Heart Blocks and Pacemakers - Calgary Emergency Medicine
advertisement

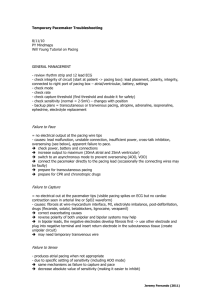
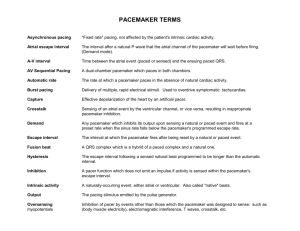
Heart Blocks and Pacemakers Juliette Sacks January 25, 2007 Core Rounds Objectives ► Review heart blocks, their clinical significance and management ► Provide an overview of pacemaker components, nomenclature and functions ► Discuss complications of pacemaker implantation ► Talk about pacemaker malfunction ► Touch on ED management and disposition of pacemaker patients ► Offer a precis of temporary pacing modalities. ► ICDs not covered in this talk. Case ► 85 y.o. F complaining of feeling “off” and being “just so tired” ► Denies CP, SOB ► Vaguely recalls feeling a bit “unsteady” on a couple of occasions ► PMHx: osteoporosis, hypothyroidism and depression ► Meds: Calcium, Vit D, Celexa, Synthroid Case cont’d ► Vitals: HR 45, regular RR 16 BP 108/75 02 sats 97% on RA Afebrile Granny’s EKG: Atrioventricular Blocks ► Definition: Delay or interruption in the transmission of an impulse from the atria to the ventricles Conduction may be delayed, intermittent or absent. ► Duration Transient Permanent ► Causes may be: Anatomical Functional Etiology ► Fibrosis and sclerosis of the conduction system ► Ischemic heart disease ► Drugs ► Increased vasovagal tone ► Valvular disease ► Congenital heart disease ► Other: Cardiomyopathies, myocarditis, hyperkalemia, infiltrating malignancies, miscellaneous Surgery – CABG, valve replacement Sclerosis and fibrosis of the conduction system ► ► Account for 50% of AV block 2 idiopathic entities: 1. Lev’s Disease: – – – “sclerosis of left side of the heart” Affects older people Associated with calcific aortic and mitral valves that extends into the adjacent conduction system 2. Lenegre’s Disease: ► ► ► ► ► Progressive fibrotic, sclerodegenerative disease Affects younger people May be hereditary Slow progression to complete heart block Presents with bradycardia and some degree of AVB Ischemic Heart Disease ► Accounts for 40% of AV block ► Chronic or acute ischemic changes can disrupt conduction ► With AMI: 20% will develop AVB ► 8% 1st degree AVB ► 5% 2nd degree AVB ► 6% 3rd degree AVB ► Up to 20% increased mortality with bradycardia and/or blocks post AMI Drugs ► Cardiac medications: Digitalis, CCB (especially verapamil), B-blockers ► Class Ia: Quinidine, procainamide, disopyramide ► Cholinergics: cholinesterase inhibitors ► Opioids and sedatives ► Drugs with Class IA type effects: TCAs, carbamazepine, quinine, chloroquine ► Cocaine Increased Vagal Tone ► Vasovagal ► Pain ► Occulocardiac reflex ► Diving reflex ► Carotid sinus massage ► Hypersensitive carotid sinus syndrome Stimulation of carotid sinus leads to bradyasystole and then to pre/syncope Cardioinhibitory: >3s of asystole with carotid stimulation Vasodepressor effects Valvular Disease ► Due to extension of calcification into conduction system ► Associated with AV and MV repair ► Repair of VSD: including transcoronary ablation of septal hypertrophy Infectious ► AVB with the following usually indicates poor prognosis: ► Myocarditis: Viral: Cocksackie B Bacterial: Diptheria Protozoal: Chagas disease Spirochetal: Lyme disease Syphilis, toxoplasmosis Other ► ► ► ► ► ► ► ► Congenital heart disease, neonatal SLE syndrome Familial heart disease: cardiac sodium channel SCN5A linked mutations Cardiomyopathies: HOCM, amyloidosis, sarcoidosis Endocrine causes: Hyperthyroidism hypoadrenalism Hyperparathyroidism Acromegaly Electrolyte abnormalities: Hyperkalemia: >6.3 meq/L Hypercalcemia Hypermagnesemia Infiltrative malignancies: lymphoma, multiple myelomas Neuromuscular degenerative diseases Cardiac tumours First Degree Heart Block ► SA node is normal Normal P wave ► AV node conducts more slowly than normal Prolonged PR interval >0.2s PR interval is constant ► Rest of conduction is normal Normal QRS First Degree AVB ► ► ► ► Conduction delay can occur in: Atrium: 3% of cases May be due to intratrial pathology EKG findings: widening of P wave and decreased P wave voltage AV node: Most common site Common causes: increased vagal tone, CCB, digoxin, BB EKG findings: long PR interval with a narrow or wide P wave and narrow