriferous (sweat) glands collagen & elastic fibers (gives skin its elasticity, strength): extreme stretching striae (stretch marks) BASIS OF SKIN COLOR 3 pigments contribute: 1. Melanin 2. Hemoglobin (hgb) 3. Carotene MELANIN made from a.a. tyrosine using enzyme tyrosinase then stored in organelle called a melanosome exposure to UV light increases enzymatic activity & more (& darker) melanin produced melanin absorbs UV radiation preventing it from damaging DNA which skin cancer HEMOGLOBIN in RBCs rosy color to lighter skinned individuals blushing: due to increased blood flow (autonomic nervous system at work) CAROTENE yellow-orange pigment precursor of vit. A ALBINISM inherited inability to produce melanin most due to cell’s inability to produce tyrosinase VITILIGO partial or complete lack of melanocytes from patches of skin produces irregular white spots ? Immune system malfunction? SKIN COLOR AS DIAGNOSTIC CLUE cyanotic: when blood not adequately oxygenated mucous membranes, nail beds & skin appears bluish SKIN COLOR AS DIAGNOSTIC CLUE jaundice: due to build up of bilirubin (yellow pigment) in skin, sclera; usually indicates liver disease SKIN COLOR AS DIAGNOSTIC CLUE erythema: redness of skin caused by engorgement of capillaries due to: injury, infection, inflammation, allergic reaction SKIN COLOR AS DIAGNOSTIC CLUE pallor: paleness of the skin, seen in shock & anemia ACCESSORY STRUCTURES OF THE SKIN all develop from embryonic epidermis include: Hair Nails Glands HAIR (PILI) present on most skin surfaces x palmar surfaces of hands, soles & plantar surfaces of feet genetic & hormonal influences determine the thickness & pattern of distribution of hair HAIR functions: protection scalp, eyebrows, eyelashes: from getting foreign objects in eyes nose, ear canals: trap foreign objects sensitive to light touch touch receptors in hair root plexus ANATOMY OF A HAIR HAIR composed of columns of dead, keratinized cells bonded together by extracellular proteins ANATOMY OF A HAIR shaft: portion of hair that projects from scalp root: portion below scalp follicle: surrounds root of hair arector pili: smooth muscle extends from side of hair follicle superficial dermis TYPES OF HAIR lanuga: grows on fetus @ ~ 5 months fetal age; sheds b/4 birth vellus hair: short, fine hair that grows over baby @~ 2-3 months after birth terminal hair: coarse hair that develops after puberty HAIR GROWTH CYCLE HAIR COLOR mostly due to amt & type of melanin in keratinzed cells dark hair has eumelanin blondes & redheads have pheomelanin gray: loss of melanin white: loss of melanin + air bubbles in shaft of hair SKIN GLANDS exocrine glands ass’c with the skin: 1. sebaceous glands 2. sudoriferous glands eccrine sweat glands apocrine sweat glands SEBACEOUS GLANDS “oil” glands most connected to hair follicles rest secrete directly onto surface of skin (lips, eyelids, genitals) secrete oily substance called sebum onto hair keeps hair from getting brittle ACNE inflammation of sebaceous glands colonized with bacteria infection cyst which destroys epidermal cells (cystic acne) acne is not caused by eating chocolate or fried foods SUDORIFEROUS GLANDS sweat glands sweat onto skin surface or hair follicles CERUMINOUS GLANDS modified sweat glands in external ear canal skin (subQ layer) secrete cerumen (ear wax provides a sticky barrier that impedes entrance of foreign bodies NAILS plates of tightly packed, hard, dead, keratinized epidermal cells that form a clear, solid covering over the dorsal surfaces of the distal portions of the 20 digits average growth ~ 0.04 in/wk fingernails grow slightly faster than toe nails FUNCTIONS OF A NAIL help us grasp & manipulate small objects protect ends of digits allows scratching PARTS OF EXTERIOR OF A NAIL ANATOMY OF A NAIL PARTS OF A NAIL body: visible part root: part buried matrix: where cells divide to produce growth FUNCTIONS OF THE SKIN (#7) 1. Thermoregulation 1. the homeostatic regulation of body temperature skin achieves this in 2 ways: sweating 2. evaporation of sweat requires nrg (body heat) so body cools down as sweat evaporates adjusting flow of blood in dermis vessels dilate when body too warm vessels constrict when body too cold FUNCTIONS OF THE SKIN 2. Blood Reservoir skin carries ~ 8 – 10% of total blood flow in resting adult FUNCTIONS OF THE SKIN 3. Protection keratin protects underlying tissues from microbes, abrasion, heat, & chemicals lipids released retard evaporation of water from skin surface guarding vs. dehydration & retard water from entering thru skin sebum moistens skin & has antibacterial properties acidic pH of sweat bacteriostatic melanin protects DNA in skin cells from UV damage Langerhans cells alert immune system if microbes does attack / macrophages ingest microbes FUNCTIONS OF THE SKIN 4. Cutaneous Sensations skin contains variety of nerve endings & receptors touch pressure vibration tickle pain temperature FUNCTIONS OF THE SKIN 5. Excretion elimination of wastes from the body only small amt substances excreted from skin ~400 mL water/day ~200 mL sweat (sedentary adult) small amts salts, CO2, NH3, & urea FUNCTIONS OF THE SKIN 6. Absorption