CHAPTER 56- THE BIRTH PROCESS INTRODUCTION: LDRP
advertisement

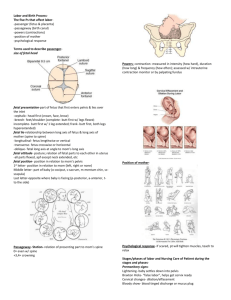
CHAPTER 56- THE BIRTH PROCESS INTRODUCTION: 1. LDRP room- homelike environment 2. Delivery in labor room 3. May have family and friends present ONSET OF LABOR: 1. 2 theories: a. Mechanical- uterus wants to be emptied b. Hormonal- changes in maternal progesterone, estrogen, oxytocin and prostaglandin and increase in fetal production of cortisol SIGNS OF IMPENDING LABOR: 1. Lightening: a. Descent of fetus into pelvis b. In primagravida, can occur up to 2 weeks before the start of labor c. In multigravida, if occurs they are already in labor d. SOB is relieved- uterus and fetus drop and the pressure on the diaphragm is relieved e. Now have: leg cramps, urinary frequency and edema of Les 2. Braxton-Hicks contractions a. Irregular, intermittent b. No softening or thinning of cervix c. Is considered false labor 3. Cervix: a. Matures and ripens at 34 weeks b. Becomes more spongy and softer c. Effacement may begin with thinning and shortening of the cervix 4. Bloody Show: a. Blood tinged mucous plug expelled b. Labor usually begins 24 to 48 hours after bloody show 5. Rupture of membranes (ROM): a. Usually occurs after labor begins b. If engagement (presenting part comes down into pelvis inlet) has not yet occurred, risk for prolapsed cord (cord washes out with fluid) is present. c. If labor doesn’t begin spontaneously within 12 to 24 hours, induction is done to prevent infection. d. To verify amniotic fluid, use nitrazine paper- if + will turn blue after moistened with the discharge 6. GI disturbance: a. Ingestion b. Nausea and vomiting c. Diarrhea d. 1-3 lb. weight loss 7. Sudden burst of energy MATERNAL SYSTEMIC RESPONSES TO LABOR: 1. CV system: a. CO increases – every time uterus contracts 400 ml of blood volume is returned to maternal circulation b. BP increases during each contraction, so take BP between contractions c. BP increases due to anxiety and pain 2. Resp. system: a. During labor O2 consumption doubles b. If fetus gets hypoxic or acidotic, distress c. If mom hyperventilates, CO2 in blood decreases 3. Renal system: a. If bladder distended, impeded fetal descent b. Uterus compresses ureters so urine output decreases c. Encourage voiding as lessened urge to void is present 4. GI system: a. peristalsis and absorption decreases b. gastric emptying time is prolonged c. increase in gastric acidity d. dry mouth and lips e. no solid foods in the event of an emergency such as C/S 5. Fluid and Electrolyte imbalance: a. temp of mom increases b. perspires profusely c. increase in fluid loss d. keep IV fluids running so no dehydration 6. Immune system: a. WBC increase to as much as 25,000 b. WBC stays elevated during early part of post-partum period c. cannot detect true infection process because of this 7. Integumentary system: a. minute tears in vagina and perineum 8. MS system: a. increased muscle activity b. fatigue c. +1 proteinuria d. backache e. leg cramps 9. Neurological system: a. euphoric at beginning of labor then serious then amnesiac b. pain threshold increases due to endorphins c. sedative effect due to endorphins d. pain i. is individualized, subjective, very personal with a wide range of expressions ii. see cultural considerations iii. 1st stage- visceral pain- stimuli in uterus, cervix, pelvic ligament iv. 2nd stage- traction and distention on pelvic structures around vaginaperineum 4 MAJOR VARIABLES AFFECTING LABOR: 1. PASSAGE: A. Bony pelvis: i. Size and shape of pelvis must be big enough for the head to pass thru. ii. Usually size and shape determined by palpation or ultrasound B. Uterus: i. Upper part thickens, lower part thins forming a tube with each contraction C. Cervix: i. Pressure on cervix leads to effacement and dilitation D. Vagina: i. Increased blood flow, connective tissue loosens and leads to stretching of vagina E. Perineum: i. pressure of fetus leads to stretching and thinning of perineum 2. PASSENGER: A. Size: a. b. c. d. Largest part of fetus is head Fetal head molds to mother’s pelvis during labor Bones of fetal skull not fused, so they can move +/or overlap Fontanelles are areas where sutures meet, can be palpated thru the cervix and help determine fetal position B. Fetal attitude: a. Relationship of fetal body parts to one another. b. Ideal attitude at term is flexion with head flexed onto chest, arms flexed (bent) over chest, and hips and knees bent on abdomen. c. If any part of the fetus is extended, labor