RESPIRATION

RESPIRATION
Dr. Zainab H.H
Dept. of Physiology
Lec.1,2
“Roses are red,
Violets are blue,
Without your lungs
Your blood would be, too.”
David D. Ralph, MD
New England Journal of Medicine
objectives
Describe the mechanism of respiration
List the non respiratory functions of the lung
Describe the basic structures of the lung
Respiratory System
Made up of:
1. Gas exchanging organ – Lungs
2. Pump that ventilates the lungs – consists of:
Chest wall
Respiratory Muscles – increase and decrease the size of the thoracic cavity
Areas in the Brain – control the muscles
Tracts and Nerves – connect the brain to the muscles
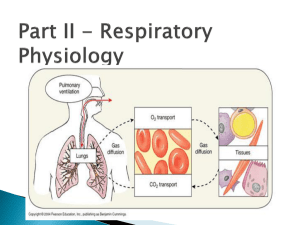
Basics Of Respiration
A process involving:
Taking up of Oxygen from the air.
Utilizing the Oxygen in the tissues.
Removal of the Carbon dioxide formed.
O
2
Tissues:
Use of O
2
Removal
Of CO
2
Respiration
The term respiration includes 3 separate functions:
1. Ventilation:
I.
Breathing.
2. Gas exchange:
I.
II.
3. O
I.
2
Between air and capillaries in the lungs.
Between systemic capillaries and tissues of the body.
utilization:
Cellular respiration.
External Respiration
1)
2)
3)
Inspiration: The process of taking in of air (O
2
) from the external environment.
Expiration: Giving out of air (CO
2
) from the body to the external environment.
Exchange of gases between the body and the external environment.
Internal Respiration
1)
2)
Tissue or Cell level Respiration.
Oxygen is utilized by tissues for the metabolism of organic molecules.
Oxygen Carbon Dioxide
TISSUES
Non Respiratory Functions Of
Lungs
I. Defense & Protection:
1.
Warms & humidifies the air.
2.
3.
4.
5.
Dust particles are trapped by the
Bronchial secretions.
The Ciliary Escalator removes trapped matter by expectoration(Cough)
Secretory Ig.A provides Immunity against airborne microbes.
Pulmonary Alveolar Macrophages(PAMs) engulf foreign bodies by Phagocytosis.
Non Respiratory Functions Of
Lungs
II. Metabolism & Other functions:
1.
Regulation of blood pH.
2.
Synthesis of proteins, Fats &
Carbohydrates.
3.
4.
Fibrinolysis & removal of blood clots.
Phonation or Speech.
Non Respiratory Functions Of
Lungs
7.
8.
9.
5.
6.
Removal of vasoactive local hormones.(Bradykinin, PGE, E
2 etc.)
ACE (from Pulmonary Capillary endothelium) converts Angiotensin I into Angiotensin II.
Destruction of Thrombocytes.
Maintaining Body Water balance
Thermoregulation.
Functional division of
Respiratory System
1)
2)
Conducting zone
- All the structures air passes through before reaching the respiratory zone.
Respiratory zone
- Region of gas exchange between air and blood.
Includes terminal respiratory bronchioles and alveolar sacs.
Thoracic Cavity
1)
2)
Diaphragm:
Sheets of striated muscle divides anterior body cavity into
2 parts.
Above diaphragm: thoracic cavity:
Contains heart, large blood vessels, trachea, esophagus, thymus, and lungs.
Below diaphragm: abdominopelvic cavity:
Contains liver, pancreas, GI tract, spleen, and genitourinary tract.
Thoracic Cavity
Structures in the central region “ mediastinum ” enveloped by two layers of pleural membranes.
1.
Parietal (superficial) – lines the inside of thoracic wall.
2.
Visceral (deep) – covers lung surface
The visceral pushed against parietal pleura
Under normal condition – little or no air
There is potential space “ intrapleural space = pleural cavity ”
Pleural Cavity
A.
B.
Filled with fluid produced by the pleural membranes.