QRS Bundle of His: Drugs that block sodium channels can impair depolarization and slow conduction (Quinidine, procainamide) First Degree AVB ►Clinical significance – none ►Treatment – none ►May progress to 2nd or 3rd degree AVB Second Degree AVB ► Some atrial impulses fail to reach the ventricles ► 2 types: Mobitz Type I (Wenckebach): progressive PR interval lengthening to a non-conducted P wave Mobitz Type II: PR interval constant prior to P wave that does not conduct to the ventricles. SECOND DEGREE A-V BLOCK (MOBITZ I OR WENCKEBACH) Mobitz Type I (Wenckebach) AVB ► Most often involves AV node ► Benign ► Features: Gradually increasing PR interval Gradually decreasing R-R interval Dropped beat Largest delay occurs in the first beat and then decreases beat to beat until block occurs and cycle is reset Group beating: 3:2,4:3 etc. Second Degree Heart Block (2º) Mobitz Type I (Wenkebach) PR PR PR DROPPED BEAT Mobitz Type I ► Clinical implications: Often asymptomatic May have some symptoms eg lethargy, confusion If cardiac output is reduced, patient may experience angina, syncope or heart failure due to bradycardia and resultant hypoperfusion state. Can occur in athletes with high vagal tone Elderly: aging prolongs cycle length Further implications: ► Underlying IHD: Mobitz type I can be complication of inferior MI as: RCA supplies inferior and posterior walls and AV and SA nodes Associated with increased mortality ► Treatment: Removing reversible causes (ischemia, increased vagal tone, medications Pacemaker if symptomatic during day No pacemaker is symptoms at night ► May progress to 3rd degree AVB MOBITZ TYPE II Mobitz Type II AVB ► Always occurs below the AV node 20% within Bundle of His 80% in bundle branches ► Widened QRS ► PR interval may be normal or slightly prolonged but constant ► Non-conducted P wave on EKG ► Clinical implications: Dizziness Presyncope Syncope Mobitz Type II AVB ► Type II is permanent and may progress to higher levels of block ► Treatment: Remove reversible causes Potential candidates for pacemaker insertion Second Degree AVB 2:1 ► Unable to classify as Mobitz type I or II ► Ratio of 2 P waves to 1 QRS ► Clinical significance: Will be associated with symptoms (dizziness, lethargy etc.) May progress to 3rd degree AVB ► Treatment - pacemaker THIRD DEGREE A-V BLOCK Third degree (complete) AVB ► No atrial impulses reach the ventricles due failure of AV node therefore no P wave conduction ► AV dissociation (Ps marching through…) ► QRS complex: Narrow: block at AV node to level of bundle of His Wide: block below level of bundle of His ► More distal the block the slower the escape rhythm If <40bpm: pacemaker is unreliable causing profound bradycardia or asystole Syncope is very common Clinical Significance ► Clinical Implications: Dizziness Presyncope Syncope Ventricular tachycardia Ventricular fibrillation Confusion Can worsen angina and CHF ► Treatment: Pacemaker! Class I Indications for Permanent Pacing in Adults per AHA/ACC 1. • • • • • • 3rd degree AVB at any anatomic level associated with any of the following: Symptomatic bradycardia (secondary to AVB) Symptomatic bradycardia (secondary to drugs required for management of dysrhythmias or other medical conditions) Documented asystole >3s or escape rate of <40 bpm in awake, asymptomatic patient After ablation of AV node Postoperative AVB that is not expected to resolve Neuromuscular disease with AVB (neuromuscular dystrophies) 2. Symptomatic bradycardia from 2nd degree AVB regardless of type or site of block. 3. Chronic bifascicular or trifascicular block with intermittent 3rd degree AV block or type II 2nd degree AVB. 4. After AMI with any of the following: Persistent 2nd degree AVB at the His-Purkinje level with bilateral bundle branch block or 3rd degree AVB at or below His-Purkinje system Transient 2nd or 3rd degree infranodal AVB and associated BBB Symptomatic, persistent 2nd or 3rd degree AVB 5. Sinus node dysfunction with symptomatic bradycardia or chronotropic incompetence. 