more difficult C. Fetal lie: a. How baby is laying in the uterus b. Up and down- longitudinal c. Lays across- transverse D. Fetal presentation: a. Determined by how the baby is laying in the uterus and the part of the fetus that enters pelvis first. b. The presenting part of the fetus is the parts of fetus in contact with cervix c. Most common type is the cephalic (head-95%), next is breech (4%), then shoulder (1%). d. Cephalic is further characterized by the part of the head entering the pelvis first: i. Vertex- occiput presenting part ii. Brow- sinciput presenting part iii. Face- face presenting part e. Breech differentiated by attitude of fetus’s legs: i. Complete with buttocks presenting first, hips and knees flexed on abdomen ii. Frank with hips flexed, knees extended, buttock presenting part iii. Footling breech with hips and knees extended as presenting part- single or double footling f. Shoulder presentation: i. occurs in transverse lie ii. presenting part usually shoulder but may be arm, back, abdomen or side. E. Fetal position: a. Relationship of the identified landmark on presenting part of the 4 quadrants of the mother’s pelvis. Fetal position reflects the orientation of the fetal head or butt within the birth canal. b. See pg 1759. 3. POWERS: A. Primary Power: a.involuntary uterine contractions leads to cervical effacement and dilatation during 1st stage of labor. B. Secondary Power: a.voluntary use of abdominal muscles by mother to push during 2nd stage of labor C. Uterine Contractions: a. Uterus contacts and relaxes rhythmically b. When the mother rests between contractions it allows blood flow and oxygenation to the fetus c. Contraction begins in top of uterus (fundus) and spreads over uterus in about 15 seconds d. Leads to effacement and dilatation e. A contraction has 3 phases: i. Increment- increased intensity of a contraction (longest phase) ii. Acme- peak of contraction iii. Decrement- decreased intensity of a contraction f. Characteristics of a contraction: i. frequency- time from beginning of one contraction to beginning of next contraction (one contraction plus resting period)- should be less than 60 seconds ii.duration- length of one contraction from beginning of increment to conclusion of decrement- should not be longer than 90 seconds. iii.intensity- strength of contraction at the ACME g. Contraction affected by position of mother: i. If lie on back, contractions often more frequent but less intense ii. If lie on side, contractions less frequent but more intenseimproves progress in labor and prevents supine hypotensive syndrome. D. Once cervix fully dilated: a. Mother to take deep breath at beginning of contraction, holds her breath and voluntarily pushes in a Valsalva type bearing down through the contraction. b. Urge to push and bear down is spontaneous- called Ferguson’s reflex. 4. PSYCHE: A. Mother’s attitude toward labor and preparation for labor B. Attitude shaped by: a. Expectations b. Experience c. Culture d. Values C. Important for mother to relax. If anxious or fearful as catecholamines are secreted if doesn’t relax. This can suppress uterine contractions and restrict blood flow to the placenta. D. Childbirth preparation classes help mom to work with baby not against E. If expectations realistic, more positive experience. STAGES OF LABOR: 1. Stages 1&2 vary depending on how many children and stages 3 &4 same for all. 1. First stage: A. Dilatation and effacement: a. Begins with onset of regular contractions b. Ends with cervical dilatation is complete (10cm) c. Longest stage d. Divided into 3 phases: latent, active, transition B. Latent: a. Ends when cervix is dilated 4 cm b. Contractions begin 10 to 20 minutes apart and increase in frequency to every 5-7 mins. c. Duration begins at 15 to 20 secs. To 30 to 40 secs. d. Intensity mild at first then moderate e. Alert and talkative f. Glad that labor has started but anxious about what’s next g. A good time to review preparation for labor h. Instruct in breathing techniques i. If membranes haven’t ruptured, may walk around at this time C. Active: a. Begins when cervix 4 cm and ends when 8cm dilated b. Frequency every 3-5 minutes c. Duration 40-60 secs. d. Intensity moderate to strong e. Discomfort noted f. Focuses more on breathing techniques during contraction g. Less talkative D. Transition: a. Dilation begins at 8cm and ends at 10cm b. Frequency every 2-3 minutes c. Duration 60-90 secs d. Little rest between contractions e. Intensity strong f. Remind to focus, relax, breathe with each contraction g. Very aware of progress h. May become restless i. May fear being alone j. Characteristics: restlessness, hyperventilates, bewilderment, anger, difficulty following directions, focuses on self, irritability, statements like “don’t touch me”, nausea, vomiting, very warm feeling, perspirations on upper lip, increased rectal pressure. 