Hemodynamics(1)
advertisement

Hemodynamics
updated 4/25/2012
Hemodynamics is the study of the forces
that influence the circulation of blood.
Meaning literally "blood movement" is the
study of blood flow or the circulation.
How bad is your day?
Is everything working the way it is supposed to?
Goal:
The goal of hemodynamic monitoring is to maintain adequate
tissue perfusion. Classical hemodynamic monitoring is based on
the invasive measurement of systemic, pulmonary arterial and
venous pressures, and of cardiac output.
- Monitors do not always “tell the truth.”
-Therapeutic decision-making based on numbers alone is
never appropriate and can be dangerous, even deadly.
Trace a drop of blood through the heart
Ventricular Preload
Ventricular preload refers to the degree that the myocardial
fiber is stretched prior to contraction (end-diastole).
Within limits, the more the myocardial fiber is stretched during
diastole (preload), the more strongly it will contract during
systole, and therefore the greater the myocardial contractility
will be.
Ventricular Afterload
Ventricular afterload is defined as the force against which the ventricles
must work to pump blood.
Determined by:
1) The volume and viscosity of the blood ejected
2) The peripheral vascular resistance
3) The total cross-sectional area of the vascular space into which blood is
ejected.
Arterial systolic blood pressure best reflects the ventricular afterload.
Blood Volume
Although total blood volume varies with age, body size and sex,
the normal adult volume is 5 Liters.
75% is in the systemic circulation
15% in the heart
10% in the pulmonary circulation
Overall, about 60% of the total blood volume is in the veins and
about 10% in the arteries.
The capillary bed normally contains about 75ml of blood but has
the capacity to hold 200ml.
Hypovolemia due to bleeding out, shock (shunt), dehydration
Hypervolemia due to fluid overload (IV therapy, renal disease, CHF)
Stoke Volume
Stroke Volume is the volume of blood ejected by the ventricles
(particularly the left ventricle) during each contraction or systole.
The preload, afterload, and myocardial contractility are the major
determinates of stroke volume. {normal SV is 60-130 ml/beat}
Note: The heart does not eject all the blood it contains during systole.
ESV = a small volume that remains in the heart called the end-systolic
volume, remains behind in the ventricles
EDV = during the resting phase, or diastole, the ventricles fill back up to a
volume called the end-diastolic volume
EDV-ESV = Stroke Volume
Normal stoke volume of 70ml, we can compute an ejection fraction (EF)
SV / EDV = EF
or 70 / 110 = 0.64 or 64%
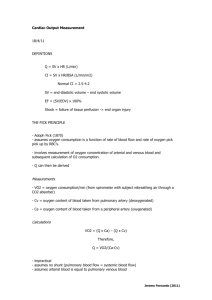
Cardiac Output
Stoke Volume is determined by:
1) Ventricular preload
2) Ventricular afterload
3) Myocardial contractility
Cardiac Output directly influences blood pressure
CO is measured via a special PA catheter using the thermodilution method
CO is the volume of blood pumped in 1 minute
SV x HR = CO {normal CO is 4-8 L/min}
If SV is 70ml and HR is 72 bpm, the CO is 5,040 ml/min
If HR is 100 bpm and CO is 8L (8000ml):
800ml ÷ 100bpm = 80ml SV
BSA is needed to calculate
both the Stroke Volume Index (SVI)
and the Cardiac Index (CI)
BSA can be calculated by the following formula,
or by the Dubois Body Surface Chart as shown:
BSA =
1+ weight in Kg + (height in cm – 160) ÷ 100
Stoke Volume Index and Cardiac Index
Stroke Volume Index (SVI)
Assuming the heart rate remains the same, as the stroke volume index increases or decreases, the
cardiac index also increases or decreases.