It does 2 things:
Act as lubricants – parietal and visceral pleural past each other
Helps hold parietal and visceral pleural membrane together
Muscles Of Respiration
For Inspiration
1.
2.
Diaphragm – 75%
External intercostals
3.
4.
5.
Sternocleidomastoid
Serratus (anterior)
Scaleni
For Expiration
1.
2.
Internal intercostals
Abdominal recti
Physical aspects of
Ventilation
Ventilation - mechanical process that moves air in and out of the lungs.
Pressure difference induced by change in lung volumes
Air move from high to low pressure between conducting zone & terminal bronchioles
Quiet Inspiration
Active process:
Contraction of diaphragm, increases thoracic volume vertically.
Contraction of parasternal and external intercostals, raising the ribs; increasing thoracic volume laterally.
Pressure changes:
Alveolar changes from 0 to –3 mm Hg.
Intrapleural changes from –4 to –6 mm Hg.
Transpulmonary pressure = +3 mm Hg.
Expiration
Passive process.
The diaphragm, thoracic muscles, thorax, and lungs recoil.
Pressure changes:
Intrapulmonary pressure changes from –3 to +3 mm Hg.
Intrapleural pressure changes from –6 to –3 mm
Hg.
Transpulmonary pressure = +6 mm Hg.
The air we breathe!
Definitions
Atmospheric Air: Air at the normal sea level.
Alveolar Air: The inspired air which has reached the alveoli. (Before the exchange of gases)
Expired Air: The air which is exhaled after the exchange process.
Atmosphere
The air that envelopes the
Planet earth.
The air that we normally live in.
Has a pressure of 1 Atmosphere or 760mm of Hg.
Boyle’s Law
Gas pressure in closed container is inversely proportional to volume of container
Changes in lung volume changes in intrapulmonary pressure.
Increase in lung volume decreases intrapulmonary pressure.
Air goes in.
Decrease in lung volume, raises intrapulmonary pressure above atmosphere.
Air goes out.
Atmospheric &
Intrapulmonary Pressures
During inspiration – air enters the lungs
(atmospheric pressure > intrapulmonary
“intrapleural” pressure)
Quiete inspiration – intrapulmonary pressure 3 mmHg sub atmospheric.
During expiration – air goes out of the lung
(intrapulmonary “intrapleural” pressure > atmospheric pressure)
Quiete expiration - intrapulmonary pressure 3 mmHg greater than atmospheric pressure.
Intrapleural Pressure
Pressure in the intrapleural space.
It is negative, due to lack of air in the intrapleural space.
More negative during inspiration – expansion of thoracic cavity
It is normally lower than intrapulmonary pressure during both inspiration and expiration
Intrapleural Pressure
1.
2.
During inspiration, the intrapleural pressure falls further for two reasons: as the lung expands, the elastic recoil increases. This increases the pull on the lung away from the chest wall, dropping the intrapleural pressure further.
the fall in the alveolar pressure is transmitted to the intrapleural space, increasing the pressure drop
During expiration, the intrapleural pressure returns to its resting level
Transpulmonary “transmural”
Pressure
The pressure across the lung wall.
It is the difference between intrapulmonary and intrapleural pressure.
It keeps the lung against chest wall
Change in lung volume parallel changes in thoracic volume during inspiration & expiration.
The Alveoli
Air sacs - Honeycomb-like clusters
~ 300 million in the two lungs
25-50 mm in diameter
Large surface area (60–80 m 2 ) for diffusion.
Each alveolus: only 1 thin cell layer “airblood barrier = 0.3µm = 1/100 th hair width”.
Total air barrier is 2 cells across (2 m m)
(alveolar cell and capillary endothelial cell).
The Alveolar Cells
1)
2)
alveoli are lined by two types of epithelial cells
Type I pneumocytes structural cells.
Thin squamous epithelial cells
95-97% (gas exchange)
Type II granular pneumocytes
Round or cup-like secretary cells
Secrete pulmonary surfactant
Reabsorb Na + and H within alveoli”
2
O “prevent buildup of fluid
The Alveolar Cells
The alveoli contain pulmonary alveolar macrophages (PAMs)