Learning Guide- Hemodynamic Monitoring
advertisement

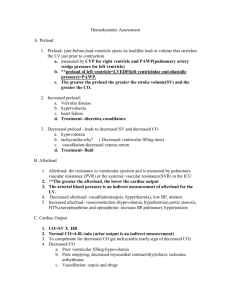
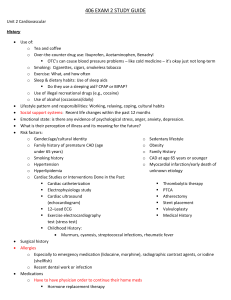
Learning Guide- Hemodynamic Monitoring F12 Complete the following statements: (Notes & Lewis text) and online for A&P review #1 A&P review #2 1. The (cardiac) conduction system is specialized nerve tissue responsible for creating and transporting the electrical impulse or ______ ________. 2. During systole, the _______ and ______ valves are open and the ________ and ________ valves are closed. 3. During diastole, the _______ and ________ valves are open and the _______ and __________ are closed. 4. Atrial contraction is referred to as atrial _____ and is responsible for as much as 30% contribution to CO. 5. The left ventricle never ejects the entire volume it receives during systole. The portion of blood the left ventricle ejects during systole is referred to as the _______ ______. What amount is normal-_____%? 6. Preload is the volume of blood that is in the ventricle just before ejection occurs and is called the ________ _____ _______ _______ pressure and when measured is known as _______ 7. What is the formula for calculating the MAP? At what point is perfusion to vital organs compromised? 8. Define SVR and factors that would increase SVR and factors that would decrease SVR. 9. Define preload. What conditions/factors affect preload? Notes, etc. 10. Define afterload. What conditions/factors affect preload? Notes, 11. Describe CO and factors that effect CO. Explain Stoke Volume as related to CO Explain Heart Rate as related to CO 12. Define “contractility” and factors that influence cardiac contractility. 13. PAWP measures: What influences PAWP? RNSG 2432 475 14. Describe the PA catheter as it advances through the heart and explain the measurements/values that are obtained as the catheter is advanced. (Identify normal values for each and nursing implications of altered values.) 15. What values are obtained from CVP monitoring? What are “normal” values? 16. What does the PA catheter measure? What are normal Pulmonary Artery Pressures (PAP) Hemodynamic Monitoring Study Questions (quick review---use to help answer question above) 1. What does CVP measure and what is a normal CVP? What would this mean in the care of my clients? ~ CVP is a measure of blood volume and venous return. It reflects RIGHTSIDED filling pressures. It is primarily used to monitor fluid volume status. ~ Normal range for CVP is 2-8 cm H20 or 2-6 mmHg ~ Hypovolemia and shock DECREASE the CVP. Fluid overload, vasoconstriction, and cardiac tamponade INCREASE CVP. ~ If CVP is decreased, client needs fluid to increase preload. If CVP is increased, client needs diuresis, vasodilation to decrease afterload, or treatment for cardiac tamponade! 2. What is a PA catheter; what does a PA catheter measure, and where is it placed? ~ A PA catheter is a flow-directed, balloon-tipped catheter, a.k.a. the Swan-Ganz. PA = pulmonary artery. ~ A PA catheter measures pressures in the right atrium, pulmonary artery, and left ventricle. It is used to evaluate left ventricular and overall cardiac function. ~ It is inserted into a central vein and threaded into the right atrium. A small balloon allows the catheter to be drawn into the right ventricle and from there into the pulmonary artery. Once in place, the balloon is deflated and the multiple lumens of the catheter allow measurement of pressures in the right atrium, pulmonary artery, and left ventricle. 3. What is a normal PA pressure and under what conditions would a PA pressure be increased? What does it mean in the care of my clients? ~ Normal PA is around 25/10 mmHg. Normal mean pulmonary artery pressure is about 15 mmHg. ~ Pulmonary artery pressure is increased in left-sided heart failure. Manifestations of left-sided heart failure result from pulmonary congestion and decreased cardiac output. PA pressure measurement allows restoration of fluid balance while avoiding overcorrection of the problem. Nursing interventions for heart failure would be appropriate. RNSG 2432 476 4. What is PAWP (PCWP or PWP); what does it measure and what does this value mean? How does it relate to the Left Ventricular End Diastolic Pressure (LVEDP)? ~ PAWP is pulmonary artery wedge pressure. It measures pressures generated by the left ventricle. It is used to assess left ventricular function. Normal PAWP is 6-12 mmHg. PAWP is increased in left ventricular failure and pericardial tamponade. It is decreased in hypovolemia. ~ PAWP reflects LVEDP under normal conditions, that is, when LVEDP (ventricular preload) is increased, PAWP is increased also. 5. How is PAWP obtained? The measurement of PAWP is obtained by slowly inflating the balloon with 1.5 mL of air while observing the distal lumen pressure tracing. As the line becomes “wedged,” the tracing changes shape and amplitude. When the tracing changes from arterial to atrial, the catheter is said to be wedged and PAWP is measured at the end of expiration. 6. What is cardiac output/cardiac index and what do these values mean? What is normal cardiac output/cardiac index? ~ Cardiac output/cardiac index are used to assess the heart’s ability to meet the body’s oxygen demands. Because body size affects overall cardiac output, the cardiac index is a more precise measurement of heart function. ~ The cardiac index is a calculation of cardiac output per square meter of body surface area. The normal cardiac index is 2.2-4.0 L/min/m2. CO = SV x HR. Normal resting CO is 4-8 L/min and varies with body size. 7. What is SVR; How is it determined? What is MAP? ~ SVR is systemic vascular resistance. SVR is primarily determined by vessel diameter and distensibility (compliance.) Factors such as SNS input, circulating hormones (epinephrine, norepinephrine, atrial natriuretic hormone, and vasopressin) and the renin-angiotensin system affect SVR. ~ SVR is calculated by: SVR = (MAP – CVP) x 80/cardiac output * MAP is mean arterial pressure is the amount of arterial that is necessary to maintain adequate perfusion of vital organs…usually 60 mmHg and is calculated by Systolic BP + 2 (Diastolic BP) divided by 3 RNSG 2432 477