The stroke volume index reflects:
contractility of the heart
overall blood volume status
amount of venous return
Example:
SV / BSA = SVI
60 ml/beat ÷ 2 m2 = SVI of 30 ml/beat/m2
Cardiac Index (CI)
If CO is being determined, the CI should also be calculated for additional information on heart
function. Calculated as CO / BSA = CI
Example: 5 L/min ÷ 2 m2 = 2.5 L/min/m2
Normal, resting Cardiac Index is 2.5–4 L/min/m2 of BSA
Play YouTube Video
Hemodynamic Video Lecture:
Graphic Display (duration = 4 minutes) :
http://www.youtube.com/watch?v=G9C-4i3RNs8&feature=related
Pulmonary Vascular Resistance (PVR)
The PVR measurement reflects the afterload of the right ventricle.
(PA – PCWP) / CO x 80 = PVR
(normal PVR = 80-240 dynes/sec/cm-5, or 1-3 mmHg/L/min)
Increased PVR – Chemical:
Decrease alveolar oxygenation (alveolar hypoxia)
Decreased pH (acidemia)
Increased PCO2 (hypercapnia)
Increased PVR – Pharmacologic Agents:
Epinephrine (Adrenalin®)
Norepinephrine (Levophed®, Levarterenol®)
Dobutamine (Dobutrex®)
Dopamine (Intropin®)
Phynelephrine (Neo-Synephrine®)
PVR cont.
Increased PVR – Hyperinflation of Lungs:
Mechanical ventilation
CPAP, PEEP, ↑Vt
Increased PVR – Pathology:
Vessel blockage or obstruction
Caused by a thrombus or an embolus
(blood clot, fat cell, air bubble, or tumor mass)
Vessel wall disease
Sclerosis, Endarteritis, Polyarteritis, Scleroderma
Vessel destruction or obliteration
Emphysema or Pulmonary interstitial fibrosis
Vessel compression
Pneumothorax, Hemothorax, or Tumor mass
PVR cont.
Decreased PVR – Pharmacologic Agent:
Oxygen
Isoproterenol (Isuprel®)
Aminophylline
Calcium-blocking agent
Decreased PVR – Humoral Substances:
Acetylcholine
Bradykinin
Prostaglandin E
Prostacyclin (prostaglandin I2)
Systemic Vascular Resistance (SVR)
(aka Peripheral Vascular Resistance)
The SVR measurement reflects the afterload of the left ventricle.
Circulatory Resistance is derived by dividing the mean blood pressure by the
cardiac output: BP ÷ CO = Resistance
(normal SVR = 900-1,400 dynes/sec/cm-5, or 15-20mm Hg/L/min)
Generally, if vascular resistance increases, BP increases.
Blood pressure can be used to reflect pulmonary or systemic resistance.
Increased SVR – Vasoconstricting Agents:
Epinephrine (Adrenalin®)
Norepinephrine (Levophed®, Levarterenol®)
Dopamine (Intropin®)
Phynelephrine (Neo-Synephrine®)
Increased SVR – Abnormal Conditions:
Hypovolemia
Septic shock (late stages)
↓PCO2
SVR cont.
Decreased SVR – Vasodilating Agents:
Nitroglycerin
Nitroprusside (Nipride®)
Morphine
Amrinone (Inocor®)
Hydralazine (Apresoline®)
Methyldopa (Aldomet®)
Diazoxide (Hyperstat®)
Decreased SVR – Abnormal Conditions:
Septic shock (early stages)
↑PCO2
Nitric Oxide Therapy (NO)
Because it relaxes capillary smooth muscle,
inhalation of NO improves blood flow to
ventilated alveoli.
This reduces intrapulmonary shunting,
improves arterial oxygenation, and lowers
pulmonary vascular resistance and
pulmonary artery pressures.
Knowledge of the effect of NO therapy on
patient outcomes awaits further study.
{AARC Clinical Practice Guidelines}
NO in the Cath-Lab
Although NO is used often in the Cath-Lab; research on its effect is limited.
