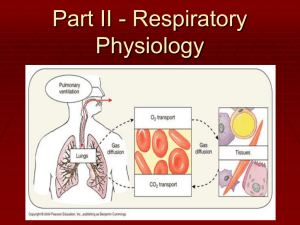
One final point about lung ventilation
advertisement
A 23-year old male comes to the ER with multiple stab wounds and extreme difficulty in breathing. Shortly after arriving to the ER the patient loses consciousness. The ER doctor notes a large stab wound in the right third intercostal space. Why was the patient having difficulty breathing and eventually lost consciousness? What is the clinical term for this condition? Can the diaphragm and accessory ribcage muscles still increase intraplueral VOLUME? What about changes in intraplueral pressure? Physiologically, why does this condition lead to ineffective lung ventilation? The anatomy between the chest wall and the surface of the lungs is crucial for effective lung ventilation. The chest wall is lined with a thin layer of tissue called the PARIETAL PLEURA. Between the parietal pleura and the lung surface is a thin layer of fluid called INTRAPLEURAL FLUID. The intrapleural fluid creates stickiness between the parietal pleura and the lungs (via surface tension). This stickiness makes the lungs move together with the ribcage and the diaphragm; thus allowing the Alveolar Pressure to be effectively altered by diaphragm and ribcage movements! Pneumothorax is a clinically important trauma in which air enters the space between the lungs and the pleura and breaks the surface tension between them. This GREATLY reduces the ability of the diaphragm and other muscles to alter Alveolar Pressure because the lungs no longer move in unison with the movements generated by these muscles. Because changing Alveolar Pressure is responsible for bulk flow of air into and out of the lungs, a drastic reduction in the ability to alter Alveolar pressure will result in ineffective lung ventilation!