6. Recurrent syncope caused by carotid sinus stimulation. Pacemaker indications: Class IIa ► Complete AVB without symptoms: >40bpm while awake = Class IIa indication UNLESS: ► Activity or exercise is limited ► Heart begins to enlarge ► LV function is depressed ► LA enlargement is noted ► Intra- or infra-Hisian block issuspected with of without QRS widening ► QT interval prolongation ► Ventricular arrhythmias ► Episodic profound bradycardia (during sleep or awake) Pacemaker indications: take home points! ► Complete AVB with: Associated symptoms Ventricular pauses >3s Resting HR <40 bpm while awake = pacemaker! Granny ► Remember Granny? ► Well, she can be helped by some of the information in the next part of the talk… Quiz ► Here is a photo of the first pacemaker invented (obviously not an internal device!) ► Circa 1950 ► True or false: the inventor was Canadian… True! ► Courtesy of John Hopps - an engineer from the University of Manitoba. ► He recognized that if a heart stopped beating it could be started again by artificial stimulation using mechanical or electric means. ► Current pacemakers provide electrical stimulation to cause cardiac contraction when intrinsic cardiac electrical activity is slow or absent. A Brief History of Pacemakers Just kidding…but did you know? ► ► ► ► ► The implantable cardiac pacemaker was discovered by mistake! Wilson Greatbatch was building an oscillator to record heart sounds. When he accidentally installed a resistor with the wrong resistance into the unit, it began to give off a steady electrical pulse. Greatbatch realized that the small device could be used to regulate the human heart. After two years of refinements, he had handcrafted the world's first successful implantable pacemaker (patent #3,057,356). Until that time, the apparatus used to regulate heartbeat was the size of a television set, and painful to use. Greatbatch later went one step further, inventing a corrosion-free lithium battery to power the pacemaker. All told, his pacemakers and batteries. Thus in 1985 the National Society of Professional Engineers named Greatbatch's invention one of the ten greatest engineering contributions to society of the last 50 years. Pacemaker Functions 1. 2. 3. 4. Stimulate cardiac depolarization Sense intrinsic cardiac function Respond to increased metabolic demand by providing rate responsive pacing Provide diagnostic information stored by the pacemaker Pacemaker Components Combine with Body Tissue to Form a Complete Circuit ► Pulse generator: power source or battery ► Leads or wires ► Cathode (negative electrode) ► Anode (positive electrode) ► Apex of right ventricle Lead IPG Anode Cathode The Pulse Generator: ► Submuscular or subcutaneous implantation location ► Contains a lithium battery that has a 410 year lifespan ► Slow, gradual decrease in power over time ► A sudden power failure is very uncommon Circuitry Battery Electronic Circuitry ► Sensing circuit ► Timing circuit ► Output circuit Lead System Bipolar ► Lead has both negative, (Cathode) distal and positive, (Anode) proximal electrodes ► Separated by 1 cm ► Larger diameter: more prone to fracture ► Compatible with ICD Unipolar ► Negative (Cathode) electrode in contact with heart ► Positive (Anode) electrode: metal casing of pulse generator ► Prone to oversensing ► Not compatible with ICD Difference on an ECG? Bipolar ► current travels only a short distance between electrodes ► small pacing spike: <5mm + Anode Cathode Difference on an ECG? Unipolar ► current travels a longer distance between electrodes ► larger pacing spike: >20mm + Anode Cathode Pacemaker Code I Chamber Paced II Chamber Sensed III Response to Sensing IV Programmable Functions/Rate Modulation V: Ventricle V: Ventricle T: Triggered P: Simple programmable A: Atrium A: Atrium I: Inhibited M: Multiprogrammable D: Dual (A+V) D: Dual (A+V) D: Dual (T+I) C: Communicating O: None O: None S: Single S: Single (A or V) (A or V) O: None V Antitachy Function(s) P: Pace S: Shock D: Dual (P+S) R: Rate modulating O: None O: None Common Pacemakers VVI Ventricular Pacing : Ventricular sensing; intrinsic QRS Inhibits pacer discharge ► VVIR As above + has biosensor to provide Rateresponsiveness ► DDD Paces + Senses both atrium + ventricle, intrinsic cardiac activity inhibits pacer d/c, no activity: trigger d/c ► DDDR As above but adds rate responsiveness to allow for exercise ► Rate Responsive Pacing ► When the need for oxygenated blood increases, the pacemaker ensures that the heart rate increases to provide additional cardiac output Adjusting Heart Rate to Activity Normal Heart Rate Rate Responsive Pacing Fixed-Rate Pacing Daily Activities Rate Response ► Rate responsive (also called rate modulated) pacemakers provide patients with the ability to vary heart rate when the sinus node cannot provide the appropriate rate ► Rate responsive pacing is indicated for: Patients who are chronotropically incompetent (heart rate cannot reach appropriate levels during exercise or to meet other metabolic demands) Patients in chronic atrial fibrillation with slow ventricular response Single Chamber ► VVI - lead lies in right ventricle ► Independent of atrial activity ► Use in AV conduction disease Paced Rhythm Recognition AAI / 60 Paced Rhythm Recognition VVI / 60 Advantages and Disadvantages of Single-Chamber Pacing Systems Advantages ► Implantation single lead Disadvantages of a ► Single ventricular lead does not provide AV synchrony ► Single atrial lead does not provide ventricular backup if A-to-V conduction is lost Dual Chamber Typically in pts with nonfibrillating atria and intact AV conduction ► Native P, paced P, native QRS, paced QRS ► ECG may be interpreted as malfunction when none is present ► May have fusion beats ► Four “Faces” of Dual Chamber Pacing ► Atrial Pace, Ventricular Pace (AP/VP) AV AP V-A VP Rate = 60 bpm / 1000 ms A-A = 1000 ms AV AP VP V-A Four “Faces” of Dual Chamber Pacing ► Atrial Pace, Ventricular Sense (AP/VS) AV AP V-A VS Rate = 60 ppm / 1000 ms A-A = 1000 ms AV AP VS V-A Four “Faces” of Dual Chamber Pacing ► Atrial Sense, Ventricular Pace (AS/ VP) AV AS V-A VP V-A AV AS Rate (sinus driven) = 70 bpm / 857 ms A-A = 857 ms VP Four “Faces” of Dual Chamber Pacing ► Atrial Sense, Ventricular Sense (AS/VS) AV AS V-A VS Rate (sinus driven) = 70 bpm / 857 ms Spontaneous conduction at 150 ms A-A = 857 ms AV AS V-A VS Paced Rhythm Recognition DDD / 60 / 120 Paced Rhythm Recognition DDD / 60 / 120 Pacemaker Interventions ► Magnet application No universal function of magnet Does not inhibit or turn off pacemaker Model-specific magnet that activate a reed switch that coverts unit to asynchronous pacing at a pre-set rate that is no longer inhibited by patient’s intrinsic electrical activity. ► Interrogation / Programming Model-specific pacemaker programmer can non-invasively obtain data on function and reset parameters Magnet Application Complications of Pacemaker Implantation ►Infection ►Venous obstruction ►Pacemaker Syndrome Infection ► ► ► ► ► ► ► ► ► ► 2% for wound and ‘pocket’ infection 1% for bacteremia with sepsis NB pacemaker = foreign body! Patient may have symptoms of pain, local inflammation, hematoma Blood cultures should be drawn Culprits are S. aureus (60%) and S. epidermidis (70%) Vancomycin should be started pending cultures Pacemaker and leads are removed if bacteremic Temporised with transvenous pacing iv antibiotics for 4-6 weeks with new components implanted. Venous Obstruction Incidence 30-50% ► Can involve axillary, innominate, subclavian veins and SVC ► 1/3 have chronic complete venous obstruction but are asymptomatic due to collateralization ► 0.5-3.5% develop symptoms which include: edema, pain, venous engorgement of the ipsilateral arm to insertion ► US, venography, CT to diagnose acute thrombosis ► Heparin, lifetime warfarin; early thrombolytic therapy is most effective ► Venous Access Issues ► Pneumo / hemothorax ► Air embolism ► CONTROVERSIAL: association of PE with pacemaker ► RARE: SVC syndrome from pacemaker leadinduced thrombosis Pacemaker Syndrome ► ► ► 20% of patients present with new complaints or worsening of initial symptoms that led to pacemaker insertion More commonly with single chamber pacer AV synchrony is lost retrograde VA conduction atrial contraction against closed MV + TV jugular venous distention + atrial dilation sx of CHF and reflex vasodepressor effects ► Symptoms: Pre/syncope Orthostatic dizziness Fatigue Exercise intolerance Weakness Lethargy Chest fullness or pain Cough Uncomfortable pulsations n neck or abdomen RUQ pain Other Pacemaker Syndrome ► 1/3 of patients can adapt and these symptoms resolve ► 1/3 require that a dual chamber pacer replace the single chamber pacer ► If symptoms occur with dual chamber pacer then optimizing timing of ventricular pacing is key ► Beware: symptoms of pacemaker syndrome and pacemaker malfunction are the same! Pacemaker Malfunction Four categories: • • • • Failure to Capture Inappropriate sensing: under or over Inappropriate pacemaker rate The good news! • • Rarely immediately life threatening Occurs in <5% of patients bold indicates most common malfunctions Failure to Capture ► Absence of pacemaker spikes despite indication to pace ► Caused by: Battery depletion - rare Fracture of pacemaker lead – most common problem Disconnection of lead from pulse generator unit Lead displacement – due to change cardiac Exit block – failure of an adequate stimulus to depolarize the paced chamber ► Seen in changes in endocardium in contact with pacing system i.e. infarction, ischemia, hyperkalemia, class III antiarrhythmics (amiodarone, bertylium) No Capture ► Pacemaker artifacts do not appear on the ECG; rate is less than the lower rate Pacing output delivered; no evidence of pacing spike is seen A: failure to capture atria in DDD Sensing ► Sensing is the ability of the pacemaker to “see” when a natural (intrinsic) depolarization is occurring Pacemakers sense cardiac depolarization by measuring changes in electrical potential of myocardial cells between the anode and cathode Accurate Sensing... ► Ensures that undersensing will not occur – the pacemaker will not miss P or R waves that should have been sensed ► Ensures that oversensing will not occur – the pacemaker will not mistake extracardiac activity for intrinsic cardiac events ► Provides for proper timing of the pacing pulse – an appropriately sensed event resets the timing sequence of the pacemaker Inappropriate sensing: Undersensing ► Pacemaker incorrectly misses an intrinsic depolarization paces despite intrinsic activity ► Appearance of pacemaker spikes occurring earlier than the programmed rate: “overpacing” ► May or may not be followed by paced complex: depends on timing with respect to refractory period ► Causes: AMI, progressive fibrosis, lead displacement, fracture, poor contact with endocardium Undersensing ► Pacemaker does not “see” the intrinsic beat, and therefore does not respond appropriately Intrinsic beat not sensed Scheduled pace delivered VVI / 60 Undersensing ► An intrinsic depolarization that is present, yet not seen or sensed by the pacemaker P-wave not sensed Atrial Undersensing Inappropriate sensing: Oversensing ►Detection of electrical activity not of cardiac origin intermittent, irregular pacing or inhibition of pacing activity ►State of “underpacing” Accurate Sensing Requires That Extraneous Signals Be Filtered Out ► Sensing amplifiers use filters that allow appropriate sensing of P waves and R waves and reject inappropriate signals ► Unwanted signals most commonly sensed are: T waves Far-field events (R waves sensed by the atrial channel) Skeletal myopotentials (e.g., pectoral muscle myopotentials) Oversensing Marker channel shows intrinsic activity... ...though no activity is present VVI / 60 ► An electrical signal other than the intended P or R wave is detected Environmental Factors Interfering with Sensing ► Electrocautery: causes temporary pacemaker inhibition ► MRI: alters pacemaker circuitry and results in fixed-rate or asynchronous pacing ► Cellular phone: pacemaker inhibition, asynchronous pacing ► Arc welding ► Lithotripsy ► Microwaves ► Mypotentials from muscle Inappropriate Pacemaker Rate ► Rare reentrant tachycardia seen with dual chamber pacers ► Premature atrial or ventricular contraction sensed by atrial lead triggers ventricular contraction retrograde VA conduction sensed by atrial lead triggers ventricular contraction etc etc etc ► Tx: Magnet application: fixed rate, terminates tachyarrthymia, ► Reprogram to decrease atrial sensing Causes of Pacemaker Malfunction ► ► ► ► Circuitry or power source of pulse generator Pacemaker leads Interface between pacing electrode and myocardium Environmental factors interfering with normal function Pulse Generator ► Loose