"Cardiac catheterization in congenital heart disease patients is frequently more time consuming
because of small vessel size, the multiple measurements that must be made, the instability of the
patients (particularly neonates and infants), the frequency of multiple sites of arterial-venous
admixture, and performance of other required interventions (e.g., Rashkind procedure). For example,
evaluation of pulmonary artery hypertension may require administration of oxygen, nitric oxide, or
other agents and repeated measurement of pulmonary blood flow pressures and cardiac output."
http://www.aapc.com/memberarea/forums/archive/index.php?t-1214.html
Monitoring Devices
Non-Invasive:
SpO2
BP cuff
TEE (Transesophageal Echocardiography)
Invasive:
ABG
Radial Arterial Line Catheter
CVP
SvO2
Swan-Ganz
SpO2 Monitoring
SpO2 Quiz
Blood Pressure Monitoring
Blood Pressure
Systemic arterial BP is the force exerted against the walls of the arteries when blood is
pumped through them.
In other words:
Blood pressure (BP) is a function of the Cardiac Output (CO) times the Systemic
Vascular Resistance (SVR)
CO x SVR = BP
Normal CO = 4-8 L/min
Normal SVR = 15-20 mmHg/L/min
Normal BP with proper size cuff and use of a sphygmomanometer = 120/80 mmHg
{Systolic normal range = 100-140mmHg; Diastolic normal range = 60-90mmHg}
Infants and children <10 years of age
Systolic 60-100 mmHg
Diastolic 20-70 mmHg
Mean BP
Calculate the Mean BP
Systolic – Diastolic = Pulse Pressure (PP)
PP x 1/3 = _____ + diastolic = Mean
{Mean arterial pressure = 70-105mmHg}
If BP is 130/90, then:
130 – 90 = 40 (PP)
40 x .33 = 13.2
13.2 + 90 = 103
If BP is 90/40, then:
90 – 40 = 50
50 x .33 = 16.5
16.5 + 40 = 57
Why calculate the Mean Blood Pressure?
Most physician’s drug orders are given to nursing based on it.
“if mean is less than (#), then give x_dose”
All else being constant, the mean arterial pressure is directly
related to the volume of blood in the vascular system, and
inversely related to its capacity
Volume ÷ Capacity = MAP (Mean Arterial Pressure)
Transesophageal Echocardiography (TEE)
An echocardiogram (echo) uses high-frequency sound waves to
produce a graphic outline of the heart’s movement.
A Transesophageal echo (TEE) test is a type of echo test in which
the ultrasound transducer, positioned on an endoscope, is
guided down the patient’s throat into the esophagus (the "food
pipe" leading from the mouth into the stomach). An endoscope
is a long, thin, flexible instrument that is about ½ inch in
diameter.
The TEE test provides a close look at the heart’s valves and
chambers, without interference from the ribs or lungs. TEE is
often used when the results from standard echo tests are not
sufficient, or when your doctor wants a closer look at your
heart.
TEE may be combined with Doppler ultrasound and color
Doppler to evaluate blood flow across the heart’s valves.
Transesophageal Echocardiography
Arterial Blood Gas (ABG)
Radial Arterial Line Catheter
aka: A-line, Art-line, RAL
Insertion recommended for the following situations;
1. The patient needs continuous monitoring of blood pressure
[a hypotensive pt is receiving medication such as Levophed, vasopressin,
dopamine]
2. Frequent arterial blood samples needed for blood gas analysis
Note: a newborn will have the line placed into the umbilical artery
Radial Arterial Line Catheter
Play YouTube Video
Setting Up a Pressure Transducer :
A-line catheter setup (duration = 5 minutes) :
http://www.youtube.com/watch?v=58TQjvHd_sQ&feature=related
(all the parts for setup + flushing the line)
A-line & CVP setup (duration = 10 minutes) :
http://www.youtube.com/watch?v=uv6t1raryjM&feature=related
(demonstrates “burping the bag”)
Video – placing the Art-line (duration = 2 minutes) :
http://www.youtube.com/watch?v=Vt7ONGDeP3w&feature=relmfu
(placing the catheter & drawing blood)
RAL continued
Central Venous Pressure (CVP)
via a Central Line Catheter
The tip of the central-line catheter resides in the superior vena cava just
above the right atrium
This CVP is a measurement of the pressure in the Right Atrium
Two factors that influence the Right Atrial pressure:
1) Blood volume returning to it
2) Function of the Right Ventricle
CVP line inserted to:
1. Monitor the patient’s right-sided (right atrium) heart pressure
2. To rapidly administer a large volume of IV fluids
3. To administer cardiac medications during a CPR attempt
CVP cont.
