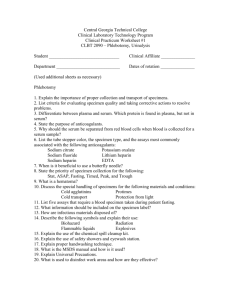
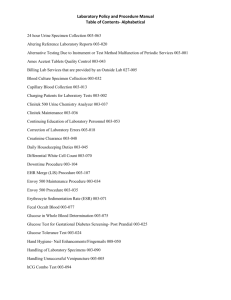
Training Curriculum of Laboratory Standards for Primary
advertisement

Training Curriculum of Laboratory Standards for Primary Health Care Clinics in Iraq June 2013 List of Contents List of contents List of abbreviations Introduction Part One: Trainers guide How to use the manual Structure of the training course Approaches to training and learning Part Two: Training modules Module1: Introduction, Setting up a primary health care laboratory, and safety in the laboratory Session1: Introduction and Setting up a primary health care laboratory Session 2: Safety in the laboratory Module 2: Hematology Session 1: Collection and handling of blood and automated blood count techniques Session 2: Manual techniques Module 3: Serology Session 1: RPR Test, TPHA Test, Widel Test, and Rose Bengal Test Session 2: CRP Test, ASO latex slide agglutination Test, RF, Toxoplasmosis Test, Infectious mononucleosis Test, Rota Virus Latex Test, and Pregnant Test Module 4: Bacteriology Session 1: General urine examination and general stool examination Session 2: Urine culture, throat swab, and nasal swab Session 3: Smart tests, preparation of media and staining smears Module 5: Parasitology and biochemistry Session 1: Parasitology Session 2: Biochemistry Annex 1 References 1 2 5 6 7 8 9 39 40 41 45 60 61 88 119 120 137 156 157 186 211 233 234 243 274 284 Page | 2 Acronyms AAFB AIDS ALP ALT AST BHSP CRP CSF CV DNA EDTA ELISA ESR GIT Hb HCG Hct Hi HiCN HIV IDDM Ig IHA IU KIA LDH LPS MAC MCH MCV MIU MoH MPV MPXI MRSA NIDDM PCV PDW PHC PPE R Acid and Alcohol Fast Bacilli Acquired Immune Deficiency Syndrome Alkaline Phosphatase Alanine Aminotransferase Aspartate Aminotransferase Basic Health Services Package C- Reactive Protein Cerebro-Spinal Fluid Coefficient of Variation Deoxyribonucleic Acid Ethylenediaminetetraacetic Acid Enzyme-Linked Immunosorbent Assay Erythrocyte Sedimentation Rate Gastro Intestinal Tract Hemoglobin Human Chorionic Gonadotropin Hematocrit Meth hemoglobin Hemiglobincyanide Human Immune Virus Insulin Dependent Diabetes Miletus Immunoglobulin Indirect Haemogglutination International Unit Klinger Iron Agar Low Density Lipids Lipopolysaccharides MacConky Mean Corpuscular Hemoglobin Mean Corpuscular Volume Motility-Indole-Urase Ministry of Health Mean Platelet Volume Mean Peroxidase Activity Index Methicillin Resistant Staph Aurous Non-Insulin Dependent Diabetes Mellitus Packed Cell Volume Platelet Distribution Width Primary Health Care Personal Protective Equipment Reactive Page | 3 RBCs RDW RF RNA RPM RPR SD SHb SOPs SPA SR TCBS TNCC TPHA TSA URC USAID UTI VCA VDRL WBC XLD Red Blood Cells Red cell Distribution Width Rheumatoid Factor Ribonucleic Acid Round Per Minute Rapid Plasma Reagin Standards Deviation Sulphemoglobin Standard Operating Procedures Suprapubic Aspirate Strong Reactive Thiosulfate Citrate Bile Salts Total Nucleated Cell Count Treponema Pallidum Particle Agglutination Tryptic Soya Agar University Research Company United States Agency of International Development Urinary Tract Infection Viral Structural Antigens Venereal Disease Research Laboratory White Blood Cells Xylose Lysine Desoxycholate Page | 4 Introduction The Iraqi Ministry of Health (MoH) is undergoing health reform and moving forward with reorganizing and stabilizing its health services. Ensuring access to routine, high quality, and equitable healthcare has emerged as a critical need, and the Government of Iraq (GoI) is responding with vigor and commitment to improving the quality of primary health care (PHC) services. To assist with these efforts, USAID awarded University Research Co. LLC (URC) the four-year Primary Health Care Project in Iraq (USAID/PHCPI) to support the MoH in achieving its goal of improving the quality of care for all Iraqis. The project aims to strengthen health sector capacity to provide essential PHC services and expand availability of such services throughout the country, with increasing coverage for vulnerable and at-risk populations, such as children under five, women, and internally displaced persons. The "Laboratory Standard Operating Procedures," often called the "Methods," discusses how the experiment occurred. Documenting the procedures of the laboratory experiment is important not only so that others can repeat the results but also so that you can replicate the work later, if the need arises. Historically, laboratory procedures have been written as firstperson narratives as opposed to second-person sets of instructions. Achieving a proper depth in laboratory procedures is challenging. In general, adequate information should be given in order to let the staff able to do the procedure. For that reason, details that will affect the outcome are included. The Basic Health Services Package for Iraq was considered in developing this guideline as all the SOPs for the investigations are listed in the BHSP. Page | 5 Part 0ne Trainer’s Guide Page | 6 Part I: Trainer’s Guide This training curriculum is a guide to assist trainers in improving health care by training health professionals by applying laboratory standards in primary health care centers Materials in this document are designed for training service providers who work at a variety of health facilities in Iraq. The modules can be used to train health professionals, physicians and other health workers in group training or, with adaptation, as a basis of individualized or self-directed learning. Trainers implementing this course should be thoroughly familiar with the guideline. The trainers need to have a positive attitude about the participants and their training work. Training may be implemented either off-site or on-site. In off-site training, a group of participants come together from several health facilities and then return to apply what has been learned. Off-site training may be the most appropriate way to reach individuals from many small sites. On-site training refers to training held in a health facility team where the participants work. Both types of training can be very effective. When training is conducted offsite, it may be more difficult to observe actual clinical settings. On the other hand, when training takes place on-site, there may be interruptions due to participants being called away for other responsibilities. How to Use the Manual This manual is designed as a working instrument for trainers and facilitators. The module schedule contains a condensed summary of the contents organized in units and is meant as a check list for the facilitator/s before and during the course. The time indicated for each unit is an average time span based on experience, and can vary according to the composition and dynamics of each respective group. The manual is divided into two parts. The first part is an introduction to the training course giving an overview over the rationale, objectives, and target groups for the course. It includes the present section on recommendations on how to use the manual, introducing the structure, training methods and course schedule. It also contains information on how to organize a workshop / training course and concludes with some recommendations on the limitations of the document and how to deal with them. The second part presents the actual training contents, methods, didactic materials and additional literature recommended for each content area, organized/compiled in the different modules of the program. Every training course starts with the introduction of participants and team presenting the course objectives, contents, methods and program and allowing participants to express their expectations and fears. The course content is presented according to three broad content areas (modules), subdivided into different sessions: Page | 7 Overall learning objectives: states the objectives to be achieved at the end of the module in terms of knowledge, skills and competence. Schedule: gives an overview over the time span, methods, materials and recommended content for each session / topic and states the specific objectives of each session. Sessions: are subdivisions/sessions of the module that follow a logical flow to develop the content of the module. Specific objectives of the sessions: relate to the content and the expected level of competence to be achieved and can also be used as basis for the development of exam questions. Background informationfor the facilitator: includes background information important for the facilitator to develop the content of the module, necessary and recommended definitions, concepts, theory and its applications. Exercises: describe practical applications of the theory and are meant to facilitate the learning process through experiential approaches: role plays, games, etc. (see list of exercises). Handouts: are the essential documentation for the participants about the content of the session / module stating the objectives, listing the key words, developing the concept / theory of the content, and giving recommendations for further reading. References: additionally recommended literature, articles and books, which are related to the content of the module. Structure of the Training Course The training course has been planned as a three days course. However, it is also possible to shorten the course due to limited time and / or to select modules according to learning objectives and needs. As well the time can be expanded in order to deal more in depth with the content and allow for more exercises, practical, field work. The time frame of the training course consists of six working hours per day. These hours are divided into two morning and two afternoon sessions. Each session normally has duration of 2 hours. The number of course trainers/ facilitators can range from one to two per course according to the requirements. Also, for special topics, external resource persons should be asked to lecture and work with the group in their respective areas of expertise. The trainee facilitator ratio should be 15 to one, a ratio of 20 or 25 to one still being acceptable. The total number of participants should not exceed 25. The course structure and training methods not only allow for the development of knowledge, skills, competence and change of attitudes of the participants. The course concept is also Page | 8 designed to be put into practice by participants after the training during their work or by organizing their own training courses. Approaches to Training and Learning The training course outlined in this document is based on adult learning principles, competency-based training and performance improvement. Selected elements of the strategies that guided the development of this material and should guide its implementation and use are listed below. How people learn best People learn best when the following conditions are met: Participants are motivated and not anxious, know what is expected of them and treated with respect Information and skills are interesting, exciting, meaningful, and build on what participants already know, encourage problem-solving and reasoning Experiences are organized, logical, practical, include a variety of methods, and protocols and procedures are available New learning experiences are relevant to work and training needs of participants, and are applied immediately Training involves every participant in active practice and participants share responsibility for learning Training is a team activity, including trainers and co-trainers, providing participants with a variety of experiences and limiting trainer’s biases The trainer acts as a facilitator of the learning process rather than a teacher who “spoon feeds” the learner The role and responsibilities of the trainers/facilitators and those of the participants/learners are clearly defined with: o The facilitators responsible for providing the learners with the necessary opportunities to acquire the knowledge and skills necessary to perform the tasks for which they are being trained o The facilitators responsible for providing the learners with the necessary opportunities to be exposed to the attitudes necessary to implement the acquired skills in a systematic manner and initiate the process of internalizing these attitudes o The learner remains responsible for her/his learning The transactional relationships between the learners and the facilitators are at the level of adult to adult characterized by mutual respect and support Trainers are knowledgeable and competent in the subject matter and skills, use a variety of training methods, pay attention to individual participants’ concerns, and provide motivation through feedback and reinforcement Page | 9 Participants must be selected according to specific criteria, such as the relevance of the training content to the job expectations/tasks Participants must have the necessary prerequisite level to enable them to benefit from the learning experience Feedback is immediate and focused on behavior that the participants can control Assessment of learning and skills is based on objectives that the participants understand Knowledge, skills and attitudes This course aims to improve health care by changing health workers’ knowledge, skills and attitudes. Knowledge includes the facts that the participants need to know to perform their jobs. Tips on increasing knowledge through training Start with what the participants already know or have experienced Use a variety of educational resources, including participatory activities that require participants to use their knowledge Use learning aids Review and summarize often Assess knowledge to verify learning Skills include the specific tasks that participants need to be able to perform. Tips on increasing skills through training Describe the skill Provide protocols and procedures Demonstrate the skill Have participants demonstrate the skill Verify that each skill is practiced correctly Assess skill by observation using a checklist Attitudes affect behaviors, such as whether learned skills are applied and interactions with clients. Page | 10 Tips on changing attitudes and behavior through training Provide information and examples Include direct experience Invite discussion of values, concerns and experience Use role plays and brainstorming Model positive attitudes Assess changes in attitude by observing behavior Methods The training will use a participatory and “hands on” approach where the role of the trainers is to facilitate learning by the participants. The responsibility for learning remains with the participants. Participants learn more and stay engaged in learning activities when they play an active role in their learning and a variety of training methods are used. The following methods are recommended in the curriculum/modules. Selected Training Methods Brainstorming Case study Clinical session Demonstration Discussion Field visits Plenary group exercises Group assignments Individual assignments Individual exercises Interview Lecture-Discussion Mini-lecture Observations Pairs exercises Presentation Questions and answers Research Return demonstration Role play Self-directed activities Small group discussion Simulation Small group exercises Summary Survey Team building exercises Page | 11 In each module or session This document contains an outline of a training plan for each of the key areas of content. Each module contains the following sections: Front page with a module number, module objectives, module content by session and an estimated duration for the module. Session plans covering the various content areas. Each session contains the following sections: Trainer Preparation: This section lists the specific preparations that trainers should make for the session. Preparations for every session include: Making sure the room is properly arranged Ensuring that markers and flip chart or a writing board with chalk or markers are available Reviewing the training plan Reviewing steps for the methods used in the training session Ensuring that the resources needed to facilitate the learning process are available including copying materials that participants need Methods and Activities: This section lists the methods and activities that are used in the module. General instructions for methods that are frequently used are included in this introductory material. Instructions for participatory activities are included in the training plan. Resources: The relevant reference materials/handouts and other resources needed are listed here. Evaluation/assessment: Evaluation methods for the knowledge or skills included are listed. Questionnaires and skills checklists are included where needed. Estimated Time: The time that each session/module will require depends upon the particular group of participants, the amount of time available and other constraints. The module gives a general time range to allow for flexible scheduling. Training Plan: This section gives the specific learning objectives or purpose of a session, the key ”must know” content, and the appropriate training methods and activities for each objective. All modules include one or more activities that give participants structured, participatory practice with the content of the module. Handouts: When specific activities require handouts, these are included after the training plan and should be copied before the session in which they will be used Page | 12 Skills Checklists: Each session that includes skills objectives includes a skills assessment checklist. The checklist is used by the trainer to evaluate the participant’s skill based on observation of the specific steps included in the skill. The skills checklists are also used by each participant to assess their performance and take charge of their own learning. They can also be used by other participants for peer assessment. It is recommended that these checklists not only be used during training to assess the acquisition of skills, but also for post training evaluation and supervision. Note: There are various possible formats for modules and sessions. Provided the necessary information is included for the trainer to use, the selection of format will depend on how comfortable the trainers are in using it. Methods:Instructions for methods used frequently in this training course are included here. Activities for specific methods are included with the sessions where they are used. Mini-lecture Trainer makes a short (5 to 15minutes) presentation using the materials available. Minilectures are used to provide information and knowledge. They insure that all participants have an adequate level of information and insure standardization and uniformity of this information. Mini-lectures should be kept short and should be followed by questions and answers for clarification to enable participants to better understand the content of the session/module and clarify issues, and questions and answers for evaluation to ensure comprehension. Questions and Answers (Q&A) Questions and answers sessions are used to recall information or elicit participants’ knowledge (in introductory sessions in order to assess training needs), for clarification (to ensure that participants understand information/content), presentation of information (to elicit information that participants may already know) and evaluation (to assess acquisition of knowledge and fill gaps in participants’ knowledge). Steps for Questions and Answers for clarification 1. 2. 3. 4. Trainer asks participants if they have questions If a participant has a question, trainer asks another participant to answer If the participant’s answer is correct and complete, trainer reinforces If the participant’s answer is incorrect and/or incomplete, trainer may ask questions that lead the participant to a more correct answer or ask another participant to answer 5. If the answer is still incorrect and/or incomplete after two or three trials, trainer corrects and/or completes and informs the participants where to find the information 6. If there are no questions, trainer asks questions to verify knowledge and follows the same steps (3, 4, 5) Page | 13 Steps for Questions and Answers to elicit information from participant (s) 1. Trainer asks participants questions 2. If a participant’s answer is correct and complete, trainer reinforces 3. If the participant’s answer is incorrect and/or incomplete, trainer may ask questions that lead the participant to a more correct answer or ask another participant to answer 4. If the answer is still incorrect and/or incomplete after two or three trials, trainer corrects and/or completes and informs the participants where to find the information Brainstorming Brainstorming is an excellent way to find out what participants already know and gaps in their knowledge. Brainstorming brings participants experience into the classroom and lets the participants know that their experience is valuable. Brainstorming is also a very effective way for problem solving. A brainstorming session should always end with a summary. Steps for brainstorming 1. Trainer asks an open-ended question 2. Participants shout out their answers or ideas: Until no more ideas are generated, or at least every participant has a chance to contribute or time allocated has run out No ideas are discarded criticized or analyzed, but clarifying questions can be asked 3. Trainer records ideas on newsprint or in another format where all can see them How to Use the Manual This manual is designed as a working instrument for trainers and facilitators. The module schedule contains a condensed summary of the contents organized in units and is meant as a checklist for the facilitator/s before and during the course. The time indicated for each unit is an average time span based on experience, and can vary according to the composition and dynamics of each respective group. The manual is divided into two parts. The first part is an introduction to the training course giving an overview over the rationale, objectives, and target groups for the course. It includes the present section on recommendations on how to use the manual, introducing the structure, training methods and course schedule. It also contains information on how to organize a workshop / training course and concludes with some recommendations on the limitations of the document and how to deal with them. Page | 14 The second part presents the actual training contents, methods, didactic materials and additional literature recommended for each content area, organized/compiled in the different modules of the program. Every training course starts with the introduction of participants and team presenting the course objectives, contents, methods and program and allowing participants to express their expectations and fears. The course content is presented according to three broad content areas (modules), subdivided into different sessions: Overall learning objectives: states the objectives to be achieved at the end of the module in terms of knowledge, skills and competence. Schedule: gives an overview over the time span, methods, materials and recommended content for each session / topic and states the specific objectives of each session. Sessions: are subdivisions/sessions of the module that follow a logical flow to develop the content of the module. Specific objectives of the sessions: relate to the content and the expected level of competence to be achieved and can also be used as basis for the development of exam questions. Background information for the facilitator: includes background information important for the facilitator to develop the content of the module, necessary and recommended definitions, concepts, theory and its applications. Exercises: describe practical applications of the theory and are meant to facilitate the learning process through experiential approaches – role-plays, games, etc.… (See list of exercises). Handouts: are the essential documentation for the participants about the content of the session / module stating the objectives, listing the key words, developing the concept / theory of the content, and giving recommendations for further reading. References: additionally recommended literature, articles and books, which are related to the content of the module. Structure of the Training Course The training course has been planned as a three days course. It is possible to shorten the course due to limited time and / or to select modules according to learning objectives and needs. The time can also be expanded in order to deal more in depth with the content and allow for more exercises, practical, fieldwork. Page | 15 The time frame of the training course consists of six working hours per day. These hours are divided into two mornings and two afternoon sessions. Each session normally has duration of two hours. The number of course trainers/ facilitators can range from one to two per course according to the requirements. Also, for special topics, external resource persons should be asked to lecture and work with the group in their respective areas of expertise. The trainee facilitator ratio should be 15 to one, a ratio of 20 or 25 to one still being acceptable. The total number of participants should not exceed 25. The course structure and training methods not only allow for the development of knowledge, skills, competence and change of attitudes of the participants. The course concept is designed for participants to put into practice after the training during their work or by organizing their own training courses. Approaches to Training and Learning The training course outlined in this document is based on adult learning principles, competency-based training and performance improvement. Selected elements of the strategies that guided the development of this material and should guide its implementation and use are listed below. How People Learn Best People learn best when the following conditions are met: Participants are motivated and not anxious, know what is expected of them and treated with respect Information and skills are interesting, exciting, meaningful, and build on what participants already know, encourage problem-solving and reasoning Experiences are organized, logical, practical, include a variety of methods, and protocols and procedures are available New learning experiences are relevant to work and training needs of participants, and are applied immediately Training involves every participant in active practice and participants share responsibility for learning Training is a team activity, including trainers and co-trainers, providing participants with a variety of experiences and limiting trainer’s biases The trainer acts as a facilitator of the learning process rather than a teacher who “spoon feeds” the learner Page | 16 The role and responsibilities of the trainers/facilitators and those of the participants/learners are clearly defined with: o The facilitators responsible for providing the learners with the necessary opportunities to acquire the knowledge and skills necessary to perform the tasks for which they are being trained o The facilitators responsible for providing the learners with the necessary opportunities to be exposed to the attitudes necessary to implement the acquired skills in a systematic manner and initiate the process of internalizing these attitudes o The learner remains responsible for her/his learning The transactional relationships between the learners and the facilitators are at the level of adult to adult characterized by mutual respect and support. Trainers are knowledgeable and competent in the subject matter and skills, use a variety of training methods, pay attention to individual participants’ concerns, and provide motivation through feedback and reinforcement Participants must be selected according to specific criteria, such as the relevance of the training content to the job expectations/tasks Participants must have the necessary prerequisite level to enable them to benefit from the learning experience Feedback is immediate and focused on behavior that the participants can control Assessment of learning and skills is based on objectives that the participants understand Knowledge, Skills and Attitudes This course aims to improve health care by changing health workers’ knowledge, skills and attitudes. Knowledge includes the facts that the participants need to know to perform their jobs. Tips on increasing knowledge through training Start with what the participants already know or have experienced Use a variety of educational resources, including participatory activities that require participants to use their knowledge Use learning aids Review and summarize often Assess knowledge to verify learning Page | 17 Skills include the specific tasks that participants need to be able to perform. Tips on increasing skills through training Describe the skill Provide protocols and procedures Demonstrate the skill Have participants demonstrate the skill Verify that each skill is practiced correctly Assess skill by observation using a checklist Attitudes affect behaviors, such as whether learned skills are applied and interactions with clients. Tips on changing attitudes and behavior through training Provide information and examples Include direct experience Invite discussion of values, concerns and experience Use role plays and brainstorming Model positive attitudes Assess changes in attitude by observing behavior Methods The training will use a participatory and “hands on” approach where the role of the trainers is to facilitate learning by the participants. The responsibility for learning remains with the participants. Participants learn more and stay engaged in learning activities when they play an active role in their learning and a variety of training methods are used. The following methods are recommended in the curriculum/modules. Page | 18 Selected Training Methods Brainstorming Case study Clinical session Demonstration Discussion Field visits Plenary group exercises Group assignments Individual assignments Individual exercises Interview Lecture-Discussion Mini-lecture Observations Pairs exercises Presentation Questions and answers Research Return demonstration Role play Self-directed activities Small group discussion Simulation Small group exercises Summary Survey Team building exercises In each Module or Session This document contains an outline of a training plan for each of the key areas of content. Each module contains the following sections: Front page with a module number, module objectives, module content by session and an estimated duration for the module. Session plans covering the various content areas. Each session contains the following sections: Trainer Preparation: This section lists the specific preparations that trainers should make for the session. Preparations for every session include: Making sure the room is properly arranged Ensuring that markers and flip chart or a writing board with chalk or markers are available Reviewing the training plan Reviewing steps for the methods used in the training session Ensuring that the resources needed to facilitate the learning process are available including copying materials that participants need Methods and Activities: This section lists the methods and activities that are used in the module. General instructions for methods that are frequently used are included in this introductory material. Instructions for participatory activities are included in the training plan. Resources: The relevant reference materials/handouts and other resources needed are listed here. 0|Page Evaluation/assessment: Evaluation methods for the knowledge or skills included are listed. Questionnaires and skills checklists are included where needed. Estimated Time: The time that each session/module will require depends upon the particular group of participants, the amount of time available and other constraints. The module gives a general time range to allow for flexible scheduling. Training Plan: This section gives the specific learning objectives or purpose of a session, the key “must know” content, and the appropriate training methods and activities for each objective. All modules include one or more activities that give participants structured, participatory practice with the content of the module. Handouts: When specific activities require handouts, these are included after the training plan and should be copied before the session in which they will be used. Skills Checklists: Each session that includes skills objectives includes a skills assessment checklist. The checklist is used by the trainer to evaluate the participant’s skill based on observation of the specific steps included in the skill. Each participant is to use the skills checklists to assess their performance and to take charge of their own learning. Other participants can also use the skill checklists for a peer assessment. It is recommended that these checklists should be used for both during training to assess the acquisition of skills and also for post-training evaluation and supervision. Note: There are various possible formats for modules and sessions. The format selected will depend on how the necessary information provided and the how comfortable the trainers are in using it. Methods: Instructions for methods used frequently in this training course are included here. Activities for specific methods are included with the sessions where they are used. Mini-lecture Trainer makes a short (5 to 15 minutes) presentation using the materials available. Minilectures are used to provide information and knowledge. They insure that all participants have an adequate level of information and insure standardization and uniformity of this information. Mini-lectures should be kept short and should be followed by questions and answers for clarification to enable participants to better understand the content of the session/module and clarify issues, and questions and answers for evaluation to ensure comprehension. 1|Page Questions and Answers (Q&A) Q&A sessions are used to recall information or elicit participants’ knowledge (in introductory sessions in order to assess training needs), for clarification (to ensure that participants understand information/content), presentation of information (to elicit information that participants may already know) and evaluation (to assess acquisition of knowledge and fill gaps in participants’ knowledge). Steps for Questions and Answers for Clarification 1. 2. 3. 4. Trainer asks participants if they have questions If a participant has a question, trainer asks another participant to answer If the participant’s answer is correct and complete, trainer reinforces If the participant’s answer is incorrect and/or incomplete, trainer may ask questions that lead the participant to a more correct answer or ask another participant to answer 5. If the answer is still incorrect and/or incomplete after two or three trials, trainer corrects and/or completes and informs the participants where to find the information 6. If there are no questions, trainer asks questions to verify knowledge and follows the same steps (3, 4, 5) Steps for Questions and Answers to Elicit Information from Participant(s) 1. Trainer asks participants questions 2. If a participant’s answer is correct and complete, trainer reinforces 3. If the participant’s answer is incorrect and/or incomplete, trainer may ask questions that lead the participant to a more correct answer or ask another participant to answer 4. If the answer is still incorrect and/or incomplete after two or three trials, trainer corrects and/or completes and informs the participants where to find the information Brainstorming Brainstorming is an excellent way to find out what participants already know and the gaps in their knowledge. Brainstorming brings participants experience into the classroom and lets the participants know that their experience is valuable. Brainstorming is also a very effective way for problem solving. A brainstorming session should always end with a summary. 2|Page Steps for Brainstorming 1. Trainer asks an open-ended question 2. Participants shout out their answers or ideas: Until no more ideas are generated, or at least every participant has a chance to contribute or the time allocated has run out No ideas are discarded, criticized or analyzed, but clarifying questions can be asked 3. Trainer records ideas on newsprint or in another format where all can see them 4. Trainer leads a discussion of each of the ideas generated 5. Trainer clearly marks ideas that are agreed upon 6. Trainer summarizes or asks participants to summarize points of agreement 7. Trainer moves to the next question only after finishing discussion of previous question 8. Ideas generated in brainstorming can be used for summarizing, as input to group exercises, and to relate content to participant experience Case Study A case study is method of training. Data and information about a case, preferably a real one or based on one, is presented to the participants for review and analysis. It includes specific questions to be answered. Case studies are an effective way to allow participants to practice using information to solve problem, the highest level of knowledge objective. They are also effective in providing participants opportunities to explore their attitudes and confront/compare them with other participants and trainers’ attitudes. Moreover, case studies allow for the identification of gaps in knowledge. Participants, individually or in small groups are asked to study the case and prepare responses to the questions. The responses are then processed. During the processing the trainer must encourage and ensure that all participants get a chance to provide inputs. Processing can be done using questions and answers and/or discussion. The questions must be answered in an orderly manner in the sense that each question must be answered fully and the inputs summarized before moving to the next question. Answer key must be given to the participants after the processing of the case study. Case studies can be presented in different format. They can be based on the presentation of a real patient, the files of a patient, a written description of a case, an illustration such as a photograph or slides of a case, or a video. This method is not used in this curriculum but trainers can develop case studies based on local conditions/data as additional exercises if time permits. 3|Page Discussion Discussion is indicated when the outcome is not predetermined in advance and is “still negotiable.” Therefore, using discussion to provide “scientific” knowledge/information or a decision that has already been made and not to be changed can lead to frustration. Discussion is recommended for plenary or small groups to explore attitudes, values and opinions. It can confront/compare different options of “doing things” ensuring that the “why” is covered. The trainer’s role during the discussion is to facilitate the process, and ensure that the discussion remains “on track” and that every participant gets a chance to contribute. When small groups do not have the same assignment/topic to discuss, each group presents their output(s) and discussion follows immediately after the presentation before moving to the next group. Time management is essential to ensure that no groups are “short changed” and has ample time for the presentation and discussion. If all the groups have the same assignment, all groups present before discussion takes place. Only clarification questions are allowed during the presentation. Processing the output(s) must focus on the points of agreement before moving to the differences. If time does not allow for all groups to present, one group can present and the other groups complete from their own group’s output before the discussion starts. Every discussion must be followed by a summary. Demonstration Demonstration is a very effective way to facilitate learning of a skill or initiation of the development of an attitude. The facilitator should use this method to show the skill(s) and/or the attitude(s) addressing more than one sense at a time. Often a demonstration can effectively replace a presentation provided the facilitator explains as s/he is doing. A demonstration should always be followed by a Q&A clarification session before the learners are required to do a return demonstration. Steps for a Demonstration 1. 2. 3. 4. Trainer assembles resources needed for the demonstration Trainer ensures that participants are ready, can hear and see Trainer explains what s/he is going to do Trainer instructs participants on what is expected of them (e.g. to observe closely, to take notes if appropriate, to use the skills checklist when appropriate etc.) 4|Page 5. 6. To prepare for the Q&A, and Because they are required to do return demonstration(s) for practice Trainer demonstrates while explaining the skill(s)/attitude necessary for each step of the procedure being demonstrated Trainer conducts a Q&A for clarification at the end of the demonstration Return Demonstration Return demonstrations provide the learners the opportunity to practice the skills necessary to perform the procedures they are being trained on. The trainer must ensure that each learner/participant has the opportunity to practice enough times to reach a preset minimum acceptable level of performance. Steps for a Return Demonstration 1. Trainer reminds participants of what is expected of them: To practice the procedure/skills To observe when others are practicing to be able to ask for clarification To observe when others are practicing to be able to provide feedback and peer evaluation 2. Trainer divides participants into small groups, if more than one workstation. (Note: each workstation requires at least one facilitator/trainer). 3. Participants take turns practicing the procedure/skills 4. Trainer ensures that all participants can hear and see 5. While each participant is practicing trainer can provide guidance as necessary provided it does not interfere with the process and confuse the participant 6. After each participant, trainer solicits feedback from other participants 7. After feedback from other participants, trainer reinforces what is correct and corrects and/or completes feedback 8. Each participant needs to practice more than once or until control of the skill, as time permits 9. If participant(s) need more than time permits, trainer arranges for additional practice opportunities Simulation/Simulated Practice A simulated practice is an effective method to allow participants to practice procedures/skills in a specific environment. It recreates as closely as possible the “real world” without the stress involved in practicing procedures/skills that they do not control yet in the field. It is recommended to have participants practice on models before they do perform the procedure/ use the skill in the work place. During a simulation the participant practices tasks that are part of her/his actual role in the workplace or that s/he will perform in the job s/he is being trained for. 5|Page Use the same steps as for a demonstration/return demonstration practice. Role – play Role-plays are an effective method to practice procedures/skills in the training room. They are especially effective to practice procedures/skills that deal with human interactions such as health education and counseling sessions. They are also very effective when the learning objective deal with attitudes. In a role play participants “play roles” that are not necessarily their roles in the “real world.” Often they are asked to play the role of someone they would be dealing with. In this case it is called “role reversal” or “reverse role play”. This allows the participants to explore and discover how other perceive/live the interaction. A role play must always be processed to analyze the lessons learned. Summary Every time a training method allows for inputs through exchanges between the trainer(s) and the participants and between the participants themselves; it must be followed by a summary session to “tie up the loose ends” and provide the participants with clear answers. If this does not happen, there is the likelihood that the participants will forget the “correct” answers. The trainer should facilitate a summary to ensure that there are “no loose ends.” If time permits, it is recommended to use the summary for evaluation. In this case, the trainer can use the Q&A method. Steps for a Summary for Evaluation 1. Trainer asks a participant to summarize 2. Trainers reinforces if the summary is correct/complete 3. Trainer asks another participant to correct/complete if the summary is incorrect/incomplete 4. Trainer repeats steps 2 and 3 5. Trainer corrects/completes if after 2 or 3 trials the summary is still incorrect/incomplete. Discussion Lecture Discussion Lecture is introducing scientific material to the listeners. It involves them in the discussion and exchanging viewpoints, raising questions and answering them. This leads to enriching the training process and increasing the chances of its success. The main difference between it and the short lecture is that the trainees are given the chance for questioning and discussion during the lecturing. 