connections Similar to lead fracture Intermittent failure to sense or pace ► Migration Dissects along pectoral fascial plane Failure to pace ► Twiddlers syndrome Manipulation lead dislodgement Leads ► Dislodgement or fracture (anytime) Incidence 2-3% Occurs if pacemaker is placed medially Failure to sense or pace Dx with CXR, lead impedance ► Insulation breaks Current leaks failure to capture Dx with measuring lead impedance (low) Case continued… ► Granny has had a pacemaker implanted 8d ago. ► She went home feeling just fabulous! ► She is in the ED with sharp, stabbing retrosternal chest pain that started after tea this morning. ► The pain is pleuritic. ► When pressed, she says she was “quite winded” getting up the stairs from the cellar yesterday. ► Diagnosis? Cardiac Perforation ► ► Can happen early or late (days to weeks) post implantation Need high index of suspicion because: Often well tolerated due to small puncture size May auto-tamponade May be asymptomatic May have hiccups May have pleuritic retrosternal chest pain, SOB ► May have increased pacing threshold ► Px: may hear pericardial friction rub ► CXR, FAST helpful ► Echo mandatory to rule out ► Pacemaker Mediated Tachycardia (PMT) ► PMT is a paced rhythm, usually rapid, which is sustained by ventricular events conducted retrogradely (i.e., backwards) to the atria ► PMT can occur with loss of AV synchrony caused by: PVC Atrial non-capture Atrial undersensing Atrial oversensing Built in solution: PMT Intervention ► Designed to interrupt a Pacemaker-Mediated Tachycardia DDD / 60 / 120 Pseudomalfunction: Hysteresis ► Allows a lower rate between sensed events to occur; paced rate is higher Lower Rate 70 ppm Hysteresis Rate 50 ppm Management: History ► Most complications and malfunctions occur within first few weeks or months ► Pacemaker identification card: should tell you what you need to know about the device ► Syncope, near syncope, orthostatic dizziness, lightheaded, dyspnea, palpitations ► Pacemaker syndrome: diagnosis of exclusion Management: Physical Exam ► Look for : Fever: think pacemaker infection Cannon “a” waves: AV asynchrony Bibasilar crackles if CHF Pericardial friction rub if perforation of RV Management: adjuncts ► CXR: Determine tip position Determine number of leads and position ► EKG May reveal failure to sense or pace Low pacing rate Abnormally rapid rhythm = pacemakermediated tachycardia Management: ACLS ► Drugs and defibrillation as per ACLS guidelines ► Recommended to keep paddles >10cm from pulse generator ► May transcutaneously pace ► Transvenous pacing may be inhibited by venous thrombosis: may need fluoroscopic guidance AMI + Pacers ► Difficult diagnosis ► Most sensitive indicator is ST-T wave changes on serial ECG ► If clinical presentation strongly suggestive then should treat as AMI ► Coarse VF may inhibit pacer (oversensing) ► Successful resuscitation may lead to failure to capture (catecholamines, ischemia) Disposition ► Admit Pacemaker infections /unexplained fever or WBC Myocardial perforation Lead # or dislodgement Wound dehiscence / extrusion or erosion Failure to pace, sense, or capture Ipsilateral venous thrombosis Unexplained syncope Twiddlers syndrome Disposition ► Potentially fixable in ED w/ help Pacemaker syndrome Pacemaker-mediated tachycardia Oversensing Diaphragmatic pacing Myopotential inhibitors Temporary Pacing Modalities 1. 2. Transcutaneous Transvenous Emergency Pacing ► Hemodynamically compromising bradycardia ► Bradycardia with escape rhythms ► Overdrive pacing of refractory tachycardia ► Bradyasystolic cardiac arrest (within 5 minutes) ► Bradycardia dependent ventricular tachyarrhythmia (Torsade-de-Pointes) Indications for temporary pacing ► With AMI with: Symptomatic sinus node dysfunction Mobitz type II 2nd degree AVB 3rd degree AVB New left, right or alternating BBB or bi-fascicular block Before electrical cardioversion of a patient with sick sinus syndrome or with a high level of dependency to a permanent pacemaker Prior to permanent pacemaker implantation Prior to PA cath insertion if underlying LBBB Transcutaneous Pacing Pitfalls: ► Capture is obtained between 40-80 mA regardless of age, body weight and BSA ► May