↓ CVP usually indicates that the patient is hypovolemic
↑ CVP may suggest:
1. Fluid overload
check for elevated BP, crackles in bases of lungs
2. Tricuspid valve or pulmonic valve insufficiency or stenosis
3. Right ventricular failure
if a COPD pt with pulmonary HTN has RV failure, the condition is:
cor pulmonale
4. Cardiac tamponade
5. Atrial or Ventricular septal defect with left-to-right intracardiac shunt
6. Pulmonary embolism
CVP
SvO2
Mixed venous oxygen saturation (SvO2) is measured from a mixed venous blood
sample. Small changes in PvO2 (pressure of mixed venous oxygen) lead to large changes in
SvO2, and therefore large changes in CvO2.
As a result, the SvO2 measurement is a sensitive index of cardiac output (CO) and
tissue perfusion if VO2 is stable.
Continuous SvO2 monitoring has been suggested as an alternative to intermittent,
serial CO measurements. Based on the Fick equation (see separate slide), if total body
oxygen consumption, hemoglobin, and SaO2 remain constant, a change in CO
should be reflected by a parallel change in SvO2.
Low PvO2, SvO2 and ScvO2 (CVP measurement with fiber-optic technology) values are often
seen in patients with heart failure because the slow flow of blood through the
tissues results in more oxygen being extracted.
SvO2 Monitoring
SvO2 may be continuously monitored
through a fiber-optic reflectance oximetry
system incorporated in a five-lumen
pulmonary artery catheter.
=
CCO/SvO2 catheter
A new pulmonary artery balloon flow-directed
catheter combines a fiber optic photometric
system for continuous display of mixed venous
blood oxygen saturation (SO2) with the capacity for
hemodynamic measurements including
thermodilution cardiac output estimation.
SvO2 Monitoring
Photometric detection system having multiple
path length flow
The thermodilution technique has become the de facto clinical
standard for measuring cardiac output because of its ease of
implementation and the long clinical experience using it in various
settings. It is a variant of the indicator dilution method, in which a
known amount of a substance is injected into the blood stream and
its concentration change measured over time at a downstream site.
As its name implies, the thermodilution method uses a thermal
indicator, whereas other indicator dilution methods use various
substances, such as indocyanine green dye.
http://web.squ.edu.om/med-Lib/MED_CD/E_CDs/anesthesia/site/content/v03/030286r00.HTM
http://www.patsnap.com/patents/view/US7236248.html
Fick Equation
VO2 max
… (aka: maximal oxygen consumption, maximal oxygen uptake, peak oxygen uptake or
aerobic capacity) …
is the maximum capacity of an individual's body to transport and use oxygen
during incremental exercise, which reflects the physical fitness of the individual.
The name is derived from V = volume per time, O2 = oxygen, max = maximum.
Q x (CaO2 – CvO2) = VO2 max
Q is the cardiac output of the heart
CaO2 is the arterial oxygen content
CvO2 is the venous oxygen content
Swan-Ganz Catheter
Used to measure hemodynamic and central pressure variables
such as pulmonary capillary wedge pressure
Measure several hemodynamic parameters directly
The development of the pulmonary artery catheter by Swan and
Ganz in the late 1960s began a new era in assessment of left
ventricular and pulmonary performance.
Unlike the CVP that is placed in the right jugular vein, the Swan
Ganz is usually placed into the subclavian.
Swan-Ganz Catheter
•
•
•
•
•
•
•
The Swan-Ganz catheter is a balloon-tipped catheter made of
polyvinyl chloride that is used to measure CVP, PAP and PCWP.