2. Second stage: A. Birth of baby, stage of expulsion: a. Begins with complete cervicasl dilation b. Ends with birth of baby c. Frequency: q 2-3 minutes d. Duration: 60-90 secs. e. Intensity- strong f. Can now push and bear down- may make her feel she is in control g. As head descends, increased desire to push h. Perineum bulges, then flattens, labia separates, baby’s head is seen but recedes between contractions i. Once head is seen between contractions, crowning has occurred and birth is imminent j. Episiotomy maybe done at this time B. Mechanisms of Labor: a. A series of movements and position changes that occur as the fetus moves through the birth canal b. Also called cardinal movements c. Engagement: i. Occurs when presenting part of fetus fully enters the true pelvis ii. Happens before labor has begun in first time mother and after labor has begun in multigravida d. Descent: i. Begins with engagement and continues with each contraction throughout labor process e. Flexion: i. Fetal head bent forward causing chin to rest on sternum ii. Allows narrowest part of the head to enter pelvic outlet f. Internal rotation: i. Head rotates so occiput is next to the symphysis pubis g. Extension: i. Occiput pivots under symphysis pubis and fetal head becomes extended and pushes outward out of vagina ii. Head born at this time h. Restitution and external rotation: i. Once head out it rotates back to be in normal alignment with shoulders- called restitution ii. Shoulders now rotate to be in anteroposterior position under the symphysis pubis i. Expulsion: i. Baby’s body slides out after gentle downward pressure on baby’s head to allow the anterior shoulder to emerge and the baby’s head is gently raised so the posterior shoulder can be delivered. 3. Third stage: A. Delivery of placenta a. Begins with birth of baby and ends with delivery of placenta b. Should take between 5-30 minutes. c. Signs that placenta has separated: i. Globular shape of uterus ii. Gush of blood from the vagina iii. More of cord protrudes from vagina (is visible) d. Once these signs appear, is asked to push one more time to expel the placenta e. Placenta is disposed of according to facility policy but may be requested by family for cultural reasons. 4. Fourth stage: A. Recovery: a. 1st 4 hours after birth of baby b. Blood loss between 250-500 ml c. Moderate decrease in systolic and diastolic Bp and increase in P rate. d. Uterus should be contracted and in midline of abdomen about the level of the U. e. Mother may be hungry and thirsty f. Shaking chill may be experienced- this is normal g. May have urinary retention- can stop uterus from contracting ADMISSION OF CLIENT IN LABOR: 1. different for each person 2. goals: a. establish nurse-patient relationship b. assess condition of mother and fetus c. determine what stage of labor mother is in: i. when did it begin? ii. how frequent and how long are the contractions? iii.rupture of membranes? iv.# of pregnancies, if not 1st, how did the others go? 3. nurse to make: a. them feel welcome, b. determine expectations about birth c. and identify cultural values/preferences 4. initial assessment: a. physical exam b. listen to FHR c. station: i. relationship of fetal presenting part to the ischial spine ii. measured in cms iii.Measured below (-) or above (+) ischial spine d.contractions: i. assess by placing fingers of one hand on fundus of uterus ii. use light pressure to keep fingers still- should feel contraction iii.contraction begins in fundus and spreads down uterus iv.assess 3 contractions in a row I. Time each begins and ends II. Time lapse between contractions III. Intensity a. Mild contraction- uterus is easily indented with the fingertips-feels like tip of nose b. Moderate contraction- uterus is more difficult to indent with fingertips, feels like the chin c. Strong contraction- uterus unable to be indented with the fingertips, feels like the forehead 5. Nursing process assessment: a. Comfort of mother b. Her ability to cope c. Her desire to urinate or defecate d. Vital signs e. FHR f. Frequency, duration, interval and intensity of contractions g. Fetopelvic