6|Page Discussion lecture uses the principles of the lecture and discussion together in applying this method. Privileges of the discussion lecture: 1. Drawing the trainees attention because it is a method of communication between the two sides in more than one direction 2. Increasing the interaction between the trainees and trainer and among trainees themselves 3. Allowing the exchange of viewpoints 4. Operating according to the rules and principles of seniors education 5. Allowing the provision of information and decision taking in the same session Faults of discussion lecture: 1. Discussion may lead to the deviation from the basic subject and this neglecting the fundamental points of the subjects 2. It cannot be used in gaining the skills 3. It may lead to open the door of the discussion about information and firm decisions that cannot be changed and this leads to disappointment Evaluation Evaluation of learning and training objectives Evaluation or assessment of learning and of training objectives allows trainers, program managers and participants to know how successful a training program has been. Ongoing evaluation and assessment allows trainers to identify gaps in learning and to fill those gaps. Evaluation also assists in revising learning experiences for later trainings. Many strategies can be used to evaluate learning. Some of the most useful methods include: Knowledge assessments: Written or oral questions that require participants to recall, analyze, synthesize, organize or apply information to solve a problem. The knowledge component of a skill objective should be assessed prior to beginning skill practice in a training room or clinical session. Questionnaires: Written exercises that assist trainers and participants to identify and fill gaps in knowledge. Questionnaires can be administered as self-assessments. In some situations, it may be 7|Page reasonable to have participants use course materials or to work together on questionnaires. Skill checklists: Observation of a participant performing a skill and assessment of the performance using a checklist. Simulated practice (using real items or models in a situation that is similar to actual practice) should ideally be assessed prior to beginning clinical practice with clients. The trainer and other participants should use the checklists to observe simulated (training room) performance and actual practice and provide feedback to help improve the performance. The checklists can also be used by the participant for self-assessment. During the training participants should be trained on how to use the checklists. They should also be encouraged to use them after the training to continue assessing their own performance and improving it. Additional techniques for evaluation include: projects, reports, daily reflection, on-site observation, field performance, and discussion. Each training module includes assessment of learning methods and tools: Q&A should be used to frequently identify gaps in knowledge and fill them. Questionnaires are included with every module and can be used for self-assessment. To use them as self-assessment, participants complete the questionnaire and then use any course materials to check their own answers. Trainers should work with participants filling out the questionnaires to make sure that all gaps in knowledge are filled before practicing and evaluating skills. When time permits, process responses in plenary to address any issues and fill the gaps in knowledge. At the end of this activity the answer key needs to be distributed to the participants. Skills Checklists are included for each of the skills that are included in this training curriculum. Participants can use the Skills Checklists as learning guides during practice sessions in training room or clinical sessions. To evaluate skills, trainers should generally observe participants three times with coaching as needed to ensure the skills are learned. Evaluation of the Participants Participants’ learning can be evaluated through different methods. This includes Q&A, synthesis of sessions done by selected participants, self-assessment following the micro-sessions, peer assessment through feedback provided by other participants following the micro-sessions and assessment of performance by facilitators. 8|Page Each participant will practice more than once, preferably three times. The curriculum is for use to plan, organize, conduct and evaluate the training through simulated microsessions. A checklist will be used both by participants for self and peer assessment, and by the facilitators. Videotaping the micro-sessions or at least significant segments of the micro-sessions and reviewing the taped segments after each session will enable the participants to assess their own progress in terms of acquisition of training/facilitation skills. This evaluation approach is time consuming, but is very effective in helping participants assess their own performance. It can also stabilize feedback received from their peers and the trainers/facilitators. Post – training evaluation of the learners must be conducted within three to six months after the end of the training. Further post – training evaluation and follow- up can be integrated into routine supervision. It is highly recommended to use the skills checklists used during the training for post – training evaluation and follow-up. Evaluation of the Training The “End of Training” evaluation can be done through a questionnaire (Form 1). The participants are asked to respond and express their opinions about various aspects of the workshop, such as organization, the process, the facilitation, and a general assessment. The “End of Module” evaluation can be done through a questionnaire (Form 2). The participants are asked to respond and express their opinions about various aspects of the module. This includes the relevance of the module objective to the course ones, the relevance of the content to the objectives, the adequacy of the content, the presentation of the content, the effectiveness of the methodology, the facilitation and the sequencing of the content. A confidence/satisfaction index can be calculated to determine how confident the learners feel that they acquired the knowledge and skills necessary to perform the tasks they have been trained for, and how committed they feel to using those skills to ensure the quality of the services they are to provide. The confidence index applies to the training objectives and acquisition of skills and knowledge and to the degree to which the participants feel that they able to apply what they have learned during the training. The satisfaction index applies to the organization and implementation of the training. The items are labeled in the form of statements followed by a scale 5 (Strongly Agree), 4 (Agree), 2 (Disagree), and 1 (Strongly Disagree). Five (5) represents the highest level of satisfaction/confidence (agreement with the statement) and one (1) represents the 9|Page lowest. The participants are asked to select the level that expressed their opinion best. A space for comments is provided after each statement. The confidence and satisfaction indices are calculated by multiplying the number of respondents by the correspondent coefficient in the scale, then adding the total. The total is multiplied by 100. The product is divided by the total number of respondents to the statement multiplied by 5. 60% represents the minimal acceptable level and 80% a very satisfactory level of performance. For example, if the total number of respondents is 19 and 7 of them selected 5 on the scale, 6 selected 4, 4 selected 2, and 2 selected 1, then the index will be (5x7)+(4x6)+(2x4)+(1x2) multiplied by 100, divided by (5X19). A 100% index would if the total number of respondents selected 5. In this case it would be 95. In this example the index is 72.63%. The training content and process are evaluated on a continuing basis through daily evaluations using methods such as “things liked the best” and “things liked the least” and/or “quick feedback” forms. The facilitators will use the results of this evaluation during their daily meeting to integrate the feedback and adapt the training to the participants needs. “Where Are We?” sessions will be conducted with the participants to assess the progress in content coverage and process towards reaching the training goals and learning objectives. Comments are analyzed and categorized. Only significant comments, those mentioned more than once and/or by more than one participant, are retained. The facilitators need to use the results of this evaluation during their daily meeting to integrate the feedback and adapt the training to the participants needs. Feedback and assessment of training experiences allows trainers and program managers to adapt training to better meet participants’ needs. Trainers can also assess their own performance in facilitating the learning experience of participants using a standardized “facilitation skills” checklist (Form 4). 10 | P a g e Form 1: END OF COURSE EVALUATION QUESTIONNAIRE TRAINING CENTER: DATE: COURSE TITLE: INSTRUCTIONS This evaluation will help adapt the course to your needs and to those of future participants. It is anonymous. Please respond freely and sincerely to each item. The items are labeled in the form of statements followed by a scale where: 5 = strong agree 4 = agree 2 = disagree 1 = strongly disagree Please circle the number that expresses your opinion; the difference between strongly agree and agree, and between strongly disagree and disagree are a matter of intensity. Add your comments in a specific and concise manner, in the space provided after each statement. If that is not sufficient feel free to use extra paper. If you select 2 or 1, make sure to suggest how to make the situation better, practical, and offer solutions. N.B: Course goals objectives and duration will vary based on the type of training conducted. Adapt the form to each specific course by including in it the relevant course items. 11 | P a g e COURSE GOALS The Course Achieved Its Goals 1. To provide the participants with the opportunities to acquire/update the knowledge and skills necessary to: 1.1 Play an effective role as a member of the Primary Health Care (PHC) Center team to improve the quality of care and services 5–4–2–1 Comments: 1.2 Use the team approach to solve problems at the PHC center level 5–4–2–1 Comments: 2. Provide the participants with opportunities to be exposed to and 5–4–2–1 initiate the development of attitudes favorable to the systematic use of the knowledge and skills acquired in team building and problem solving to improve the quality of care and services Comments: 12 | P a g e COURSE OBJECTIVES 1. The course helped me reach the stated objectives: 1.1 Apply the team approach principles to play an effective role as a member of the Model PHC Center service delivery team 5–4–2–1 Comments: 1.2 Use the team approach to implement the problem solving cycle to solve service delivery and management problems at the PHC Center level 5–4–2–1 Comments: 1.3 Explain the importance of being an effective team member of the Model PHC Center to improve the quality of care and services 5–4–2–1 Comments: 13 | P a g e 1.4 Explain the importance of using the team approach to implement the problem solving cycle to solve service delivery and management problems at the Model PHC center 5–4–2–1 Comments: 2. The course objectives are relevant to my job description / task I perform in my job: 5–4–2–1 Comments: 3. There is a logical sequence to the units that facilitates learning: 5 – 4 – 2 – 1 Comment: 14 | P a g e ORGANIZATION AND CONDUCT OF THE COURSE 1. Time of notification was adequate to prepare for the course 5–4–2–1 Comments: 2. Information provided about the course before arriving was adequate 5–4–2–1 Comments: 3. Transportation arrangements during the course were adequate (if 5 – 4 – 2 – 1 applicable) Comments: 4. Training site (Training Center) was adequate 5–4–2–1 15 | P a g e Comments: 5. The educational materials (including reference material) used were 5 – 4 – 2 – 1 adequate both in terms and quantity and quality in relation to the training objectives and content Comments: 16 | P a g e 6. The methodology and technique used to conduct the training were effective in assisting you to reach the course objectives 5–4–2–1 7. Clinic/ practice site, as applicable, was adequate 5–4–2–1 Comments: 8. Relationships between participants and course managers and support 5 – 4 – 2 – 1 staff were satisfactory Comments: 9. Relationships between participants and trainers were satisfactory and 5 – 4 – 2 – 1 beneficial to learning Comments: 10. Relationships between participants were satisfactory 5–4–2–1 Comments: 17 | P a g e 11. The organization of the course was adequate (Time, breaks, supplies, resource materials) 5–4–2–1 Comments: Additional comments: 18 | P a g e GENERAL ASSESSMENT 1. I can replicate this training in my future work 5–4–2–1 Comments: 2. I would recommend this training course to others 5–4–2–1 Why or Why Not? 3. The duration of the course (10 days) was adequate to reach all objectives and cover all necessary topics 5–4–2–1 Comments: General comments and suggestions to improve the course (Please be specific) 19 | P a g e Form 2: END OF MODULE EVALUATION QUESTIONNAIRE COURSE: DATE: MODULE NUMBER & TITLE: INSTRUCTIONS This evaluation is intended to solicit your opinions about the modules. Your feedback will help adapt the course to your needs and to those of future participants. It is anonymous. Please respond freely and sincerely to each item. The items are labeled in the form of statements followed by a scale where: 5 = strongly agree 4 = agree 2 = disagree 1 = strongly disagree Please circle the number that best expresses your opinion; the differences between strongly agree and agree, and between strongly disagree and disagree are a matter of intensity. Add your comments in a specific and concise manner in the space provided after each statement. If that space is not sufficient feel to use extra paper. If you select 2 or 1, make sure to write specific comments on how to improve the module. 20 | P a g e EVALUATION ITEMS 1. The module objectives are relevant to the course objectives 5–4–2–1 Comments: 2. The content / topics covered in the unit are relevant to the 5 – 4 – 2 – 1 objectives Comments: 3. The content / topics were adequate to help me achieve the 5 – 4 – 2 – 1 objectives Comments: 4. The content / topics were clear and well-presented Comments: 5–4–2–1 5. The training methods and activities were effective in facilitating 5 – 4 – 2 – 1 learning Comments: 21 | P a g e 6. The training methods and activities were conducted adequately to 5 – 4 – 2 – 1 facilitate learning Comments: 7. These are important topics that will enable me to better perform my 5 – 4 – 2 – 1 job Comments: (specify these points) 8. There is a logical sequence to the sessions and topics that facilitates 5 – 4 – 2 – 1 learning Comments: 9. There are certain topics that need further clarification Comments: (specify these points) 5–4–2–1 10. The training materials and resources provided were adequate Comments: 5–4–2–1 22 | P a g e 23 | P a g e 11. Training materials and resources were provided on time to facilitate 5 – 4 – 2 – 1 learning Comments: 12. The training materials and resources used were adequate to facilitate 5 – 4 – 2 – 1 my learning Comments: 13. The training site was adequate Comments: 5–4–2–1 14. The clinic/ practice site was adequate (if applicable) Comments: 5–4–2–1 General comments (if any not covered): 24 | P a g e Form 3: QUICK FEEDBACK FORM TRANING COURSE: DATE: LOCATION: MODULE NUMBER AND TITLE: SESSION NUMBER AND TITLE: INSTRUCTIONS This evaluation is anonymous. Please respond freely and sincerely to each item. The items are labeled in the form of statements followed by a scale where: 5 = strongly agree 4 = agree 2 = disagree 1 = strongly disagree Please circle the description that expresses your opinion best; the difference between strongly agree and agree, and between strongly disagree and disagree are a matter of intensity. Add your comments in a specific and concise manner, if you have any, in the space provided after each statement. If that space is not sufficient feel free to use extra paper. If you selected 2 or 1 please make sure to give comments (e.g. Why? Solutions?) 1. The session objectives are relevant to the tasks in the job description 5–4–2–1 Comments: 2. The methods/learning activities were adapted to the objectives 5–4–2–1 Comments: 25 | P a g e 3. The materials provided were adequate to cover all of the content 5–4–2–1 Comments: 4. The time allocated to the session was adequate to cover all the topics 5–4–2–1 Comments: 5. The facilitation (conduct of the session) helped reach the session 5 – 4 – 2 – 1 objectives Comments: 6. The content of the training was clearly presented 5–4–2–1 Comments: 7. The materials/resources were used in a way that helped me learn 5–4–2–1 Comments: 8. There are points of content that need further clarifications 5–4–2–1 (Specify what specific content areas) Other Comments: 26 | P a g e Form 4: TRAINING SKILLS CHECKLIST This checklist is used with the relevant curriculum to give feedback on the trainer’s performance. The checklist contains a list of items to be observed: If they are observed a check mark (√) is entered in the column observed under adequate or inadequate depending on the performance. Comments are entered in the appropriate column to clarify/specify what is observed or not observed. Is not observed a check mark (√) and comments are entered in the appropriate columns. The finding and comments are analyzed and discussed with the trainers supervised. Any immediate corrective action(s) taken and further action(s) needed must be entered in the spaces provided. The trainers supervised must be given an opportunity to comment and the comments must be entered in the appropriate space. The form must be dated and signed by the trainer and the supervisor. It is then filed in the trainer’s file for future follow-up and reference. Legend: A = Adequate NA = NOT adequate Items Observed A NO = NOT observed NA NO Comments 1.Planning of the session Relevant sessions plan selected from curriculum Organization conduct and evaluation of training in conformity with curriculum (based on observation during the session) 2.Organizing the session Arrive before beginning of session Ensure that all training resources are in place Ensure that equipment is in working condition Ensure that training site is set up in accordance with the requirements of 27 | P a g e the training objective (s) and methodology Prepared/rehearsed for the training (based on observation of mastery in conducting activities and using resources during training) Items Observed A NA NO Comments 3. Conducting the session 3.1 Introduction Introduce oneself - Name - Job - Experience relevant to topic Introduce/let team members introduce themselves Module: - Introduce topic - Present objective - Clarify topic and objectives - List sessions - Establish linkage with job/task Session - Introduce topic - Present objectives - Clarify topics and objectives - Establish linkage with module - Establish linkage with preceding session(s) - Explain methodology Present evaluation methodology State estimated duration 3.2 Facilitation skills Clarifying Make sure participants are ready before starting on any content item Make sure participants can hear: - Trainer - Other participants 28 | P a g e Make sure participants can see: - Writing - Illustrations/ educational aids - Trainer - Each other Make sure s/he look at participants Make sure s/he can hear participants Use appropriate educational material Summarize after each content topic item before moving to next topic Use examples relevant to objectives, content, and participants learning. Items Observed A NA NO Comments Ensuring Active Participation Ask participants questions Allow participants to ask questions Allow participants to question/discuss/make contributions Ensure that all participants contribute Provide participants with opportunities to practice Adapt to participants’ learning capability (speed, learning activities, use of educational material) Encourage participants through: - Listening - Letting participants complete their interventions - Not being judgmental - Maintaining cordial relationships with participants 29 | P a g e Mastering Training Conduct the learning activities as per session plan Use the training resources/ materials as per plan Cover content adequately (relevant, clear, concise, complete, concrete, credible, consistent and correct) Follow curriculum for learning/training activities Use content as per curriculum 1. Evaluating learning/training process Check that participants understand Check that participants learn skills Provide supportive feedback by: - Reinforcing the positive learning - Correcting any errors - Correcting any incomplete learning Listen to participants comment about one’s performance (without making it personal) Adapt one’s performance based on feedback from participants Allow participants to answer questions asked by the group. Additional comments or observations Analysis of findings 30 | P a g e Action (s) taken Further action (s) needed Trainer’s comments Trainer’s name & signature Supervisor’s name & signature Date: 31 | P a g e Part Two Training Modules 32 | P a g e Module One: Introduction, Setting up a primary health care laboratory, and safety in the laboratory Module Objectives: At the end of this module the participant will be able to: 1. Identify Setting up a primary health care laboratory 2. Explain safety in the laboratory Modules Sessions Session 1: : Introduction and Setting up a primary health care laboratory Session 2: safety in the laboratory Evaluation/ Assessment Questions and answers, participants’ summaries, trainer’s evaluation Estimated Training Time 3.30 hours 33 | P a g e Module 1 Session 1: Introduction and Setting up a primary health care laboratory Objectives At the end of this session participants will be able to: 1. Explain introduction about laboratory standards 2. Identify Setting up a primary health care laboratory Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Mini-lecture Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 50 minutes 34 | P a g e Session plan -1- 35 | P a g e Objectives 1.1.1. Explain introduction about laboratory standards Content 1.1.2.Identify Setting up a primary health care laboratory The "Laboratory Standard Operating Procedures," often called the "Methods," discusses how the experiment occurred Documenting the procedures of the laboratory experiment is important not only so that others can repeat the results but also so that you can replicate the work later, if the need arises Methodology Mini-lecture 25 minutes Mini-lecture Figure 1: Plan for a one room laboratory 25 minutes 36 | P a g e Setting up a primary health care laboratory A one room laboratory: Figure 1 sets out the possible arrangement of a peripheral medical laboratory attached to a health center. It shows a laboratory suitable for carrying out some or all of the techniques described in the manual. The plan is limited to one room, since often this is all the space that is available for the laboratory. The room should measure at least 5m X 6m. Figure 1: Plan for a one room laboratory Alternative plan for a one-room laboratory ( check figure2) 1: outpatient’s table; 2: hand-operated centrifuge; 3: microscopes; 4: hematology area; 5: colorimeter; 6: water bath ; 7: electric centrifuge; 8: syphilis serology and biochemistry area; 9: reagent refrigerator; 10: reagent shelf; 11: glassware shelf; 12: balance; 13: staining box; 14: area for examination of sputum specimens; 15: Bunsen burner; 16: sinks; 17: waste sink; 18: bed for patients; 19: record-keeping area; 20: area for examination of stool specimens; 21: area for examination of urine specimens; 22: area for reception of specimens; 23: gas bottle. 37 | P a g e Figure 2: Indicates another possible arrangement of a peripheral laboratory. 38 | P a g e Module 1 Session 2: Safety in the laboratory Objectives At the end of this session participants will be able to: 1. Identify physical, chemical, and biological hazards 2. Explain safety measures 3. Explain Cleaning, disinfection, sterilization and disposal of biohazard waste 4. Explain Disposal of Biohazard Waste Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Question and answers, discussion-lecture, mini-lecture, discussion Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 150 minutes 39 | P a g e Session plan 2 Objectives Content 1.2.1. Identify physical, chemical, and biological hazards 1.2.2. Explain safety measures Methodology Sources of laboratory hazards : - Physical - Chemical - Biological Questions & answers Safely Designed and Organized Laboratory Safe use of Laboratory Equipment Safe use of Electrical Equipment Safe use and Storage of Chemicals and Reagents Preventing Laboratory Infection Practice of Personal Hygiene Strict Prohibition of Mouth Pipetting Miscellaneous Elements of a Laboratory Safety Program Management Responsibility Safety Officer Responsibility Discussion- lectures 30 minutes 60 minutes 40 | P a g e 1.2.3. Explain Cleaning, disinfection, sterilization and disposal of biohazard waste 1.2.4. Explain Disposal of Biohazard Waste Supervisor Responsibility Employees’ Responsibility Cleaning glassware Glass containers Pipettes General rules Laboratory waste Sharps Residual body fluids Chemical wastes Mini-lecture 30 minutes Discussion 30 minutes 41 | P a g e Safety in the Laboratory Quite common hazards and accidents occur in the laboratory, the need and importance of laboratory safety should be the real concern of the laboratory. Laboratory accidents and hazards are controlled by the use of: Simple precautions Foresight (prudence) Safety devices Above all a ‘real concern’ or a ‘built in concern’ or ‘safety mindedness’ for oneself and the other fellow working at the next bench is very essential. Laboratory accidents range from minor injury, illness or loss of body parts to death. There are many factors that contribute to laboratory accidents. These include: Poorly designed laboratory Overcrowding of materials Poor training Lack of concentration Noisy and untidy working environment Carelessness and neglect Overwork and fatigue Hot and humid climatic conditions Hurrying to finish work on time Emergency condition (especially during night hours) Source of Laboratory Hazards Physical Chemical Biological 1. Physical Hazards A. Poorly Designed Laboratory Buildings Due attention should be given in the design of laboratories. The management, the laboratory personnel and the architecture should be involved in the standard design of the lab, B. Burns Burns may be caused by: Flammable chemicals and stains, or by reagents catching alight. Fires from spirit lamps, Bunsen burners, lighted tapers (e.g. when heating Ziehl-Neelsen stain), or from faulty electrical equipment or overloaded circuits. Spirit burners should not be used in direct sunlight because in bright light the flame can be difficult to see. 42 | P a g e Corrosive chemicals being spilt on the skin or ingested when mouth – pipetting. C. Electric shock Electric shock can be caused by: Faulty electrical circuits. Incorrect installation of equipment. Touching exposed live wires. D. Cuts Cuts may be caused by: Breakages. Using glassware that is cracked or has damaged edges. Walking on glass chippings. 2. Chemical Hazards A. Toxic harmful chemicals Inhaling fumes from toxic chemicals Ingesting toxic chemicals by mouth pipetting Skin contact B. Explosive chemicals Injury from explosions can be caused by: Incompatible chemical exploding Leaking gas C. Flammable chemicals causing fire Burns D. Kinds of chemicals a. Corrosive (strong acids & alkalis) Concentrated sulphuric acid Nitric acid Sodium hydroxide Potassium Hydroxide b. Toxic irritating chemicals-cause death or serious ill health if swallowed, inhaled, and by skin contact. Potassium cyanide – Chloroform Barium chloride - Sodium azide c. Flammable chemicals Ether – Acetone Romanowsky stains - Methanol d. Explosive chemicals Picric acid e. Carcinogens Chemicals that cause cancer through ingestion, inhalation, skin contact Proven carcinogen chemicals include benzidin, otoulidine, and Nitrophenol. 43 | P a g e The risk is proportional to the length of exposure, frequency of exposure, and concentration of the chemical. 3. Biological Hazards Laboratory acquired infections Infection can be caused by: Pathogens being inhaled in aerosols (airborne droplets) when snap-closing specimen containers, dispensing or pipetting infectious fluids, or centrifuging infectious material in open buckets. Aerosols may also be formed and inhaled following breakages or after spilling infectious fluids. Breakages in centrifuges can be particularly hazardous if the centrifuge is opened before the aerosols have settled. Pathogen being ingested from contaminated fingers, or in food that has been contaminated, e.g. by being stored in a laboratory refrigerator. Care should be taken to avoid the fingers or other parts of the body touching infected material. Mouth-pipetting specimens and cultures is one of the commonest ways of ingesting pathogens. Pathogens entering the skin through needle punctures, cuts, scratches, insect bites, sores or other open skin lesions. Laboratory workers must always handle infected needles with great care. Pathogens can also be acquired from unclean or nondisinfected room floors and walls, water taps and laboratory benches. Pathogens are acquired directly through careless contacts with patients or carrier staff through breathing, hand contact, etc. 4 .Safety Measures Safely Designed and Organized Laboratory It is clear that a poorly designed laboratory and overcrowding can increase the risk of laboratory accidents. It is, therefore, important to know how the laboratory should be designed with regard to safety considerations. The following are some of the features. A. Adequate floor, bench and storage space B. A floor that is well constructed with a surface that is nonslip, impermeable to liquids, and resistant to those chemicals used in the laboratory. C. Walls those are smooth, free from cracks, impermeable to liquids and easily washable. D. A door at each end of the lab so that lab staff will not be trapped should a firebreak out. E. Adequate ventilation with windows that can be opened. F. Sectioning of the laboratory into separate rooms with places for patients, visitors, and reception of specimens. G. Bench surface that are without cracks, impervious, washable, and resistant to disinfectants and chemicals. 44 | P a g e H. Suitable storage facilities that include a well-ventilated, fire proof, locked store, for the storage of flammable chemicals. I. A good supply of gas, water, electric power & wall electric points J. Provision of protective safety cabinets, fire extinguishers at accessible points, and adequate waste disposal area, etc. Safe use of Laboratory Equipment A. Positioning Suitable and ideal place for operation Avoid overcrowding of a bench with equipment Position equipment correctly that requires special facilities like ventilation, shield from sunlight, and great care. B. Installation Should be carried out by the supplier or by the health unit electrician or trained lab equipment technician. Important points to consider for safe installation Ensure that the voltage of the new equipment is the same as that of the electricity supply. Check that the power required by the instrument does not exceed the power supply circuit of the lab. Make sure that the equipment is wired correctly, and the wiring system have grounded conductor. Safe use of Electrical Equipment The supplier should demonstrate the use of an apparatus. If this is not possible, the operation and service manual should be carefully studied before the equipment is operated. Points to consider with regard to the safe use of electrical equipment: 1. Hands should be dry completely, and also the floor on which the operator is standing. 2. The electric supply must be disconnected when performing any maintenance and at the end of the day’s work. 3. If a fuse should blow, do not automatically put in a new one until the circuit is checked. Safe use and Storage of Chemicals and Reagents Even in the smallest lab, dangerous chemicals are used directly or incorporated into stains and reagents. These include highly flammable chemicals such as ether or methanol, highly corrosive chemicals such as phenol or sulphuric acid, or toxic and harmful chemicals such as formaldehyde solution. The correct handling and storage of hazardous chemicals is essential to prevent injury and damage. It is particularly important to keep chemicals out of direct sunlight and avoid overheating in chemical stores and the laboratory. Overheating can decompose many chemicals, cause explosions, or the formation of toxic fumes. 45 | P a g e Labeling of dangerous chemicals and reagents To reduce accidents caused by chemicals, many countries have introduced legislation, requiring manufacturers to label dangerous chemicals with hazard symbols and to provide simple safety instructions. The six accepted danger symbols currently in use are toxic, corrosive, explosive, oxidizing, highly flammable, and harmful or irritant. Figure 3: Common symbols of hazards Preventing Laboratory Infection All specimens received in the lab should be regarded as potentially pathogenic. For example, a blood specimen sent for measuring hemoglobin may contain highly infectious organisms. Laboratory acquired infections can be prevented by: Practicing personal hygiene Wearing of laboratory coat and protective gloves Safe handling of specimens and infectious materials. Avoiding mouth-pipetting Disposing safely of specimens and contaminated material. Being immunized against highly infectious pathogens Practice of Personal Hygiene This includes: Washing of hands and arms with soap and water before and after work Wearing protective clothing and gloves whenever possible. Covering any cuts, insect bites open sores, or wounds with a water proof adhesive dressing. Wearing closed shoes and not walking barefoot. Not eating, drinking, chewing gum, smoking or applying cosmetics in any part of the lab. Safe Handling and Disposal of Specimens Special precautions should be taken when collecting specimens, especially blood specimens, and when testing specimens and handling infected material. Safety measures involved are: Careful handling and disposal of materials used for collecting specimens. Making contaminated materials non-infectious by using appropriate decontamination methods. 46 | P a g e Wearing gloves and a plastic apron when collecting blood suspected of having a highly infectious disease like AIDS. Avoid contamination of fingers, other body parts, and working surface. Specimens suspected of having hepatitis, and AIDS must be labeled ‘HIGH RISK’. Strict Prohibition of Mouth Pipetting Pathogens may be ingested during mouth pipetting, either by direct aspiration or from the mouth ends of pipettes which have been contaminated from fingers or benches. Accidents caused by mouth pipetting include infection, poisoning, chemical burns, and other injuries from chemicals. There are many inexpensive and simple ways to measure and dispense safely without mouth pipetting. Miscellaneous Immunization- protective inoculations against certain pathogenic organisms are necessary. The use of signs- display suitable safety signs both prohibitive (don’t) and commands (do). First aid- basic practical training in first aid helps to reduce suffering and consequences of serious accidents. Elements of a Laboratory Safety Program A successful laboratory safety program requires the participation of persons at every level of the laboratory staff. Safety does not occur only with the appointment of safety officer or safety committee. Safety does not occur by having employees solely perform their assigned duties in manner which they feel is most efficient. Laboratory safety requires the full participation of every member of the staff. Management Responsibility Establish a policy relative to the design and implementation of his safety program. Delegate authority for implementing the program Provide a safe and healthful work place Provide fund for the implementation of the program Assess the program- establish a mechanism to ensure safety Establish safety committee- regular report, recommendations regarding need for modification of the program. Safety Officer Responsibility Technical advisor to the program Assist in the development of safe work method Advise management on safety issues Assist safety committee Provide a variety of communication, e.g. hazard notice, safety data 47 | P a g e Review a variety of plans which include facility designs, special equipment purchase in relation to safety. Supervisor Responsibility Train the staff in lab practices required for safe conduct of work. Evaluate regularity of the laboratory facilities, equipment, personnel and work place. Correct unsafe condition as fire hazards, physical hazards, and defective equipment. Employees’ Responsibility Use of safe equipment Report of malfunctioning of equipment Report injuries or exposure Report hazard or unsafe condition to supervisors 5. Cleaning, disinfection, sterilization and disposal of biohazard waste. Cleaning glassware Instructions for cleaning: glass containers (Erlenmeyer flasks, beakers, test-tubes) pipettes Glass containers New glassware Glassware that has never been used may be slightly alkaline. In order to neutralize it: Prepare a bowl containing 3 liters of water and 60 ml of concentrated hydrochloricacid (i.e. a 2% solution of acid). Leave the new glassware completely immersed in this solution for 24 hours. Rinse twice with ordinary water and once with demineralized water. Dry. Dirty glassware Preliminary rinsing: Rinse twice in cold or lukewarm water (never rinse bloodstained tubes in hot water), If the glassware has been used for fluids containing protein, it should be rinsed immediately and then washed (never allow it to dry before rinsing). Soaking in detergent solution: Prepare a bowl of water mixed with washing powder or liquid detergent. Put the rinsed glassware in the bowl and brush the inside of the containers with a test-tube brush. Leave to soak for 2–3 hours. Rinsing Remove the articles one by one. Rinse each one thoroughly under the tap, then soak them all in a bowl of ordinary water for 30 minutes. 48 | P a g e Rinse each article in a stream of clean water. (Do not forget that traces of detergent left on glassware can lead to false laboratory results.) Draining Place containers (beakers, flasks, measuring cylinders) on the pegs of a draining rack. Place test-tubes upside-down in a wire basket. Drying Place the glassware in wire baskets and dry in a hot-air oven at 60 °C. Alternatively, place the baskets in a sunny spot in the laboratory and cover them with a fine cloth. Plugging The clean dry glassware should be put away in a cupboard to protect it from dust. It is recommended that glass containers be plugged with non-absorbent cotton wool or their mouths covered with small caps made from newspaper or, preferably, thin sheets of paraffin wax or clinging plastic, if available. Pipettes Immediate rinsing Once a pipette has been used, rinse it immediately in a stream of cold water to remove blood, urine, serum, reagents, etc. Soaking in water After rinsing, place the pipettes in a large, plastic measuring cylinder (or bowl) full of water. If the pipettes have been used to measure infected material, leave them in a cylinder full of disinfectant solution (e.g. a quaternary ammonium compound or 1% bleach solution; see pages 84 and 85) for 4 hours. Soaking in detergent and rinsing Follow the instructions given above for soaking and rinsing of laboratory glassware. Blocked pipettes Put blocked pipettes in a cylinder filled with dichromate cleaning solution. Slide them carefully into the solution and leave for 24 hours. The next day, pour the dichromate solution into another cylinder (it can be used four times). Hold the cylinder containing the pipettes under the tap and rinse thoroughly. Remove the pipettes one at a time. Check that the obstruction has been washed away. Rinse again. Leave to soak in ordinary water for 30 minutes, then change the water and soak for a further 30 minutes. Warning: Dichromate cleaning solution is highly corrosive and should be used with extreme care. If it is accidentally splashed on the skin or clothing or into the eye(s), wash at once with large quantities of water. 49 | P a g e Drying Dry heat-resistant glass pipettes in a hot-air oven at 60 °C and ordinary pipettes in an incubator at 37 °C. Alternatively, leave pipettes to air-dry. Using the vacuum pump This is a small instrument made of metal, plastic or glass that is attached to the water tap. Turn the water on hard to drive a strong jet through the pump. This causes air to be sucked into the side arm of the pump and the rubber tubing attached to it. Fit this rubber tubing over the tip of the pipette. 3. Dip the other end of the pipette into the rinsing liquid (water or detergent solution), which is sucked through the pipette and discharged by the pump into the sink (Fig ). 6. Disposal of Biohazard Waste A. General rules Prior to any treatment, all biohazard wastes, including those to be incinerated, should be enclosed in a puncture-resistant, biohazard bag that is color-coded or labeled with the biological hazard symbol. Untreated biohazard waste is not to be disposed of in the municipal waste (system) stream. All biohazard waste must be treated by chemical disinfection or autoclaving before in any way being disposed of in the municipal waste stream. 50 | P a g e After disinfection, but before disposal in the municipal waste stream, all treated biohazard wastes (apart from liquids) should be enclosed in an unmarked outer bag that is not red or labelled with the biohazard symbol. Any biohazard waste that has been treated as described below and packaged such that it is clearly evident that the waste has been effectively treated, is not subject to be treated as biohazard waste and may be collected, transported for incineration or disposed of as municipal waste. The person handling the emptying of waste bins, waste bottles or sharps containers must be careful not to touch anything without protective clothing and must use gloves to avoid contracting infections from the waste. The waste bins, sharps containers, etc., must be clearly indicated/marked: Biohazard wastes. B. Laboratory waste Discarded swabs, cotton, sample containers and other biohazard but non-sharp objects used for sample collection should be placed in a covered trash container lined with an autoclavable biohazard yellow bag. Visibly soiled or splashed tourniquets and Vacutainer holders should be discarded and new equipment used. Disposable plastics such as tips, culture plates, micro plates, petri dishes, test tubes, etc., used for testing of samples should be disposed of in a covered waste bin lined with an autoclavable biohazard yellow bag, autoclaved and transported for incineration. Pipettes should be soaked in special pipette baskets in 10 % household bleach overnight, before being thrown in a waste bin lined with an autoclavable biohazard yellow bag, autoclaved and incinerated. Reusable glassware such as cylinders, flasks and beakers should be disinfected with 10 % household bleach over night before washed and autoclaved. C. Sharps All sharp implements used in the laboratory need to be handled carefully. They can easily break the skin and increase the risk of infection with infectious agents. Broken glassware must also be handled as sharps. The laboratory should have a special box for broken glassware If needles are used, they should never be recapped before disposal. Recapping needles may lead to somebody accidentally pricking him or herself. Dispose of all sharps directly into a with a secure perforated sharps disposal container lid. The lid only allows the implements into the container but not out. The sharps container should be puncture-resistant, leak proof on the sides and bottom, and colorcoded or labeled with a biohazard symbol. Note: When selecting sharps containers, look for special safety features such as lids that lock tight for safe disposal and a container that can be sterilized by steam, gas, or chemicals. If sharps containers are not specifically constructed to be autoclaved, the 51 | P a g e resulting mass of melted plastic is extremely hazardous due to the needles that often protrude. When full, seal top, autoclave, then arrange for incineration. Decontamination is achieved by autoclaving the sharp implements. Incineration destroys the sharps completely hence eradicating the chances of accidental injury to people in the community. D. Residual body fluids Ensure that all tubes/containers containing residual body fluids are properly sealed to avoid spillage. These are then stored temporarily in waste bins lined with disposal bags. Transfer the disposal bags, together with contents, into autoclaving bags stick a piece of autoclavable tape on the bag and then autoclave as required. After the autoclaving cycle is completed, transport and incinerate the whole package to completely destroy the tubes. E. Chemical wastes The following procedure is adopted for most chemicals used in low concentrations. Collect all liquid chemical waste in properly labeled bottles with a little concentrated disinfectant (i.e., JIK). Keep monitoring the rising level of waste in the trap bottles. Never fill the trap bottles to the very top to avoid spillage. Empty the contents of the trap bottle down the drain, preferably a special sink in the laboratory, and wash down with more disinfectant, liquid soap and a large volume of water. Minimum disinfection time of any liquid Biohazard Waste is 30 minutes. Note:Some disinfectants react with organic compounds, acids, or bases. Consider this when selecting your disinfectant before commencing your work. SAFETY PRECAUTIONS Anybody handling Biohazard Wastes should always put on laboratory protective clothing and gloves and keep to the laboratory safety practices to avoid viral and other infectious disease transmissions. Any spills or splashes of infectious material should be immediately cleaned up with absorbent material using an approved disinfectant such as dilute 10% bleach or chlorhexidine solution. Decontaminating bench tops and other surfaces Bench tops should be wiped with a disinfectant (a phenolic disinfectant, 1% sodium hypochlorite [bleach], or 70% isopropyl alcohol) routinely after working with infectious agents or clinical specimens or after spills, splashes, or other contamination by infectious materials. Solutions of disinfectants should be maintained at the work station. 