The catheter also allows for the aspiration of blood from the
pulmonary artery for mixed venous blood gas sampling and
injection of fluids to determine cardiac output.
The distal channel (lumen) is used for the measurement of PAP
and for obtaining mixed venous blood from the pulmonary artery.
The proximal channel (lumen) is used for the measurement of
CVP or right atrial pressure and for the injection of fluids to
determine cardiac output.
The balloon inflation channel controls the inflation and deflation
of a small balloon, located about 1cm from the distal tip of the
catheter, and is used to measure PCWP.
The fourth channel is an extra port for the continuous infusion of
fluid, when necessary.
This catheter is also equipped with a computer connector to
measure cardiac output with the use of the thermodilution
technique.
Values
HEMODYNAMIC VALUE
ABBREVIATION
Directly Measured from the Swan-Ganz:
Central Venous Pressure
Right Atrial Pressure
Right Ventricle
Mean Pulmonary Artery Pressure
Pulmonary Capillary Wedge Pressure
(aka: Pulmonary Artery Wedge)
(aka: Pulmonary Artery Occlusion)
Cardiac Output
CVP
RAP
RVP
PA
<8 mmHg [<6 depending on textbook]
2–8 mmHg [2-6 depending on textbook]
0–5 mmHg [systolic = 20-30mmHg]
9–20 mmHg [systolic = 20-30mmHg
diastolic = 6-15mmHg]
PCWP
CO
Calculated from the direct measurements listed above:
Stroke Volume
SV
Stroke Volume Index
SVI
Cardiac Index
CI
Right Ventricular Stroke Work Index
RVSWI
Left Ventricular Stroke Work Index
LVSWI
Pulmonary Vascular Resistance
PVR
Systemic Vascular Resistance
NORMAL RANGE
SVR
4–12 mmHg
4–8 L/min
60–130 ml
30–50 ml/beat/m2
2.5–4.2 L/min/m2
7–12 g m/m2
40–60 g m/m2
20–120 dynes/sec/cm¯5
or, 1.5–3.0 mmHg/L/min
800–1500 dynes/sec/cm¯5
or, 15–20 mmHg/L/min
Play YouTube Video
Pulmonary Artery Catheterization :
Catheter placement (duration 50 sec) :
http://www.youtube.com/watch?v=sygNe0McMK4&feature=related
Swan-Ganz Monitoring
The pacer leads are connected directly to the
pacemaker. If cardiac pacing is not required, the lumen
can be used for infusions and blood sampling.
Play YouTube Video
Swan Ganz Catheter Placement :
Physician’s Lecture (duration = 9 minutes) :
http://www.youtube.com/watch?v=PjRRPhMj0os&feature=related
(monitoring pressures)
Physician’s Lecture (duration = 6 minutes) :
http://www.youtube.com/watch?v=OYabV1H6p78
(heart model demonstration)
Put It All Together
A burn victim is being monitored in the ICU.
Pertinent data are below:
PvO2
PCWP
Mean PAP
CVP
Urine Output
45 torr
4 mm Hg
11 mm Hg
4 cm H2O
5 mL/hr
As the respiratory therapist, you should recommend:
A.
B.
C.
D.
An increase in intravascular volume
The initiation of diuretic therapy
Assist/Control ventilation
An increase in FIO2
A burn victim is being monitored in the ICU.
Pertinent data are below:
PvO2
PCWP
Mean PAP
CVP
Urine Output
45 torr
4 mm Hg
11 mm Hg
4 cm H2O
5 mL/hr
As the respiratory therapist, you should recommend:
A. An increase in intravascular volume
Are you Hemodynamically stable today?
Or is everything out of the norm?
Open Book Test
May use:
> EGAN’s Fundamentals of Respiratory Care
> Clinical Assessment in Respiratory Care
> Basic Clinical Lab Competencies – Gary White
> Comprehensive Exam Review – J.R. Sills