see INCREASED pacing threshold with: Suboptimal lead position Poor skin-electrode contact Post surgical chestwall disruption Emphysema Pericardial effusion PPV Hypoxia/ischemia/shock/acidosis/hyperkalemia After electrical cardioversion/defibrillation After prolonged resuscitation/arrest Transcutaneous Pacing ► Initiation of pacing: Use maximal current output and asynch setting Adjust current to ~10mA above threshold Confirm capture by: ►Pulse palpation ►Doppler ►Arterial line tracing Pitfalls/Complications ► Failure to recognise underlying VF ► Failure to recognise that pacemaker is NOT capturing ► Complications: Painful Induction of arrhythmias Tissue damage Transvenous Pacing ► Most consistent and reliable means of temporary pacing ► Can permit atrial and/or ventricular pacing ► Stable ► Well tolerated ► Significant potential complications Transvenous Pacing ►4 letter coding system: 1st letter: indicates paced chamber (V,A,D) 2nd letter: indicates sensed chamber (V,A,D) 3rd letter: mode of response when an event is sensed ►I = inhibited ► T = triggered ► D = inhibited or triggered ► 0 = neither inhibited, nor triggered 4th letter: R indicates rate responsiveness (only in permanent device) Can be uni or bipolar ► ► ► ► ► ► Unipolar System Simple Less sophisticated electrode Dipole is between tip of electrode and generator Higher risk of oversensing Larger spike on EKG Bipolar System ► More complex electrode ► Larger electrode ► Dipole is at tip of electrode ► Lower risk of oversensing ► Small spike on EKG ► Higher risk of electrode failure ► Contraindications to transvenous pacing ► Tricuspid valve mechanical prosthesis ► Existing endocarditis ► Infected endocardial pacemaker lead ► Sepsis/bacteremia ► Ventricular arrhythmias Capture ► Depends on: Stable catheter position Viability of paced myocardial tissue Electrical integrity of pacing system Most common cause of lost capture is lead dislodgement/perforation ► Other causes include: ► Poor endocardial contact Local myocardial necrosis/fibrosis/inflammation/ edema Hypoxia/acidosis/electrolyte abnormalities/drug effects Lead fracture Generator malfunction/battery failure Unstable electrical connections Sensing problems Undersensing ► Lead dislodgement/ perforation ► Local tissue necrosis/fibrosis ► Lead fracture ► Electrocautery ► Generator malfunction ► Unstable electrical connections ► ► Oversensing ►P wave sensing ► T wave sensing ► Myopotential sensing ► Electromagnetic interference ► Poor electrical contacts, connections ► Lead fracture Complications ► Arrhythmias ► Thromboembolic events - ? Need to anticoagulate ► Clinical infection/phlebitis ► Bacteremia ► Perforation ► Knotting of catheter ► Tricuspid valve damage ► Induction of RBBB ► Phrenic nerve or diaphragmatic pacing without myocardial perforation Myocardial Perforation ► Symptoms ► Signs ► Pericardial ► Pericardial chest pain ► Shoulder pain ► Diaphragmatic pacing ► Skeletal muscle pacing ► Dyspnea ► Hypotension (?tamponade) rub ► Intercostal or diaphragmatic pacing ► Failure to pace or sense ► New pericardial effusion or tamponade Investigations ► EKG: Change in QRS morphology +/- axis Failure to pace or sense Pericarditis pattern ► CXR: Change in lead position Extra-cardiac location of lead tip Thanks! References ► ► ► ► ► ► ► ► ► Thanks to Karen Hillier, Pacemaker Nurse Clinician Rosens: Chapter 28 Barold, S. Serge. Cardiac pacemakers step by step : an illustrated guide. Blackwell, 2004. Haim M et al. Frequency and prognostic significance of high degree atrioventricular block in patients with first non-Q wave acute myocardial infarction. Am J Cardiol. 1997;79:674. Lamas G et al. Ventricular Pacing or Dual Chamber Pacing for Sinus Node Dysfunction. NEJM. 2002;346(24):1854-61. Lamas G et al. A simplified approach to predicting the occurrence of complete heart block during acute myocardial infarction. Am J Cardiol. 