52 | P a g e Decontamination of spills The following procedure is recommended for decontaminating spills. • Isolate the area to prevent anyone from entering. • Wear gloves and protective clothing (e.g., a gown or lab coat, shoes, and a mask [if the spill may contain a respiratory agent or if the agent is unknown]). • Absorb or cover the spill with disposable towels. • Saturate the towels with an appropriately diluted intermediate or high-level disinfectant (e.g., a phenolic formulation or household bleach). • Place disinfectant-soaked towels over the area and leave them in place for at least 15 minutes before removing and discarding them. • Wipe area using clean disinfectant-soaked towels and allow area to air dry. • Place all disposable materials used to decontaminate the spill into a biohazard container. • Handle the material in the same manner as other infectious waste. 53 | P a g e Module two: Hematology Module Objectives: At the end of this module the participant will be able to: 3. Apply collection and handling of blood 4. Apply Automated Blood Count Techniques 5. Apply manual techniques Modules Sessions Session 1: Collection and handling of blood and automated blood count techniques Session 2: Manual techniques Evaluation/ Assessment Questions and answers, participants’ summaries, trainer’s evaluation Estimated Training Time 9 hours 54 | P a g e Module 2 Session 1: Collection and handling of blood and automated blood count techniques Objectives At the end of this session participants will be able to: 1. Apply collection and handling of blood 2. Explain hemoglobin concentration, red blood cell count, and counting systems 3. Explain reliability of electronic counters 4. Explain Packed Cell Volume and Mean Cell Volume 5. Explain variation in red cell volumes: red cell distribution width and total white blood cell count 6. Explain automated differential count 7. Explain new white cell parameters and platelet count 8. Explain mean platelet volume, reticulocyte count, and immature reticulocyte fraction 9. Explain calibration of automated blood cell counters 10. Explain flagging of automated blood counts Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Mini-lecture, Question & answers, discussion-lecture, discussion, brain storming Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 290 minutes 55 | P a g e Session plan -1Objectives 2.1.1. Apply collection and handling of blood Content 2.1.2. Explain hemoglobin concentration, red blood cell count, and counting systems 2.1.3. Explain reliability of electronic counters Methodology General precautions: Technical errors: Venous blood collection: Capillary (peripheral) blood Differences between capillary and venous blood Serum Mini-lecture Hemoglobin concentration Red blood cell count Counting systems - Impedance counting - Light scattering Question & answers 30 minutes 30 minutes Electronic counts are Mini-lecture precise, but care needs to be taken so 30 minutes that they are also accurate. The recorded count on the same sample may vary from instrument to instrument and even between different models of the same instrument. 56 | P a g e 2.1.4. Explain Packed Cell Volume and Mean Cell Volume Setting discrimination thresholds Modern automated blood cell counters estimate PCV by technology that has little connection with packing red cells by centrifugation With automated instruments, the derivation of the RBC, PCV, and MCV are closely interrelated Automated instruments require calibration before the PCV or MCV can be determined The MCV, and therefore the PCV, as determined by an automated counter, will vary with certain cell characteristics other than volume The automated MCV and PCV are prone to certain errors that do not occur or are less of a problem with manual methods Discussion-lecture 30 minutes Discussion 2.1.5. Explain variations in red cell volumes: red cell distribution width Automated instruments produce volume 30 minutes 57 | P a g e and total white blood cell count distribution histograms that allow the presence of more than one population of cells to be appreciated The total WBC is determined in whole blood in which red cells have been lysed Mini-lecture 2.1.6. Explain automated differential count 30 minutes 2.1.7. Explain new white cell parameters and platelet count Most automated differential counters that are now available use flow cytometry incorporated into a full blood counter rather than being stand-alone differential counters Question & answers 30 minutes Automated white cell counters can analyze cell characteristics by novel technologies and identify cell types by features that differ greatly from those used when a blood film is examined visually . Three techniques for setting 58 | P a g e thresholds have been used: (a) Platelets can be counted between two fixed thresholds (e.g., between 2 and 20 fl; (b) Pulses between fixed thresholds can be counted with subsequent fitting of a curve and extrapolation so that platelets falling outside the fixed thresholds are included in the computed count. (c) Thresholds can vary automatically, depending on the characteristics of individual blood samples, to make allowance for microcytic or Mini-lecture fragmented red 30 minute cells or for giant platelets 2.1.8. Explain mean platelet volume, reticulocyte count, and immature reticulocyte fraction The calculated MPV is very dependent on the technique of measurement and on length and conditions of storage prior to testing the blood. Automated reticulocyte counts 59 | P a g e 2.1.9. Explain calibration of automated blood cell counters 2.1.10. Explain flagging of automated blood counts have been developed by using the fact that various dyes and fluorochromes combine with the RNA of reticulocytes Fully automated instruments provide a measure of the various degrees of reticulocyte maturation because the most immature reticulocytes, produced when erythropoietin levels are high, have more RNA and fluoresce more strongly than the Mini-lecture mature 30 minutes reticulocytes normally present in the peripheral blood Methods are recommended for calibrating an automated blood cell counter: - By using fresh normal blood specimens - By use of a stable calibrant - By use of a commercial calibrant Brain storming 20 minutes 60 | P a g e Flagging” refers to a signal that the specimen being analysed may have a significant abnormality because one or more of the blood count variables are outside specified limits (usually 2SD) or there is a qualitative abnormality that requires a quality control check and/or additional investigation 61 | P a g e Hematology 1. Collection & Handling of blood General precautions: Technical errors: Always wear disposable plastic gloves, especially if there is any hand cut. Always be careful when handling syringes, needles & lancets. Always use disposable syringes, needles & lancets. Always take care of specimen identification & request forms. Faults in sample Collection (See below). Faults in sample Transport & Storage (identification error, how long delay & at what temp.). Technical errors from sample collection: Insufficient or excess anticoagulant. Inappropriate anticoagulant. Inadequate mixing with anticoagulant. Patient &/or specimen identification error. Delay in transit to lab. Venous blood collection: The phlebotomist should enter a training program. Venous blood, mixed with an anticoagulant, is preferred for most hematological examinations. Best site is the antecubital vein, & in obese subject may use the dorsum of the hand. Needle guage: for adults 21 (0.8mm), for children 23 (0.6mm). Make sure of proximal & distal fixation of the vein. Skin preferably cleaned with 70% alcohol. Steps to facilitate obtaining a venous blood sample are: Warming the patient’s arm. Using a tourniquet (should be loosened once entered the vein to avoid hemoconcentration and hemolysis). Tapping the skin over the site of the vein. Asking the patient to open & clench his fist several times. Advantages of using the tourniquet: - Blood filling of the vein. 62 | P a g e - Proximal fixation of the vein. Disadvantages of using the tourniquet: - Hemoconcentration. - Red cell hemolysis. Always notice the blood level marker in tubes containing an anticoagulant. After puncture: elevate the arm, apply pressure & adhesive dressing. There is no difference in using glass or plastic tubes except in coagulation study (where plastic or siliconized glass tubes should be used). Avoid hemolysis of blood by: Minimal use of the tourniquet. Withdraw blood slowly. Do not use very fine needled. Deliver the blood gently into the tube. Avoid frothing during mixing the tube. Capillary (peripheral) blood: It is often necessary to obtain blood by skin puncture in babies and infants and in adults with poor veins. Capillary blood may be obtained from a freely flowing stab wound made with a sterile lancet on: - The plantar surface of a warmed and cleansed heel (babies less than 3 months of age). The correct site for puncture of the heel is shown in Fig. 1.4. - The plantar aspect of the big toe (infants). - A finger, thumb or ear lobe (older children and adults). The lateral or posterior aspect of the heel should not be used in a baby, as the underlying bone is much closer to the skin surface than it is on the plantar aspect. Osteomyelitis of the calcaneal bone has resulted from puncture of the bone. In older patients a finger (excluding the fifth finger) or the thumb is preferred. The palmar surface of the distal phalanx is the preferred site on a digit, since the underlying bone is closer to the skin surface on other aspects. The middle or ring finger of the non-dominant hand is preferred; these digits are less painful than the index finger. Previous puncture sites should be avoided, to reduce the risk of infection. In adults, skin punctures should ideally be more than 1.5 mm deep in order that the lancet passes through the dermal– subcutaneous junction where the concentration of blood vessels is greatest, permitting a free flow of blood. Lancets used for heel puncture in full-term babies must not exceed 2.4 mm in length, since this is the depth below the skin of the calcaneal bone. Much shorter lancets are available and should be selected for use in premature babies. Safety lancets, with a blade that retracts permanently after first use, have been developed in order to reduce the risk of accidental injury to phlebotomy staff. 63 | P a g e Capillary samples should be obtained from warm tissues so that a free flow of blood is more readily obtained. If the area is cool then it should be warmed with a wet cloth. The skin should then be cleansed with 70% alcohol and dried with sterile gauze (since traces of alcohol may lead to haemolysis of the specimen). The first drop of blood may be diluted with tissue fluid and should be wiped away with sterile gauze square. Flow of blood may be promoted by gentle pressure, but a massaging or pumping action should not be employed, since this may lead to tissue fluid being mixed with blood. Differences between capillary and venous blood: Venous blood and “capillary” blood are not quite the same. Blood from a skin puncture is a mixture of blood from arterioles, veins, and capillaries, and it contains some interstitial and intracellular fluid. However, there are negligible differences when a free flow of blood has been obtained. The differences may be exaggerated by cold with resulting slow capillary blood flow. The packed cell volume (PCV), RBCs count, and Hemoglobin concentration (Hb) of capillary blood are slightly greater than in venous blood. Also the total leukocyte and neutrophil counts are higher. Conversely, the platelet count appears to be higher in venous than in capillary blood. This may be the result of adhesion of platelets to the site of the skin puncture. Serum: The difference between plasma and serum is that the latter lacks fibrinogen and some of the coagulation factors. Blood collected to obtain serum should be delivered into sterile tubes with caps or evacuated collection tubes and allowed to clot undisturbed for about 1 hour at room temperature (18-25°C). Then the clot should be loosened gently from the container wall by means of a wooden stick or a thin plastic or glass rod. Rough handling will cause hemolysis. The tubes are centrifuged for 10 min at about 1200 rpm. The supernatant serum then is pipetted into another tube and centrifuged again for 10 min at about 1200 rpm. The supernatant serum is transferred to tubes for tests or for storage. For most tests, serum should be kept at 4°C until used, but if testing is delayed, serum can be stored at -20°C for up to 3 months and at -40°C or less for long-term storage. Frozen specimens should be thawed on the bench or in a water bath at room temperature, and then inverted several times to ensure homogeneity before use for a test. Do not refreeze thawed specimens. 64 | P a g e Figure 4:Anterior surface of the left arm showing veins most suitable for venepuncture. Figure 5: Venepuncture technique using needle and syringe. 65 | P a g e Figure 6: Venepuncture technique using an evacuated container; the distal end of the needle has been screwed into the holder and the proximal needle has then been unsheathed and inserted into a suitable vein. Figure 7:The areas of the foot of a baby or infant which are suitable for obtaining capillary blood. 2. Part One: Automated Blood Count Techniques A variety of automated instruments for performing blood counts are in widespread use. semi-automated instruments require some steps (e.g., dilution of a blood sample) to be carried out by the operator. Fully automated instruments require only that an appropriate blood sample is presented to the instrument. Semiautomatic instruments often measure a small number of components (e.g., WBC and Hb). Fully automated multichannel instruments usually measure from 8 to 20 components, including some variables that have no equivalent in manual techniques. Automated instruments usually have a high level of precision, which, for cell counting and cell-sizing techniques, is greatly superior to that achievable with manual techniques. If instruments are carefully calibrated and their correct operation is ensured by quality 66 | P a g e control procedures, they produce test results that are generally accurate. When blood has abnormal characteristics, the results for one or more parameters may be aberrant; instruments are designed so that such inconsistent results are “flagged” for subsequent review. The abnormal characteristics that lead to inaccurate counts vary between instruments, so it is important for instrument operators to be familiar with the types of factitious results to which their instruments are prone. Blood cell counters may have automated procedures for sample recognition (e.g., by bar-coding), for ensuring that adequate sample mixing occurs, for taking up the test sample automatically, and for detection of clots or inadequately sized samples. Ideally, blood sampling is carried out by piercing the cap of a closed tube so that samples that carry an infection hazard can be handled with maximum safety. Laboratories performing large numbers of blood counts each day require fully automated blood counters capable of the rapid production of accurate and precise blood counts, including platelet counts and differential counts, either three-part or five- to seven-part. The sample throughput required varies with the workload and the timing of arrival of blood specimens in the laboratory, but for most large laboratories a throughput of 100 or more samples per hour is required. Sample size and the availability of a “predilute” mode are particularly relevant if the laboratory receives many paediatric specimens. Choice of an instrument for an individual laboratory, as well as for point-of-care sites outside the laboratory, should take account of capital expenditure and running costs, including maintenance and reagents; size of instrument; requirements of services such as water, compressed air, drainage, and an electricity supply with stable voltage; environmental disturbance by generation of heat, vibration, and noise; any influence on performance by the ambient temperature and humidity; storage requirements for the often bulky reagents; ease of operation; and the likely level of support that can be expected from the manufacturer. Most automated instruments, however, count for a specified period of time rather than on an exact volume of blood; they therefore require calibration by means of the direct counts derived from instruments counting cells in a defined volume of diluted blood. For some variables, instruments are calibrated by the manufacturer, but others require calibration in the laboratory. Performance characteristics of an instrument vary over time, so periodic recalibration is needed; both when quality control procedures indicate the necessity and when certain components are replaced. 2.1 Hemoglobin Concentration Most automated counters measure haemoglobin by a modification of the manual HiCN method with cyanide reagent or with a nonhazardous chemical such as sodium lauryl sulphate, which avoids possible environmental hazards from disposal of large 67 | P a g e volumes of cyanide-containing waste. Modifications include alterations in the concentration of reagents and in the temperature and pH of the reaction. A nonionic detergent is included to ensure rapid cell lysis and to reduce turbidity caused by cell membranes and plasma lipids. Measurements of absorbance are made at a set time interval after mixing of blood and the active reagents but before the reaction are completed. 2.2 Red Blood CELL Count Red cells and other blood cells can be counted in systems based on either aperture impedance or light-scattering technology. Because large numbers of cells can be counted rapidly, there is a high level of precision. Consequently, electronic counts have rendered the RBC and the red cell indices derived from it (the MCV and the MCH) of much greater clinical relevance than was possible when only a slow and imprecise manual RBC was available. 2.3 Counting Systems Impedance Counting Impedance counting, first described by Wallace Coulter in 1956 depends on the fact that red cells are poor conductors of electricity, whereas certain diluents are good conductors; this difference forms the basis of the counting systems used in Beckman– Coulter, Sysmex, Abbott, Roche, and a number of other instruments. For a cell count, blood is highly diluted in a buffered electrolyte solution. The flow rate of this diluted sample is controlled by a mercury siphon (as in the original Coulter system) or by displacement of a tightly fitting piston. This result is a measured volume of the sample passing through an aperture tube of specific dimensions (e.g., 100 mm in diameter and 70 mm in length). By means of a constant source of electricity, a direct current is maintained between two electrodes, one in the sample beaker or the chamber surrounding the aperture tube and another inside the aperture tube. As a blood cell is carried through the aperture, it displaces some of the conducting fluid and increases the electrical resistance. This produces a corresponding change in potential between the electrodes, which lasts as long as the red cell takes to pass though the aperture; the height of the pulses produced indicates the volume of the cells passing through. The pulses can be displayed on an oscillograph screen. The pulses are led to a threshold circuit provided with an amplitude discriminator for selecting the minimal pulse height, which will be counted. The height of the pulses is used to determine the volume of the red cells. 68 | P a g e Figure 8: Effect of threshold discrimination (horizontal axis) in separating cell signals from background noise. Light Scattering Red cells and other blood cells may be counted by means of electro-optical detectors. A diluted cell suspension flows through an aperture so that the cells pass, in single file, in front of a light source; light is scattered by the cells passing through the light beam. The scattered light is detected by a photomultiplier or photodiode, which converts it into electrical impulses that are accumulated and counted. The amount of light scattered is proportional to the surface area and therefore the volume of the cell so that the height of the electrical pulses can be used to estimate the cell volume. The high-intensity coherent laser beams used in current instruments have superior optical qualities to the noncoherent tungsten light of earlier instruments. Sheathed flow allows cells to flow in an axial stream with a diameter not much greater than that of a red cell; light can be precisely focused on this stream of cells. Electro-optical detectors are used for red cell sizing and counting in Bayer-Technicon systems and for white cell differential counting in a number of other instruments. 69 | P a g e 2.4 Reliability of Electronic Counters Electronic counts are precise, but care needs to be taken so that they are also accurate. The recorded count on the same sample may vary from instrument to instrument and even between different models of the same instrument. Inaccuracy may be introduced by : 1-coincidence (i.e., by two cells passing through an orifice simultaneously and being counted as one cell. 2-pulse being generated during the electronic dead time of the circuit. 3-Recirculation of cells that have already been counted. 4-red cell agglutination (which causes a clump of cells to be counted as one Cell). 5-by the counting of bubbles, lipid droplets, microorganisms, or extraneous Particles as cells. 6-Faulty maintenance may lead to variation in the volume aspirated or the flow rate. 7-Single-channel instruments may have their thresholds set incorrectly, and multichannel instruments may be incorrectly calibrated. Coincidence correction; in some instruments, this is done automatically by electronic editing. Errors of coincidence can be detected by carrying out a series of measurements at various dilutions of the same specimen, plotting the data on graph paper, and then extrapolating the graph to the baseline for the true value. Alternatively, the need for coincidence correction can be avoided by having the dimensions and flow characteristics of the aperture through which the cells pass such that cells can only pass in single file; this may be achieved by sheath flow or hydrodynamic focusing in which diluted blood is injected into a sheath of fluid as it flows into the sensing zone. This induces the cells to pass through the centre of the sensing zone in single file and free of distortion. Coincidence can be more effectively reduced with sheathed flow and precisely focused light in an electro-optical detector than in an impedance counter so that less dilution of the blood sample is needed. Electrical impulses generated by recirculation of cells can be eliminated by electronic editing. recirculation of cells in the region of the aperture can be prevented by “sweep flow” in which a directed stream of diluent sweeps cells and debris away from the aperture, thus preventing cells from being recounted and debris from being counted as cells. Inaccurate counts consequent on red cell agglutination are usually the result of cold agglutinins. They are recognized as erroneous because of an associated marked factitious elevation of the MCV. A correct count can be achieved by prewarming the blood sample and, if necessary, also prewarming the diluent. 70 | P a g e A correct RBC and, particularly, a correct measurement of the MCV are dependent on the use of an appropriate diluent. For impedance counters, pH, temperature, and rate of ionization have to be standardized and remain constant because changes alter the electrical field and may lead to artefactual alterations in the size, shape, and stability of the blood cells in the diluent. Diluents must be free of particles and give a background count of less than 50 particles in the measured volume. The correct diluent for each individual instrument must be used; other diluents, even those made by the same manufacturer, may not be interchangeable. Any laboratories using diluents other than those recommended by the manufacturer of the instrument must satisfy themselves that no error is being introduced. For red cell counting in simple single-channel counters a suitable diluent requires a pH of 7.0–7.5 and osmolality of 340 ± 10 mmol. Physiological saline (9 g/l NaCl) or phosphate-buffered saline, which have the advantages of simplicity and ready availability, can be used as a red cell diluent, provided that the counts are performed immediately after dilution to avoid errors owing to sphering. Commercial solutions of saline (for intravenous use) are usually particle-free. Other solutions may require filtration through a 0.22- or 0.45-mm micropore filter to remove dust. Setting Discrimination Thresholds An accurate RBC requires that thresholds be set so that all red cells, but a minimum of other cells, are included in the count. Some counters have a lower threshold but no upper threshold so that white cells are included in the “RBC.” Because the WBC is usually very low in relation to the RBC, this is not usually of practical importance; however, an appreciable error can be introduced if the WBC is greatly elevated, particularly if the patient is also anaemic. The setting of the lower threshold is of considerable importance because it is necessary to ensure that microcytic red cells are included in the count without also counting large platelets. Current multichannel instruments, both impedance counters and counters using lightscattering technology, have thresholds that are either precalibrated by the manufacturer or are automatically adjusted, depending on the characteristics of individual blood samples. Single-channel impedance instruments capable of performing a direct RBC require setting of thresholds so as to separate pulses generated by red cells from background noise and from pulses generated by platelets. This is done by adjusting the aperture current and the pulse amplification. A simple method is to dilute a fresh blood sample and carry out successive counts on the suspension, while the lower threshold control is moved incrementally from its maximum to its minimum position. At the maximum position, the count should be zero or close to zero, and the counts will increase as the amplitude is reduced. The counts at each setting are plotted on arithmetic graph paper. 71 | P a g e Figure 9: Setting Discrimination Thresholds Method to establish working conditions of cell counters. The correct setting of the threshold (at arrow) is intended to exclude noise pulses without loss of the signal pulses produced by the blood cells. The correct threshold setting is at the left of the horizontal part of the graph before the line begins to slope. It is important to check that the setting selected is valid for microcytic cells. The threshold can be defined more precisely for an individual sample by means of a pulse height analyser linked to the counting system. The lower threshold is correctly set if beyond this point there are less than 0.5% of the counts at the peak (mode) of the pulse size distribution curve. 2.6 Packed Cell Volume and Mean Cell Volume Modern automated blood cell counters estimate PCV by technology that has little connection with packing red cells by centrifugation. It is sometimes convenient to use different terms to distinguish the manual and automated tests, and for this reason the International Council for Standardization in Haematology has suggested that the term “haematocrit” (Hct) rather than PCV should be used for the automated measurement. 72 | P a g e However, it should be noted that, in the past, the terms “packed cell volume” and “haematocrit” have been used interchangeably for the manual procedure. With automated instruments, the derivation of the RBC, PCV, and MCV are closely interrelated. The passage of a cell through the aperture of an impedance counter or through the beam of light of a light-scattering instrument leads to the generation of an electrical pulse the height of which is proportional to cell volume. The number of pulses generated allows the RBC to be determined, as discussed earlier. Pulse height analysis allows either the MCV or the PCV to be determined. If the average pulse height is computed, this is indicative of the MCV, and the PCV can be derived by multiplying the estimated MCV by the RBC. Similarly, if the pulse heights are summated, this figure is indicative of the PCV, and the MCV can, in turn, be derived by dividing the PCV by the RBC. Automated instruments require calibration before the PCV or MCV can be determined. Calibration of the PCV can be based on manual PCV determinations. Alternatively, the MCV can be calibrated by means of the pulse heights generated by latex beads, sdtabilize cells, or some other calibrant containing particles of known size; however, unfixed human red cells that are biconcave and flexible will not necessarily show the same characteristics in a cell counter as latex particles or some other artificial calibrant. Aperture-impedance systems measure an apparent volume that is greater than the true volume, being influenced by a “shape factor; this factor is less than 1.1 for young, flexible red cells; is between 1.1 and 1.2 for fixed biconcave cells; and is about 1.5 for spheres, whether they be fixed cells or latex spheres. The MCV, and therefore the PCV, as determined by an automated counter, will vary with certain cell characteristics other than volume. As indicated earlier, such characteristics include shape, which in turn is partly determined by flexibility. With impedance counters, the normal disc-shaped red cell becomes elongated into a cigar shape as it passes through the aperture; this is caused by deformation in response to shear force, which occurs in cells of normal flexibility. Cells with a reduced haemoglobin concentration undergo more elongation than normal cells; this leads to a reduced “shape factor,” a reduced pulse height in relation to the true size of the cell, and underestimation of the MCV. Conversely, cells with abnormally rigid membranes and cells such as spherocytes with a high haemoglobin concentration will undergo less deformation than normal and the MCV will be overestimated. Earlier lightscattering instruments also underestimated the volume of red cells with a reduced haemoglobin concentration because light scattering was affected by the haemoglobin concentration. These artefacts are seen even with normal red cells of varying haemoglobin concentration but are more apparent with red cells from patients with defects in haemoglobin synthesis such as those from patients with iron deficiency. Light-scattering instruments have been developed to avoid artefacts of this type. Cells are isovolumetrically sphered so that their light-scattering characteristics are uniform and should follow the laws of physics. 73 | P a g e The automated MCV and PCV are prone to certain errors that do not occur or are less of a problem with manual methods. These include those resulting from microclots or partial clotting of the specimen, extreme microcytosis, and the presence of cryoglobulins or cold agglutinins; the last is a relatively common cause of factitious elevation of the MCV because clumps of cells are sized as if they were single cells. Because the RBC is underestimated, the PCV is less affected, although it is also inaccurate. It is rare for warm agglutinins to cause a similar problem. Sickling may cause a factitious increase in MCV and PCV, whereas alterations in plasma osmolarity occurring, for example, in severe hyperglycemias also cause factitious elevation of the MCV and PCV. 2.7 VARIATIONS IN RED CELL VOLUMES: RED CELL DISTRIBUTION WIDTH Automated instruments produce volume distribution histograms that allow the presence of more than one population of cells to be appreciated. Instruments may also assess the percentage of cells falling above and below given MCV thresholds and “flag” the presence of an increased number of microcytes or macrocytes. Such measurements may indicate the presence of a small but significant increase in the percentage of either microcytes or macrocytes before there has been any change in the MCV. The RDW is derived from pulse height analysis and can be expressed either as the standard deviation (in fl) or as the coefficient of variation (CV) (%) of the measurements of the red cell volume. Current Beckman-Coulter and Bayer-Technicon instruments express the RDW as the SD, and Sysmex instruments express it as either the SD or the CV. The normal reference range is in the order of 12.8 ± 1.2% as CV and 42.5 ± 3.5 fl as SD. However, widely different ranges have been reported; therefore it is important for laboratories to determine their own reference ranges. The RDW expressed as the CV has been found of some value in distinguishing between iron deficiency (RDW usually increased) and thalassaemia trait (RDW usually normal) and between megaloblastic anaemia (RDW often increased) and other causes of macrocytosis (RDW more often normal). 2.8 TOTAL WHITE BLOOD CELL COUNT The total WBC is determined in whole blood in which red cells have been lysed. The lytic agent is required to destroy the red cells and reduce the red cell stroma to a residue that causes no detectable response in the counting system without affecting leucocytes in such a manner that the ability of the system to count them is altered. Various manufacturers recommend specific reagents, and for multichannel instruments that also perform an automated differential count use of the recommended reagent is essential. Fully automated multichannel instruments perform WBCs by impedance or lightscattering technology or both. Residual particles in a diluted blood sample are counted after red cell lysis or, in the case of some light-scattering instruments, after the red 74 | P a g e cells have been rendered transparent. Thresholds are set to exclude normal platelets from the count, although giant platelets are included. Some or all of any nucleated red cells present are usually included, so that when nucleated red cells are present the count approximates more to the TNCC than to the WBC. Factitiously low automated WBCs occasionally occur as a consequence of leucocyte agglutination, prolonged sample storage, or abnormally fragile cells (e.g., in leukaemia). Factitiously high counts are more common and usually result from failure of lysis of red cells. With certain instruments this may occur with the cells of neonates or be consequent on uraemia or on the presence of abnormal haemoglobin such as haemoglobin S or haemoglobin C; high counts may also be the result of microclots, platelet clumping, or the presence of a cryoglobulin. 2.9 AUTOMATED DIFFERENTIAL COUNT Most automated differential counters that are now available use flow cytometry incorporated into a full blood counter rather than being stand-alone differential counters. Increasingly, automated blood cell counters have a differential counting capacity, providing either a three-part or a five- to seven-part differential count. Counts are performed on diluted whole blood in which red cells are either lysed or are rendered transparent. A three-part differential count assigns cells to categories usually designated: (a) “Granulocytes” or “large cells”; (b) “Lymphocytes” or “small cells”; and (c) “Monocytes,” “mononuclear cells,” or “middle cells.” In theory, the granulocyte category includes eosinophils and basophils, but in practice it is common for an appreciable proportion of cells of these types to be excluded from the granulocyte category and to be counted instead in the monocyte category. Five- to seven-part differential counts classify cells as neutrophils, eosinophils, basophils, lymphocytes, and monocytes and in an extended differential count may also include large immature cells (composed of blasts and immature granulocytes) and atypical lymphocytes (including small blasts). Automated instruments performing three-part or five-to seven-part differential counts are able to “flag” or reject counts from the majority of samples with nucleated red cells, myelocytes, promyelocytes, blasts, and atypical lymphocytes. To a lesser extent, instruments incorporating a three-part differential count, although not capable of enumerating eosinophils or basophils, are able to flag a significant proportion of samples that have an increased number of one of these cell types. Automated differential counters using flow cytometry classify far more cells than is possible with a manual differential count. Automated counts are consequently much more precise than manual counts; however, with certain cell categories—specifically monocytes and basophils—the degree of precision is sometimes less than would be expected for the number of cells counted, indicating that such cells are not always classified in a consistent manner. The accuracy of automated counters is less impressive than their precision. With all types of counters, unusual cell characteristics 75 | P a g e or ageing of a blood specimen can lead to misclassification of cells. Although the majority of samples containing abnormal cells are “flagged,” this is not invariably so; the presence of nucleated red cells, immature granulocytes, atypical lymphocytes, and blasts (even occasionally quite large numbers of blasts) may not give rise to a “flag.” However, human observers performing a 100-cell manual differential count also miss significant abnormalities. In general, automated counts have compared favourably with routine manual counts, especially if the instruments are assigned only two functions—performing differential counts on normal samples and “flagging” abnormal samples. If morphological abnormalities are flagged, microscopic examination of a stained blood film should always be undertaken. In the presence of a significant number of NRBC, the total count is neither a true “WBC” nor a true “TNCC” and the absolute WBC counts calculated from the total will necessarily be somewhat erroneous. Instruments currently in use that count NRBC and correct the WBC for NRBC interference include the Abbott CellDyn 4000, the Sysmex XE2100, and the Beckman-Coulter LH750. Differential counters based on pattern recognition in stained blood films were initially preferred by many haematologists, but they were relatively slow, and because they could count only a small number of cells in a reasonable time, the precision of the automated count was no better than that of a manual count. However, with improved computing technology and with the use of artificial neural networks, such instruments (e.g., DiffMaster, CellVision AB, SE-223 70, and Lund, Sweden) are now capable of providing a useful differential count on blood samples containing abnormal cells. Up to 30 films an hour can be processed and reviewed, and abnormal cells can be reclassified if required. 2.10 New White Cell Parameters Many instruments are able to “flag” the presence of atypical or “variant” lymphocytes by features such as alteration in size and in impedance or light-scattering characteristics. Automated white cell counters can also analyse cell characteristics by novel technologies and identify cell types by features that differ greatly from those used when a blood film is examined visually. It is possible, for example, to identify eosinophils by the ability of their granules to polarize light or to detect a left shift or the presence of blasts by the reduced light scattering of the nuclei of more immature granulocytes. There is also the potential to produce information that is not directly analogous with that available from a manual differential count. Instruments that incorporate a cytochemical reaction give information on enzyme activity expressed as the mean peroxidase activity index (MPXI). An increased MPXI has been observed in infections, in some myelodysplasias and leukaemias, in the acquired immune deficiency syndrome (AIDS), and in megaloblastic anaemia, whereas a reduced MPXI occurs in inherited and acquired neutrophil peroxidase deficiency. It has been suggested that the parameters used for defining leucocyte types might also allow detection of the presence of malaria pigment as a screening test in areas where malaria is prevalent. 76 | P a g e 2.11 PLATELET COUNT Platelets can be counted in whole blood using the same techniques of electrical or electro-optical detection as are used for counting red cells. An upper threshold is needed to separate platelets from red cells, and a lower threshold is needed to separate platelets from debris and electronic noise. Recirculation of red cells near the aperture should be prevented, as pulses produced may simulate those generated by platelets. Three techniques for setting thresholds have been used: (a) Platelets can be counted between two fixed thresholds (e.g., between 2 and 20 fl; (b) Pulses between fixed thresholds can be counted with subsequent fitting of a curve and extrapolation so that platelets falling outside the fixed thresholds are included in the computed count. (c) Thresholds can vary automatically, depending on the characteristics of individual blood samples, to make allowance for microcytic or fragmented red cells or for giant platelets. A new method for platelet counting by flow cytometry has been developed Platelets in a blood sample are labelled fluorescently with a specific monoclonal antibody or combination of antibodies, and by measuring the RBC :platelet ratio the platelet count can be calculated. Suitable antibodies to platelet antigens are CD41, CD42, and CD61. This method using CD41 and CD61 has been adopted by the International Council for Standardization in Haematology as the reference method some instruments now provide an automated immunological platelet count for diagnostic use. Although these instruments can count platelets down to levels of 10 × 109/l or less, it should be noted that precision at these levels is often poor with CVs of 22– 66% being observed and with mean counts differing appreciably between instruments. Factitiously low automated platelet counts may be the result of giant platelets being identified as red cells, EDTA-induced platelet clumping, and satellitism. Misleadingly high platelet counts may be due to markedly microcytic or fragmented red cells, to cell fragments in leukaemia, or to bacteria or fungi. 2.12 Mean Platelet Volume The same techniques that are used to size red cells can be applied to platelets. The calculated mean platelet volume (MPV) is very dependent on the technique of measurement and on length and conditions of storage prior to testing the blood. When MPV is measured by impedance technology, it has been found to vary inversely with the platelet count in normal subjects. If this curve is extrapolated, it has been found that data fit the extrapolated curve when thrombocytopenia is caused by peripheral platelet destruction; however, the MPV is lower than predicted when thrombocytopenia is caused by megaloblastic anaemia or bone marrow failure. The MPV is generally greater than predicted in myeloproliferative disorders, but differentiating essential thrombocythaemia from reactive thrombocytosis on this basis has not been very successful. Other platelet parameters that can be computed by automated counters include the platelet distribution width (PDW), which is a measure of platelet anisocytosis, and the 77 | P a g e “plateletcrit,” which is the product of the MPV and platelet count and, by analogy with the haematocrit, may be seen as indicative of the volume of circulating platelets in a unit volume of blood. The PDW has been found to be of some use in distinguishing essential thrombocythaemia (PDW increased) from reactive thrombocytosis (PDW normal). The plateletcrit does not appear to provide any information of clinical value. 2.13 RETICULOCYTE COUNT Automated reticulocyte counts have been developed by using the fact that various dyes and fluorochromes combine with the RNA of reticulocytes. Following binding of the dye, fluorescent cells can be enumerated using a flow cytometer. Most fully automated blood counters now incorporate a reticulocyte counting capacity so that use of a stand-alone reticulocyte counter is no longer necessary and use of a general purpose flow cytometer is no longer appropriate. An international standard for this method has been published by ICSH. The dyes used in the different systems include auramine O (Sysmex), thiazole orange (ABX), CD4K 530 (Abbott), as well as nonfluorescent dyes such as oxazine 750 (Bayer-Technicon) and the traditional New methylene blue (Beckman-Coulter, Abbott). After staining, it is necessary to separate the reticulocytes from unstained red cells, and, because the dyes also combine with DNA of nucleated cells, these cells must also be excluded. The threshold for this exclusion is determined by the intensity of fluorescence and particle sizing. Although the separation of reticulocytes from mature red cells is not always clearcut, automated reticulocyte counts correlate well with manual reticulocyte counts, although absolute counts may differ because automated counts are dependent on the conditions of incubation and the method of calibrating the instrument. Precision is much superior to that of the manual count because many more cells are counted and the subjective element inherent in recognizing late reticulocytes is eliminated. Potential sources of inaccuracy are the inclusion of some leucocytes and platelets and, less often, Howell–Jolly bodies or malarial parasites in the “reticulocyte” count. Automated reticulocyte counts are fairly stable in blood that has been stored for 1–2 days at room temperature or up to 3–5 days at 4°C. 2.14 Immature Reticulocyte Fraction Fully automated instruments provide a measure of the various degrees of reticulocyte maturation because the most immature reticulocytes, produced when erythropoietin levels are high, have more RNA and fluoresce more strongly than the mature reticulocytes normally present in the peripheral blood. Parameters indicating reticulocyte immaturity have potential clinical relevance. For example, an increase in mean fluorescence intensity indicative of the presence of immature reticulocytes has been noted as an early sign of engraftment following bone marrow transplantation. 