relationships- fetal lie, attitude, presentation, station h. Condition of membranes i. Maternal behavior: tone of voice, facial expressions j. Maternal verbalization 6. Nursing interventions: a. Continuous assessment of labor progress and fetal well-being i.any changes outside of normal, report STAT b. provide maternal physical care: i. comfort measures- fluids, ice chips, oral care, frequent position changes, relaxation (including effleurage) measures, cold washclothes to head and neck, provide encouragement and praise, keep mother informed of progress, encourage urination every 2 hours, back rub, apply pressure to sacral area, walking, shower, Jacuzzi, analgesics. c.keep bed linen clean and dry, change linen savers often d. ambulation: i. helps to increase uterine activity, distract from discomfort, provide maternal control ii.can walk only if membranes are intact, presenting part engaged after ROM or has not had any pain medication e.position: i. side-lying position best – promotes blood flow and O2 to placenta and fetus ii.if wants to lie on back need to elevate one hip with a pillow iii.squatting or hands and knees positions help to change and occiput fetal posterior position to an anterior position f.food and fluid intake: i. clear liquids ii.ice chips iii.IV fluids started iv.keep accurate I&O g.elimination: i.encourage to void q 2 hrs. ii.distended bladder stops the descent of the fetus, causes undue discomfort and leads to bladder atony (no tone) post birth iii.if allowed , take to BR; if bedbound use bedpan iv.if cannot void and bladder is distended, may need to catherize; v. if can’t insert catheter, presenting part is probably compressing urethra- notify DR. vi.keep rectal area clean h.assist client and support person i.identify support person ii. breathing techniques I.goals: A. provide adequate O2 to mother and baby B. provide a focus of attention C. decrease pain and anxiety D. increase mental and physical relaxation II. breathing techniques: A.3 types: a. slow deep chest breathing is used until it is no longer effective. Take cleansing breath, then inhale through nose and exhale through pursed lips (6 to 9 br/min.) then take another cleansing breath. b.shallow breathing- take cleansing breath, then inhale and exhale through mouth about 4 times every 5 secs. May be increased to 2 breaths/sec. at peak of contraction c.Pant-blow breathing- use when contractions become very intense. Similar to shallow breathing except every 3 to 4 breaths a forceful exhalation (blow) made through pursed lips. Cleansing blow at beginning and end of contraction. iii.keep pt. informed of their progress in labor and provide positive feedback iv.if siblings will be present for labor and birth be sure a single person (not nurse or s/o) is responsible for taking care of child(ren). 7. Providing pharmacological comfort measures: a. Systemic medications i. Only used if 1. client willing to receive them 2. vs stable 3. fetus at term 4. fetus has normal movement 5. no late or variable decelerations 6. no meconium in amniotic fluid 7. at least 3-5cm cervical dilation 8. presenting part is engaged 9. no complications 10. effects on fetus depends on doses given, timing, rate and pharmokinetics of med 11. IV route preferred (faster and more reliable) b. Regional blocks i. Types: 1. Epidural a. Used for pain control b. May be continuous or intermittent c. Local anesthetic drug is used through a catheter placed in the epidural space d. Fentanyl or sufentanil added to provide faster and longer-lasting relief e. Advantages: good pain control, client can participate in the birth process f. Disadvantages: maternal hypotension, bladder distention, epidural catheter migration, nausea and vomiting, pruritis, delayed respiratory depression. 2. Intrathecal: a. Small dose of fentanyl, sufentanil or morphine is injected into the subarachnoid space b. Advantages: rapid onsetr, no sedation, no hypotensive effect, no motor block so patient can walk during labor c. Disadvantages: d. Large amount needed 3. Local infiltration: a. Local anesthetic is injected into the operineum (Novocaine, Xylocaine) b. Used for episiotomy, suturing, or laceration or when pudental block cannot be used c. Advantages: procedure technically uncomplicated, free of complications d. Disadvantages: large amount needed 4. Pudental: a. Injection of anesthesia into the pudental nerve b. Provides perineal, external genitalia and lower vaginal anesthesia c. General anesthesia 8. May be hospitalized or sent home