passage of materials from external environment body cells absorption of water-soluble materials negligible lipid-soluble materials do absorb: fat-soluble vitamins (A, D, E, K) certain drugs (can be administered transdermally) gases: O2 & CO2 toxins: acetone, CCl4, salts of Hg, Pb, Ar, substances in poison ivy & poison oak FUNCTIONS OF THE SKIN 7. Synthesis of Vitamin D requires activation of a precursor molecule in the skin by UV rays in sunlight modified by enzymes in liver & kidneys producing calcitriol the most active form of vit. D calcitriol: aids in absorption of calcium in GI tract SKIN WOUND HEALING skin damage sets in motion a sequence of events that repairs the skin to as normal as it can in both structure & function depending on depth of wound 1 of 2 processes occur epidemal wound healing deep wound healing EPIDERMAL WOUND HEALING abrasion: portion of skin has been scraped away in response to injury: basal cells of nearby uninjured skin break contact with bm, enlarge, & migrate across the wound migration continues across wound until meet cells advancing from other side of wound contact inhibition: cells stop migrating when touch another cell DEEP WOUND HEALING when injury extends deeper than epidermis repair process more complex & scars form healing occurs in 4 phases: 1. Inflammatory phase 2. Migratory phase 3. Proliferative phase 4. Scar formation INFLAMMATORY PHASE blood clot forms loosely unites edges of wound inflammation develops vascular response vasodilation cellular & increased permeability of vessels response phagocytic fibroblasts WBCs (neutrophils), macrophages MIGRATORY PHASE clot scab epithelial cells migrate beneath scab to bridge wound fibroblasts begin secreting collagen & glycoproteins scar *tissue filling wound called granulation tissue PROLIFERATIVE PHASE extensive growth of epithelial cells beneath scab & deposition of collagen in random patterns (fibroblasts) growth of blood vessels SCAR FORMATION aka maturation phase scab falls off epidermis restored collagen fibers become more organized fibroblasts disappear blood vessels restored to normal scar tissue less elastic, fewer blood vessels, +/- accessory structures of skin SCARS fibrosis: process of scar formation 2 types raised scars 1. hypertrophic scar 2. scar remains w/in boundaries of wound keloid extends boundaries of wound site SCAR FORMATION aka maturation phase scab falls off epidermis restored collagen fibers become more organized fibroblasts disappear blood vessels restored to normal scar tissue less elastic, fewer blood vessels, +/- accessory structures of skin BURNS tissue damage caused by excessive heat, electricity, radioactivity, or corrosive chemicals that denature proteins in skin cells destroy skin’s ability to maintain homeostasis graded by their severity: 1st & 2nd degree = partial thickness burns; 3rd degree = full thickness 1ST DEGREE BURNS only epidermis is damaged example: sunburn symptoms: localized redness, swelling, & pain tx: immediate flushing with cool water (lessens pain) healing: 3 – 6 days +/- peeling of skin results: normal 2ND DEGREE BURN epidermis & upper dermis damaged, some skin function lost, ass’c structures not damaged symptoms: same as 1st degree + blisters (epidermis separates from dermis due to accumulation of tissue fluid) example: any burn with blisters 2ND DEGREE BURNS tx: if 2° infection: antibiotics lasts: 3 – 4 wks with +/- scarring AVOID: WEAR SUNSCREEN! 3RD DEGREE BURNS destroys epidermis, dermis, & subQ no initial edema or pain or sensations (receptors destroyed) most skin functions lost as healing starts marked edema regeneration: months, + scarring tx: +/- skin grafting SYSTEMIC EFFECTS OF A BURN greater threat to life than burn itself include: 1. large loss of water, plasma, plasma proteins 2. 3. 4. 5. shock bacterial infection reduced circulation of blood decreased urine production diminshed immune response MAJOR BURNS used to estimate extent & severity of burns major burn considered a 3° burn that covers > 10% of body or a 2° burn that covers > 25% of surface area of body or any 3° burn on face, hands, feet, or perineum if burn > 70% surface area > ½ patients die RULE OF 9’S SKIN CANCER 3 common forms: 1. Basal cell carcinoma 2. Squamous cell carcinoma 3. Malignant melanoma 1 & 2 50% more common in males BASAL CELL CARCINOMA > 78% all skin cancers arises in cells from stratum basale Sun-exposed areas rarely metastasizes. SQUAMOUS CELL CARCINOMA ~20% of all skin cancers arise from squamous cells in epidermis variable tendency to metastasize MALIGNANT MELANOMA arise from melanocytes ~2% of all skin cancers deadliest form of skin cancer spreads rapidly, can die w/in months of dx ~1/50 Americans will develop in their lifetimes (was 1/500 in 1930’s) increase partly due to hole in ozone layer (more UV rads) main reason: more people spend more time in sun &/or tanning beds MALIGNANT MELANOMA key to successful tx is early detection early warning signs: ABCD A: asymetrical lesion B: borders are irregular C: color is uneven; may have multiple coloration D:diameter: ordinary moles <0.25 in (pencil eraser) DEVELOPMENT OF THE INTEGUMENTARY SYSTEM