78 | P a g e The characteristics of reticulocyte output in different types of anemia’s can be especially appreciated from an output bivariate graph relating fluorescent intensity to reticulocyte count. As described earlier, low total count with a relatively high immature reticulocyte fraction (IRF) is indicative of a repopulating marrow, whereas a reticulocytopenia with low IRF is typical of severe aplastic anaemia or renal failure A high total count with high IRF occurs in acute haemolysis and blood loss, whereas a low to normal total count with a high IRF occurs in dyserythropiesis and in early response to haematinics. The appearance of reticulocytes with high fluorescence also heralds response when severe aplastic anaemia is being treated with immunosuppressive therapy 2.15 CALIBRATION OF AUTOMATED BLOOD CELL COUNTERS The following methods are recommended for calibrating an automated blood cell counter 1. By using fresh normal blood specimens to which values have been assigned for Hb, PCV, RBC, WBC, and platelet count by standardized reference methods 2. By use of a stable calibrant (either preserved blood or a substitute) to which values appropriate for the instrument in question have been assigned by comparison with fresh normal blood 3. By use of a commercial calibrant with assigned values suitable for the instrument in question For reasons of convenience and economy, control materials are commonly used as calibrants; but this practice is not recommended. Such materials are not sufficiently stable to serve as calibrants and their stated values are often approximations that are not assigned by reference methods. They are designed to give test results within a stated range over a stated period rather than a specific result. The procedure for assigning values to fresh blood samples and indirectly to a stable calibrant is as follows: 1. 4 ml blood specimens are obtained from three haematologically normal volunteers and are anticoagulated with K2 EDTA. 2. The Hb value is assigned by using the haemiglobincyanide method and the mean of two measurements. 3. The PCV is assigned by the microhaematocrit method, taking the mean of measurements in four microhaematocrit tubes. 4. The RBC is assigned by performing counts on a single-channel apertureimpedance counter capable of performing a direct cell count; the mean of two dilutions, each counted twice, is used. 79 | P a g e 5. The MCV is assigned by calculation from the RBC and PCV. 6. The WBC is assigned by performing counts on a single-channel apertureimpedance instrument capable of performing direct cell counts; the mean of two dilutions, each counted twice, is used. 2.16 FLAGGING OF AUTOMATED BLOOD COUNTS “Flagging” refers to a signal that the specimen being analysed may have a significant abnormality because one or more of the blood count variables are outside specified limits (usually 2SD) or there is a qualitative abnormality that requires a quality control check and/or additional investigation. This usually includes a blood film review. Although it is theoretically desirable for every blood count to include examination of a stained film, this is being challenged by increasing workloads requiring time- and cost-effective rationalization, as well as by the use of automated analyzers that report differential leucocyte counts on every specimen. Consequently, fewer blood films are being examined microscopically. Thus, a decision of when a blood film should be made, stained, and examined should take account of flagging and the need to ensure analytic reliability. This includes a check of any significant changes from a recent previous count (delta-check), as well as any specific clinical circumstances. The following is a guide to this selection. Blood count request: Is it a first time count or repeat count? First time count: Is it a routine screening test or special category? If Routine: Analyzer report for blood count alone Film required if any flags are signalled If Special category: Film required: 1. Diagnosed blood disease patients 2. Patients receiving radiotherapy and/or chemotherapy 3. Renal disease 4. Neonates 5. Intensive care unit 6. If special tests have also been requested for: infectious mononucleosis, haemolytic anaemia, enzymopathy, abnormal haemoglobins 7. If the clinical details on the request form indicate lymphadenopathy, splenomegaly, jaundice or suggest the possibility of leukaemia or lymphoma 8. Specific requests by clinician Repeat count: Film required: 1. Delta check positive when compared with previous record 2. Any flag occurs in present count 3. On each occasion for patients with known blood diseases, for neonates, and when specifically requested by clinicians 80 | P a g e Module 2 Session 2: Manual techniques Objectives At the end of this session participants will be able to: 1. Estimate hemoglobin concentration 2. Estimate PCV or Hct 3. Estimate total WBC count 4. Estimate platelet count 5. Estimate ESR 6. Estimate reticulocyte count 7. Apply preparation of blood films on slides 8. Explain antiglobulin or coombs test 9. Determine the blood ABO and Rh group Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Mini-lecture, discussion, question & answer, brain storming Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 255 minutes 81 | P a g e 2.2.1. Estimate hemoglobin concentration 2.2.2. Estimate PCV or Hct Mini-lecture The hemoglobin concentration (Hb) may be estimated by measurement of its color, by its power of combining with oxygen or carbon monoxide, or by its iron content Reference range Men =150 +_ 20g/l Women =135 +_ 15g/l The haematocrit ×1000 is about three times the haemoglobin expressed in g/l In conjunction with estimations of haemoglobin and red blood cell count (RBC), it can be used in the calculation of red cell indices. Factors affecting the test: -Factors decerasing microhaematocrit - Factors increasing microhaematocrit Reference rage Men =0.45+_ 0.05(l/l) Women = 0.41+_0.05(l/l) 30 minutes Discussion 30 minutes 82 | P a g e 2.2.3. Estimate total WBC count Question & answers Visual counting of blood cells is an acceptable alternative to electronic counting for white cell, while, it is not recommended for routine red cell counts because the number of cells that can be counted within a reasonable time in the routine laboratory will be too few to ensure a sufficiently precise result Factors affecting the test Range of WBC count in health 4.0–10.0 × 109/l 2.2.4. Estimate platelet count 30 minutes Question & answers 30 minutes Manual counts are used routinely in under-resourced laboratories, and they are still needed even in wellequipped laboratories for blood samples with a significant proportion of giant platelets Factors affecting the test Range of platelet Count 280 ± 130 × 109/l 83 | P a g e Mini-lecture 2.2.5 Estimate ESR 30 minutes 2.2.6. Estimate reticulocyte count Question & answers 2.2.7. Apply preparation of blood films on slides Essentially it is the measurement after 1 hour of the sedimentation of red cells in diluted blood in an openended glass tube of 30 cm length mounted vertically on a stand. Range in health - Men - Women - Pregnancy Factors affecting the test Reticulocytes are juvenile red cells; they contain remnants of the ribosomal ribonucleic acid (RNA) that was present in larger amounts in the cytoplasm of the nucleated precursors from which they were derived Factors affecting the test Range of Reticulocyte Count in Health 50–100 × 109/l (0.5–2 30 minutes Mini-lecture 84 | P a g e Blood films should 30 minutes be made on clean glass slides. Films made on cover glasses have negligible advantages and are unsuitable for modern laboratory practice. Films may be spread by hand or by means of an automated slide spreader, the latter being either a standalone instrument or a component of an automated blood cell counter. 2.2.8. Explain antiglobulin or coombs test Mini-lecture The antiglobulin test is probably the most important test in serology and blood banking DAT IAT 25 minutes Brain storming 2.2.9. Determine the blood ABO and Rh group 20 minutes Materials Method Discrepancies 85 | P a g e Manual Techniques 4.3.1 Hemoglobin Estimation Introduction The hemoglobin concentration (Hb) may be estimated by measurement of its colour, by its power of combining with oxygen or carbon monoxide, or by its iron content. The procedures to be described are all colour or light-intensity matching techniques, which also measure, to a varying extent, any methaemoglobin (Hi) or sulphaemoglobin (SHb) that may be present. Clinical significance This test is done to detect if the patient is suffering from anaemia or rather high Hb Concentration as in polycythaemia. Principle: To measure hemoglobin concentration (Hb), a known volume of carefully mixed whole blood is added to a diluent which lyses red cells to produce a hemoglobin solution; lysis occurs because of the hypotonicity of the diluent. The Hb is then determined from the light absorbance (optical density) of the solution of hemoglobin or its derivative at a selected wavelength. Specimen Venous or free-flowing capillary blood that has been anticoagulated with: ethylenediaminetetra-acetic acid (EDTA). Glassware and equipment EDTA tubes, dispenser or micropipette, test tubes, spectrophotometer or colorimeter. HAEMIGLOBINCYANIDE (CYANMETHAEMOGLOBIN) PROCEDURE 86 | P a g e The haemiglobincyanide (Cyanmethemoglobin) procedure is the internationally recommended procedure for determining the haemoglobin concentration of blood. The basis of the procedure is dilution of blood in a solution containing potassium cyanide and potassium ferricyanide. Haemoglobin, Hi, and HbCO, but not SHb, are converted to HiCN. The absorbance of the solution is then measured in a spectrometer at a wavelength of 540 nm or a photoelectric colorimeter with a yellow–green filter. Reagents: Diluent The original (Drabkin's) reagent had a pH of 8.6. The following modified solution, Drapkin-type reagent, as recommended by the International Committee for Standardization in Haematology, has a pH of 7.0–7.4. It is less likely to cause turbidity from precipitation of plasma proteins and requires a shorter conversion time (3–5 min) than the original Drabkin's solution, but it has the disadvantage that the detergent causes some frothing: Potassium ferricyanide (0.607 mmol/l) 200 mg Potassium cyanide (0.768 mmol/l) 50 mg Potassium dihydrogen phosphate (1.029 mmol/l) 140 mg Nonionic detergent 1 ml Distilled or deionized water To 1 litre The pH should be 7.0–7.4 and must be checked with a pH meter at least once a month. The diluent should be clear and pale yellow in colour. When measured against water as a blank in a spectrometer at a wavelength of 540 nm, absorbance must be zero. If stored at room temperature in a brown borosilicate glass bottle, the solution keeps for several months. If the ambient temperature is higher than 30°C, the solution should be stored in the refrigerator but brought to room temperature before use. It must not be allowed to freeze. The reagent must be discarded if it becomes turbid, if the pH is found to be outside the 7.0–7.4 range, or if it has an absorbance other than zero at 540 nm against water blank. Procedure Make a 1 in 201 dilution of blood by adding 20 μl of blood to 4 ml of diluent, or according to the manufactures instructions Stopper the tube containing the solution and invert it several times. Let the test sample stand at room temperature for at least 5 min (to ensure the complete conversion of haemoglobin to haemiglobinocyanide), and then pour it into a cuvette and read the absorbance in a spectrometer at 540 nm or in a photoelectric colorimeter with a suitable filter, against a reagent blank. The absorbance of the test sample must be measured within 6 hours of its initial dilution. The absorbance of a commercially available HiCN standard (brought to room temperature if previously stored in a refrigerator) should also be compared to a reagent blank in the same spectrometer or photoelectric colorimeter as the patient sample. The standard should be 87 | P a g e kept in the dark, and, to ensure that contamination is avoided, any unused solution should be discarded at the end of the day on which the ampoule is opened. Calculation of Haemoglobin Concentration Preparation of Standard Graph and Standard Table When many blood samples are to be tested, it is convenient to read the results from a standard graph or table relating absorbance readings to haemoglobin in g/l for the individual instrument. This graph should be prepared each time a new photometer is put into use or when a bulb or other components are replaced. It can be prepared as follows: Prepare five dilutions of the HiCN reference standard (or equivalent preparation) (brought to room temperature) with the cyanide–ferricyanide reagent according to the Table below because the graph will be used to determine the haemoglobin measurements, it is essential that the dilutions are performed accurately. Dilutions of haemiglobincyanide (HiCN) reference solution for preparation of standard graph Haemoglobin [*] HiCN volume Tube (%) (ml) Reagent volume (ml) 1 100 (full strength) 4.0 (neat) None 2 75 3.0 1.0 3 50 2.0 2.0 4 25 1.0 3.0 5 0 None 4.0 (neat) * As percent of haemoglobin in reference solution. The haemoglobin concentration of the reference preparation in each tube should be plotted against the absorbance measurement. For example, if the label on the reference preparation states that it contains 800 mg/l, (i.e. 0.8 g/l) and the procedure for haemoglobin measurement uses a dilution of 1:201, the respective haemoglobin concentrations of tubes 1–5 would be 160 g/l, 120 g/l, 80 g/l, 40 g/l, and zero. Using linear graph paper, plot the absorbance values on the vertical axis and the haemoglobin values on the horizontal axis. The points should fit a straight line that passes through the origin. Providing that the standard has been correctly diluted, this provides a check that the calibration of the photometer is linear. From the graph, it is possible to construct a table of readings and corresponding haemoglobin values. This is more convenient than reading values from a graph when large numbers of measurements are made. It is important that the performance of the instrument does not vary and that its calibration remains constant in relation to haemoglobin measurements. To ensure this, the reference preparation should be measured at frequent intervals, preferably with each batch of blood samples. 88 | P a g e Supplementary information Inaccuracy in estimation of Hb due to: The slow conversion of carboxyhemoglobin to methemoglobin leads to overestimation of the Hb if the test is read at 3 minutes, since carboxyhemoglobin absorbs more light at 540 nm than does cyanmethemoglobin. This difficulty can be overcome by prolonging the reaction time to 30 min before reading. The difference between the 5 and 30 min readings can be used as a semiquantitative procedure for estimating the percentage of HbCO in the blood. Spectrophotometers and photometers are both sensitive to the effect of turbidity, which may be caused by a high WBC, high concentrations of lipids or plasma proteins, or non-lysed red cells. Increased turbidity causes a factitiously elevated estimate of Hb. When the WBC is high, turbidity effects are circumvented by centrifugation or filtration of the solution prior to reading the absorbance. When turbidity is due to a high level of plasma protein, it can be cleared by the addition of either potassium carbonate or a drop of 25% ammonia solution. When turbidity is due to hyperlipidemia, a blank can be prepared from the diluent and the patient’s plasma or the lipid can be removed by diethyl ether extraction and centrifugation. Calculation of Haemoglobin Concentration Reference range Haemoglobin Men 150 ± 20 g/l Women 135 ± 15 g/l Units g / l, mg/dl 89 | P a g e 4.3.2 PACKED CELL VOLUME OR HAEMATOCRIT Introduction The haematocrit ×1000 is about three times the haemoglobin expressed in g/l. In conjunction with estimations of haemoglobin and red blood cell count (RBC), it can be used in the calculation of red cell indices. However, its use in under-resourced laboratories may be limited by the need for a specialized centrifuge and a reliable supply of capillary tubes. Clinical significance The packed cell volume (PCV) can be used primarily as a simple screening test for anaemia, as a reference procedure for calibrating automated blood count systems, and as a rough guide to the accuracy of haemoglobin measurements. Principle The centrifuge used for the capillary tubes provides a relative centrifugal force (g) of about 12000 g, and 5 min centrifugation results in precipitation of RBC in the distal end. Specimen Anticoagulated blood sample, because the PCV gradually increases with storage, the test should be performed within 6 hours of collecting the blood sample, but a delay of up to 24 hours is acceptable if the blood is kept at 4°C. Failure to mix the blood sample adequately will produce an inaccurate result. The degree of oxygenation of the blood also affects the result because the PCV of venous blood is ∼2% higher than that of fully aerated blood (which has lost CO2 and taken up O2). To ensure adequate oxygenation and sample mixing, the free air space above the sample should be >20% of the container volume. Glassware and equipment Anticoagulant K2-EDTA tube is recommended, because K3-EDTA causes shrinking of the red cells, reducing the PCV by about 2%. Anticoagulant concentration in excess of 2.2 mg/ml may also cause a falsely low PCV as a result of cell shrinkage. Capillary Tubes Variation of the bore of the tubes may cause serious errors if they are not within the narrow limits of defined specifications that should be met by manufacturers: length 75 ± 0.5 mm; internal diameter 1.07–1.25 mm, wall thickness 0.18–0.23 mm; and bore taper not exceeding 2% of the internal diameter over the entire length of the tube. 90 | P a g e Centrifuge Centrifuges should be checked at intervals (at least annually) by a tachometer for speed and by a stopwatch for timer accuracy. Efficiency of packing should also be tested by centrifuging samples of normal and polycythaemic blood for varying times from 5 to 10 min to determine the minimum time for complete packing of the red cells. Procedure MICROHAEMATOCRIT PROCEDURE The microhaematocrit procedure is carried out on blood contained in capillary tubes 75 mm in length and having an internal diameter of about 1 mm. The tubes may be plain for use with anticoagulated blood samples or coated inside with 1 iu of heparin for the direct collection of capillary blood. The centrifuge used for the capillary tubes provides a centrifugal force of c 12000 g, and 5 min centrifugation results in a constant PCV. When the PCV is greater than 0.5, it may be necessary to centrifuge for a further 5 min. Allow blood from a well-mixed specimen, or from a free flow of blood by skin puncture, to enter the tube by capillarity, leaving at least 15 mm unfilled. Then seal the tube by a plastic seal (e.g. Cristaseal, Hawksley, and Lancing, Sussex). Sealing the tube by heating is not recommended because the seals tend to be tapered and there is the likelihood of lysis. After centrifugation for 5 min, measure the proportion of cells to the whole column (i.e., the PCV) using a reading device. Accuracy of Microhaematocrit The microhaematocrit procedure has an adequate level of accuracy and precision for clinical utility. Attention must be paid to a number of factors that may produce an inaccurate result. Reading The test should be read as soon as possible after centrifugation because the red cells begin to swell and the interface becomes progressively more indistinct. To avoid errors in reading with the special reading device, a magnifying glass should be used. White cells and platelets (the buffy coat) must be excluded as far as possible from the reading of the packed red cells. If a special reading device is not available, the ratio of red cell column to whole column can be calculated from measurements obtained by placing the tube against arithmetic graph paper or against a ruler. Supplementary information Plasma Trapping The amount of plasma trapped between red cells, especially in the lower end of the red cell column, and red cell dehydration during centrifugation generally counterbalance each other, and the error caused by trapped plasma is usually not more than 0.01 PCV units. Thus, in routine practice, it is unnecessary to correct for trapped plasma, but if 91 | P a g e the PCV is required for calibrating a blood cell analyser or for calculating blood volume, the observed PCV should be reduced by a 2% correction factor after it has been centrifuged for 5 min or for 10 min with polycythaemic blood. It is, however, preferable to use the surrogate reference procedure. Plasma trapping is increased in macrocytic anaemias, spherocytosis, thalassaemia, hypochromic anaemias, and sickle cell anaemia; it may be as high as 20% in sickle cell anaemia if all the cells are sickled. Factors affecting the test: Reference range Packed cell volume (PCV) or Haematocrit (Hct) Men 0.45 ± 0.05 (l/l) Women 0.41 ± 0.05 (l/l) Units % or L / L 4.3.3 Total White Blood Cell Count Introduction Visual counting of blood cells is an acceptable alternative to electronic counting for white cell, while, it is not recommended for routine red cell counts because the number of cells that can be counted within a reasonable time in the routine laboratory will be too few to ensure a sufficiently precise result. 92 | P a g e Principle: The principles of manual cell counts, the use of the haemocytometer counting chamber for manually counting white cells and platelets in a known surface area. Clinical significance Some of the common Causes of leucocytosis: Bacterial infections Inflammation and tissue necrosis Metabolic disorders (e.g. uraemia, eclampsia, acidosis, gout) Neoplasms of all types (e.g. carcinoma, lymphoma, melanoma) Acute haemorrhage or haemolysis Drugs (e.g. corticosteroid therapy (inhibits margination): lithium, tetracycline) Chronic myeloid leukaemia, myeloproliferative disease, polycythaemia vera, myelofibrosis, essential thrombocythaemia Treatment with myeloid growth factors (e.g. G-CSF, GM-CSF) Infectious mononucleosis, rubella, pertussis, Infectious hepatitis, cytomegalovirus, HIV, herpes simplex or zoster tuberculosis, toxoplasmosis, brucellosis, syphilis Chronic lymphoid leukaemias Acute lymphoblastic leukaemia Non-Hodgkin's lymphoma (some) Thyrotoxicosis. Some of the common Causes of leucopenia: Selective neutropenia Drug-induced Systemic lupus erythematosus Felty's syndrome Hypersensitivity and anaphylaxis Viral (e.g. hepatitis, influenza, HIV) Fulminant bacterial infection (e.g. typhoid, miliary Tuberculosis) Specimen Venous or free-flowing capillary blood that has been anticoagulated with ethylenediamine tetra-acetic acid (EDTA). Thorough mixing of the blood specimen before sampling is essential for accurate test results. Ideally, tests should be performed within 6 hours of obtaining the blood specimen because some test results are altered by longer periods of storage. However, results that are sufficiently reliable for clinical purposes can usually be obtained on blood stored for up to 24 hours at 4°C. Glassware and equipment Counting Chambers The visibility of the rulings in the counting chamber is as important as the accuracy of calibration, so that chambers with a “metallised” surface and Neubauer or Improved Neubauer rulings are recommended. These have nine 1 mm × 1 mm ruled areas, which, when covered correctly with the special thick cover glass, each contain a volume of 0.1 μl of diluted blood. Coverslips designed for mounting of microscopy preparations must 93 | P a g e not be used with counting chambers. The sample is introduced between the chamber and the coverglass using a pipette or capillary tube, and the preparation is viewed using a ×40 objective and ×6 or ×10 eyepieces. With Neubauer and Improved Neubauer chambers, count the cells in 4 or 8 horizontal rectangles of 1 mm × 0.05 mm (80 or 160 small squares) or in 5 or 10 groups of 16 small squares, including the cells that touch the bottom and left-hand margins of the small squares. Figure 10: Counting chamber Microscope Micropipette Test tube Reagents: Diluent To make the counting of white cells easier, diluted whole blood is mixed with a fluid to lyse the red cells and stain the white cell nuclei deep violet-black. The diluent is 2% (20 ml/l) acetic acid coloured pale violet with gentian violet. Procedure Make a 1 in 20 dilution of blood by adding 0.1 ml of well-mixed blood (lack of adequate mixing is a major source of error) to 1.9 ml of diluent in a 75 × 10 mm plastic (or glass) tube. After sealing the tube with a lid or tightly fitting bung, mix the diluted blood in a mechanical mixer or by hand for at least 2 min by tilting the tube to an angle of about 120 degrees combined with rotation, thus allowing the air bubble to mix the suspension. Fill a clean dry counting chamber, with its coverglass already in position, without delay. This is simply accomplished with the aid of a plastic Pasteur pipette or a length of stout capillary glass tubing that has been allowed to take up the suspension by capillarity. 94 | P a g e Take care that the counting chamber is filled in one action and that no fluid flows into the surrounding moat. Leave the chamber undisturbed on a bench for at least 2 min for the cells to settle, but not much longer, because drying at the edges of the preparation initiates currents that cause movement of the cells after they have settled. The bench must be free of vibrations, and the chamber must not be exposed to draughts or to direct sunlight or other sources of heat. It is important that the coverglass should be of a special thick glass and perfectly flat, so that when laid on the counting chamber, diffraction rings are seen. The coverglass should be of such a size that when placed correctly on the counting chamber the central ruled areas lie in the centre of the rectangle to be filled with the cell suspension. Factors affecting the test: If any of the following filling defects occur, the preparation must be discarded and the filling procedure must be repeated using another clean dry chamber: Overflow into moat Chamber area incompletely filled Air bubbles anywhere in chamber area Any debris in chamber area To obtain a coefficient of variation of 5%, it is necessary to count about 400 cells in practice, it is reasonable to count 100 white cells. To minimise distribution errors, count the cells in the entire ruled area (i.e., 9 × 0.1 μl areas in an Improved Neubauer counting chamber). Counting in only one or two fields results in a wide variance that is reduced as more cells are counted. However, high precision is achieved only when thousands of cells are counted, which is only possible with automated cell counters. Calculation WBC/I Thus, if N cells are counted in 0.1 μl, then the WBC/l is as follows: (e.g., if 115 cells are counted, the WBC is 115 × 200 × 106/l = 23 × 109/l) Range of White Blood Cell Count in Health 95 | P a g e White blood cell count 4.0–10.0 × 109/l Units × 109/l 4.3.4 PLATELET COUNT Introduction Manual counts are used routinely in under-resourced laboratories, and they are still needed even in well-equipped laboratories for blood samples with a significant proportion of giant platelets. However, for all other samples, automated full blood counters produce platelet counts with a precision that is much superior to that of manual platelet counts. Principle: Manual platelet counts are performed by visual examination of diluted, lysed whole blood using a Neubauer or Improved Neubauer counting chamber as for total white cell counts. Clinical significance This test is used for detection of thrombocytosis or thrombocytopenia which occurs in many diseases. Specimen Platelet counts are best performed on ethylenediaminetetra-acetic acid (EDTA)-anticoagulated blood that has been obtained by clean venipuncture. They can also be carried out on blood obtained by skin prick, but the results are less satisfactory than those on venous blood. Skinprick platelet counts are significantly lower than counts on venous blood and less constant; a variable number of platelets are probably lost at the site of the skin puncture. Glassware and equipment Counting Chambers The visibility of the rulings in the counting chamber is as important as the accuracy of calibration, so that chambers with a “metallised” surface and Neubauer or Improved Neubauer rulings are recommended. These have nine 1 mm × 1 mm ruled areas, which, when covered correctly with the special thick cover glass, each contain a volume of 0.1 μl of diluted blood. Coverslips designed for mounting of microscopy preparations must not be used with counting chambers. The sample is introduced between the chamber and the coverglass using a pipette or capillary tube, and the preparation is viewed using a ×40 objective and ×6 or ×10 eyepieces. With Neubauer and Improved Neubauer chambers, count the cells in 4 or 8 horizontal rectangles of 1 mm × 0.05 mm (80 or 160 small squares) or in 5 or 10 groups of 16 small squares, including the cells that touch the bottom and left-hand margins of the small squares. 96 | P a g e Figure11: Counting Chamber Microscope Micropipette Test tube Reagents: 1% ammonium oxalate, which lyses red cells, as a diluent produces a higher and more accurate count than use of formal citrate, which leaves red cells intact. Procedure The diluent consists of 1% aqueous ammonium oxalate in which the red cells are lysed. This procedure is recommended in preference to that using formal-citrate as diluent, which leaves the red cells intact and is more likely to give incorrect results, when the platelet count is low. Before diluting the blood sample, examine it carefully for the presence of blood clots. If these are present, a fresh specimen should be requested because clots will cause the platelet count to be artificially low. Make a 1 in 20 dilution of well-mixed blood in the diluent by adding 0.1 ml of blood to 1.9 ml of ammonium oxalate diluent (10 g/l). Not more than 500 ml of diluent should be made at a time, using carefully clean glassware and fresh glass-distilled or deionised water. If possible, the solution should be filtered through a micropore filter (0.22 μm) and kept at 4°C. For use, a small part of the stock is refiltered and dispensed in 1.9 ml volumes in 75 × 12 mm tubes. Mix the suspension on a mechanical mixer for 10–15 min. Fill a Neubauer counting chamber with the suspension, using a stout glass capillary or Pasteur pipette. Place the counting chamber in a moist Petri dish and leave untouched for at least 20 min to give time for the platelets to settle. Examine the preparation with the ×40 objective and ×6 or ×10 eyepieces. The platelets appear under ordinary illumination as small (but not minute) highly refractile particles if viewed with 97 | P a g e the condenser racked down; they are usually well-separated, and clumps are rare if the blood sample has been skillfully collected. To avoid introducing into the chamber dirt particles, which might be mistaken for platelets, all equipment must be scrupulously clean. Platelets are more easily seen with the phase-contrast microscope. A special, thin-bottomed (1 μm) counting chamber is best for optimal phase-contrast effect. The number of platelets in one or more areas of 1 mm2 should be counted. The total number of platelets counted should always exceed 200 to ensure a coefficient of variation of 8–10%. Calculation Thus, if N is the number of platelets counted in an area of 1 mm2 (0.1 μl in volume), the number of platelets per litre of blood is: Range of platelet Count Platelet count 280 ± 130 × 109/l Factors affecting the test: The errors associated with manual cell counts are technical and inherent. Technical errors can be minimized by avoiding the following: Poor technique in obtaining the blood specimen Insufficient mixing of the blood specimen Inaccurate pipetting and the use of badly calibrated pipettes or counting chambers Inadequate mixing of the cell suspension Faulty filling of the counting chamber Careless counting of cells within the chamber Units × 109/l 98 | P a g e 4.3.5 Erythrocyte Sedimentation Rate Introduction Inflammatory response to tissue injury (the acute-phase response) includes alteration in serum protein concentration, especially increases in fibrinogen, haptoglobin, caeruloplasmin, immunoglobulins (Ig), and C-reactive protein (CRP), and decrease in albumin. The changes occur in acute infection, during active phases of chronic inflammation, with malignancy, in acute tissue damage (e.g., following acute myocardial infarction), or with physical injury. Principle: Essentially it is the measurement after 1 hour of the sedimentation of red cells in diluted blood in an open-ended glass tube of 30 cm length mounted vertically on a stand. Clinical significance Measurement of the acute-phase response is a helpful indicator of the presence and extent of inflammation or tissue damage and response to treatment. The usual tests are estimation of CRP and measurement of the erythrocyte sedimentation rate (ESR); Specimen Either collect venous blood in ethylenediaminetetra-acetic acid (EDTA) and dilute a sample accurately in the proportion of 1 volume of citrate to 4 volumes of blood, or collect the blood directly into the citrate solution. Glassware and equipment The recommended tube is a straight glass or rigid transparent plastic tube 30 cm in length and not less than 2.55 mm in diameter. The bore must be uniform to within 5% throughout. A scale graduated in mm extends over the lower 20 cm. The tube must be clean and dry. Specially made racks with adjustable levelling screws are available for holding the sedimentation tubes firmly in an exactly vertical position. The rack must be constructed so that there will be no leakage of the blood from the tube. Reagents: Diluent prepare a solution of 109 mmol/l trisodium citrate (32 g/l Na3Ca6H5O7.2H2O). Filter through a micropore filter (0.22 mm) into a sterile bottle. It can be stored for several months at 4°C but must be discarded if it becomes turbid through the growth of moulds. Procedure Conventional Westergren Procedure The test should then be carried out on the diluted sample within 4 h of collecting the blood, although a delay of up to 6 h is permissible provided that the blood is kept at 4°C. EDTA blood can be used within 24 h if the specimen is kept at 4°C, provided that 1 volume of 109 mmol/l (32 g/l) trisodium citrate is added to 4 volumes of blood immediately before the test is performed. 99 | P a g e Mix the blood sample thoroughly and then draw it up into the Westergren tube to the 200 mm mark by means of a teat or a mechanical device; mouth suction should never be used. Place the tube exactly vertical and leave undisturbed for exactly 60 min, free from vibrations and draughts and not exposed to direct sunlight. Calculation Read to the nearest 1 mm the height of the clear plasma above the upper limit of the column of sedimenting cells. The result is expressed as ESR = X mm in 1 h. A poor delineation of the upper layer of red cells may sometimes occur, especially when there is a high reticulocyte count. Range in Health There is a progressive increase with age, but older than 70 years it is difficult to define a strictly healthy population for determining normal values. Erythrocyte sedimentation rate ranges in health Age (years) 95% Upper limit (mm in 1h) Men 17–50 10 51–60 12 61–70 14 >70 about 30 Women 17–50 12 51–60 19 61–70 20 >70 about 35 Pregnancy First half 48 (62 if anaemic) Second half 70 (95 if anaemic) In the newborn, the ESR is usually low. In childhood and adolescence, it is the same as for normal men with no differences between boys and girls. It is increased in pregnancy, especially so in the later stages, and independent of anaemia. Factors affecting the test: Modified Procedures Length of Tube 100 | P a g e The overall length of the tube is not a critical dimension for the test provided that it fits firmly in an appropriate holding device. The tube must, however, be long enough to ensure that packing of the cells does not start before the test has been completed. Temp: should be between 18-25 C Hemolysis: affect the rate of sedimentation Plastic Glass Tubes A number of plastic materials (e.g., polypropylene and polycarbonate) are recommended as substitutes for glass in Westergren tubes. Nevertheless, not all plastics have similar properties, and it must be demonstrated that the ESR with the chosen tubes is reproducible and not affected by the plastic. Disposable Glass Tubes Disposable glass tubes should be supplied clean and dry and ready for use. It is necessary to show that neither the tube material nor the manufacturer's cleaning process affect the ESR. Capillary Procedure Short tubes of narrower bore than in the standard tube are available mainly for tests on infants. These are, however, no longer in general use, and it is necessary to establish normal ranges or a correction factor to convert results to an approximation of ESR by the Westergren procedure. Time Sedimentation is measured after aggregation has occurred and before the cells start to pack usually at 18-24 min. From the rate during this time period the sedimentation that would have occurred at 60 min is derived and converted to the conventional ESR equivalent by an algorithm. Sloping Tube Red cells sediment more quickly when streaming down the wall of a sloped tube. This phenomenon has been incorporated into automated systems in which the end-point is read after 20 min with the tube held at an angle of 18 degrees from the vertical. This has been shown to give results comparable to the conventional procedure. Anticoagulant EDTA blood can be used without citrate dilution, at least if packed cell volume (PCV) is below 0.36 (haemoglobin < 110 g/l); less precise results are obtained when the PCV is higher. The readings from undiluted samples must then be adjusted as for the standardised procedure (see below). Because of the biohazard risk of blood contamination inherent in using open-ended tubes, it is now recommended that, where possible, a closed system be used in routine 101 | P a g e practice. Manual procedures are available that avoid transfer of the blood into the sedimentation tube. Automated closed systems use either blood collected in special evacuated tubes containing citrate or EDTA blood. A sample is taken up through a pierceable cap and then automatically diluted in the system if this is required. Some systems use sloping tubes at an angle of 18 degrees to obtain results rapidly, and one model of the Ves-matic (Diesse) also incorporates centrifugation. Whenever a different procedure or tube is planned, a preliminary test should be carried out to check precision and to compare results with those obtained by the standardised procedure described in the following section. Units Mm / hour 4.3.6 RETICULOCYTE COUNT Introduction Reticulocytes are juvenile red cells; they contain remnants of the ribosomal ribonucleic acid (RNA) that was present in larger amounts in the cytoplasm of the nucleated precursors from which they were derived. Ribosomes have the property of reacting with certain basic dyes such as azure B, brilliant cresyl blue, or New methylene blue (see below) to form a blue or purple precipitate of granules or filaments. Principle On exposure of unfixed cells to certain dyes that contains only basic component of the stain, such as brilliant cresyl blue or new methylene blue, the ribosomes are precipitated and stained by the dye, to appear as a reticular network. With these stains red cells stain a pale greenish-blue while the reticulum stains bluish-purple. Clinical significance The number of reticulocytes in the peripheral blood is a fairly accurate reflection of erythropoietic activity, assuming that the reticulocytes are released normally from the bone marrow and that they remain in circulation for the normal time period. Specimen Venous blood that has been anticoagulated with ethylenediaminetetra-acetic acid (EDTA). Thorough mixing of the blood specimen before sampling is essential for accurate test results. Ideally, tests should be performed within 6 hours of obtaining the blood specimen because some test results are altered by longer periods of storage. However, results that are sufficiently reliable for clinical purposes can usually be obtained on blood stored for up to 24 hours at 4°C. Glassware and equipment EDTA tubes, dispenser or micropipette, test tubes, slides, Microscope. 102 | P a g e Reagents Staining Solution Dissolve 1.0 g of New methylene blue or azure B in 100 ml of iso-osmotic phosphate buffer pH 6.5. Procedure Deliver 2 or 3 drops of the dye solution into a 75- × 10-mm plastic tube by means of a plastic Pasteur pipette. Add 2–4 volumes of the patient's EDTA-anticoagulated blood to the dye solution and mix. Keep the mixture at 37°C for 15–20 min. Resuspend the red cells by gentle mixing, and make films on glass slides in the usual way. When dry, examine the films without fixing or counterstaining. The exact volume of blood to be added to the dye solution for optimal staining depends on the RBC. A larger proportion of anaemic blood, and a smaller proportion of polycythaemic blood, should be added than of normal blood. In a successful preparation, the reticulofilamentous material should be stained deep blue and the nonreticulated cells should be stained diffuse shades of pale greenish blue. Films should not be counterstained. The reticulofilamentous material is not better defined after counterstaining, and precipitated stain overlying cells may cause confusion. Moreover, Heinz bodies will not be visible in fixed and counterstained preparations. If the stained preparation is examined under phase contrast, both the mature red cells and reticulocytes are well defined. By this technique, late reticulocytes characterized by the presence of remnants of filaments or threads are readily distinguished from cells containing inclusion bodies. Satisfactory counts may be made on blood that has been allowed to stand (unstained) for as long as 24 hours, although the count will tend to decrease after 6–8 hours unless the blood is kept at 4°C. Counting Reticulocytes An area of film should be chosen for the count where the cells are undistorted and where the staining is good. A common fault is to make the film too thin; however, the cells should not overlap. To count the cells, use the ×100 oil-immersion objective and, if possible, eyepieces provided with an adjustable diaphragm. If eyepieces with an adjustable diaphragm are not available, a paper or cardboard diaphragm, in the centre of which has been cut a small square with sides about 4 mm in length, can be inserted into an eyepiece and used as a less convenient substitute. The counting procedure should be appropriate to the number of reticulocytes present. Very large numbers of cells have to be surveyed if a reasonably accurate count is to be obtained when only small numbers of reticulocytes are present. When the count is less than 10%, a convenient procedure is to survey successive fields until at least 100 reticulocytes have been counted and to count the total red cells in at least 10 fields to determine the average number of red cells per field. Calculation Number of reticulocytes in n fields = x 103 | P a g e Average number of red cells per field = y Total number of red cells in n fields = n ×y Reticulocyte percentage = [x ÷ (n × y)] × 100% Absolute reticulocyte count = % × RBC Thus, when the reticulocyte percentage is 3.3 and the RBC is 5 × 1012/l, the absolute reticulocyte count per litre is as follows: [3.3/100] × 5 × 1012 = 165 × 109 It is essential that the reticulocyte preparation be well spread to ensure an even distribution of cells in successive fields. When the reticulocyte count exceeds 10%, only a relatively small number of cells will have to be surveyed to obtain a standard error of 10%. Factors affecting the test: It is essential that the reticulocyte preparation be well spread and well stained. Other important factors that affect the accuracy of the count are the visual acuity and patience of the observer and the quality and resolving power of the microscope. The most accurate counts are carried out by a conscientious observer who has no knowledge of the supposed reticulocyte level, thus eliminating the effect of conscious or unconscious bias. Range of Reticulocyte Count in Health The range of reticulocyte in adults and children is 50–100 × 109/l (0.5–2.5%). In infants (full term, cord blood) it is 2–5%. Carry out a rough platelet count to determine the approximate concentration, and add an appropriate amount of the suspension to preserved blood. Mix well for 20 min and, with continuous mixing, dispense into sterile containers. Cap and seal. At 4°C, the preparation should have a shelf life of 3-4 months. Before use, resuspend by thorough shaking by hand, followed by mechanical mixing for approximately 15 min. 4.3.7 PREPARATION OF BLOOD FILMS ON SLIDES Introduction Blood films should be made on clean glass slides. Films made on cover glasses have negligible advantages and are unsuitable for modern laboratory practice. Films may be spread by hand or by means of an automated slide spreader, the latter being either a stand-alone instrument or a component of an automated blood cell counter. Clinical significance 104 | P a g e It’s used for diagnosis of various blood diseases. Principle Although we can judge the proportions of red cells and white cells in a tube of sedimented blood, we get far more information if the blood is carefully mixed and a thin layer is spread on a glass slide to form a blood film. The blood cells are then preserved by exposure to the alcohol methanol, a process known as fixation. The fixed film of blood is stained with a mixture of several dyes so that the individual cells can be recognized when they are examined with a microscope. Specimen Blood films can be prepared from fresh blood with no anticoagulant added or from ethylenediaminetetra-acetic acid (EDTA)-anticoagulated blood. Heparinized blood should not generally be used because its staining characteristics differ from those of EDTA-anticoagulated blood. Good films can be made in the following manner, using clean slides, if necessary wiped free from dust immediately before use. Slides should measure 75 × 25 mm and approximately 1 mm thick; ideally, they should be frosted at one end to facilitate labelling, but these are more expensive. Glassware and equipment EDTA tubes, dispenser or micropipette, spreader, slides, Microscope. Reagents Leishman's Stain Weigh out 0.2 g of the powdered dye, and transfer it to a conical flask of 200–250 ml capacity. Add 100 ml of methanol and warm the mixture to 50°C for 15 min, occasionally shaking it. Allow the flask to cool and filter. It is then ready for use, but it will improve on standing. Buffered Water Make up 50 ml of 66 mmol/l Sörensen's phosphate buffer of the required pH to 1 litre with water at a pH of 6.8. An alternative buffer may be prepared from buffer tablets, which are available commercially. Solutions of the required pH are obtained by dissolving the tablets in water. Manual Procedure Spreading Blood Films First, make a spreader from a glass slide that has a smooth end. Using a glass cutter, break off one corner of the slide, leaving a width of about 18 mm as the spreader. A spreader can be used repeatedly unless the edge becomes chipped, but it must be thoroughly washed and dried between films. 