1986;57:1213. Mangrum JM, DiMarco JP. The evaluation and Management of bradycardia. NEJM. 2000;342(10):703-9. www.uptodate.com for heart blocks and pacemaker information ACC/AHA Guidelines for Pacemaker implantation: http://www.acc.org/qualityandscience/clinical/guidelines/april98/jac5507gtc.ht m CHB and AMI ► Incidence of new CHB 5.4% ► Occurring 2.6 days post MI ► Developed in: >60 y.o. Comorbid CHF Associated with increased risk of developing cardiogenic shock MILIS Trial: Predictors of CHB ►1 point for each of the following: PR prolongation 2nd degree AVB LAFB or LPFB LBBB RBBB 1.2-6.8% with score of zero 7.8-10% with score of 1 25-30% with score of 2 36% with a score of 3 or more ► Risk of Progression: CHB and NSTEMI ► SPRINT Study Group: 610 patients with first NSTEMI: ►2nd or 3rd degree AVB in 7% (45/610) ►These patients had: Increased rate of cardiac arrest Increased rate of CHF Increased rate of elevated cardiac markers Higher in hospital mortality Larger and more complicated infarctions No difference in mortality outcomes at 5 years CHB post AMI and the Elderly ► Incidence 4.7% ► New AVB in 3.2% ► More commonly associated with inferior MI compared to anterior MI (7.3 vs 3.0%) ► Associated with increased in hospital mortality but no change in long term mortality outcomes Infarct location and conduction disturbances ► Inferior MIs: 1. 2. 3. Conduction changes can occur acutely to days post MI RCA supplies the SA node, AV node, and bundle of His Sinus bradycardia Up to 40% of patients within hours of infarct Due to increased vagal tone May be due to transient sinus node dysfunction 9.8% of patients May be transient (x days) From an infranodal lesion Narrow QRS Develops from 1st to 3rd degree AVB Asymptomatic bradycardia Resolves within 5-7d Mobitz type I AVB CHB ► Anterior MI: 1st degree AVB below AV node with widened QRS 2nd degree type II with unpredictable clinical course with block progression CHB occurs in first 24h: ►Abrupt onset ►Wide and unstable escape ryhthm ►High mortality: arrhythmias and pump failure ►Due to extensive necrosis of bundle branches Permanent Pacing ► 3rd degree AVB within or below the HisPurkinje system ► Persistent 2nd degree AVB ► Transient advanced infranodal AVB with bundle branch blocks due too infarction ► Symptomatic and persistent 2nd or 3rd degree AVB ACC/AHA/NASPE: indications for permanent pacing in acquired atrioventricular (AV) block in adults Class I ► 1. Third-degree and advanced second-degree AV block at any anatomic level, associated with any one of the following conditions: ► a. Bradycardia with symptoms (including heart failure) presumed to be due to AV block. (Level of Evidence: C) b. Arrhythmias and other medical conditions that require drugs that result in symptomatic bradycardia. (Level of Evidence: C) c. Documented periods of asystole 3.0 seconds or any escape rate <40 beats per minute in (bpm) in awake, symptom-free patients. (Levels of Evidence: B, C) d. After catheter ablation of the AV junction. (Levels of Evidence: B, C) There are no trials to assess outcome without pacing, and pacing is virtually always planned in this situation unless the operative procedure is AV junction modification. e. Postoperative AV block that is not expected to resolve after cardiac surgery. (Level of Evidence: C) f. Neuromuscular diseases with AV block, such as myotonic muscular dystrophy, Kearns-Sayre syndrome, Erbs dystrophy (limb-girdle), and peroneal muscular atrophy, with or without symptoms, because there may be unpredicatable progression of AV conduction disease. (Level of Evidence B:) ► 2. Second-degree AV block regardless of type or site of block, with associated symptomatic bradycardia. (Level of Evidence: B) Class IIa 1. Asymptomatic third-degree AV block at any anatomic site with average awake ventricular rates of 40 beats per minute or faster especially if cardiomegaly or left ventricular (LV) dysfunction is present. (Levels of Evidence: B, C) 2. Asymptomatic type II second-degree AV block with a narrow QRS. When type II second-degree AV block occurs with a wide QRS, pacing becomes a Class I recommendation. (Level of Evidence: B) 3. Asymptomatic type I second-degree AV block at intra- or infraHis levels found at electrophysiological study performed for other indications. (Level of Evidence: B) 4. First- or second-degree AV block with symptoms suggestive of pacemaker syndrome. (Level of Evidence: B) ► Adapted from Gregoratos, G, Abrams, J, Epstein, AE, et al. Circulation 2002; 106:2145.