105 | P a g e Place a small drop of blood in the centre line of a slide about 1 cm from one end. Then, without delay, place a spreader in front of the drop at an angle of about 30 degrees to the slide and move it back to make contact with the drop. The drop should spread out quickly along the line of contact. With a steady movement of the hand, spread the drop of blood along the slide. The spreader must not be lifted off until the last trace of blood has been spread out; with a correctly sized drop, the film should be about 3 cm in length. It is important that the film of blood finishes at least 1 cm before the end of the slide. The thickness of the film can be regulated by varying the pressure and speed of spreading and by changing the angle at which the spreader is held. With anaemic blood, the correct thickness is achieved by using a wider angle, and, conversely, with polycythaemic blood, the angle should be narrower. The ideal thickness is such that on microscopy there is some overlap of red cells throughout much of the film's length. The leucocytes should be easily recognizable throughout most of the film. With poorly made films the leucocytes will be unevenly distributed, with monocytes and other large leucocytes being pushed to the end and the sides of the spread. An irregular streaky film will occur if the slide is greasy, and dust on the surface will cause patchy spots. The films should be allowed to dry in the air. In humid conditions the films may be exposed to a current of warm air (e.g., from a hairdryer), but this should be in a microbiological safety hood. Labeling Blood Films The film should be labelled immediately after spreading. Write either a laboratory reference number or the name of the patient and the date in pencil on the frosted end of the slide or on the film itself (writing on the thickest part, which is least suitable for microscopic examination). A label written in pencil will not be removed by staining. A paper label should be affixed to the slide later. If blood films are to be stored for future reference, apply the paper label in such a manner that it is easily read when the slides are filed. Fixing Blood Films Dry the films in the air. Leave for 3 min in the fixative this must be done without delay and the films should never be left unfixed for more than a few hours. If films are sent to the laboratory by post, it is preferable that, when possible, they are thoroughly dried and fixed before dispatch. STAINING BLOOD FILMS Romanowsky stains are used universally for routine staining of blood films, and satisfactory results can be obtained. Air dries the film and flood the slide with the stain. After 2 min, add double the volume of water and stain the film for 5–7 min. Then wash it in a stream of buffered water until it has acquired a pinkish tinge (up to 2 min). After the back of the slide has been wiped clean, set it up right to dry. 106 | P a g e When several batches of films are being stained in succession, the staining solution should be renewed at intervals (e.g., after each 50 slides). Loss of staining power is usually the result of precipitation of the eosin Y, and this will result in the nuclei staining blue instead of purple. Carry out a rough platelet count to determine the approximate concentration, and add an appropriate amount of the suspension to preserved blood . Mix well for 20 min and, with continuous mixing, dispense into sterile containers. Cap and seal. At 4°C, the preparation should have a shelf life of 3-4 months. Before use, resuspend by thorough shaking by hand, followed by mechanical mixing for approximately 15 min. 4.3.11 Antiglobulin or Coombs' Test The antiglobulin test is probably the most important test in serology and blood banking. The antiglobulin test (Coombs' test) was introduced by Coombs, Mourant, and Race in 1945 as a method for detecting “incomplete” Rh antibodies (i.e., IgG antibodies capable of sensitizing red cells but incapable of causing agglutination of the same cells suspended in saline) as opposed to “complete” IgM antibodies, which do agglutinate saline-suspended red cells. Coombs' test is divided into direct and indirect antiglobulin tests: In the direct antiglobulin test (DAT), the patient's cells, after careful washing, are tested for sensitization that has occurred in vivo. In the indirect antiglobulin test (IAT), normal red cells are incubated with a serum suspected of containing an antibody and subsequently tested, after washing, for in vitro–bound antibody. The DAT is used to demonstrate in vivo attachment of antibodies to red cells, as in autoimmune hemolytic anemia, alloimmune HDN, and alloimmune hemolysis following an incompatible transfusion. The IAT has wide application in blood transfusion serology, including antibody screening and identification and cross-matching. DAT: A spin tube technique is recommended for the routine antiglobulin test. The test should be carried out in glass tubes. Plastic tubes are not recommended because they may adsorb IgG, which could neutralize anti-IgG of the antiglobulin reagent. Use a blood sample in EDTA anticoagulant. If a cold-reacting autoantibody is present, the patient's red cells should be washed three times in a large volume of saline warmed to 37°C to wash off cold antibodies and obtain a smooth suspension of cells. There is no risk of washing off adsorbed complement components. However, the washing process should be accomplished as quickly as possible and the test should be set up immediately afterward because bound warm antibody occasionally elutes off the cells when they are washed and falsenegative results may be obtained. “Saline” refers to 9 g/l NaCl buffered to pH 7.0. DAT Method:Make 5% suspension of red cells that have been washed three times in saline. If failed to wash the red cells properly then the antihuman globulin antisera may be neutralized by immunoglobulins or complement in the surrounding serum or plasma and cause a false negative result. 107 | P a g e Add 1 drop of the cell suspension to 2 drops of anti-human globulin reagent. Centrifuge for 1 minute at 150g. Examine for agglutination after gently re-suspending the button of cells. A concave mirror and good light help in macroscopic readings. If the result appears to be negative, confirm this microscopically. 108 | P a g e Figure 12: Coombs Test 109 | P a g e 4.3.12 ABO & Rh Group The test used to determine the blood ABO and Rh group Materials 1- Slide 2- Anti-A Monoclonal sera 3- Anti-B Monoclonal sera 4- Anti-D Monoclonal sera 5- EDTA blood Method 123456- Add one drop of each colored anti-sera on the slid To each anti-sera add one drop of EDTA blood Mix the blood with anti-sera Rotating the slide by hand many times read the result within 2-5 mintes Record the result If Rh negative, test it by tube method: A. Add one volume of antiD sera to test tube. B. Add one volumeof 2% red cells suspension. C. mix suspension by traping the tube. D. leave the suspension undisturbed for 15 min and read result. Discrepancies A- False Positive 1- Rouleaux formation 2- Auto-immune hemolytic anemia B- False Negative Occurred when the anti-sera is impotent or expired 110 | P a g e Module three: Serology Module Objectives: At the end of this module the participant will be able to: 1. Apply serological tests Modules Sessions Session 1: RPR Test, TPHA Test, Widel Test, and Rose Bengal Test. Session 2: CRP Test, ASO latex slide agglutination Test, RF, Toxoplasmosis Test, Infectious mononucleosis Test, Rota Virus Latex Test, and Pregnant Test Evaluation/ Assessment Questions and answers, participants’ summaries, trainer’s evaluation Estimated Training Time 5 hours 111 | P a g e Module 3 Session 1: RPR Test, TPHA Test, Widel Test, and Rose Bengal Test Objectives At the end of this session participants will be able to: 1. Understand RPR Test 2. Understand TPHA Test 3. Understand Widel Test 4. Understand Rose Bengal Test Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Mini-lecture, question & answers, discussion-lecture Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 115 minutes 112 | P a g e Session plan -1- Objectives 3.1.1. Understand RPR Test 3.1.2. Understand TPHA Test 3.1.3. Understand Widel Test 3.1.4. . Understand Rose Bengal Test for brucellosis Content Methodology Principle Material Procedure Interpretation Limitation Mini-lecture Principle Material Procedure Interpretation of results Question & answers Principle Material Procedure Introduction Most species of pathogenic for human Principles Materials Procedure Limitation of the procedure 25 minutes 30 minutes Question & answers 30 minutes Discussion-lecture 30 minutes 113 | P a g e 5. Serology 5.1Rapid Plasma Reagin (RPR) TEST Principle Syphilis is a chronic venereal infection caused by the spirochaete micro-organism Treponema pallidum. As the organism cannot be cultured on artificial media, diagnosis of syphilis depends on the detection of specific antibodies by serological tests in combination with clinical findings. The RPR test is “non-treponemal” in that the antibodies detected are not specific for T. pallidum, although their presence in patient’s serum or plasma is strongly associated with infection by the organism. This test measures antibody (IgG and IgM) produced in response to lipoidal material released from damaged host cells as well as to lipoproteinlike material released from the spirochaetes. These antibodies tend to disappear after successful treatment of the infection. The RPR test consists of modified VDRL antigen containing microparticulate carbon, which aggregates in the presence of reagin type antibodies in serum or plasma, indicating a positive result. The aggregation can be read macroscopically. Non-reactive samples typically appear as a smooth non-aggregated pattern, which may form buttons in the centre of the test area . Material 1. Carbon antigen reagent 2. Positive Control 3. Negative Control 4. Disposable Test Slides 5. Disposable Pipette Stirrers (pipstirs) 6. Dispenser 7. Needle 8. Specimen collection container 9. Timer 10. Automatic card rotator (100 rpm) 11. (0.85%) physiological saline (semi quantitative test only). 12. Test tubes for sample dilution (semi quantitative test only). 114 | P a g e PROCEDURE a. 1. 2. 3. 4. 5. 6. 7. 8. 9. b. 1. 2. 3. 4. 5. 6. Qualitative Test Allow all reagents, controls and samples to reach room temperature before use. Draw the sample into the pipstir taking care not to transfer any cellular elements. Hold the pipstir over a test card circle and allow one drop (50µl) of specimen to fall onto the test card. It is important to hold the dispenser in a vertical position whilst dispensing the sample. Spread the specimen evenly over the entire test circle using the mixing (broad) end of the pipstir. Shake the vial of carbon antigen reagent to ensure even mixing. Attach the needle to the dispenser. Withdraw sufficient carbon antigen for the number of tests being performed. Keeping the dispenser in a vertical position allow one drop to fall onto the specimen. Do not mix. Return unused antigen from the dispenser to the glass vial. Rotate the tile for 8 minutes preferably on an automatic rotator at 100 rpm. Read and interpret results macroscopically in good light. Semi Quantitative Test Prepare doubling dilutions of the sample from the undiluted specimen to 1:32 using physiological saline. Mix well. Using the pipstirs , place one drop (50µl) of each dilution onto a separate test card circle. Using the mixing (broad) end of the pipstir spread each dilution evenly over the test circle, starting at the highest dilution (1:32), proceeding to the lowest (1:2). Continue as from 5 in the Qualitative Test. After 8 minutes rotation, read the test and note the last circle in the dilution series that has a positive result. If the highest dilution tested (1:32) is reactive, proceed with a further dilution series by preparing doubling dilutions of the sample from 1:32 to 1:512 using physiological saline. Mix well and continue as from 2 in the semi quantitative test. INTERPRETATION Quality Control It is recommended that the kit positive and negative controls are run with each batch of test specimens. For the assay to be valid the positive control provided should give a strong positive pattern and the negative control provided should give a clearly negative result. Results 115 | P a g e Qualitative Test Positive result Reactive (positive) samples display characteristic agglutination ranging from slight (weak-reactive) to intense (reactive). A strong positive reaction is seen as large aggregates in the centre of the test circle. Weakly positive reactions are seen as small aggregates around the edge of the test circle. Negative result Negative results show no aggregates. The carbon antigen either remains in a smooth suspension or forms a distinct button. Figure 13: Appearance of Positive and Negative RPR Results Semi Quantitative Test Results may be graded from strong to non-reactive and the titre expressed as the reciprocal of the last dilution showing a positive reaction. 1. Strong Reactive (SR): Large clumps of carbon particles with a clear background. 2. Reactive (R): Large clumps of carbon particles, more dispersed than strong reactive. 3. Weak Reactive (WR): Small clumps of carbon particles with light grey background. 4. Trace Reactive (TR): Slight clumping of carbon particles, typically seen as a button of aggregates in the centre of the test circle or dispersed around the edge of the test circle. 5. Non-Reactive (NR): A smooth grey pattern or a button of non-aggregated carbon particles in the centre of the test circle. 116 | P a g e Reactive samples should be recorded as antibody positive and must be subjected to further tests to determine the presence or absence of specific anti-Treponemal antibody. Limitations As with all reagin tests the RPR test may give a small proportion of false positive results. Diseases such as infectious mononucleosis, leprosy, lupus erythematous, vaccinia and viral pneumonia can cause such reactions. Reactive RPR test specimens should be tested with further serological tests (i.e. TPHA and FTA-abs) since, as with any serological procedure, the diagnosis should not be made on a single reactive result. As with other serological tests, the RPR test cannot distinguish between syphilis and other pathogenic Treponemal infections e.g. Yaws. 5.2 TPHA(Treponema pallidum Haemagglutination Assay ) TEST Principle Serological screening tests for syphilis using cardiolipin and lecithin as antigens are simple to perform but biological false positive reactions occur frequently because the tests use non-treponemal antigens. TPHA reageants are used to detect human serum antibody to T.pallidum by means of an indirect haemagglutination (IHA) method. Preserved avian erythrocytes are coated with antigenic components of pathogenic T.pallidum . These Test Cells agglutinate in the presence of specific antibodies to T.pallidum, and show characteristic patterns in microtitration plates. Any non-specific reactions occurring are detected using the Control Cells, which are avian erythrocytes not coated with T.pallidum antigens. Non-specific reactions may also be absorbed out using these Control Cells. Antibodies to non-pathogenic treponemes are absorbed by an extract of Reiter’s treponemes, included in the cell suspension. Test results are obtained in 45-60 minutes and the cell agglutination patterns are both easily read and long lasting. TPHA test has been shown to be a convenient and specific test for the diagnosis of treponemal infection, having a specificity and a sensitivity comparable to that of the FTA-ABS test (Fluorescent treponemal antibody absorption Test) . It requires minimum laboratory equipment and is very simple to perform. Material 1. Test cells; preserved avian erythrocytes sensitised with T.pallidum antigen. 2. Control cells;preserved avian erythrocyte. 3. Diluent. 117 | P a g e 4. Positive control serum; (prediluted 1:20)This will give an equivalent titre of 1/640:/2560 in the quantitative test. 5. Non-reactive control serum; (prediluted 1:20). 6. Accurate pipettes for delivering 10,25,75 and 190 microlitres. 7. U-Well microtitration plates. Procedure Qualitative method Each sample requires 3 wells of a microtitration plate. 1. 2. 3. 4. Add 190µl of diluent to Well 1. Add 10µl serum to Well 1. Using a micropipette, mix contents of Well 1 and transfer 25µl to Wells 2 and3. Ensure that the Test and Control Cells are thoroughly resuspended. Add 75µl of control cells to Well 2. Add 75µl of Test Cells to Well 3. 5. Tap the plate gently to mix the contents thoroughly. 6. Incubate 45-60 minutes at room temperature. ( Keep the plate away from heat, direct sunlight and any source of vibration). 7. Read results. Results are stable for 24hrs if the plate is covered and the above precautions are observed. Quantitative test Each sample requires 8 Wells of a microtitration plate. Labelled A through to H. 1. Add 25µl of diluent to Wells B to H inclusive. 2. Transfer 25µl of 1:20 serum dilution from screening test to Wells A and B. 3. Take 25µl of diluted serum from Well B and serially dilute from Wells B to H inclusive in 25µl aliquots, discarding 25µl of diluted serum from Well H. 4. Ensure that the Test Cells are thoroughly resuspended. Add 75µl of Test cells to wells A to H inclusive. This will give a dilution of serum of 1/ 80 in Well A through 1/ 10240 Well H. 5. Shake the plate gently to mix the contents thoroughly. 6. Incubate for 45-60 minutes at room temperature.( Keep the plate away from heat, direct sunlight and any source of vibration). 7. Read results. Results are stable for 24hrs. if the plate is covered and the above precautions are observed. Table1: TPHA results RESULTS TEST CELLS CONTROL CELLS Strong Positive Full cell pattern covering the bottom of the well. No agglutination tight button 118 | P a g e Weak Positive Cell pattern covers approx. 1/3 of well bottom No agglutination tight button Indeterminate Cell pattern shows a distinctly open centre No agglutination tight button Negative Cells settled to a compact bottom, typically with a small clear centre. No agglutination tight button Positive reaction Non-specific * Non-specific absorption Positive reaction 1. Add 100µl of test serum to a small tube then add 400µl of Control Cells. Mix well and stand for 1 hour. 2. Centrifuge for 15 minutes at 1000 rpm and test the supernatant by the qualitative method. Note: The sample is now at 1/5, this should be taken into account when preparing the dilutions. If the result is repeatedly non-specific the sample should be tested by another method eg . FTA-ABS. INTERPRETATION OF RESULTS Strong positive reactions may show some folding at the edge of the cell mat. When the Test well is positive , the Control well should be observed. The Control cells should settle to a compact button. They should not be used as a comparison for Non-Reactive serum patterns since the Control Cells will give a more compact pattern than the Test Cells. Agglutination in the Control well indicates the presence of non-specific agglutinins in the sample, the test should be reported as INVALID. A serum that gives this result may be absorbed using the Control Cells as detailed under Non-specific absorption. A doubtful reaction with Test Cells should be reported as INDETERMINATE. This result may indicate a low level of antibody in early primary syphilis or yaws. This sample should be first retested in the qualitative test then a further sample should be tested at a later date to determine whether or not there is a rising titre. It is also advisable to perform another confirmation test (FTA-ABS) to complete the profile of the test serum. 5.3 Widal Test ((agglutination test)) Introduction 119 | P a g e The widal agglutination test for the diagnosis of the enteric fever, The patients' serum is tested directly for antibody by entire a slide of tube method, These test are either qualitative and semi quantitative. The rapid slide test is used primarily as a screening procedure especially useful when large numbers of sera must be examined. The tube test should be used to confirm positive result obtained by the slide test. The degree to which agglutination occurs depends upon the concentration of the antigen, the amount of antibody present, the composition of the salt solution and the temperature. Sera from normal patients may show positive agglutination with widal antigen due the previously immunization, past infection, or the present of antibodies to related antigen. titer detected as a result of active infection or recent immunization. It is therefore, necessary to evaluate two or more serum samples, taken at 3 to 5 days intervals after the onast of disease. a progressive increase in titers is the prime evidence of recent infection or immunization. Martials 1. antigens: Antigen are nonviable bacteria cells(salmonella)in 0.5% phenolized saline and stained 2. Serological pipettes, 0.2 ml with 0.1 ml gradation. 0.1 ml capacity 3. Class agglutination slide with bow 4. Wooden applicator sticks 5. Physiological saline (0.85% NaCl) 6. Rotatory shaker (if available) Procedure: - Specimen collection: Collect 5-10 ml of blood in the sterile plain tube without anticoagulant. Allow the blood to clot for 20-30 min, serum maybe kept for up to 24 hours at 2.8 c. If sample to be kept for longer periods , it should be frozen, do not refreeze one it thawed serum The antigen should be allowed to warm to room temperature prior to use in test. A- Slide method 1- deliver 0.08,0.04,0.02,0.01 and 0.005 ml of test serum on to separate ring, using 0.2 ml pipette 2- Shake the antigen vial in order to thoroughly mix the contents. 3- Add one drop of antigen to each circle, mix antigen and serum, using a new tooth pick or applicator for each circle. 4- Rock the slide for 1-3 min (lock the kit procedure) or using rotatory shaker if available. 120 | P a g e 5- The degree of agglutination observe in each ring is estimated as follow. 6- Dilution giving a 2+ agglutination is the end point or titer of that serum. Note: storage kit: Widal kit, store at 2-8°C, antigen are ready for use as supplied Measure titer: The titer is the reciprocal of the highest final dilution procedure a 2 +agglutination Table 2:Record agglutination Degree of agglutination 100% back ground clear to slightly hazy 4+ 75% back ground slightly cloudy 50% back ground moderately cloudy 2+ 25% back ground cloudy 1+ 3+ None negative Table 3: Determination of antibody titer The titer is reciprocal of the highest dilution producing (2+) agglutination Serum ml correlation dilution 0.08 1:20 0.04 1:40 0.02 1:80 0.01 0.005 1:160 1:320 121 | P a g e Table 4: Example of slide test are shown in the following table Slide test results Slide test result Serum ml readying 0.08 0.04 0.02 0.01 0.005 1:20 1:40 1:80 1:160 1:320 dilution Serum titers or endpoint Agglutination reaction Serum No 1 ++++ ++++ ++++ ++ - 1:160 Serum No 2 ++++ +++ ++ - - 1:80 Serum No 3 +++ ++ ++ _ _ 1:80 Note: 1-If auto-agglutination of antigen is suspected (Show by low power microscope) the vial antigen is unstable and should be discarded. 2-patints, occasionally fail to develop any serum agglutinin The chart below give approximate indication of the significant of serum titers. Table 5: indication of significant serum titers Serum agglutinins Disease Febric antigen widal antigen appear maximum titer and significance 122 | P a g e Typhoid fever Para typhoid fever salmonella infection Salmonella O group D Salmonella O group A Salmonella O group B 7-10 Days 3-5 week 1:80 (in early stage)=suspicious 1:160 and rising= strong suspicious Those characterized by prolonged fever and typhoid like symptoms present antibodies of titers similar to above Note: 1-The minimal titers defined as positive of the O typhoid antigen and H antigen must be determined for individual geographic areas. 2-Cross-reaction occur with both non Styphi group dsalmonella and salmonella from other groups 3-A single elevated titer for (O) equal to or greater than (1:320) or H equal to or greater then (1:640) is considered positive. 5.4 Rose Bengal Test for Brucellosis Introduction Human brucellosis –undulant or Malta fever: Brucellosis is systemic infection in which any organ or system of body can be involved. Human become infected by three primary routes 1-ingestion of infected unpasteurized animal milk products 2-inhaltion of infected aerosolized particles 3-Direct contact with infected animal parts through rupture of skin and mucous membrane including the conjunctiva. Brucellosis is one of the most commonly reported bacterial infection acquired in laboratory , within laboratory aerosolizing is primary mechanism of the transmission, so it is required biosafety level 3 precaution for isolation in Lab . Most species of pathogenic for human are: 1- Br abroteus from cows 2- Br melitens from goats and sheep 3- Br suis from pigs (USA) 4- Br canis from dog Definitive diagnosis of brucellosis require isolation of the organism in culture of blood , bone marrow or other tissues. 123 | P a g e the cultures , should be incubated in 5% to 10 % CO2 in humidified atmosphere incubated for 3 weeks before discarded as negative. The mean way of diagnosis of brucellosis is by serological test. Become of the difficulty of isolating the organism (serological test) the serum agglutination test (SAT) is widely used and detected antibodies for Br abroteus and Br melitensis. Rose Bengal test (agglutination test) for brucellosis it is remain an inexpensive sensitive and specified test for acute case , but it is not useful in following up of patients or in diagnosis relapses . Principle The rose Bengal an agglutination test reaction used for the diagnosis of brucellosis. The patients’ serum is tested directly for antibody by either a slide or tube method. The test are qualitative and semi qualitative. A number of antigens are available commercially for use is the rapid slide test. The test is performed by mixing serum and antigen in ruled squired on a glass slide. This test is widely used and detected antibodies to Brucellosis aborteas, Br. Melitensis. In case of a cute infection a titer of 1:160 or greater in rapid slide method are consider diagnosis if this result fits the clinical and epidemiologic findings. Materials: 1. Antigen Brucellosis aborteas, nonviable. Bacterial cells in 0.05% phenolized saline and stained. 2. Serological pipettes 0.2 ml with 0.1 ml graduation. 0.1 ml capacity 3. Class agglutination slide with row 4. Wooden applicator sticks 5. Physiological saline(0.85% NaCl) 6. Rotator shaker if available Procedure Specimen collection Collect 5-10 ml of blood in the sterile plain tube without anticoagulant. Allow blood to clot for 20-30 mint, serum may be kept for up to 24 hours at 2-8 C° e . If samples to be kept for longer period, it should be frozen don’t refreeze once themed serum A1. 2. 3. The antigen should be allow to warm to room temperature prior to use in test Slide method. delivers 0.08,0.04,0.02,0.01 and 0.005 ml of test serum on to separate ring using 0.2 ml pipette. Shake the antigen vial in order to thoroughly mix the contents. Add one drop of antigen to each circle mixer antigen and serum , using a new tool pick or applicator for each circle. 124 | P a g e 4. Rock the slide for 1-3 min (lock the kit procedure) or using rotatory shaker if available. 5. The degree of agglutination observe in each ring is estimated as follow. Record agglutination Degree of agglutination 100% back ground clear to slightly hazy 75% back ground slightly cloudy 50% back ground moderately cloudy 25% back ground cloudy None 4+ 3+ 2+ 1+ negative Note: Storage kits Rose Bengal kit store at 2-8C° antigen are ready for use as supplied Table 6: Determination of antibody titer The titer is reciprocal of the highest dilution producing (2+) agglutination Serum Ml correlation dilution 0.08 1:20 0.04 1:40 0.02 1:80 0.01 0.005 1:160 1:320 The serum dilation giving a 2+ agglutination is the end point or titer of the serum. Measure titer is reciprocal of the highest final dilution producing (2+) agglutination Example of rose bagel test result are shown in the flowing table Table 7: Examples of Rose Bengal results Slide test result 0.08 0.04 0.02 0.01 0.005 Serum titers or endpoint 125 | P a g e Serum (ml) readying 1:20 1:40 1:80 1:160 1:320 dilution Agglutination reaction Serum No 1 ++++ ++++ ++++ ++ - 1:160 Serum No 2 ++++ +++ ++ - - 1:80 Serum No 3 +++ ++ ++ _ _ 1:80 Limitation of the procedure 1- The serum agglutination test SAT measure both antibodies IgG and IgM in serum of patient 2- After cure the antibodies for brucellosis, usually persistent for more than one year 3- Use 2-mercaptoethanol (detect IgG only) to identify chronic or relapse Brucellosis cases. 4- Any titer high than 1:40 with 2-mercaptoethanol lgG indicative active infection (i.e. relapses or chronic infection). 5- A single titer of greater than 160 or more is considered significant. 6- Prozone phenomena may give false negative result which is possible because of the high antibody concentration so serum dilution is recommended to avoid this. 7- False positive reaction may result from cross-reaction with antibodies of cholera, yersinia or francisella. 8- False negative and false positive reaction can be avoided by routinely dilution the serum beyond at 1:320 126 | P a g e Module 3 Session 2: CRP Test, ASO latex slide agglutination Test, RF, Toxoplasmosis Test, Infectious mononucleosis Test, Rota Virus Latex Test, and Pregnant Test Objectives At the end of this session participants will be able to: 1. Understand CRP Test 2. Understand ASO latex slide agglutination Test 3. Understand RF 4. Understand Toxoplasmosis Test 5. Understand Infectious mononucleosis Test 6. Understand Rota Virus Latex Test 7. Understand Pregnant Test Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Mini-lecture, question & answers, discussion-lecture Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 190 minutes 127 | P a g e Session plan -2- 128 | P a g e Objectives 3.2.1. Understand CRP Test 3.2.2.Understand ASO latex slide agglutination Test 3.2.3. Understand RF Content Principle Material Reagent preparation Procedure Results and interpretation Principle Material and reagents Procedure 3.2.4. Understand Toxoplasmosis Test Principle Material Specimen collection and preparation Reagent preparation Assay procedure Results and interpretation Qualitative method Semi-Quantitative method Principle of test Materials Method Manual wash procedure Methodology Mini-lecture 25 minutes Question & answers 20 minutes Mini-lecture 30 minutes Discussion- lecture 45 minutes 129 | P a g e 3.2.5. Understand Infectious mononucleosis Test 3.2.6. Understand Rota Virus Latex Test Reagents of infectious mononucleosis test Methods Results and interpretation in reports Question & answers Principle Materials Method Result and interpretation Question & answers Rapid test for detection of human chorionic gonodotrophin in urine Direct hGG latex pregnancy kit 3.2.7.Understand Pregnant Test 20 minutes 20 minutes Discussion- lecture 30 minutes 130 | P a g e 131 | P a g e 5.5 C-REACTIVE PROTEIN ( CRP) TEST PRINCIPLE C-Reactive Protein (CRP) in patient’s sera has been found in association with acute infections, necrotic conditions and a variety of inflammatory disorders. There is a strong correlation between serum levels of CRP and the onset of the inflammatory process. Monitoring the levels of CRP in patient’s sera indicates the effectiveness of treatment and the assessment of patient recovery. CRP latex particles are coated with antibodies to human CRP. When the latex suspension is mixed with serum containing elevated CRP levels on a slide, clear agglutination is seen within 2 minutes. MATERIAL 1- Suspension of polystyrene latex ( approximately 1%) particles coated with AntiCRP antibodies. 2- Positive Control. Serum containing CRP antibodies. 3- Negative Control. Serum free of CRP antibodies. 4- Stirrers 5- Plastic slide 6- Micro-pipettes capable of dispensing 50μl. 7- Isotonic saline (0.9% NaCI) REAGENT PREPARATION o o All reagents should be brought to room temperature (20 C to 25 C) and mixed gently to resuspend latex prior to use. Do not induce foaming. The test slide should be thoroughly cleaned before use as traces of detergent or prior specimen may affect the result. Recommended cleaning procedure: 1. Used cards must be immediately immersed in a disinfectant solution. Follow disinfectant manufactures guidelines. 2. The reaction circles must be physically rubbed with non-abrasive material to ensure removal of possible adhering particles. 3. Thoroughly rinse in purified water. 4. Allow reaction card to dry. 132 | P a g e 5. Spray cards with a 70% alcohol solution. 6. Allow the alcohol to evaporate prior to re-use. PROCEDURE Qualitative Method 1. Allow kit reagents and patient serum to come to room temperature. 2. Transfer one drop (50μl) of patient’s serum to the test circle on the slide. 3. Shake the latex reagent, then using the dropper provided, add one drop of suspension to the test circle. 4. Mix the drops using a disposable stirrer ensuring coverage of the test circle with the mixture. 5. Gently and evenly, rock and rotate the test slide for 2 minutes whilst examining the test slide for agglutination. Semi Quantitative Method 1. Using isotonic saline prepare serial dilutions of the patients serum (1/2, 1/4, 1/8, 1/16, 1/32, 1/64 and so on) 2. Transfer one drop (50μl) of each serum dilution to the test circle on the slide. 3. Shake the latex reagent, then using the dropper provided, add one drop of suspension to the test circle. 4. Mix the drops using a disposable stirrer ensuring coverage of the test circle with the mixture. 5. Gently and evenly, rock and rotate the test slide for 2 minutes whilst examining the test slide for agglutination. RESULTS AND INTERPRETATION Examine the test slide under a strong light source after 2 minutes. Kit controls or known level value samples should be tested with each test run. The kit negative control should give a negative result after 2 minutes. The kit positive control should give a positive result at a titre of 1/4 +/- one double dilution after 2 minutes. If levels of controls or users known samples do not give expected results, test results must be considered invalid. Qualitative Method A positive result is indicated by the obvious agglutination pattern of the latex, in a clear solution. A negative result is indicated by no change in the latex suspension on the test slide. Latex CRP kit has a detection limit of 6mg/litre of CRP in the patient’s serum. Positive results will be obtained at a CRP serum concentration above 6mg/litre and negative results will be obtained at 6mg/Litre and below. Semi-Quantitative Method 133 | P a g e The serum CRP concentration can then be calculated approximately by multiplying the dilution factor (i.e 2, 4, 8 or 16) by the detection limit, i.e. 6, to give the number of mg/Litre concentration e.g. if the agglutination titre appears at 1/8 the approximate serum CRP concentration is 8 x 6 = 48 mg/Litre. Titres of 500 mg/Litre have been detected with CRP with no prozone ( hook ) effect. 5.6 ASO latex slide agglutination test Principle Streptococcal infections are very common in all populations, and a high percentage of people will have antibodies against streptococci. The b-haemolytic group A streptococci produce two haemolysins: oxygen-labile streptolysin O and oxygen-stable haemolysin S. Only reduced (non-oxidized) streptolysin O is immunogenic and is used for the test. The antistreptolysin O test is based on the fact that patients with Streptococcus pyogenes (group A streptococcal) infections develop antibodies that inhibit the haemolytic activity of streptolysin O. The antibodies are usually long-lasting and a single increased titre is not an indication of a current infection. Only a fourfold or greater rise in titre on successive serum samples taken 10–14 days apart should be considered indicative of recent infection. This test is mainly used in the diagnosis of acute rheumatic fever, acute glomerulonephritis and other post-streptococcal diseases. There are two types of commercial antistreptolysin O test kits: The ASO latex slide agglutination test is used to screen sera to identify those with raised ASO titres (200 IU or higher). The ASO tube test is a haemolysis inhibition test that is used to determine ASO antibody titre in serum samples that are positive in the ASO latex slide agglutination test. Atitre of less than 50 IU does not confirm the diagnosis of acute rheumatic fever. Materials and reagents 1- Disposable cards, with 6 wells each Disposable dropper 2- Positive control serum 3- Sensitized latex reagent (with streptolysin O) 4- Applicator sticks Procedure 1- Dilute the serum 1: 20. (Or according to kit literature). 2- Place 1 drop of the serum solution in a well on the disposable card. 3- Use a new dropper to add 1 drop of sensitized latex reagent. 134 | P a g e 4- Use an applicator stick to mix the two drops and spread them over the entire well. 5- Examine for agglutination within 2 minutes. A positive reaction appears as a fine agglutination within 2 minutes. A negative reaction shows no agglutination. 5.6 Rheumatoid Factor (RF) PRINCIPLE Rheumatoid Factor (RF) is found in sera of patients with Rheumatoid Arthritis and is believed to be IgM antibodies directed against the patient’s own immunoglobulin G. RF is a rapid latex agglutination test kit for the detection of (RF) in human serum. RF latex particles are coated with specially purified human gamma globulin, When the latex suspension is mixed with serum containing elevated RF levels on a slide, clear agglutination is seen within 2 minutes. RF has a detection limit of 8 IU/ml of RF in the patient serum . Material 1- Suspension of Polystyrene latex particles ( approximatly 1.25% ) coated with suitably modified Fc fraction of IgG in stabilizing buffer. 2- Positive Control. Serum containing Rheumatoid Factor antibodies. Working Strength. 3- Negative Control. Serum free of Rheumatoid Factor antibodies. 4- Stirrers 5- Plastic slide 6- Micropipettes capable of dispensing 50 μl. 7- Isotonic saline (0.9% NaCI) SPECIMEN COLLECTION AND PREPARATION Obtain a sample of venous blood from the patient and allow a clot to form and retract. Centrifuge clotted blood sample and collect clear serum. Fresh serum samples are required. Do not use haemolysed, contaminated or lipaemic serum for testing as this will adversly affect the results. o o Serum may be stored at 2 C to 8 C for up to 48 hours prior to testing. If longer storage is o required, store at –20 C for up to 6 weeks. Thawed samples must be mixed prior to testing. Do not repeatedly freeze-thaw the specimens as this will cause false results. REAGENT PREPARATION 135 | P a g e o o All reagents should be brought to room temperature (20 C to 25 C) and mixed gently prior to use. Do not induce foaming. The test slide should be thoroughly cleaned before use as traces of detergent or prior specimen may affect the result. Recommended Cleaning procedure: 1- Used cards must be immediately immersed in a disinfectant solution. Follow disinfectant manufactures guidelines. 2- The reaction circles must be physically rubbed with non-abrasive material to ensure removal of possible adhering particles. 3- Thoroughly rinse in purified water. 4- Allow reaction card to dry. 5- Spray cards with a 70% alcohol solution. 6- Allow the alcohol to evaporate prior to re-use. ASSAY PROCEDURE Qualitative Method 1. Allow kit reagents and patient serum to come to room temperature. 2. Transfer 50μl of patient’s serum to the test circle on the slide. 3. Shake the latex reagent, then using the dropper provided, add one drop of suspension to the test circle. 4. Mix the drops using a disposable stirrer ensuring coverage of the test circle with the mixture. 5. Gently and evenly, rock and rotate the test slide for 2 minutes whilst examining the test slide for agglutination. Semi Quantitative Method 1. Using isotonic saline prepare serial dilutions of the patients serum (1/2, 1/4, 1/8, 1/16, 1/32, 1/64 and so on) 2. Transfer 50μl of each serum dilution to the test circle on the slide. 3. Shake the latex reagent, then using the dropper provided, add one drop of suspension to the test circle. 4. Mix the drops using a disposable stirrer ensuring coverage of the test circle with the mixture. 5. Gently and evenly, rock and rotate the test slide for 2 minutes whilst examining the test slide for agglutination. 136 | P a g e RESULTS AND INTERPRETATION Examine the test slide under a strong light source after 2 minutes. Kit controls or known level value samples should be tested with each test run. The kit negative control should give a negative result after 2 minutes. The kit positive control should give a positive result at a titre of 1/4 +/- one double dilution after 2 minutes. If levels of controls or users known samples do not give expected results, test results must be considered invalid. QUALITATIVE METHOD A positive result is indicated by the obvious agglutination pattern of the latex, in a clear solution. A negative result is indicated by no change in the latex suspension on the test slide. Positive results will be obtained at a RF serum concentration of 8 IU/ml or more and negative results will be obtained at a RF concentration below 8 IU/ml. SEMI – QUANTITATIVE METHOD The serum RF concentration can then be calculated approximately by multiplying the dilution factor (i.e 2, 4, 8 or 16) by the detection limit, i.e. 8, to give the number of IU/ml concentration e.g. if the agglutination titre appears at 1/8 the approximate serum RF concentration is 8 x 8 = 64 IU/ml. Titres of 1074 IU/ml have been detected with Avitex RF with no prozone ( Hook ) effect. 5.7 Toxoplasmosis Test Toxoplasma IgG ELISA Introduction Toxoplasma gondii is an intracellular protozoan parasite with a worldwide distribution. Although cats are the definitive host, human infection results from ingestion of contaminated soil, careless handling of cat litter, ingestion of raw or undercooked meat or transmission from mother to foetus through the placenta. When a seronegative woman becomes infected with T. gondii during pregnancy, the organism is often transmitted to the foetus. Infection during the first trimester may lead to spontaneous abortion, stillbirth, or overt disease in the neonate. The Toxoplasma IgG kit is a rapid ELISA designed for the qualitative or quantitative detection of IgG antibodies to Toxoplasma gondii in human serum. Principle of the test 137 | P a g e Diluted serum or plasma specimens (1:100) are incubated for 20 minutes to allow specific antibodies to T. gondii to bind to the antigencoated wells. After washing away unbound antibodies and other serum constituents, T. gondii specific IgG is detected using rabbit anti-human IgG conjugated to horseradish peroxidase. After 20 minutes incubation, unbound conjugate is removed by washing, and TMB enzyme substrate is added for 10 minutes. A blue colour develops if antibodies to T. gondii are present. Addition of stop solution gives a yellow colour and the optical densities of controls, standard(s) and samples are measured using a microplate reader. Materials 1. Microplate 96 wells in 12 X 8 break-apart strips, pre-coated with T.gondii purified antigens enriched for P30 antigen 2. Reagent 1: Sample Diluent 100mM Tris-buffered saline, pH 7.2 with antimicrobial agent, 10ml, (blue), concentrate (x10) 3. Reagent 2: Wash Buffer 100mM Tris-buffered saline with detergent, pH 7.2, 100 ml, concentrate (x10) 4. Reagent 3: Conjugate (peroxidase conjugated rabbit anti-human IgG), 12 ml, (red), ready to use 5. Reagent 4: TMB Substrate, 12 ml, ready to use 6. Reagent 5: Stop solution, 12 ml, ready to use 7. Standards1: (for quantitative assays), 15 IU/ml, 50 IU/ml; 150 IU/ml (blue), ready to use 8. Standard1: (for qualitative assays) 8 IU/ml, (yellow), ready to use 9. Positive control1: 100 IU/ml (red), 1ml, ready to use 10. Negative control: 1 ml (green), 1ml, ready to use 11.Distilled or de-ionised water Equipment 12345- 10mm X 60mm tubes for dilution, pipettes 10μl, 100μl, 1000μl; repeating dispenser 100μl, microplate reader with 450nm filter, microplate washing device. 138 | P a g e Samples Only freshly drawn and properly refrigerated sera or plasma should be used in this assay. Avoid haemolysed, lipemic or bacterial contaminated sera. Sera should be stored at 2-8ºC for no longer than 5 days. If delay in testing is anticipated, store test sera at –20ºC. Avoid multiple freeze-thaw cycles. Method Ensure that all materials are at room temperature before beginning the procedure. We recommend that the standards and the controls are always run in duplicate. Samples may be run singly or in duplicate. 1. Assemble the number of strips required for the assay. 2. The sample diluent X10 concentrate contains 0.09% sodium azide as preservative. Prepare sufficient working strength diluent for the assay run. However, if the working strength diluent is to be stored for more than 1 week, add sodium azide (0.9g/L). Store unused sample diluent concentrate and dilute sample diluent at 2 – 8oC. Dilute the Sample Diluent (Reagent 1) 1:9 in distilled water to make sufficient buffer for the assay run e.g. add 10ml sample diluent concentrate to 90 ml water. 3. Dilute patient samples 1:100 (e.g. 5μl serum plus 0.5 ml diluent). It is important to dispense all samples and controls into the wells without delay. Therefore ensure that all samples are ready to dispense. 4. For qualitative determinations, dispense 100 μl of the negative control, the 8 IU/ml standard, the positive control and the diluted patient sample into the wells. For quantitative determinations, use sample diluent as 0 IU/ml and additionally dispense the 15 IU/ml, 50 IU/ml and 150 IU/ml standards. 5. Place the strips into the incubation bag provided and incubate for 20 minutes at room temperature. During all incubations, avoid direct sunlight and close proximity to any heat sources. 6. Dilute the Wash Buffer (Reagent 2) 1: 9 in distilled water to make sufficient buffer for the assay run e.g. add 50ml wash buffer concentrate to 450ml water. The diluted wash buffer is stable for two months at 2 - 8°C. 7. After 20 minutes, decant or aspirate the well contents and wash the wells 3 times using an automatic plate washer or the manual wash procedure (see below). Careful washing is the key to good results. Blot the wells on absorbent paper before proceeding. Do not allow the wells to dry 139 | P a g e Out . Manual Wash Procedure: Empty the wells by inversion. Using a multi-channel pipette or wash bottle, fill the wells with ash buffer. Empty by inversion and blot the wells on absorbent paper. Repeat this wash process two more times. 8. Dispense 100μl of Conjugate (Reagent 3) into each well. This reagent is colour coded red. Keep all pipettes and other equipment used for Conjugate ompletely separate from the TMB Substrate reagent! Incubate the wells for 20 minutes in the incubation bag at room temperature. 9. After 20 minutes, discard the well contents and carefully wash the wells four times with wash buffer. Ensure that the wells are completely washed. Blot the microplate on absorbent paper to remove final drops of wash fluid. Do not allow the wells to dry out. 10. Using a repeating dispenser, rapidly dispense 100μl of TMB Substrate (Reagent 4) into each well. Incubate the plate for 10 minutes. 11. Add 100μl of Stop Solution (Reagent 5) to each well. To allow equal reaction times, the stop solution should be added to the wells in the same order as the TMB Substrate. 12. Read the optical density in a microplate reader within 10 minutes. Interpretation Qualitative determinations Negative samples: OD < 8 IU/ml OD Positive samples: OD >/= 8 IU/ml OD Quantitative determinations Plot the optical densities of the standards against their respective concentrations. Draw a line to join the points. Read the concentrations of unknowns from this graph. Concentrations below 8 IU/ml are considered negative; concentrations above 8 IU/ml are considered positive for anti-toxoplasma IgG. A negative result indicates no current or previous infection with T.gondii. Such individuals are presumed to be susceptible to primary infection. However see Limitations below. A positive result indicates a current or previous infection with T. gondii. 140 | P a g e 5.8 Infectious Mononucleosis test Principle Is a qualitative determination of the nonspecific heterophile antibodies that result from primary infection by Epstein – Barr Virus and causing the clinical presentation of Infectious mononucleosis. The IM- Latex is a slide agglutination test also can get semi-quantitative detection of Heterophile antibodies . Latex particles coated with antigenic extract of beef erythrocyte membranes and are agglutinated when mixed with samples containing IM heterophile antibodies. Materials and reagents Preparedness: Reagents Table 8: Reagents of Infectious Mononucleosis Test Latex Latex particles coated with antigenic extract of beef erythrocytes membranes , phosphate buffer, pH 7.2. Sodium azide , 0,95 g/L. Control +ve Human serum with anti – IM antibodies titer ≥ 1/4 . Sodium azide , 0.95g/L Control -ve Animal serum . Sodium azide , 0.95g/L Disposable slides Storage: when stored tightly closed at 2-8 oC do not freeze. (according to kit literature) Samples : Fresh serum . Stable 7 days at 2-8 oC or 3 months at – 20 oC. Samples with presence of fibrin should be centrifuged. Do not use highly hemolized or lipemic samples. Equipment : 1- Mechanical rotator with adjustable speed at 80-100 r.p.m. 2- Centrifuge. 3- Automatic micropipette Methods: Qualitative Method : 1- Allow reagents and samples to reach room temperature. 141 | P a g e 2- Place 50 ul of the sample and one drop of each Positive and Negative controls into separate circles on the slide test. 3- Swirl the IM – Latex reagent gently before using and add one drop ( 50ul) next to the samples to be tested. 4- Mix the drops with stirrer , spreading them over the entire surface of the circle . Use different stirrers for each sample. 5- Place the slide on a mechanical rotator at 80-100 r.p.m. for 2 minutes .False positive results could appear if the test is read later than two minutes. Semi quantitative method: 1- Make serial two ford dilutions of the sample in 9 g/L saline solution. 2- Proceed for each dilution as in the qualitative method. Results and Interpretations in reports: Examine macroscopically the presence or absence of visible agglutination immediately after removing the slide from the rotator. The presence of agglutination indicates a titer ≥ 1/28 of anti IM heterophil antibodies by the Davidson method. The titer in the semi- quantitative method is defined as the highest dilution showing a positive result. The following are the limitations of the test: 1- False positive results may be obtained in some geographical areas where the horse serum is used as a prophylactic measure (vaccination). Also this could be seen in patients with leukemia, Burkitts Lymphoma, Pancreatic carcinoma, viral hepatitis, CMV infections and others. 2- False negative results also encountered and in such Patients either repeat testing after interval of several days to get a high heterophil antibody titer or look for specific antibodies against viral structural antigens like anti VCA IgM . Quality Control: Positive and Negative controls are recommended to monitor the performance of the procedure, as well as the comparative pattern for a better result interpretation. 5.9 Rota Virus Latex Test Principle of the method and clinical significance: Rapid latex agglutination assay for the detection of rotavirus in faecal samples this virus has been shown to be principle causative agent of gastro-enteritis. Patients may harbor up to 108 virus particles per gram of faeces. Materials and reagents Preparedness: 142 | P a g e Material insert in kit: Test reagent latex, control negative ,Positive bovine rotavirus control inactivated ( ready to use ),5 x concentrated extraction buffer pH 7.2,Agglutination slides ,pipette Specimen collection and storage: Prepare a 10% suspension of the faecal sample by adding 0.1 g /0.1 ml of sample to 1 ml of extraction buffer in screw capped vial. Mix well and stand in room temperature for 2 minutes. Specimen may be stored 24 hours at the time of the test .If storage is more than 24 hour the specimen should be stored at -20 oC in freezer . Safety warnings: Do not pipette by mouth, use disinfectant 70% alcohol, waste must be treated as biohazardous and incinerated. Method: 123456- Add 10 ml of extraction buffer to 40ml de-ionize water. Add 2 gms of faecal sample to 2 ml of extraction buffer. Mix well on vortex mixer. Stand at room temperature for 10 minutes. Centrifuge test sample for 10 minutes about 800 g. Place one drop of the supernatant from the faecal sample onto the circle of test slide and use the 2 circle for control reagent. 7- Add one drop of control latex reagent next to the drop of faecal sample on circle 1. 8- Add one drop of test latex reagent next to drop of faecal sample on circle 2. 9- Spread the control latex reagent and test latex reagent in circle 1, 2 by disposable pipette. 10- Gently tilt the test slid backward and forward for 2 minutes. Results and Interpretations in reports: 1- Positive result is indicated by the visible agglutination of the latex particles which occur within few seconds. 2- Negative result is indicated by milky appearance without any visible aggregation of the latex particles. 5.10 PREGNANCY TEST 5.10.1 Rapid test for detection of human Chorionic Gonadotrophin in Urine Human chorionic gonadotrophin (hCG), a glycoprotein hormone secreted by viable placental tissue during pregnancy, is excreted in urine approximately 20 days after the last menstrual period. The levels of hCG rise rapidly reaching peak levels after 60-80 days. The appearance of hCG in urine soon after conception and its rapid rise in concentration makes it an ideal marker for the early detection and confirmation of pregnancy. Test kit utilizes the principle of Immunochromatography, a unique two-site 143 | P a g e immunoassay on a membrane. As the test sample flows through the membrane assembly within the test device in place of the dipstick, the coloured monoclonal anti-hCGcolloidal gold conjugate complexes with the hCG in the sample. This complex moves further on the membrane to the test region where it is immobilised by the monoclonal anti-hCG coated on the membrane, leading to the formation of a pink coloured line which confirms a positive test result. Absence of this coloured line in the test region indicates a negative test result. The unreacted conjugate, unbound complex, if any, and the colloidal gold conjugated rabbit IgG moves further along the membrane and are subsequently immobilised by the goat anti-rabbit IgG coated on the control region forming a pink line. This control line serves to validate the test results. SPECIMEN COLLECTION AND PREPARATION Urine samples collected at any time may be used, however, it is recommended that to maximize hCG concentration, the first voided morning specimen should be used. The urine should be collected in a clean dry container (plastic or glass) which must be free from detergent. Urine specimens should be as fresh as possible and it is preferable to test within 24 hours of collection. The sample may be stored for longer periods (72 hours) prior to use, if stored, store at 2oC to 8oC. Filtration or centrifugation is generally not necessary for urine used in this test, however, if a sample is very turbid, centrifugation or filtration may be necessary. (The use of supernatant from turbid samples allowed to sediment naturally prior to use may negate the need for sample preparation – this does not affect the hCG concentration.) REAGENT PREPARATION Devices and samples should be brought to room temperature (20 to 25) °C and mixed gently prior to use. In case the pouch has been stored at 4°C to 8°C, allow at least 30 minutes for the device to come to room temperature. Check the color of the desiccant. It should be blue. If it has turned colorless or faint blue, discard the device and use another device. ASSAY PROCEDURE 1. Open the pouch and remove the device. Once opened, the device must be used immediately. 2. Dispense two drops of urine specimen into the sample well „S‟ using the dropper provided. 3. Read the results at the end of fifteen minutes for serum or five minutes for urine. RESULTS AND INTERPRETATION Negative: Only one colored line appears on the control region „C‟ only 144 | P a g e Positive: A distinct colored line appears on the control region „C‟ and on the test region “T”. Figure 14: Results of PT The test should be considered invalid if no line appears. Repeat the test with a new device. Depending on the concentration of hCG in the specimen, positive results may appear as early as 30 seconds. Negative results must be confirmed only at the end of fifteen minutes for serum or five minutes for urine. 5.10.2 DIRECT hCG LATEX PREGNANCY KIT Detectable levels of Chorionic Gonadotropin (hCG) in urine start at 5 mIU/ml during the first week of gestation and rises to 100,000 mIU/ml at 2 to 3 months. The hCG level doubles approximately every 2.2 days during the first trimester1. Values decline from 10% to 15% of peak concentrations during 2nd and 3rd trimesters2. Direct hCG Latex kit contains one reagent of latex particles coated with monoclonal antibodies to hCG. The reagent is mixed with the urine samples. MATERIALS 1. Latex reagent. 2. Positive and negative controls. 3. Reaction slide and stirring sticks. SPECIMEN COLLECTION AND PREPARATION Generally, the first morning urine contains the highest concentration of the hCG hormone and therefore, it is more recommended for testing. However, urine collected at other periods can also be used. The urine in this case should have been kept in 2-8°C and used within 72 hours from collection time. PROCEDURES 1. Bring reagents to room temperature. 145 | P a g e 2. Place 50μl of pa�ent urine, one drop positive and one drop negative controls into different circles of the slide. 3. Add one drop of latex reagent directly to each sample. 4. Mix using the supplied sticks and spread the mixture over the entire circle. 5. Gently rock the slide. Agglutination may be observed after two minutes. Direct light source may help to observe the results. READING THE RESULT Presence of agglutination within two minutes indicates positive reaction. Lack of agglutination within two minutes indicates negative reaction. 146 | P a g e Module four: Bacteriology Module Objectives: At the end of this module the participant will be able to: 1. Apply bacteriological tests Modules Sessions Session 1: General urine examination and general stool examination Session 2: Urine culture, throat swab, and nasal swab Session 3: Smart tests, preparation of media, and staining smears Evaluation/ Assessment Questions and answers, participants’ summaries, trainer’s evaluation Estimated Training Time 10 hours 147 | P a g e Module 4 Session 1: General urine examination and general stool examination Objectives At the end of this session participants will be able to: 1. Explain macroscopical examination of urine 2. Detect and estimate glucose and protein in urine 3. Detect bilirubin in urine 4. Detect ketones bodies in urine 5. Detect abnormal elements in urine 6. Explain macroscopical examination of stool 7. Explain microscopical examination of stool Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Mini-lecture, discussion, brain storming, question & answers, discussion-lecture Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 230 minutes 148 | P a g e Session plan -1- 149 | P a g e Objectives 4.1.1.Explain macroscopical examination of urine 4.1.2.Detect and estimate glucose and protein in urine Content Introduction Appearance Odor Reaction ( PH ) Principle Method Detection of glucose in urine Detection and estimation of protein in urine 4.1.3.Detect bilirubin in urine Introduction Clinical significance Method Methodology Mini-lecture 30 minutes Discussion 30 minutes Brain storming 30 minutes Question & answers 4.1.4.Detect ketones bodies in urine Introduction Principles Materials Method Result 30 minutes Discussion-lecture Microscopical examination Colour 4.1.5.Detect abnormal elements in urine 4.1.6.Explain 60 minutes Question & answers 150 | P a g e macroscopical examination of stool 4.1.7.Explain microscopical examination of stool Consistency Pus Mucus Method Intestinal protozoa Identification of cysts Importance of cysts 20 minutes Mini-lecture 30 minutes 151 | P a g e 6. Bacteriology 6.1 General urine examination Introduction: The examination of urine provides a wide variety of useful medical information regarding the disease involving the kidney and lower urinary tract . both functional (physiologic ) and structural (anatomic disorders of the kidney and lower urinary tract my be elucidated . and diagnostic .monitoring, we believe laboratory urine tests will remain an essential part of clinical medicine The basic routine analysis consist of 4 parts : specimen evaluation , gross (physical) examination , chemical screening , and sediment examination Clinical significance Examination of urine is a fundamental investigation in patients in whom kidney disorders or infections of the urinary tract are suspected. There are also many patients who exhibit no clinical symptoms, but in whom previously unrecognized urinary tract infections can be diagnosed by urine examination Collection of urine specimens Containers for the collection of urine should be wide-mouthed, clean and dry. And we can also be used the adhesive bag for infants .If the urine specimen has to be transported for any length of time it should contain an appropriate preservative to prevent bacterial overgrowth or hatching of viable ova The specimen can be preserved for microscopic examination of the deposit by adding 8–10 drops of formaldehyde, 10% solution per 300 ml of urine. Urine preserved in this way is not suitable for other tests. Urine to be examined under the microscope must be freshly passed into a clean dry vessel. A midstream urine specimen is the most useful. Urine stored in a refrigerator may contain an excess of precipitated salts and will not be suitable for microscopy principle the elements of routine urinalysis include macroscopical examination the evolution of physical characteristics ( color, odor, and specific gravity ) pH and chemical examination ( protein , glucose. Keton bodies, bilirubin, urobilinogen. Bile pigment and 152 | P a g e bile salt) and microscopic inspection of centrifuge sediment for R.B.C pus, cast. crystal. etc.. Material( glassware & Equipment): 1- centrifuge 2- Microscope 3- Urine cup 4- conical centrifuge tube 5- slides 6- cover slide 7- Watch glasses 8- Dropper 9- Forceps 10- Indicator paper of limited pH range: for the 5.0–7.0 range and for the 6.0–8.0 range. 11- Test tube 12- burner 13- Urinometer 14- Pasteur pipette REAGENTS 12345- 20 % 5-sulfosalicylic acid Ehrlich reagent Acetic acid Lougal iodine Dipstick strip (reagent strip): should be considered as a first choice because of its practical, easy and cost effective. 6.1.1 MACROSCOPICAL EXAMINATION OF URINE Appearance Urine is normally clear straw-yellow in color. More concentrated urine may appear dark yellow, the presence of blood cells or excess salts may make the urine appear cloudy. Pigments from bile substances may make the urine appear deep yellow or brown. Urine can occasionally appear colorless. Report the appearance as clear or cloudy, colorless, pale yellow, deep yellow or brown. 153 | P a g e Color Urine varies in appearance, depending principally upon a body's level of hydration, as well as other factors. Normal urine is a transparent solution ranging from colorless to amber but is usually a pale yellow. In the urine of a healthy individual the color comes primarily from the presence of urobilin. Urobilin in turn is a final waste product resulting from the breakdown of heme from hemoglobin during the destruction of aging blood cells. Colorless urine indicates over-hydration, generally preferable to dehydration (though it can remove essential salts from the body). Colorless urine in drug tests can suggest an attempt to avoid detection of illicit drugs in the bloodstream through over-hydration. Colorless very dilute urine caused by polyuria, diabetes insipidus Dark yellow urine is often indicative of dehydration. Yellowing/light orange may be caused by removal of excess B vitamins from the bloodstream. Certain medications such as rifampin and phenazopyridine can cause orange urine. Reddish urine is termed hematuria, a symptom of a wide variety of medical conditions may be caused by porphyria (not to be confused with the harmless temporary pink or reddish tint caused by beeturia). Dark orange to brown urine can be a symptom of jaundice, rhabdomyolysis, or Gilbert's syndrome. Black or dark-colored urine is referred to as melanuria and may be caused by a melanoma. Pinkish urine can result from the consumption of beets. Greenish urine can result from the consumption of asparagus. Milky caused by lipiduria Blue urine stains can be caused by blue diaper syndrome Odor Normally with aromatic odor. Abnormally: Offensive odor due to pus increase. Acetone odor due to ketones increase ( ketonuria). Reaction (PH) 154 | P a g e Principle Colored indicator paper is dipped in the urine (or placed in a watch glass and a few drops of urine are added to it). The color changes according to the PH. The paper is then compared with a standard control chart giving the corresponding pH value. Method The urine specimen must be tested within 1 hour of collection 1- Place a strip of universal indicator paper in a watch glass, let a few drops of fresh urine fall from the dropper on to the paper alternatively, dip the test paper directly into the urine in the receptacle. 2- Pick the strip of paper up with forceps. Compare the color obtained with those shown on the standard chart .Read off the pH unit given for the color that matches the test paper most closely. 3- According to the result obtained, select a strip of indicator paper for the corresponding limited range. For example, if the pH is 6, use indicator paper for the range 5.0–7.0. If the pH is 7 or more, use indicator paper for the range 6.0– 8.0. The pH of urine is normally about 6.0 (range 5.0–7.0). Acid pH values (4.5– 5.5) are observed in some forms of diabetes, muscular fatigue and acidosis. Alkaline pH values (7.8– 8.0) are common in patients with infections of the urinary tract and in people on a vegetarian diet. Determination of the pH of urine is useful for the identification of crystalline Detection of Glucose in urine Introduction: Glucose may appear in urine at different blood glucose level , varying in individuals blood level, Glomerular, blood flow, tubular reabsorption rate and urine flow influence its appearance. Glucosuria usually occur when blood level is more than 180 to 200 mg/dl Principle Glucose is the most commonly found sugar substance in urine, particularly in diabetic patients and patients suffering from chronic renal failure. method Glucose in urine can be detected using a urine dipstick, the dipsticks are placed into the urine and immediately removed. They are then compared with a comparison chart after an appropriate time that is also specified on the chart 155 | P a g e The color changes observed on the dipstick will give a semi-quantitative estimation of the amount of substance present. This can be reported as negative, Trace , +(160-195) , ++( >200) , +++ (250-300) . According to the read of glucose strip or as an approximate value of the concentration of the substance tested for. Dipsticks must be stored according to the manufacturer’s instructions Detection and estimation of protein Principle: Protein is not normally found in urine, this is because kidneys ensure that large molecules such as protein remain in the blood. However, the kidneys sift out the smaller impurities and expel them through the urine. In case some protein does get through, the body usually re-absorbs it and uses it as an energy source. However, if there is too much protein in the blood, then some amount of protein will be present in the urine. This can happen even if the kidneys are functioning properly Elevated protein levels are observed in the urine of patients with: urinary Schistosomiasis chronic renal disease pyelonephritis diabetes mellitus systemic disorders (lupus erythematosus) multiple myeloma However, orthostatic proteinuria, a form of functional proteinuria usually seen in young men, which occurs on standing up and disappears on lying down, has no pathological significance METHOD Urine for Albumin test done by one of the following: acetic acid test 1. Prepare 1 ml of urine in a test tube then heat gently till ebullition 2.If the solution becomes turbid that indicates the presence of albumin or amorphous urate. So you must put acetic acid for insurance if the turbidity precipitated so it is amorphous urate, if still turbid so it is albumin in urine. Sulfosalicylic acid test 1-To approximately 3ml of supernatant urine in test tube and one equal amount of 3%SSA invert in the mix 2- Let to stand exactly 10 minute 156 | P a g e 3-Invert again twice Rapid test Protein can also be detected using a urine dipstick 1- Observe the degree of precipitation and grade the results according to the following: Table 9: Degree of Precipitation Negative No turbidity Trace perceptible + Distinct turbidity but no discrete granulation ++ Turbidity with granulation but no flocculation +++ Turbidity with granulation and flocculation ++++ Clumps of precipitated protein or solid precipitate Specific gravity clinical significance urinalysis is a parameter commonly used in the evaluation of kidney function and can aid in the diagnosis of various renal diseases ( eg diabetes insipidus). principle Specific gravity (which is directly proportional to urine osmolality which measures solute concentration) measures urine density, or the ability of the kidney to concentrate or dilute the urine over that of plasma. Dipsticks are available that also measure specific gravity in approximations. Most laboratories measure specific gravity with a refractometer Specific gravity between 1.002 and 1.035 on a random sample should be considered normal if kidney function is normal. Since the specific gravity of the glomerular filtrate in Bowman's space ranges from 1.007 to 1.010, any measurement below this range indicates hydration and any measurement above it indicates relative dehydration Method The Urinometer vessel is filled three fourth full with urine ( minimum volume of urine 15 ml) The urinometer is inserted with spinning motion Make sure that is floating freely ( which reading the urinometer be sure that it is not touching the sides or the bottom of cylinder avoid surface bubble read a bottom of the meniscus 157 | P a g e we can identifying the specific gravity by using dipstick Bilirubin Introduction Bilirubin, a product of hemoglobin catabolism, is characterized by its distinctive yellow pigment. The presence of bilirubin in urine is always abnormal. In most healthy individuals the amount of conjugated bilirubin excreted is not detected by the strips. In cases when bilirubin is elevated and is conjugated, it will be detected by the test strip. It is important to note that unconjugated bilirubin cannot be excreted by the kidneys because it is bound to albumin and is not soluble in water. In the liver, bilirubin combines with glucuronic acid through the action of a glucuronyl transferase to form water soluble bilirubin diglucuronide. Under normal circumstances, conjugated bilirubin passes from the bile duct and then to the intestinal tract. Intestinal bacteria reduce conjugated bilirubin to urobilinogen. Approximately half of the urobilinogen is excreted in the feces; most of the other half is recirculated through the liver. A small amount of urobilinogen bypasses the liver and is excreted in the urine Normally bilirubin is not found in a routine urine test . this test is done to detect abnormally high urine concentration of direct (conjugated ) bilirubin and help to identify the cause of jaundice . Clinical significance The presence or absence of bilirubin in urine must be correlated with serum bilirubin test, the specimen appearance is dark with yellow foam Detection Bilirubin in urine 1. Prepare 1 ml of urine in a test tube then put 2 -3 drops Iodine on the wall of test tube gently. 2. A violet ring appeared on the surface of urine 3. Shake the tube, then solution becomes violet or brownish 4- if violet ring appeared on the surface of urine mean positive result urobilinogen test Urobilinogen test is directly associated with the function of liver and any disorder or infection related to this organ can be traced in the urobilinogen test normal specimen 158 | P a g e contain small amount of urobilinogen (0.1 to 1 Ehrlich units per dl of urine) this test done to aid diagnosis of extra hepatic obstruction such as blocking of the common bile duct and to aid differential diagnosis of hepatic and pre hepatic. method Urobilinogen Analysis 1234- Add 2.5ml of afresh specimen of urine into a tube Add o.25ml of Ehrlich reagent Allow to stand for 5 minute A tea color of the urine indicate urobilinogen is present in increased amounts . A fine pink or brown color indicates that urobilinogen present in normal amount. We can also be use the dipstick to identifying the urobilinogen in urine The test for urobilnogen is based on the Ehrlich Aldehyde Reaction. Pdimethylaminobenzaldehyde in an acid medium with a color enhancer reacts with urobilinogen to form a pink-red color. The urine chemical reagent strip reactivity increases with increasing temperature. The optimum temperature for testing is 22° 26°C. A freshly voided sample is always best for ensuring optimal results False-Positive and False-Negative Urobilinogen Results False-positive results: A false positive urobilinogen reaction may occur with the chemical reagent strip method when substances known to react with Ehrlich's reagent such as sulfonamides and p-aminosalicylic acid are present in the urine. Drugs that contain Azo dyes, such as Azo Gantrisin, have a gold color that masks the reaction, causing a false positive reaction. Atypical color reactions may be obtained in the presence of high concentrations of p-aminobenzoic acid. The chemical reagent strip urobilinogen test cannot detect porphobilinogen in a urine specimen. Porphobilinogen is a molecule formed during the synthesis of the heme portion of hemoglobin. False-negative resultsDue to the instability of urobilinogen, a false negative result may occur using the chemical reagent strip method if the urine specimen has remained at room temperature for an extended period of time exposed to light. A false negative result may also occur if formalin is present. Detection of ketones bodies Introduction Normal urine does not contain ketone bodies. Acetone and other ketones bodies may appear in urine: In severe or untreated diabetes( diabetic ketoacidosis ) In certain other conditions (dehydration, vomiting, starvation and following strenuous exercise). Principle 159 | P a g e When sodium nitroprusside is added to urine containing ketone bodies, a purple color is produced. Materials and reagents 1- Test-tubes 2- Test-tube rack 3- Measuring cylinder, 10ml 4- Dropping pipette 5- Sodium nitroprusside crystals 6- Acetic acid 7- Ammonia. Method 1- Just before carrying out the test, place a sufficient amount of sodium nitroprusside crystals into a test-tube to cover the bottom 2- Add 5ml of distilled water. Shake well until the crystals are almost dissolved. (Not all the crystals are expected to dissolve as the solution is saturated.) 3- Measure 10ml of urine into another test-tube. 4- Add four drops of acetic acid to the urine, followed by 10 drops of freshly prepared Sodium nitroprusside solution and mix well 5- Holding the tip of the pipette against the side of the tube, let 20 drops (1 ml) of ammonia solution flow on to the surface of the liquid Wait for 5 minutes before reading a positive result may be obvious before this time RESULT If the result is positive purple ring appears on top of the urine. If the result is negative, no color change occurs Reporting the results of the test for detection of ketone bodies in urine a: Positive reaction; b: negative reaction. substances in urine Color change Result None = Negative Pink ring = + Red ring= ++ Purple ring =+++ Ketone bodies in urine can also be detected using a urine dipstick 6.1.2 MICROSCOPICAL EXAMINATION OF URINE Detection of abnormal elements 160 | P a g e Urine contains cells and crystals in suspension that can be collected by centrifugation or by allowing the urine to stand and the suspended particles to form a sediment. The resulting urinary deposit can be examined under the microscope In certain diseases of the urinary tract, the urinary deposits are considerably altered. Method Preparation of the deposit 1- Mix the urine specimen gently and pour 10 ml into a centrifuge tube. 2- Centrifuge the specimen at medium speed (1500RPM) for 5 minutes. 3- Pour off the supernatant by quickly inverting the tube without shaking. (The supernatant may be used for biochemical testing.) 4- Tap of the tube to re-suspend the deposit. 5- Transfer one drop of the deposit on to a slide using a Pasteur pipette and cover with a cover slip 6- Label the slide with the patient’s name or identification number. Microscopic examination Using the X10 objective and with the condenser lowered, scan the cover slip all over to look for ova of Schistosoma haematobium when indicated. Using the X40 objective and with the condenser lowered or aperture reduced, scan the coverslip area again and report any findings as a quantitative value for each high-power field The following may be found in urine 1- Erythrocytes 2- Leukocytes 3- epithelial cells 4- casts 5- fungi 6- bacteria 7- crystals 8- parasite eggs and larvae( Schistosoma haematobium ) 9- Trichomonas vaginalis 10- spermatozoa. Erythrocytes Erythrocytes in urine may be: (a) Intact: small yellowish discs, darker at the edges (8um); (b) Crenated: spiky edges, reduced diameter (5–6um); (c) Swollen: thin circles, increased diameter (9–10um). 161 | P a g e The shape of the cells often changes during storage of urine and does not have any diagnostic importance. In normal individual s occasional red blood cell (0-2HPF) may be seen in microscopic examination of the sediment Note: Erythrocytes may be found in the urine of women if the specimen has been taken during the menstrual period. Leukocytes Found in urine may be: (a) Intact: clear granular discs, 10–15mm (the nuclei may be visible); (b) Degenerated: distorted shape, shrunken, less granular; (c) Pus: clumps of numerous degenerated cells. The presence of many leukocytes, especially in clumps, indicates a urinary tract infection. How to express the quantity leukocytes found in urine deposits Place one drop of urine deposit on a slide and cover with a cover slip. Using the x40 objective, examine the deposit and count the number of leukocytes per microscope field. Report the results according to cells / high power field count. EPETHELIAL CELL Different types of epithelial cells can be observed in urine. Some of these are readily identifiable; however it is difficult to distinguish small transitional epithelial cells from WBC and renal tubular epithelial cells from transitional epithelial cells. Thus, all nonsquamous cells in urine are considered to be of transitional origin. When we are unsure about the origin of the cells in urine, we can stain a urine sediment with Wright's stain (or Diff-quik) and perform a cytological examination on the urine sediment. Epithelial cells are subjectively semi-quantified in urine (usually under low power using the 10x objective) as: none seen, few, moderate, many Transitional epithelial cells The urinary tract from the pelvis down the ureters to the bladder and the proximal urethra is lined by transitional epithelial cells. These cells vary in size and shape depending on the location from which they originate, e.g. those from the renal pelvis are more caudate whereas those from the bladder are more round to polygonal and vary in size. These cells naturally slough into the urine in quite low numbers, so none to a few transitional epithelial cells are seen in the urine from healthy animals. Note that this depends on the 162 | P a g e method of urine collection, since these cells will be sloughed (traumatically) when the bladder is catheterized. Transitional epithelial cells must be distinguished from WBC, because they both have the same granular appearance. In general, transitional epithelial cells (arrow in above image) are larger and have more irregular borders than WBC (which are uniformly more round, arrowhead in above image). Squamous epithelial cells These can be keratinized or non-keratinized. Non-keratinized squamous epithelial cells originate from the distal urethra, prepuce and/or vagina. They are larger than transitional cells and have small central nuclei. They can be round or have one or more flat border. Keratinized squamous epithelial cells are from the skin or vulva and are large cells with angular borders. They may or may not have nuclei (see upper image to the right). Nuclei are more visible in cells when the urine is stained with Sedi-stain (see central panel on right). If in doubt about the origin of the cells, a Wright's stain (routine hematologic stain) can be performed on a urine sediment and demonstrates the central nuclei and angular borders of squamous epithelial cells (lower panel on right).Squamous cells are frequently seen as contaminants in voided urine samples and can also contaminate samples collected by catheterization Renal tubular epithelial cells These are rarely seen in the urine and, as mentioned above, are very difficult to distinguish from transitional epithelial cells. If large numbers of smaller epithelial cells of uniform appearance (size and shape) are observed in the urine, a renal origin for these cells is suspected. Transitional epithelial cells tend to be more variable in size and shape (to some extent). Sloughing of large numbers of renal tubular epithelial cells would indicate renal tubular injury RBCs WBCs 163 | P a g e Squamous epithelial cells Transitional epithelial cells Neoplasia Fig15: common urine cells CAST Hyaline casts: These can be quite difficult to see in wet preparations of urine sediments with light microscopy, even with the condenser of the microscope racked down. They are much easier to visualize using phase contrast; however phase is usually not available on most microscopes. They become more visible with regular light microscopy if fat sticks to the protein matrix (Tamm-Horsfall mucoprotein) that makes up the hyaline cast (hyaline with fat) or particulate material from degenerating cells is present within the cast matrix (hyaline to finely granular cast). Granular casts: are rather short casts filled with large granules, pale yellow in color, with rounded ends. The granules come from degenerated epithelial cells from the tubules of the kidney. 164 | P a g e Fine granular casts have smaller granules that do not fill the cast Do not confuse with hyaline casts, partly covered by amorphous phosphate crystals Blood casts are filled with more or less degenerated erythrocytes, brownish in color. They are found in acute kidney disease. Pus casts are completely filled with leukocytes Hyaline casts, which may contain a few leukocytes suffering from kidney infection. Epithelial casts are filled with pale yellow epithelial cells (To make the cells more distinct, add a drop of 10% acetic acid to the deposit.) Epithelial casts have no diagnostic significance. Fatty casts are very shiny yellowish casts; the edges are indented and distinct and the ends are rounded They are soluble in ether but not in acetic acid Fatty casts are found in patients with severe kidney disease. Pseudo casts Do not mistake for casts: 1- clumps of phosphate crystals, short and clear-cut 2- aggregations of translucent mucus, the ends tapering into threads 165 | P a g e Fig16: different casts seen in urine Crystals Crystals have regular geometric shapes unlike amorphous debris, which is made up of clumps of small granules with no definite shape Except in very rare diseases, crystals in urine have no diagnostic significance. 1- Calcium oxalate (acid urine) Size: 10–20µ or about 50µ Shape: envelope-shaped or peanut-shaped Color: colorless, very shiny. 2- Uric acid (acid urine) 166 | P a g e Size: 30–150µ. Shape: varies (square, diamond-shaped, cubical or rose-shaped). Color: yellow or brownish-red. 3- Triple phosphates (neutral or alkaline urine) Size: 30–150µ. Shape: rectangular or like a fern leaf or star Color: colorless, shiny 4- Urate crystals Urates (alkaline urine) (Size: about 20µ. Shape: like a cactus or a bundle of needles Colour: yellow, shiny. Urates are often found together with phosphates. Calcium phosphate (neutral or alkaline urine) Size: 30–40µ. Shape: like a star. Colour: colourless. 5- Calcium carbonate (neutral or alkaline urine) Size: very small. Shape: similar to millet or corn grains, grouped in pairs. Colour: colourless. If acetic acid, 10% solution is added, the crystals dissolve, giving off bubbles of gas. 6- Calcium sulfate (acid urine) Size: 50–100µ. Shape: long prisms or flat blades, separate or in bundles. Calcium sulfate crystals can be distinguished from calcium phosphate crystals by measuring the pH of the urine. 7- Amorphous phosphates (alkaline urine) Amorphous phosphates appear as small, whitish granules, often scattered. 8- Amorphous urates (acid urine) Amorphous urates appear as very small, yellowish granules, which are grouped in compact clusters. They are not soluble in acetic acid, 10% solution, but dissolve if the urine is gently heated (Urine kept in the refrigerator often shows a heavy precipitate of urates.) Other crystalline deposits The following are rarely found in the urine. When present, however, they are found 9- Cystine (acid urine) Size: 30–60µ. 167 | P a g e Shape: hexagonal plates. Color: colorless, very shiny. Cystine crystals are found only in fresh urine as they are soluble in ammonia. & they are soluble in acetic acid, 10% solution (one drop per drop of deposit) They are found in patients with cystin uria, a very rare hereditary disease. 10- Acetyl sulfonamides (neutral or acid urine) Shape: varied, but often similar to sheaves of needles. Acetyl sulfonamide crystals are found in the urine following treatment with sulfonamide drugs. The presence of these crystals should be reported as they can cause kidney damage. Ammonium biurate Amorphous urate Bilirubin Calcium carbonate Calcium oxalate dihydrate Magnesium ammonium phosphate Uric acid Calcium oxalate monohydrate Calcium phosphate 168 | P a g e Cystine Tyrosine Flat plates resembling cholesterol Fig17: common urine crystals Fungi Size: 5–12µ. Shape: round or oval bodies of various sizes found together. Do not confuse with erythrocytes. Budding may be seen. Fungi are not soluble in acetic acid. Fungi are occasionally present in urine containing glucose. Check that the urine specimen is fresh. bacteria In healthy persons the urine contains practically no organisms. Bacteria may be found in patients who have an infection of some part of the urinary tract. Urethritis, cystitis or nephritis), or where bacteria from an infection elsewhere in the body are excreted in the urine The urine is centrifuged at high speed and the resulting deposit is examined under the microscope. Parasite eggs and larvae The following may be found: eggs of Schistosoma haematobium: found together with erythrocytes Trichomonas vaginalis 169 | P a g e Bacteria: Bacilli Bacteria: Cocci Schistosoma haematobium( egg) Trichomonas vaginalis (trophozoites) Fig18: Infectious agents 6.2 GENERAL STOOL EXAMINATION Introduction Many diseases are caused by infection with parasites. They are an important cause of diarrhea (which is a major health problem in developing countries. If acute diarrhea is caused by parasitic infection, this can be determined by examination of a stool specimen. Clinical Significance The Inspection of feces is important because it may lead to a diagnosis of parasitic infestation, obstructive jaundice, diarrhea, malabsorption, rectosigmoidal ,obstruction , dynsentry , ulcerative colitis , or gastrointestinal tract bleeding. 170 | P a g e Materials and reagents: Microscope Microscope slides Coverslips Wooden applicators or wire loops (0.45mm, nickel–chromium alloy wire) Grease pencils Sodium chloride, 0.85% solution Lugol iodine, 0.5% solution Examination of stool specimens for parasites Collection of specimens Inspect approximately 100 g of faeces in a clean, dry container without preservatives. A screw-top wide mouth container is most suitable. Make sure that any adult worms or segments passed are included. For collection of stool specimens for bacteriological examination (e.g. for culture of cholera and other bacteria that cause dysentery),. The container with specimen should be labeled, the urine and dirt should be excluded, urine will destroy any amoebic trophozoites and dirt will interfere with diagnosis never leave the stool specimen exposed to the air in container without lead never keep the stool specimen artificially warm and don’t leave in the sun Using Cary–Blair transport medium Cary–Blair transport medium will preserve many kinds of enteric bacteria (cholera vibrios, other vibrios, salmonella, shigella, etc.) for up to 4 weeks. The uninoculated medium may be stored in a sealed bottle at room temperature for 8–12 weeks. 1. Dip a sterile cotton wool swab in the stool specimen 2. For infants or other patients who cannot produce a stool specimen, take a rectal swab. Moisten the swab with sodium chloride solution and introduce the swab into the rectum. Turn the swab several times with a circular movement 3. Place the swab in a bottle containing Cary–Blair medium (three-quarters full) and send it to the bacteriology laboratory. If you cannot send the swab immediately, store it at room temperature. Important: Never store the swab in the incubator. 171 | P a g e Never store the swab in the refrigerator. 6.2.1 Macroscopical examination Faecal samples are best described by their colour, consistency and presence or absence of macroscopic blood, exudate and adult parasite. 1-Colour The color can be described as: Black (bleeding from upper gastrointestinal tract is more likely to cause stool black) Brown pale yellow (fat) white (obstructive jaundice) green bloody (especially blood originating from lower gut may cause the stool to be red ) clay (suggested diminution or absence of bile or presence of barium sulfate ) 2-Consistency The consistency can be described as: formed (normal shape) soft formed unformed or liquid (watery). The presence of external blood or mucus, usually seen as streaks of red or white, should be noted. Blood may be present in certain medical conditions (e.g. ulcerative colitis, schistosomiasis. 3- Pus Patient with chronic ulcerative colitis and chronic bacillary dysentery frequently pass large quantity of pus with the stool Large amount of pus never accompany amoebic colitis . No pus seen in watery stool ….. viral gastroenteritis. 4- Mucus Even in slightest quantity is abnormal Bloody mucus = inflammation of rectal canal Associated with pus and blood is found in stool of patient with ulcerative colitis , bacillary dysentery , intestinal tuberculosis Mucus with pus and blood = ulcerative colitis , bacillary dysentery . ulcerative carcinoma of colon . intestinal tuberculosis 5 - blood Blood in stool should be never ignored 172 | P a g e Bleeding upper GIT may give black- tarry appearance to stool. Bleeding from lower GIT may give red color 6- Fecal fat It is raised in malabsorption. 6.2.2 Microscopic examination Direct microscopic examination of faeces in saline or iodine suspension is useful for the following reasons: to detect motile trophozoites to detect ova and cysts present in moderate numbers to detect erythrocytes, cellular debris or excess fat Select unformed or liquid faeces when using direct microscopy for detection of trophozoites. Formed stools rarely contain motile trophozoites. Also perform a direct examination of any external blood or mucus. Method 1. Prepare a 1:1 mixture of 0.5% Lugol iodine solution. 2. Take a dry microscope slide and label it with the name or number of the patient. 3. Put: one drop of sodium chloride solution warmed to 37°C in the middle of the left half of the slide; and one drop of the iodine–acetic acid solution in the middle of the right half of the slide 4. Using an applicator or wire loop, take a small portion (about 2–3mm diameter) of the stool. a) If the stools are formed, take the portion from the centre of the sample and from the surface to look for parasite eggs. b) If the stools contain mucus or are liquid, take the portion from the mucus on the surface or from the surface of the liquid to look for amoebae. 5. Mix the sample with the drop of sodium chloride solution on the slide. 6. Using the applicator or wire loop, take a second portion of stool from the specimen as described above and mix it with the drop of iodine, acetic acid solution, discard the applicator (or flame the wire loop) after use. 7. Place a coverslip over each drop (apply the coverslips as shown in to avoid the formation of air bubbles). 8. Examine the preparations under the microscope. For the saline preparation use the x10 and x40 objectives and a x10 eyepiece. As the eggs and cysts are colorless, reduce the amount of light using the condenser aperture or lower the condenser to increase the contrast. Examine the first preparation with the x10 objective, starting at the top left hand corner as indicated in Focus on the edge of one coverslip using 173 | P a g e the x10 objective and examine the whole area under each coverslip for the presence of ova and larvae of parasit . Then switch to the x40 objective and again examine the whole area of the coverslip over the saline for motile trophozoites and the area of the coverslip over the iodine for cysts. 9. Lugol iodine–acetic acid solution causes the trophozoite forms to become nonmotile The nucleus is clearly stained but it may be difficult to distinguish between trophozoite and cystic forms. 10. Using a fine Pasteur pipette, allow a drop of 5% methylene blue solution to run under the coverslip over the saline preparation This will stain the nuclei of any cells present and distinguish the lobed nuclei of polymorphs from the large single nuclei of mucosal cells. Intestinal protozoa Protozoa are microorganisms consisting of a single cell. Intestinal protozoa may be found in stools in their motile form (trophozoites) or as cysts. Some intestinal protozoa are pathogenic (others are harmless. All these protozoa are found throughout the world. Identification of motile forms (trophozoites) The trophozoites of protozoa are motile either because of slow movements of the cell (amoebae) or because they have rapidly moving flagella (long whip-like threads) or cilia (numerous short hairs). Trophozoites are chiefly found in: watery stools stools containing mucus soft formed stools. The following features are useful for the identification of motile forms of intestinal protozoa size cytoplasm pseudopodia nuclei Ectoplasm Endoplasm Vacuoles Inclusion bodies containing erythrocytes, bacteria, yeast cells, debris, etc. nuclear membrane (chromatin) nuclear karyosome 174 | P a g e flagella Undulating membrane. Identification of cysts Cysts are the resistant forms of certain intestinal amoebae, flagellates and ciliates. They are small, round and non-motile and may have one or several nuclei. Measurement of cysts is useful for the correct identification of species. Importance of cysts The clinical importance of cysts varies from country to country. The cyst is the infective form of the organism. Healthy persons may be asymptomatic carriers of cysts and are therefore, a public health hazard. The most important problem in the laboratory is the precise identification of cysts 175 | P a g e Taenia saginata Hymenolepis nana Diphyllobothrium latum Ascaris lumbricoides Ancylostoma duodenale Trichuris trichuria Strongyloides stercoralis Clonorchis sinensis Paragonimus westermani 176 | P a g e Schistosome mansoni ova Schistosome japonicum Schistosoma haematobium Figure19: Ova in GSE Entamoeba histolytica cyst Entamoeba histolytica trophozoites Giardia lamblia cyst Giardia lamblia trophozoites Figure 20: Entamoeba histolytica & Giardia lamblia (HPF) 177 | P a g e Module 4 Session 2: Urine culture, throat swab, and nasal swab Objectives At the end of this session participants will be able to: 1. Explain urine culture 2. Explain throat swab 3. Explain nasal swab Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Discussion-lecture, question & answers Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 165 minutes 178 | P a g e Session plan -2Objectives 4.2.1. Explain urine culture Content 4.2.2. Explain throat swab 4.2.3. Explain nasal swab Methodology Introduction Media and diagnostic reagents Specimen collection Screening method Calibration Discussion -lecture Introduction Media and diagnostic reagents Bacterial agents of pharyngitis Culture and identification Discussion -lecture 60 minutes 60 minutes Question & answers Specimen Collection, Transport and Storage Correct specimen type and method of collection Staphylococci Identification 45 minutes 179 | P a g e 180 | P a g e 6.3 Urine culture Introduction Urine is the specimen most frequently submitted for culture. It also presents major problems in terms of proper specimen collection, transport, culture techniques, and interpretation of results. As with any other specimen submitted to the laboratory, the more information provided by the submitting physician the more able is the laboratory to provide the best possible culture data. The most common sites of urinary tract infection (UTI) are the urinary bladder (cystitis) and the urethra. From these sites the infection may ascend into the ureters (ureteritis) and subsequently involve the kidney (pyelonephritis). Females are more prone to infection of the urinary tract and also present the greater problem in the proper collection of specimens. In both males and females, UTI may be asymptomatic, acute, or chronic. Asymptomatic infection can be diagnosed by culture. Acute UTI is more frequently seen in females of all ages; these patients are usually treated on an outpatient basis and are rarely admitted to hospital. Chronic UTI in both males and females of all ages is usually associated with an underlying disease (e.g., pyelonephritis, prostatic disease, or congenital anomaly of the genitourinary tract) and these patients are most often hospitalized. Asymptomatic, acute, and chronic UTI are three distinct entities and the laboratory results often require different interpretation. Asymptomatic pyelonephritis in females may go undetected for some time, and is often only diagnosed by carefully performed quantitative urine culture. Chronic prostatitis is common and difficult to cure, and is often responsible for recurring UTI. In most UTI, irrespective of type, enteric bacteria are the etiological agents, Escherichia coli being isolated far more frequently than any other organism. In about 10% of patients with UTI, two organisms may be present and both may contribute to the disease process. The presence of three or more different organisms in a urine culture is strong presumptive evidence of improper collection or handling of the urine specimen. However, multiple organisms are often seen in UTI in patients with indwelling bladder catheters Expected pathogens - Enterococci - Escherichia coli - Mycobacterium tuberculosis - Other Enterobacteriaceae - Other staphylococci 181 | P a g e - Pseudomonas and other non-fermenters - Staphylococcus saprophyticus Media and diagnostic reagents - Isolation and quantitative media Blood agar CLED agar or chromogenic media MacConkey agar, with crystal violet, ) - Identification media and diagnostic reagents Kligler iron agar (KIA) Kovacs reagent for indole motility–indole–urease (MIU) medium oxidase reagent lysine–decarboxylase broth (Möller) ONPG test Simmons citrate agar For staphylococci and enterococci catalase test (H2O2) coagulase plasma bile–aesculin agar (for enterococci) novobiocin (5mg) disc for differentiating negative-coagulase staphylococci Specimen collection It cannot be overemphasized that considerable importance is attached to the method of collection of urine specimens, transport to the laboratory, and the initial efforts by the laboratory to screen and culture the urine. It is the responsibility of the laboratory to provide the physician with sterile, wide-mouthed, glass or plastic jars, beakers, or other suitable receptacles. Urine specimens may have been collected by a surgical procedure, e.g., suprapubic aspiration, cystoscopy, or catheterization. If not, the laboratory must insist on a clean-catch midstream urine specimen, particularly in females and children. Since urine itself is a good culture medium, all specimens should be processed by the laboratory within 2 hours of collection, or be kept refrigerated at 4 °C until delivery to the laboratory and processed no longer than 18 hours after collection. Whenever possible, urine specimens for culture should be collected in the morning. It is advisable to ask the patient the night before to refrain from urinating until the specimen is collected. Women A woman who is ambulatory should: 1. Wash her hands thoroughly with soap and water and dry them with a clean towel. 182 | P a g e 2. Undress in a suitable room, spread the labia, and cleanse the vulva and labia thoroughly, using sterile cotton gauze pads and warm soapy water wiping from front to rear. 3. Rinse thoroughly with warm water and dry with a sterile gauze pad. During the entire process the patient should keep the labia separated and not touch the cleansed area with the fingers. 4. Pass urine, discarding the first part of the stream. Collect the remaining urine in the sterile container, closing the lid as soon as the urine has been collected. 5. Hand the clean midstream urine, in the closed container, to the nursing personnel for prompt delivery to the laboratory. For bedridden patients, the same procedure is followed, except that a nurse must assist the patient or, if necessary, do the entire cleansing procedure before requesting the patient to pass urine. In both situations every effort must be made to collect a clean-catch urine specimen in a sterile container and to ensure that it is delivered promptly to the laboratory together with information on the patient, clinical diagnosis, and the requested procedures. Men A man who is ambulatory should: 1. Wash his hands. 2. Pull back the foreskin (if not circumcised) and pass a small amount of urine. 3. Still holding back the foreskin, pass most of the remaining urine into a sterile container. This is a midstream urine specimen. 4. Place the cover on the container and hand to nursing staff for prompt delivery to the laboratory. For bedridden patients: 1. If necessary, nursing personnel should pull back the foreskin, wash and dry the glans with soapy water and gauze pads. 2. With foreskin pulled back, the patient should pass a small amount of urine into a urinal. 3. The patient should then pass most of the remaining urine into the sterile container. The cover should be placed on the container and the specimen transported to the laboratory. Infants and children Collection of a clean-catch urine specimen from infants and children who are ill in bed or uncooperative can be a problem. Give the child water or other liquid to drink. Clean the external genitalia. The child can be seated on the lap of the mother, nurse, or ward attendant, who should then encourage the child to urinate and collect as much urine as possible in a sterile container. The container should then be covered and delivered to the laboratory for prompt processing. 183 | P a g e Culture and interpretation All urine specimens brought to the microbiology laboratory should be examined at once, or placed in a refrigerator at 4 °C until they can be examined. The examination procedure includes the following steps: 1. Examination of a Gram-stained smear. 2. A screening test for significant bacteriuria. 3. A definitive culture for urine specimens found to be positive in the screening test (step 2), and for all specimens obtained by cystoscopy, Suprapubic aspirate (SPA) , or catheterization. 4. Susceptibility tests on clinically significant bacterial isolates. Preparation and examination of a Gram-stained smear is a necessary part of the laboratory process. Using a sterile Pasteur pipette (one for each sample), place one drop of well mixed, uncentrifuged urine on a slide. Allow the drop to dry without spreading, heat-fix and stain. Examine under an oil-immersion lens for the presence or absence of bacteria, polymorphonuclear leukocytes, and squamous epithelial cells. One or more bacterial cells per oil-immersion field usually implies that there are 105 or more bacteria per milliliter in the specimen. The presence of one or more leukocytes per oil-immersion field is a further indication of UTI. Non-infected urine samples will usually show few or no bacteria or leukocytes in the entire preparation. In specimens from females, the presence of many squamous epithelial cells, with or without a mixture of bacteria, is strong presumptive evidence that the specimen is contaminated with vaginal flora and a repeat specimen is necessary, regardless of the number of bacteria per oil-immersion field. If results are required urgently, the report of the Gram-stain findings should be sent to the physician with a note that the culture report is to follow. Screening method The absence of leukocytes and bacteria in a Gram-stained smear of a clean-catch urine sample prepared as described above is good evidence that the urine is not infected. A urine specimen that is “negative” on careful examination of the Gram-stained smear does not need to be cultured. An alternative simple and effective screening test is the test strip for leukocyte esterase/nitrate reduction. The strip is dipped into the urine specimen as instructed in the package literature. Any pink colour is a positive reaction indicating the presence of leukocyte esterase and/or bacteria in excess of 105 per ml. Urine samples that are positive in the screening test should be cultured as soon as possible to prevent possible overgrowth by nonsignificant bacteria. If the strip does not develop a pink colour it is interpreted as a negative screening test, is so reported, and no culture is indicated. 184 | P a g e The test strip may not be sensitive enough to detect bacterial counts of less than 105 per ml of urine. Quantitative culture and presumptive identification Calibrated loop technique There are several culture methods for the quantification of bacteria in urine. The easiest and most commonly used are the calibrated loop technique. Of these method using CLED or chromogenic media, are considered to be the most versatile and efficient for large numbers of specimens. Chromogenic media contain various substrates which permit presumptive identification of several common species through a change in either colony pigmentation or colour of agar. They perform satisfactorily compared to CLED and have the advantage that mixed cultures are easier to detect. However, chromogenic media from different manufacturers can vary in specificity, and are relatively expensive Calibrated loop/surface streak method Mix the urine gently to avoid foaming. Dip the end of a sterile calibrated loop (eg 1 μL, 2 μL or 10 μL) in the urine to just below the surface and remove vertically, taking care not to carry over any on the shank. Use this to inoculate CLED or chromogenic agar plate and spread according to the number of specimens . A maximum of four samples per 9 cm plate is recommended for this method with a 1 μL or 2 μL loop, or two samples if using a 10 μL loop. If a 1 μL loop is used, one colony equals 1000 cfu/mL (ie 1 x 106 cfu/L). SPA, other surgically obtained urine, and urine samples with expected significant bacteriuria as low as 105 cfu/L (increased inoculum sizes are required) ,Inoculate 100 μL (0.1 mL) of specimen aseptically to a full CLED or chromogenic agar plate. Spread inoculum over entire surface of plate with a sterile loop or a spreader. Do not use a sterile swab which will absorb much of the inoculum. To isolate individual colonies, spread inoculum with a sterile loop. No. of cfu/L = No. of cfu on plate x 104. This semi quantitative method is only sensitive for screening down to106 cfu/L if a 5 μL or 10 μL loop is used (eg 5 or 10 colonies), or107 cfu/L if a 1 μL or 2 μL loop is used (eg 10 or 20 colonies). (See table below). Guidance on assessing colony counts : 185 | P a g e Interpretation of culture The basis studies for interpreting urine culture results showing that bacterial counts of ≥108 cfu/L (≥105 cfu/mL) are indicative of an infection and counts below this usually indicate contamination. In specific patient groups , counts between 108 cfu/L (105 cfu/mL) and 105 cfu/L (102 cfu/mL) may be significant. A pure isolate with counts between 107 and 108 cfu/L (104105 cfu/mL) should be evaluated based on clinical information or confirmed by repeat culture. Overall the confirmation of a UTI requires the demonstration of significant bacteriuria by quantitative culture (defined according to patient group or specimen type). Routine culture methods may not be sensitive enough to detect low bacteria levels (eg ≥107 cfu/L / ≥104 cfu/mL) and increased sensitivity will be achieved by increasing the inoculum size . The following is a list of imperial units and their equivalents. ≥105 cfu/mL equivalent to ≥108 cfu/L <105 cfu/mL equivalent to <108 cfu/L 104 cfu/mL equivalent to107 cfu/L <104 cfu/mL equivalent to <107 cfu/L 103 cfu/mL equivalent to 106 cfu/L <103 cfu/mL equivalent to <106 cfu/L 102 cfu/mL equivalent to 105 cfu/L Increased inoculum sizes are also required for persistently symptomatic patients without bacteriuria if the patient has recurrent ‘‘sterile pyuria’’, or for specimens where lower counts are to be expected, such as SPA or other surgically obtained urine. Identification Identification should be performed as rapidly as possible. Isolation of uropathogens should be performed by a surface streak procedure on both blood and MacConkey agar 186 | P a g e using calibrated loops for semi-quantitative method and incubated aerobically at 37 °C for 24 hours, and those cultures which becomes negative at the end of 24 hrs incubations will be further incubated for 48 hours. Bacterial identification should be made using biochemical tests, namely indole, citrate, oxidase, H2S production, lysine decarboxylase, lactose fermentation, urea hydrolysis, gas production, catalase, coagulase, manitol fermentation and novobiocin susceptibility test (See Flowcharts below ). Clinical specimen Primary isolation plate (blood, CLED, Staph/Strep medium or fastidious anaerobe agar) Gram stain Gram positive cocci in pairs and/or short chains Positive (Probable Staphylococcus) A weak catalase or pseudocatalase reaction may be produced by some strains of Aerococcus & Enterococcus species Catalase Negative non-haemolytic a-haemolytic (Consider Gemella) b-haemolysis (Consider Leuconostoc, Gemella, Helcococcus) Suspected Enterococcus (1-2 mm may be a, β or non-haemolytic. Consider clinical details) Optochin Sensitive Lancefield Group Resistant Rapid Aesculin hydrolysis (or PYR or group) A,B,C,D,F,G Positive S. pneumoniae: Some S. pneumoniae may be resistant to optochin: if there is a clinical suspicion of pneumococcal infection, confirm by performing bile solubility Non groupable (A,C,G, consider S.anginosus group) Negative (repeat, consider Listeria, check previous tests) “viridans” Streptococci: Occasional strains of S. oralis may be optochin sensitive: S. pseudopneumoniae optochin sensitive, bile solubility inconclusive Enterococcus spp (PYR & LAP positive) PYR positive, LAP positive consider Aerococcus, Lactococcus, Facklamia, Dolosigranulum. PYR positive, LAP negative consider Globicatella, Aerococcus viridans, Dolosicoccus Consider Aerococcus, Pediococcus, Lancefield Group B S. anginosus group (Aesc+, PYR-) PYR Negative Positive S. anginosus group Group A Further identification if clinically indicated Commercial identification system or other biochemical identification or send to the Reference Laboratory Fig 21: Identification of Streptococci and Enterococci Flowchart 187 | P a g e Clinical specimens Primary isolation plate Opaque, white, cream, yellow or orange colonies on blood agar Gram stain Gram positive cocci in clusters If there is a different Gram stain appearance refer to the appropriate SMI Negative (S. anaerobius is catalase negative) Consider other organisms Modified oxidase Resistant Positive Micrococcus (Aerobic growth only) Suspected S. aureus Catalase Positive Novobiocin Negative Sensitive DNase, clumping factor (slide or commercial latex kit) Protein A or thermostable nuclease Negative S. sciuri Group (Aesculin Positive) (Meticillin resistant strains may be mistaken for MRSA and will grow well on many chromogenic selective agars). S. saprophyticus Group Coagulase-negative Staphylococcus Positive Confirm with tube coagulase if required S. aureus Further identification if clinically indicated Commercial identification system Confirm with tube coagulase if required DNA +ve: S. aureus, S. intermedius, S. schleiferi, S. hycius, S. sciuri, S. chromogenes Protein A latex +ve: S.aureus (S. saprophyticus and S. sciuri may give false positive) Coagulase +ve: S. aureus, S. intermedius, S. hyicus, S. schleiferi Fig 22: Presumptive Identification of Staphylococcus Species Flowchart 188 | P a g e Clinical Specimens Primary isolation plate BA CLED B or CLED A, MAC DCA, XLD, CT-SMAC, TCBS, CIN agar Carbohydrate fermenting Carbohydrate non fermenting Further identification if clinically indicated Oxidase Performed from non selective medium Negative Further identification Serology for possible: Salmonella / Shigella species (XLD / DCA) E. coli O157 (CT-SMAC) all presumptive (locally confirmed) E. coli O157 should be sent to the Reference Laboratory Y. enterocolitica (CIN) (see ID 20, 21, 22, 24) Commercial identification system or other biochemical identification or send to the Reference Laboratory Positive Possible Pseudomonas species or Pasteurella species (see ID 17 & 13) Fig 23: Identification of Enterobacteriaceae Flowchart 189 | P a g e Clinical specimens Primary isolation plate Pseudomonas selective agar Blood agar (or other primary isolation media) Burkholderia cepacia selective agar Typical colonies of GNR at 16-48 hr (see Sections 3.2 and 3.3) Burkholderia cepacia complex may require up to 5 days incubation Pigment production Blue-green colonies No blue-green colonies Pink colonies on B. cepacia selective agar Oxidase test Oxidase test Gram stain of pure culture Positive P. aeruginosa growth at 42°C Negative Positive Negative Gram negative rod Further identification if clinically indicated Commercial identification kit or other biochemical identification or send to the Reference Laboratory If required, save the pure isolate on an agar slope Other Discard Fig 24: Identification of Glucose Non -Fermenting Gram negative Rods Flowchart 190 | P a g e Susceptibility tests Susceptibility tests should only be performed on well isolated colonies of similar appearance that are considered significant according to the guidelines presented above. Susceptibility tests are generally more important on cultures obtained from patients who are hospitalized or have a history of recurring UTI. Cultures from patients seen in the clinic with a primary UTI may not require a susceptibility test. 6.4 Throat swab The upper respiratory tract can be the site of several types of infection: pharyngitis, sometimes involving tonsillitis, and giving rise to a “sore throat” nasopharyngitis otitis media Sinusitis epiglottitis. Of all those infections, pharyngitis is by far the most frequent; in addition, the untreated infection may have serious sequelae. Only pharyngitis will be considered here. Bacteriological diagnosis of pharyngitis is complicated by the fact that the oropharynx contains a heavy, mixed, normal flora of aerobic and anaerobic bacteria. The normal flora generally outnumbers the pathogens and the role of the bacteriologist is to distinguish between the commensals and the pathogens. Where possible only the latter should be reported to the physician. Normal flora of the pharynx The normal flora of the pharynx includes a large number of species that should be neither fully identified nor reported when observed in throat cultures: • viridans (a-haemolytic) streptococci and pneumococci • Nonpathogenic Neisseria spp. • Moraxella (formerly Branhamella) catarrhalis (this can also be a respiratory pathogen) • Staphylococci (S. aureus, S. epidermidis) • diphtheroids (with the exception of C. diphtheriae) • Haemophilus spp. • Yeasts (Candida spp.) in limited quantity • Various strictly anaerobic Gram-positive cocci and Gram-negative rods, spirochaetes and filamentous forms. The throats of elderly, immunodeficient, or malnourished patients, particularly when they have received antibiotics, may be colonized by Enterobacteriaceae (Escherichia coli, Klebsiella spp., etc.) and by the nonfermentative Gram-negative groups (Acinetobacter 191 | P a g e spp. and Pseudomonas spp.). Such patients may also have in their pharynx a proliferation of S. aureus or of Candida spp., or other yeast-like fungi. Although these microorganisms do not cause pharyngitis, except in association with granulocytopenia, it is advisable to report such isolates to the clinician, as they occasionally indicate the existence of (or may sometimes give rise to) a lower respiratory tract infection (e.g. pneumonia) or bacteraemia. However, an antibiogram should not be performed routinely on these colonizing microorganisms. Expected pathogens Candida albicans (oropharynx) Corynebacterium diphtheriae (throat and nose) Haemophilus influenzae (ear and sinus) Moraxella catarrhalis (ear and sinus) Neisseria meningitides Pseudomonas Staphyloccoccus aureus (ear and sinus) Streptococcus pneumoniae (ear and sinus) Streptococcus pyogenes (group A, throat) Media and diagnostic reagents Isolation media Isolation media Blood agar (prepared from a glucose-free base) Chocolate agar Löffler coagulated serum or Dorset egg medium Tellurite blood agar Modified Thayer–Martin medium (for gonococci andmeningococci) Priority grading 1 2 2 2 3 Diagnostic reagents Diagnostic reagents Bacitracin disc Catalase and coagulase reagents Optochin disc Carbohydrate degradation media for Neisseria spp. Oxidase reagent V and XV factors (discs or strips) Tributyrin Priority grading 1 1 1 2 2 2 3 192 | P a g e Rapid diagnostic tests Grouping kit for haemolytic streptococci 3 Bacterial agents of pharyngitis Streptococcus pyogenes (Lancefield group A) is by far the most frequent cause of bacterial pharyngitis and tonsillitis. This infection is particularly prevalent in young children (5–12 years). Non-group-A, b-haemolytic streptococci (e.g. groups B, C and G) are uncommon causes of bacterial pharyngitis and if detected should be reported. Corynebacterium diphtheriae is the cause of diphtheria, a disease that is endemic in many countries. It can reach epidemic proportions in countries where the vaccination programme has been interrupted. Characteristically (with a few exceptions), C. diphtheriae causes a typical form of infection, characterized by a greyish-white membrane at the site of infection (pharynx, tonsils, nose, or larynx). Diphtheria is a serious disease and the diagnosis is made on the basis of clinical findings. The physician would then generally make a specific request to culture for diphtheria bacilli. (Vincent angina) is a rare condition characterized by a necrotic ulceration of the pharynx with or without formation of a pseudomembrane. It is associated, at the site of infection, with a heavy mixed flora of strict anaerobes dominated by Gram negative fusiform rods and spirochaetes, generally referred to as Fusobacterium spp. and Treponema vincentii, and possibly others. Although both species belong to the normal mouth flora, their presence in large numbers in a Gram-stained smear of ulcerated lesions should be reported as a “fusospirochaetal complex”. This microscopic diagnosis need not be confirmed by anaerobic culture, which is difficult and time-consuming. However, the presence of this complex does not exclude the need to search for other pathogens, particularly S. pyogenes. Although small numbers of C. albicans or other Candida species may be part of the normal oral flora, oral candidiasis results when the number of organisms increases considerably in certain pathological conditions, e.g. in malnourished premature babies, in immunodeficient adults (e.g. patients with HIV/AIDS), or in patients who have received broad-spectrum antimicrobials or cancer therapy. The affected area—tongue, tonsils, throat or buccal mucosa —may be extremely red, or covered with white patches or a confluent grey-white membrane (thrush). The diagnosis of candidiasis is best made by finding numerous yeast cells, some of them forming long mycelium-like filaments, in a Gram-stained smear of the exudate. Swabs from the upper respiratory tract may be submitted to the laboratory, not for the diagnosis of a clinical infection, but to detect a 193 | P a g e potential pathogen in a healthy subject, a pharyngeal or a nasal “carrier”. This should only be done as part of well-defined epidemiological surveys. The following pathogens can give rise to a carrier state in the upper respiratory tract: • Staphylococcus aureus. Sampling of patients and staff for nasal carriers is sometimes performed as part of an investigation of hospital outbreaks of Meticillin-resistant S. aureus (MRSA). • Neisseria meningitidis. Carriage of meningococci may be very prevalent (20% or more) even at non-epidemic times. Identification of pharyngeal carriers of meningococci is rarely needed, and need not be performed prior to the administration of prophylactic antibiotics to family or other close contacts of patients with meningococcal disease. • Streptococcus pyogenes. Carriage of this organism in low numbers may be prevalent, especially among schoolchildren (20–30%). • Corynebacterium diphtheriae. The carrier rate of the diphtheria bacillus is high in nonvaccinated populations. In such communities, it may be justified to identify and treat carriers among the close contacts of a patient with proven diphtheria. Carriers are rare when an immunization programme is correctly implemented. Collection and dispatch of specimens Ideally, specimens should be collected by a physician or other trained personnel. The patient should sit facing a light source. While the tongue is kept down with a tongue depressor, a sterile cotton-wool swab is rubbed vigorously over each tonsil, over the back wall of the pharynx, and over any other inflamed area. Care should be taken not to touch the tongue or buccal surfaces. It is preferable to take two swabs from the same areas. One can be used to prepare a smear, while the other is placed into a glass or plastic container and sent to the laboratory. Alternatively, both swabs may be placed in the container and dispatched to the laboratory. If the specimen cannot be processed within 4 hours, the swab should be placed in a transport medium (e.g. Amies or Stuart). Direct microscopy The fusospirochaetal complex of necrotizing ulcerative pharyngitis (Vincent angina) and Candida are best recognized on a Gram-stained smear, which should be prepared if the physician makes a special request. The Gramstained smear is not useful for the detection of streptococci or Neisseria spp. 194 | P a g e Moreover, the direct smear has poor sensitivity and specificity for the detection of the diphtheria bacillus, unless the specimen has been collected with care and is examined by an experienced microbiologist. In the absence of a physician’s request or of clinical information, a Gram-stained smear should not be made for throat swabs. Culture and identification Culture for Streptococcus pyogenes Immediately upon receipt in the laboratory, the swab should be rubbed over one-quarter of a blood agar plate, and the rest of the plate streaked with a sterile wire loop. The blood agar should be prepared from a basal agar medium without glucose (or with a low glucose content), e.g. tryptic soy agar (TSA). Acidification of glucose by S. pyogenes inhibits the production of haemolysin. Blood from any species, even human blood (fresh donor blood), can be used at a concentration of 5%. The plates should be filled to a depth of 4–5 mm. Sheep blood is preferred because it does indicate haemolysis of some commensal Haemophilus spp. and it gives no haemolysis with the zymogenes variant of Enterococcus faecalis. The recognition of b-haemolytic colonies can be improved, and their presumptive identification hastened, by placing a co-trimoxazole disc (as used for the susceptibility test) and a special low-concentration bacitracin disc over the initial streaked area. Because S. pyogenes is resistant and many other bacteria are susceptible to cotrimoxazole, this disc improves the visibility of b-haemolysis. Incubation in a candle-jar will detect most b-haemolytic streptococci. A simple way to increase haemolysis is to stab the agar surface perpendicularly by inserting the loop deep into the medium to encourage growth of subsurface colonies. After 18 hours and again after 48 hours of incubation at 35–37 ∞C, the blood plates should be examined for the presence of small (0.5–2 mm) colonies surrounded by a relatively wide zone of clear haemolysis. After Gram-staining to verify that they are Gram-positive cocci, the colonies should be submitted to specific identification tests for S. pyogenes. For clinical purposes, presumptive identification of S. pyogenes is based on its susceptibility to a low concentration of bacitracin. For this purpose, a special differential disc is used containing 0.02–0.05 IU of bacitracin. The ordinary discs used in the susceptibility test, with a content of 10 units, are not suitable for identification. A b-haemolytic streptococcus showing any zone of inhibition around the disc should be reported as S. pyogenes. If the haemolytic colonies 195 | P a g e are sufficiently numerous, the presence or absence of an inhibition zone may be read directly from the primary blood agar plate. If the colonies are less numerous, one or two should be picked from the primary plate, streaked on one-fifth of another plate to obtain confluent growth, and each inoculated area covered with a bacitracin disc. After overnight incubation, the subcultures should be read for inhibition zones. In some laboratories this presumptive identification is confirmed by serological demonstration of the specific cell wall polysaccharides. This can be done either by the classical precipitin method, or more rapidly by using a commercial kit for the rapid slide coagglutination or latex agglutination tests. If desirable, bacitracinresistant b-haemolytic streptococci can be further identified using some simple physiological tests (see Table 19). Minute colonies of b-haemolytic streptococci may be encountered, which, when grown and serologically grouped, react with group A antiserum. These streptococci are not considered to be S. pyogenes and are not associated with the serious infections caused by group A streptococci. In reporting the presence of S. pyogenes in a throat culture, a semiquantitative answer should be given (rare, +, + +, or + + +). Patients with streptococcal pharyngitis generally show massive growth of S. pyogenes, with colonies over the entire surface of the plate. Plates of carriers generally show fewer than 20 colonies per plate. Even rare colonies of b-haemolytic streptococci should be confirmed and reported. Table 10: Differentiation of b-haemolytic streptococci 196 | P a g e Culture for Corynebacterium diphtheriae Although the diphtheria bacillus grows well on ordinary blood agar, growth is improved by inoculating one or two special media: • Löffler coagulated serum or Dorset egg medium. Although not selective, both of these media give abundant growth of the diphtheria bacillus after overnight incubation. Moreover, the cellular morphology of the bacilli is more “typical”: irregularly stained, short to long, slightly curved rods, showing metachromatic granules, and arranged in a V form or in parallel palisades. Metachromatic granules are more apparent after staining with methylene blue or Albert stain than with the Gram stain. • A selective tellurite blood agar. This medium facilitates isolation when the bacilli are few in number, as is the case for healthy carriers. On this medium, colonies of the diphtheria bacillus are greyish to black and are fully developed only after 48 hours. Suspicious colonies, consisting of bacilli with a coryneform morphology on the Gramstained smear, should be subcultured to a blood agar plate to check for purity and for “typical” morphology. It should also be remembered that colonies of the mitis biotype of C. diphtheriae, which is the most prevalent, show a marked zone of b-haemolysis on blood agar. A presumptive report on the presence of C. diphtheriae can often be given at this stage. However, this should be confirmed or ruled out by some simple biochemical tests and by demonstration of the toxigenicity. As the latter requires inoculation of guinea-pigs or an in vitro toxigenic test (Elek) and has to be performed in a central laboratory, only rapid biochemical identification will be covered here. C. diphtheriae is catalase- and nitratepositive. Urea is not hydrolysed. Acid without gas is produced from glucose and maltose, generally not from saccharose. The fermentation of glucose can be tested on Kligler medium. Urease activity can be demonstrated on MIU and nitrate reduction in nitrate broth in the same way as for Enterobacteriaceae. For the fermentation of maltose and saccharose, Andrade peptone water can be used as a base with a 1% final concentration of each carbohydrate. Results can usually be read after 24 hours, although it may be necessary to reincubate for one night. It must be emphasized that the microbiology laboratory’s role is to confirm the clinical diagnosis of diphtheria. Therapy should not be withheld pending receipt of laboratory reports. 197 | P a g e Susceptibility testing Routine susceptibility tests on throat or pharyngeal isolates are most often not required, and may even be misleading. The major pathogens involved in bacterial pharyngitis are S. pyogenes and C. diphtheriae benzylpenicillin and erythromycin are considered as the antimicrobials of choice to treat both types of infection. In cases of diphtheria, treatment with antitoxin is also indicated. 6.5 Nasal Swab Nasal colonization with Staphylococcus aureus increases the risk of staphylococcal infections at other sites of the body such as postoperative wounds and dialysis access sites3. It is also associated with recurrent skin infections and nosocomial infections in nurseries and hospital wards. S. aureus is a major cause of morbidity and mortality in haemodialysis patients4 as most patients carry the organism in their anterior nares. Eradication of nasal carriage of S. aureus may be beneficial in certain clinical conditions such as recurrent furunculosis. Systemic, in addition to topical, treatment is appropriate for nasally colonised patients who have infection elsewhere. Topical antibacterial agents such as mupirocin and chlorhexidine/neomycin are preferred to systemic formulations when a patient is identified as a carrier. Nose swabs may be used to investigate carriage of Lancefield group A streptococcus and Meticillin Resistant Staphylococcus aureus (MRSA) Specimen Collection, Transport and Storage Safety considerations Use aseptic technique. Collect specimens in appropriate CE marked leak proof containers and transport specimens in sealed plastic bags. Collect swabs into Amies transport medium with charcoal22 and transport in sealed plastic bags. Compliance with postal and transport regulations is essential. Collect specimens before antimicrobial therapy where possible. Specimens should be transported and processed as soon as possible. If processing is delayed, refrigeration is preferable to storage at ambient temperature20. Delays of over 48hr are undesirable. 198 | P a g e Correct specimen type and method of collection Plain sterile cotton wool swab. Sample the anterior nares by gently rotating the swab over the mucosal surface. Unless otherwise stated, swabs for bacterial and fungal culture should then be placed in amies transport medium with charcoal. Numbers and frequency of specimen collection are dependent on clinical condition of patient. Specimen Processing Inoculate each agar plate with a swab For the isolation of individual colonies, spread inoculum with a sterile loop. Table 11: Culture media, conditions and organisms for all specimens Staphylococci Identification Staphylococci are the bacteria most frequently associated with the production of pus. Staphylococci grow well aerobically on blood agar and form opaque white to cream colonies, 1–2mm in diameter, after overnight incubation. They are unique in growing on media with a high salt content, such as MSA. They can be differentiated from streptococci by their morphology and by the production of catalase. Catalase production by staphylococci is shown by placing it in a drop of 3% hydrogen peroxide onto the colonies deposited on a clean glass slide. The appearance of bubbles of oxygen is an indication of catalase production. For clinical purposes, staphylococci can be divided into those that produce coagulase and those that do not. The coagulase-producing staphylococci belong to the species S. aureus, which is the species of greatest medical interest. Of the several coagulase-negative species, only two will be considered here—S. epidermidis and S. saprophyticus. Although S. aureus is part of the commensal microbial flora of the nose (40% of healthy adults are positive), skin, and intestinal tract, this species causes impetigo, boils, 199 | P a g e abscesses, wound infection, infection of ulcers and burns, osteomyelitis, mastitis (breast abscess), pleural empyema, pyomyositis, toxic shock syndrome, and other types of pyogenic infection. S. epidermidis is also a common commensal of the skin, nose, and other mucous membranes and possesses a very low pathogenicity. However, its presence in pus should not always be dismissed as skin contamination. Despite its low infectivity, S. epidermidis can cause skin infections at the site of an in-dwelling catheter, cannula, or other device. Infections with S. epidermidis are particularly troublesome in cardiac and orthopaedic surgery involving the insertion of prosthetic devices (artificial heart valves or artificial hips). S. saprophyticus is recognized to be a common cause of urinary tract infections in young women, being second only to E. coli in some populations. The distinctive features of the three main species of Staphylococcus are given in Table ( 1). Table 12: Differentiation of medically important species of Staphylococcus 200 | P a g e Figure 25: A flow diagram for the preliminary identification of staphylococci 201 | P a g e In view of the importance of the coagulase test in the identification of S. aureus, this test is described here in detail. Coagulase is an enzyme that causes plasma to clot. Staphylococcal coagulase exists in two forms: bound coagulase or clumping factor, which is demonstrated in the slide test, and free coagulase, which is demonstrated in the tube test. • Slide test. On a clean slide, emulsify one or a few similar colonies of staphylococci in a drop of saline. The suspension must be fairly thick. Dip a straight wire into plasma and use this to stir the bacterial suspension. Observe for clumping within 10 seconds. False-negative slide tests occur approximately 10% of the strains of S. aureus. If the slide test is negative for an isolate that seems to be pathogenic on other grounds (pigment, clinical source), it should be re-examined in the tube test. • Tube test. Dispense a few drops (0.5 ml) of plasma into a sterile 12 \ 75 mm tube, and add two drops of the pure culture in broth. A suspension with an equivalent density may also be prepared directly from growth on blood agar. Incubate the tube at 35 ∞C for 4–18 hours and then examine for clotting. The plasma used in the coagulase test may be fresh human or rabbit plasma obtained with ethylenediamine tetraacetic acid (EDTA). It should be stored in the refrigerator in small amounts (1 ml), and its performance checked with cultures of S. aureus and S. epidermidis, run in parallel. Antimicrobial susceptibility testing Prudent use of antimicrobials according to local and national protocols is recommended. Reporting Procedure Culture Report presence or absence of specific pathogens, also report results of supplementary investigations: Negatives "Staphylococcus aureus NOT isolated". "Lancefield group A streptococcus NOT isolated". Positives "Staphylococcus aureus isolated". "Lancefield group A streptococcus isolated". 202 | P a g e Module 4 Session 3: Smart tests, preparation of media and staining smears Objectives At the end of this session participants will be able to: 1. Discuss Helicobacter pylori Serum/Whole Blood 2. Explain Salmonella typhi Antigen 3. Explain Vibrio cholerae Rapid visual antigen detection test 4. Explain Preparation of Media 5. Discuss staining smear Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Mini-lecture, question & answers, discussion-lecture Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 195 minutes 203 | P a g e Session plan -3Objectives 4.3.1. Discuss Helicobacter pylori Serum/Whole Blood Content 4.3.2. Explain Salmonella typhi Antigen 4.3.3.Explain Vibrio cholera Rapid visual antigen detection test 4.3.4. Explain Preparation of Media Methodology Mini -lecture Introduction Principle of the test 30 minutes Materials and reagents Specimen collection and storage Procedure Principle of the test Question & answers Materials Specimen collection 30 minutes and storage Procedure Discussion- lecture Principle of the test Materials 45 minutes Specimen collection and storage Procedure Interpretation and reporting of results Blood agar Chocolate agar MacConky agar Mueller-Hinton agar Discussion- lecture 60 minutes 204 | P a g e 4.3.5.Discuss staining smear Cary-Blair, Amies, and Stuarts medium Mini-lecture Gram’s Stain Ziehl-Neelsen’s stain (for acid fast bacilli) 30 minutes 205 | P a g e 6.6 Smart tests 6.6.1 Helicobacter pylori Serum/Whole Blood The exact role that H. pylori plays in gastrointestinal disease still needs to be precisely defined and is the subject of ongoing research. However, the prevalence rates for H. pylori infection as demonstrated by histological and bacteriological methods can approach 90% in patients who present clinical symptoms of the gastrointestinal diseases listed below (clinical significant). H. pylori does not appear to invade the bloodstream since no isolates yet have been detected using commercial blood culture methods. H. pylori infections occur in human populations throughout the world. In developed countries, about 50% of the population may have H. pylori infection by the age of 60 years, while only 10-20% of adults in the third decade of life have it. In patients who present clinical symptoms relating to the gastrointestinal tract there are two major methods of investigation: invasive and noninvasive. Invasive methods include culture of gastric biopsy samples, histological examination of stained biopsy specimens, or direct detection of the urease activity in the biopsy (CLO test). These methods need to obtain a biopsy sample by endoscopy, which is expensive, and usually results discomfort and risk to the patient. Noninvasive techniques include urea breath tests and serological methods. Urea breath test requires the use of a small amount of radioactivity and a mass spectrometer. Serologic tests are employed to detect antibodies as human immune response to H. pylori. Two methods appear to be of great interest regarding their use in H. pylori routine serology, namely the ELISA and the Western immune blot because they offer the most versatility in regards to immunoglobulin specificity and relative ease of use. This H. pylori rapid test detects IgG antibodies specific to H. pylori infection in patient’s blood or serum. It is a noninvasive method and does not use radioactive isotopes; the assay procedures are easy and do not require professional training; it provides a rapid result. It is a useful onsite aid in the diagnosis of H. pylori infection. CLINICAL SIGNIFICANT Helicobacter pylori has been associated with a variety of gastrointestinal diseases including gastritis, duodenal and gastric ulcer, non-ulcer dyspepsia, gastric adenocarcinoma and lymphoma. PRINCIPLE OF THE TEST This assay is a double antigen chromatographic lateral flow immunoassay. The test strip in the device includes: 1) a burgundy-colored conjugate pad containing colloidal gold coupled with H. pylori antigens, and 2) nitrocellulose membrane containing a test line (T line) and a control line (C line). The T line is coated with H. pylori antigens, and the C 206 | P a g e line is coated with goat anti-H. pylori antibody. The antigens used in this device are from H. pylori cell lysate. When IgG antibodies specific to H. pylori are present in the specimen, the T line will become a burgundy-colored band. If antibodies to H. pylori are not present or are present below the detectable level, no T line will develop. The C line should always appear as a burgundy-colored band regardless of the presence of antibodies to H. pylori. The C line serves as an internal qualitative control of the test system to indicate that an adequate volume of specimen has been applied and the flow occurred. MATERIALS AND REAGENTS • Test devices, each sealed in a pouch with a dropper pipette. • 1 bottle of wash buffer-7 ml PBS diluents with 0.02% sodium azide as a preservative. • 1 package inserts (Instruction for Use). • Lancet or other blood collection device (Vacutainer blood collection tubes, sterile needles and syringes). • Timer. Do not expose the kit to temperatures over 30°C (86°F). SPECIMEN COLLECTION AND STORAGE 1- Serum • Follow standard laboratory procedures to collect serum specimens. • Serum specimens can be stored at (9-30) °C for 8 hours, at (2-8) oC for one week, and at (≤ -20) °C or lower for long term storage. Repeatedly frozen and thawed specimens are not recommended for this assay. • Any sediment in serum specimens should be removed by centrifugation. Avoid using any turbid specimens, which may be contaminated by microorganisms. 2- Whole Blood • Finger stick sampling is recommended for this assay. • Middle or ring finger is the preferred puncture site. • Clean patient’s finger with an alcohol swab. Wait until it is dry. • Puncture the fingertip with the lancet. Wipe away first sign of blood. • Gently rub the hand from palm to finger to help form a drop of blood over the punctured site. • Use the provided pipette to pick up the blood, and apply one drop of the blood to the sample well of the device. Then, follow the procedure. PROCEDURE 1. Refrigerated specimens and other test materials, including devices, must be equilibrated to room temperature before testing. 207 | P a g e 2. Remove the device from its wrap pouch prior to performing the assay, label the device with identification. 3. Add one drop of fresh blood or serum to the sample well marked "S". Allow about 30 seconds for the specimen to be absorbed totally. Discard the first three drops of wash buffer from the wash buffer squeeze bottle. Then add three drops of wash buffer into the sample well. 4. Strong positive results may be observed in 2-3 minutes or depending on manufacturers. Weak positive results may take a longer time, up to 7 minutes. For the whole blood test, a slight hemolysis might be observed, but it does not interfere with the results. INTERPRETATION OF RESULTS IMPORTANT: Interpret the results depending on manufacturers. The T line should always be interpreted independently of the C line. Figure 26: Interpretation of Smart Test Results Positive: If both the C line and T line appear, the result indicates that the IgG antibodies specific to H. pylori are detected and the result is positive. A faint line in test region indicates a borderline specimen, which should be re-tested using an alternative method for confirmation. Negative: If only the C line appears in the control region, the test indicates that no antibodies to H. pylori are detected and the result is negative. Invalid: When no control line appears within 5 minutes, repeat the test with a new test device. QUALITY CONTROL PROCEDURE • Built-in Control Features 208 | P a g e This test contains a built-in quality control feature, the C line. The appearance of the burgundy C line indicates that that an adequate volume of specimen and wash buffer has been applied and the flow occurred. • External Quality Control External controls are recommended, positive and negative, to monitor the performance of the assay. 6.6.2 Salmonella typhi Antigen Immunochromatographic rapid assay for the Detection of Salmonella Typhi Antigen in Human Stool or Serum Specimens, Typhoid fever is a life threatening illness caused by the bacterium Salmonella typhi, and was observed by Eberth (1880) in the mesenteric nodes and spleen of fatal cases of typhoid fever. It is common in developing countries where it affects about 12.5 million persons annually. The infection is acquired typically by ingestion. On reaching the gut, the bacilli attach themselves to the epithelial cells of the intestinal villi and penetrate to the lamina and submucosa. They are then phagocytosed there by polymorphs and macrophages. The ability to resist intracellular killing and to multiply within these cells is a measure of their virulence. They enter the mesenteric lymph nodes, where they multiply and, via the thoracic duct, enter the blood stream. A transient bacteremia follows, during which the bacilli are seeded in the liver, gall bladder, spleen, bone marrow, lymph nodes and kidneys, where further multiplication takes place. Towards the end of the incubation period, there occurs a massive bacteremia from these sites, heralding the onset of the clinical symptoms. The diagnosis of typhoid consists of isolation of the bacilli and the demonstration of antibodies. The isolation of the bacilli is very time consuming and antibody detection is not very specific. Other tests include the Widal reaction, has developed a test that takes only 10-20 minutes and requires only a small quantity of stool or one drop of serum to perform. It is the easiest and most specific method for detecting S. typhi infection. PRINCIPLE OF THE TEST Cortez One Step S. Typhi Antigen test is a qualitative one step immunochromatographic assay. The test employs a conation of monoclonal antibody/colloidal gold dye conjugate and a polyclonal antibody immobilized on the solid phase. This will selectively identify S. typhi antigen associated S. typhi (typhoid) infection with a high degree of sensitivity and specificity. As the specimen flows through the absorbent pad in the sample well and through the antibody/colloidal gold complex any S. typhi antigen present in the sample binds to the conjugate forming an antigen/antibody complex. The sample and dye complex continue to migrate along the membrane to the immobilized polyclonal antibody. In the presence of S. typhi, the polyclonal antibody captures the complex. This forms a visible pink/purple band 209 | P a g e in the (B) or test area of the card. If no antigen is present, there is no line formation in the (B) area. The remaining complex continues to migrate to another immobilized antibody on the membrane in the (C) or Control area of the card, and is captured which then forms a band indicating proper performance of the test. MATERIALS Each kit contains: 1. Cortez S. typhi Antigen test. Each cassette contains a test strip with S. typhi specific antibody on the test region of the membrane and colored S. typhi antibody-gold conjugate pad. 2. Fecal sample buffer – 2 bottles, 8 mL each. 3. Instruction for use. 4. Specimen collection container. 5. Timer. SPECIMEN COLLECTION AND STORAGE Cortez One Step S. typhi Antigen test can be run on stool or serum samples. The test works best on fresh samples. If testing cannot be done immediately, they should be stored at (28)°C after collection for up to 3 days. If testing cannot be done within 3 days, serum can be stored frozen at (–20) °C or colder. Shipment of samples should comply with local regulations for transport of etiologic agents. Stool and serum specimens should be collected in containers that do not contain media, preservatives, animal serum or detergents as any of these additives may interfere with the Cortez S. typhi Antigen Test. REAGENT PREPARATION Bring all reagents, including test device, to room temperature (20-30) oC before use. STOOL SPECIMEN PREPARATION Add about 1/4 gram stool to approximately 500μl of the extraction reagent provided (about 12 drops from the dropper vial provided). Mix well and allow to sit for 5 minutes or so to allow the large particles to settle.(amount of stool, extraction reagent and appropriate wetting time depending on manufacturer). Note: Watery or diarrhea specimens are inappropriate for testing. PROCEDURE 1. Bring all materials and specimens to room temperature (8 – 30) °C. 2. Remove the test card from the sealed foil pouch. 3. For stool samples: use the provided pipette to transfer sample from the upper layer of the stool extract and add 3 drops to the sample well (marked as “A”). 210 | P a g e 4. For serum samples: use the provided pipette to transfer the serum sample and add 3 drops to the sample well (marked as “A”). 5. Read the result at 20 minutes. A strong positive sample may show test band earlier. However, to confirm a result is negative, it must wait 20 minutes to read the results. Note: The amount of S. typhi antigens present in serum is typically less than that in stool. This may decrease the sensitivity of the test when using serum depending how soon after the onset of the infection the test is performed. Early infection typically exhibits greater levels of the antigen in the serum than in later infection. To confirm serum results: The use of a stool sample is recommended if serum is used first and a negative result is obtained and typhoid is still suspected, A second test run on a stool sample should be performed. INTERPRETATION OF RESULTS Positive result: A distinct pink colored band appears on test line regions, in addition to a pink line on the control line region. Negative result: No line appears in the test line region. A distinct pink line shows on the control line Region. Invalid: The control line next to the test line does not become visible within 20 minutes after the addition of the sample. Figure 27: Interpretation of Salmonella Smart Test QUALITY CONTROL 211 | P a g e 1. The control band is an internal reagent and procedural control. It will appear if the test has been performed correctly and the reagents are reactive. 2. Good Laboratory Practice recommends the daily use of control materials to validate the reliability of the device. LIMITATIONS 1. The test is for qualitative detection of S. typhi antigen in stool or serum sample and does not indicate the quantity of the antigens. 2. The test is for in vitro diagnostic use only. 3. For samples that test positive (reactive) by Cortez S. typhi Antigen Test, more specific confirmatory testing should be done. A definitive clinical diagnosis should only be made by the physician after all clinical and laboratory finding have been evaluated. The use of a rapid test alone is not sufficient to diagnose S. typhi infection even if antigen is present. Also, a negative result does not preclude the possibility of infection with S. typhi. Specificity Negative stool samples from patients in areas where typhoid is relatively rare and would yield a typical negative population, showed no false positives when the test was read within 20 minutes as specified. Samples that were positive for s. paratyphi however were also negative as the antibodies used in the S. typhi rapid test are specific for S. typhi only. 6.6.3 Vibrio cholerae Rapid visual antigen detection test Vibrio cholerae strains belonging to the O1 and O139 serogroups are capable of causing epidemic and pandemic cholera. The O1 serogroup is subdivided into two serotypes, Ogawa and Indaba. Serogroup O139, which appeared in India in 1992, has spread rapidly throughout Asian countries and is considered to be the potential eighth pandemic strain of cholera. Prompt diagnosis of cholera is of key importance to initiate effective therapy and to institute proper epidemiological measures. There are definitive indications that the incidence of this serogroup is on the rise in India and Bangladesh. Several rapid diagnostic tests for cholera have been described. Some detect the cholera toxin. The others detect the lipopolysaccharide (LPS) antigen of V. cholerae O1 or O139. Recently, a multistep colloidal gold-based colorimetric immunoassay known as SMART was also developed for direct detection of V. cholerae O1 or V. cholerae O139 in stool specimens and has demonstrated 95% sensitivity and 100% specificity for O1 strains and 100% sensitivity and 97% specificity for O139 strains. Clinical Significant Clinically, cholera may range from asymptomatic colonization to sever diarrhea with massive fluid loss, leading to dehydration, electrolyte disturbances, and death. 212 | P a g e Principle This test is an immunochromatographic rapid visual antigen detection test for V. cholerae from stool specimens. The nitrocellulose membrane is coated with monoclonal antibodies to V. cholerae O1 and O139 lipopolysaccharide (LPS) as two distinct bands. When the test sample migrates through the nitrocellulose membrane, colloidal gold particles coupled with anti-V. cholerae O1 and O139 LPS monoclonal antibodies bind to the respective antigens from the test sample, if present. This antigen-antibody complex moves through the nitrocellulose membrane and binds to the corresponding immobilized antibodies against V. cholerae O1 and/or O139, forming a magenta red color band, which confirms positive results. A control test band should always appear, irrespective of a positive or negative test sample, to validate the test procedure. Materials and equipment In countries at risk for epidemics of cholera, the laboratory’s first role is to be prepared for a possible epidemic. It must have ready or have access to the supplies and equipment necessary to identify V. cholerae O1 and/or O139 even in remote locations. Contact the local laboratory, medical center, or field site where testing will be performed in advance to ensure all necessary supplies, equipment, and personal protective equipment (PPE) will be readily available. Supplies and equipment necessary to perform the rapid test Included with the rapid test kit: Individually packaged dipsticks in aluminum pouch with desiccant Plastic, individual, single-use 5-mL test tubes for sample. Disposable transfer pipettes (plastic droppers) for stool. Foam test tube stand. Sterile normal saline or distilled water Disposable, clean sample containers for stool specimen collection. Plastic rack of appropriate size for test tubes (suggested). Watch or timer. Biosafety supplies/personal protective equipment (PPE):Gloves Goggles or face shield Lab coat. Biohazard receptacle for infectious waste. Disinfectant. Storage The rapid test kit may be stored at ambient temperature (24–26) oC but it is recommended that the kit be stored at 4oC when not in use for 6 months or more (depending on manufacturer). Specimen’s collection 213 | P a g e Fecal specimens should be collected in the early stages of any enteric illness, when pathogens are usually present in the stool in highest numbers, and before antibiotic therapy has started. Collect stool specimens from persons who are suspected of being part of an outbreak and who meet the following criteria: 1. Currently have “rice water stool.” 2. Had onset of illness less than 4 days before sampling. 3. Have not received antimicrobial treatment for the diarrheal illness. Collect stools from patients in clean (no disinfectant or detergent residue) containers with tight-fitting, leak-proof lids. Do not collect specimens from bedpans, as they may contain residual disinfectant or other contaminants. Stool should be refrigerated if possible and processed within a maximum of 2 hours after collection. Suitable specimens: Liquid fecal specimens, ideal “rice water stool”—clear, watery stools, likened to water from boiled rice, an appearance classically seen in cholera cases. Viscous, mucoid, or semisolid stools—acceptable but must be diluted before use with normal sterile saline or sterile distilled water. Unacceptable specimens: Solid stools—not recommended, as particulate matter from these specimens may clog the nitrocellulose membrane restricting migration of the sample. Rectal swabs—the dipstick assay has not been evaluated for use with rectal swabs. Procedure 1. Put on personal protective equipment (PPE): lab coat, gloves, goggles and face shield. Wear PPE at all times while handling the specimen 2. Collect stool sample in plastic cup. Label cup with patient identifier. 3. Remove 1 test tube from kit and place test tube in Styrofoam or plastic rack. Label the test tube. 4. Remove 1 plastic dropper from kit. 5. Fill dropper halfway (150–200 µL) with stool sample, and transfer to test tube. Do not put more liquid than this amount in the test tube. 214 | P a g e 6. Open packet with rapid test, Label the dipstick with patient identifier. 7. Place the dipstick in the test tube with the arrows facing DOWN. The end of the strip should be submerged in the stool. The arrows should remain ABOVE the level of the stool. 8. Wait 15–20 minutes for the test to complete. When complete, you will see a band near the top control band of the dipstick (internal control band). 9. Review and interpret results within 15–20 minutes: A. Positive, V. cholerae O1 B. Positive, V. cholerae O139 C. Positive, both V. cholerae O1 and O139 D. Negative for V. cholerae O1 and O139 E. Test did not work correctly (invalid test) Do not interpret results after 30 minutes. A B C D E 10. Place all waste in a double-lined plastic bag labeled “biohazard.” Figure28: Rapid Test Instruction Sheet, for a graphic representation of the test procedure 1. Allow time for the kit to come to room temperature before opening and using. 2. Label a clean, unused test tube with the patient identification code. Transfer 150– 200 L of the patient’s liquid stool specimen to this test tube. Note: Viscous, mucoid, or semisolid specimens should be diluted with sterile saline or distilled water before transfer to the test tube. 3. Tear open aluminum pouch at notched area. Remove the dipstick. 4. Label the dipstick with the patient identification code; take care to not touch the area marked with an arrow (dipping area). 5. Carefully place the dipstick in the test tube with stool with the arrows facing DOWN. The end of the strip should be submerged in the stool. Be sure the arrows remain ABOVE the level of the stool. 6. Leave the dipstick undisturbed for 10–15 minutes or depending on manufacturers. 7. Within 15-20 minutes, a magenta red internal “control” band will appear indicating a valid test; this line indicates that the reaction is complete. The presence of at least one or two additional magenta red lines signifies the sample is positive for V. cholerae O1 and/or V. cholerae O139. 215 | P a g e 8. Read and record the result of the test within 15–20 minutes. Do not interpret results after 30 minutes. (Reading & interpretation the result depending on manufacturers). Interpretation and reporting of results Interpret test results of each dipstick according to the manufacturer’s instructions. Guidelines for interpreting test results can be found in Table (1-1). Record all patient test results in a worksheet or notebook as a permanent record. Record results as positive, negative, or invalid. If a test needs to be repeated because of an invalid test result, record the first result (invalid), resolve the problem, and record the repeated result. Report positive and negative test results to the appropriate person in a timely manner. The report should include any comments or information the person needs to properly evaluate the test results. Table 12: Expected Test Result Outcomes for the Dipstick and Interpretation of Test Results Dipstick Test Result Interpretation POSITIVE (Figures 3-1 and 3-2, column A): Appearance of two bands, one for the control test band and one test band specific for V. cholerae O1 (Vc O1). Indicative that the sample is positive only for V. cholerae O1. POSITIVE (Figures 3-1 and 3-2, column B): Appearance of two bands, one for the control test band and one test band specific for V. cholerae O139 (Vc O139). Indicative that the sample is positive only for V. cholerae O139. POSITIVE (Figures 3-1 and 3-2, column C): Appearance of three bands, one for the control test band, one test band specific for V. cholerae O1 (Vc O1) and one test band specific for V. cholerae O139 (Vc O139) Indicative that the sample is positive for both V. cholerae O1 and O139. NEGATIVE (Figures 3-1 and 3-2, column D): Appearance of only the control test band. Indicative that the sample is negative for V. cholerae O1 and O139. 216 | P a g e INVALID (Figures 3-1 and 3-2, column E): Appearance of no control test band Indicates a procedural error, deterioration of the specimen/dipstick or the presence of particulate matter in the specimen preventing flow of fluid through the nitrocellulose membrane. Quality control Common source of error Specimens that are not classified as “watery” may clog the nitrocellulose membrane strip, limit migration of the liquid, and prevent the dipstick reaction resulting in an invalid test. These specimens should be either diluted with sterile saline or distilled water or rejected as unacceptable specimens for testing. A B C D E Figure 29:Visual Interpretation of Rapid Dipstick Test Results Precautions Be sure to run the test exactly as instructed, adhering to all procedures. Use sterile technique throughout the test procedure. Wear gloves, goggles and face shield, and a lab coat when handling and testing all clinical specimens. 217 | P a g e 6.7 Preparation of Media With just a few diagnostic materials, a laboratory can make an important contribution to individual patient care through accurate etiological diagnosis. In most developing countries bacteriological laboratory practice is hampered by a shortage of culture media and basic reagents, which are very costly to import. However, the number of culture media and reagents that have to be purchased can be reduced to the essential ones, through rational selection, as has been the case with essential drug lists. Additionally, some simple media and reagents can be produced or prepared locally. Each batch of medium prepared from individual ingredients or each different manufacturer’s lot number of commercial dehydrated medium and each batch of medium prepared from individual ingredients should be quality controlled before use. Immediately after preparation, each medium should be tested, as appropriate, with a reference strain . for proper growth characteristics as described for each medium. A record of all media preparation or purchase dates and quality control test results should be kept, and any unusual characteristic (e.g., the color of the medium or slow growth of test bacteria) should be noted. Many media call for the use of defibrinated blood. Agar media should be dispensed into 15 x 100-mm or 15 x 150-mm Petri dishes to a uniform depth of 3–4 mm; approximately 20-ml of liquid agar medium will achieve this depth in a 15 x 100-mm plate. If agar is cooled to 50°C prior to pouring, condensation is minimized. After pouring, the plates should be kept at room temperature for several hours to prevent excess condensation from forming on the covers of the dishes. Another means by which condensation will be reduced is if plates are stacked so that they cool more slowly. Alternatively, if when preparing selective media (e.g., MacConkey [MAC], xylose lysine desoxycholate [XLD], thiosulfate citrate bile salts [TCBS] agar, etc.), conditions are such that there is little chance that the cooling media will be contaminated, after the agar is poured into the plates, the lids can be placed on the dish so that a small opening is left to let the heat out, resulting in the formation of less condensation on the upper lid; the lid should remain slightly open like this for approximately 30 minutes, while the agar solidifies. If, however, it is likely that the agar will be contaminated if the lid is left partly open, the agar should be allowed to solidify with the lid closed. Note: Covering the agar while it is still hot will allow for the formation of a substantial amount of condensation on the upper lid. If the plates contain condensation, the plates should be covered at room temperature for 24 hours to allow the condensation to evaporate. After condensation has evaporated, the plates should be placed in an inverted position and stored in a plastic bag in an inverted position at 4°C. 218 | P a g e 6.7.1 Blood agar: TSA with 5% sheep blood Sheep blood agar is used as a general blood agar medium, and consists of TSA plus 5% sheep’s blood. The sheep blood agar plate should appear a bright red color. If the plates appear dark red, the blood has been added when the agar was too hot; if this happens, the medium should be discarded and a new batch prepared. A. Prepare TSA according to the instructions given on the label of the dehydrated powder. For convenience, 500 ml of molten agar can be prepared in a l-liter flask. Add 20 g of agar into 500 ml of water. Heat to dissolve. B. Autoclave at 121°C for 20 minutes. Cool to 60°C. C. Add 5% sterile, defibrinated sheep blood (i.e., add 25 ml sheep blood to 500 ml of agar). If a different volume of basal medium is prepared, the amount of blood added must be adjusted accordingly to 5% (e.g., 50 ml of blood per liter of medium). D. Dispense 20 ml into 15 x 100-mm Petri dishes. Allow the medium to solidify and dry out, place in a plastic bag, and store at 4°C. Quality control: Test each new, freshly prepared or purchased batch of blood agar plates for growth and hemolytic reaction with a strain of S. pneumoniae. The colonies are small and should appear grey to grey-green surrounded by a distinct greenish halo in the agar. 6.7.2 Chocolate agar with TSA base and growth supplement Chocolate agar with growth supplements is a medium that supports the special growth requirements needed for the isolation of fastidious organisms (when incubated in a 5% CO2 atmosphere). Chocolate agar contains a reduced concentration of agar, which increases the moisture content of the medium. Supplemented chocolate agar should support the growth of H. influenzae. Chocolate agar slants for transport and short-term storage can be prepared in the same manner as that described for agar plates, except that the medium is dispensed in 16 x 125mm screw-cap tubes and slanted before solidifying. A. Use TSA as the basal medium. Prepare double strength (i.e., 20 g in 250 ml distilled water). Autoclave and then cool to 50°C. Use the thermometer to verify the cooling temperature. B. Prepare a solution of 2% hemoglobin (i.e., 5 g in 250 ml distilled water). Mix the hemoglobin in 5–6 ml of the distilled water to form a smooth paste. Continue mixing as the rest of the water is added. Autoclave, and cool to 50°C. C. Add the hemoglobin solution to the double-strength TSA and continue to hold at 50°C. D. • Alternative to steps a-c: If a hemoglobin solution is unavailable, an alternative is to add 5% sterile defibrinated sheep, rabbit, guinea pig, or horse blood (i.e., 5 ml blood per 100-ml agar) to full-strength TSA (i.e., 20 g in 500 ml distilled water). 219 | P a g e DO NOT use human blood. After the base medium has been autoclaved and cooled to 50°C, add the blood and place in E. a hot water bath at no more than 80°C for 15 minutes or until a chocolate color is achieved. Then cool to 50°C. F. After the hemoglobin solution or the defibrinated blood has been added to the base medium and the medium has cooled to 50°C, add growth supplement (e.g., IsoVitaleX or Vitox) to a final concentration of 1%.Mix the ingredients by gently swirling the flask; avoid forming bubbles. Dispense 15–20 ml in each 15 x 100mm Petri dish. Quality control: All freshly prepared or purchased chocolate agar media should be tested to determine the medium’s capacity to support growth of the bacteria to beisolated, particularly H. influenzae. If the medium does not support the growth ofone or all of the bacteria, the medium should be discarded, and a new batch of medium should be prepared or purchased. • Chocolate agar should look brown to brownish-red in color. N. meningitidis and H. influenzae should appear as a greyish, almost translucent film on the slant’s surface with no discoloring of the medium after 24 hours of incubation; S. pneumoniae should appear as small grey to grey-green colonies with a very distinct greenish discoloring of the medium . If H. influenzae does not grow, the growth supplement (IsoVitaleX or its equivalent) may have been inadvertently omitted.C 6.7.3 MacConkey agar (MAC) MacConkey agar (MAC) is a differential plating medium recommended for use in the isolation and differentiation of lactose-nonfermenting, gram-negative enteric bacteria from lactose- ermenting organisms. Colonies of Shigella on MAC appear as convex, colorless colonies about 2–3 mm in diameter. S. dysenteriae 1 colonies may be smaller. S. Typhi colonies are flat, colorless and usually 2–3 mm in diameter. Several commercial brands of MAC are available.Most manufacturers prepare several formulations of MAC, which may vary in selectivity and thereby affect the isolation of Shigella. For example, some formulations of MAC do not contain crystal violet, a selective agent; these types are not as selective and should not be used for isolation of Shigella. Oxoid MacConkey Agar No. 3, Difco Bacto MacConkey Agar, and BBL MacConkey Agar are all suitable. 220 | P a g e A. Prepare MAC according to manufacturer’s instructions. [Note: MAC can also be prepared from individual ingredients, but this produces more lot-to-lot variation than preparation of a commercially available dehydrated formulation.] B. Sterilize the medium by autoclaving at 121°C for 15 minutes. C. Cool to 50°C and pour into Petri plates (to a uniform depth of 3–4 mm). D. Leave lids ajar for about 20 minutes so that the surface of the agar will dry. Close lids and store at 4°C for up to 1 month. If plates are to be stored for more than a few days, put them in a sealed plastic bag to prevent drying. Quality control: For quality control of MAC, the following organisms should be adequate for confirmation of selective and inhibitory growth characteristics: • E. coli should produce pink to red colonies with good to excellent growth; and, • S. flexneri should produce colorless colonies with fair to good growth, but S. dysenteriae 1 colonies may be smaller. 6.7.4 Mueller-Hinton agar Mueller-Hinton agar is the NCCLS-recommended medium used for standardized antimicrobial susceptibility testing of certain bacteria; the organisms in this document for which it is appropriate to use this formulation of Mueller-Hinton medium (i.e., unsupplemented Mueller-Hinton) are S. Typhi, Shigella spp., and V. cholerae. [Note: Several formulations of Mueller-Hinton agar are commercially available. This laboratory manual suggests that Mueller-Hinton agar medium should not be prepared from individual ingredients because this can diminish the quality. Commercial dehydrated Mueller-Hinton is carefully quality controlled before being released for sale.] A. Follow manufacturer’s instructions to prepare medium. B. After autoclaving, cool medium to 50°C in a water bath. C. Measure 60–70 ml of medium per plate into 15 x 150-mm plates, or measure 25– 30 ml per plate into 15 x 100-mm plates. Agar should be poured into flatbottom glass or plastic Petri dishes on a level pouring surface to a uniform depth of 3–4 mm. Using more or less agar will affect the susceptibility results. Agar deeper than 4 mm may cause false-resistance results, whereas agar less than 4 mm deep may be associated with a false-susceptibility report. D. Freshly prepared plates may be used the same day or stored in a refrigerator (at 2°–8°C) for up to 2 weeks. If plates are not used within 7 days of preparation, they should be wrapped in plastic to minimize evaporation. Just before use, if excess moisture is on the surface, plates should be placed in an incubator (35°– 37°C) until the moisture evaporates (usually 10–30 min). Do not leave lids ajar because the medium is easily contaminated. 221 | P a g e Quality control: Each new lot of Mueller-Hinton agar should be quality controlled before use by testing the E. coli ATCC 25922 standard strain for antimicrobial susceptibility testing. (This formulation of Mueller-Hinton agar can also be used for testing of grampositive aerobes, in which case S. aureus ATCC 25923 can be used as a quality control strain.) The pH of each new lot of Mueller-Hinton should be between 7.2 and 7.4; if the pH is outside this range, the pH of the medium should not be adjusted by the addition of acid or base, i.e., the batch of Mueller-Hinton plates should be discarded and a new batch of plates prepared. If the pH for every batch is too high or low, the entire lot of dehydrated medium may have to be returned to the manufacturer as unsatisfactory. Inhibition zone sizes / minimal inhibitory concentration (MIC) values for quality control are included in the antimicrobial susceptibility testing section of each pathogenspecific chapter. 6.7.5 Cary-Blair medium, Amies medium, and Stuarts medium Prepare each of these transport media according to the manufacturer’s instructions. [Note: Several dehydrated formulations of Cary-Blair are commercially available; some require the addition of calcium chloride and some do not.] These media can also be prepared from individual ingredients; however, it is very difficult to make a well qualitycontrolled batch and so this manual recommends purchasing them from a manufacturer. When the Cary-Blair medium is prepared, it should be dispensed into containers in sufficient volume so that swabs will be covered by at least 4 cm of medium. For example, 5- to 6-ml amounts may be dispensed into 13 x 100-mm screw cap tubes. With the caps loosened, sterilize the medium by steaming (not by autoclave) at 100°C for 15 minutes. Tighten the caps after sterilization, and store the medium at 15°–30°C. These media are quite stable if stored in tightly sealed containers in a cool dark place so that the medium does not dry out. Each may be used for up to 1 year as long as no loss of volume, visible contamination (e.g., foreign objects or bacterial growth), or color change is observed. Prepared Amies medium that has been stored for longer than 9 months, however, should be freshly steamed and the charcoal re-suspended before use. 222 | P a g e 6.8 Staining Smears 6.8.1 Gram’s Stain Organisms are classified according to their Gram staining reaction. Gram positive bacteria have thicker and denser peptidoglycan layers in their cell walls. Iodine penetrates the cell wall in these bacteria and alters the blue dye to inhibit its diffusion through the cell wall during decolourisation. Gram positive bacteria must have an intact cell wall to produce a positive reaction. Gram negative cells which do not retain the methyl/crystal violet are stained by a counterstain26. Neutral red, safranin or carbol fuchsin may be used as the counterstain. Gram ’s Method for examination of smears 1. Prepare a smear and heat gently to fix. 2. Flood the slide with 0.5% methyl/crystal violet and leave for 30 s. 3. Tilt the slide, pour on sufficient (1%) Lugol’s iodine to wash away the stain, cover with fresh iodine and allow to act for 30 s. 4. Tilt the slide and wash off the iodine with 95 - 100% ethanol or acetone until colour ceases to run out of the smear. 5. Rinse with water. 6. Pour on 0.1% counterstain (neutral red, safranin or carbol fuchsin) and leave to act for about 2 min. 7. Wash with water and blot dry. Interpretation Positive Result Gram positive organisms stain deep blue/purple. Negative Result Gram negative organisms stain pink/red. Quality Control Organisms A culture containing Gram positive and Gram negative organisms may be used for quality control. 6.8.2 Ziehl-Neelsen’s stain (for acid fast bacilli) This staining technique is used to demonstrate the presence of acid and alcohol fast bacilli (AAFB) which have waxy envelopes that make them difficult to stain and decolourise. Auramine-phenol staining is more sensitive than Ziehl-Neelsen’s and is thus more suitable for assessment of smears from clinical specimens. Ziehl-Neelsen’s staining provides morphological details and is more useful for confirming the presence of AAFB in positive cultures. 223 | P a g e Method 1. Flood the slide with strong carbol fuschin. 2. Heat gently, and once slide is just ‘‘steaming’’ leave for 3-5 min. 3. Rinse well with water. 4. Decolourise for 2-3 min with a (3% v/v) acid-alcohol solution, rinse with water, then replace with fresh acid-alcohol for 3-4 min until the slide remains a faint pink colour. 5. Rinse well with water. 6. Counter stain with (1% w/v) methylene blue or malachite green for 30 s. 7. Rinse with water and allow to dry. 8. Apply immersion oil and read with a transmitted light microscope. Note: Follow manufacturer’s procedure if commercial kits are used. Interpretation Positive Result Acid fast bacilli vary from 0.5-10 μm in length16 and stain red. Some may appear beaded. Negative Result All other organisms and background material stain green if malachite green counterstain is used or blue if methylene blue counterstain is used. Quality control Positive Control Mycobacterium species. Negative Control A proven negative smear may be used as the negative control. 224 | P a g e Module five: Parasitology and biochemistry Module Objectives: At the end of this module the participant will be able to: 1. Diagnose malaria parasite 2. Apply biochemistry tests Modules Sessions Session 1: Parasitology Session 2: biochemistry Evaluation/ Assessment Questions and answers, participants’ summaries, trainer’s evaluation Estimated Training Time 5.30 hours 225 | P a g e Module 5 Session 1: Parasitology Objectives At the end of this session participants will be able to: 1. Apply method for malaria parasite diagnosis 2. Apply staining blood films with Giemsa stain Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Mini-lecture Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 50 minutes 226 | P a g e Session plan -1- Objectives 5.1.1 Apply method for malaria parasite diagnosis. 5.1.2.Apply staining blood films with Giemsa stain Content Method - Thin film - Thick film Methodology Mini-lecture 25 minutes Mini-lecture First method Second method 25 minutes 227 | P a g e 7. Parasitology 7.1 Malaria parasite diagnosis Malaria is a serious, sometimes fatal disease resulting from infection with Plasmodium spp. transmitted by the bite of Anopheline mosquitoes.. The clinical diagnosis, where malaria is suspected based on the history, symptoms and clinical findings must always be confirmed by a laboratory diagnosis. Laboratory diagnosis of malaria involves identification of malaria parasite or its antigens/products in the blood of the patient. Clinical significance Malaria parasites are usually detected in blood films stained with Field or Geimsa stains. They may also be detected using an immunological procedure known as a dipstick test It is important for the prognosis and treatment of the disease that the species involved are identified in the laboratory. Preparation of a thick and a thin blood film on the same slide There are four species of the genus plasmodium responsible for the malarial parasite infections that commonly infect man, P.falciparum, P.vivax, P.malariae and P.ovale. The most important of these is P.falciparum because it can be rapidly fatal and is responsible for the majority of malaria related deaths Clinical significance For routine malaria microscopy, a thin and a thick film are made on the same slide. The thick film is used for the detection of parasites, while the thin film is used in identifying the species of parasite Principal Blood to be examined for malaria parasites is usually collected at a health centre. The most suitable time for collection is at the height of an episode of fever, when the parasites are most numerous in the blood. Blood specimens should always be collected before anti- malarial drugs are given Cleaning the finger before collecting a capillary bloodsample Using a lancet to puncture the ball of the finger METHOD 1. With the patient’s left hand palm upwards, select the third or fourth finger. (The big toe can be used with infants. The thumb should never be used for adults or children.) Use cotton wool lightly soaked in ethanol to clean the finger — using firm strokes to remove 228 | P a g e dirt and grease from the ball of the finger, Dry the finger with a clean piece of cotton wool (or lint). 2. With a sterile lancet, puncture the ball of the finger, using a quick rolling action. By applying gentle pressure to the finger, express the first drop of blood and wipe it away with dry cotton wool. Make sure that no strands of cotton wool remain on the finger 3. Working quickly and handling clean slides only by the edges, collect the blood as follows: Apply gentle pressure to the finger and collect a single small drop of blood, about this size _, on to the middle of the slide. This is for the thin film. Apply further pressure to express more blood and collect two or three larger drops, about this size _, on to the slide about 1 cm from the drop intended for the thin film Wipe the remaining blood away with cotton wool. Thin film: Using another clean slide as a “spreader”, and with the slide with the blood drops resting on a flat, firm surface, touch the small drop with the spreader and allow the blood to run along its edge. Firmly push the spreader along the slide, away from the largest drops, keeping the spreader at an angle of 45° Make sure that the spreader is in even contact with the surface of the slide all the time the blood is being spread. Thick film: Always handle slides by the edges, or by a corner, to make the thick film as follows: Using the corner of the spreader, quickly join the larger drops of blood and spread them to make an even thick film, allow the thick film to dry in a flat, level position protected from flies, dust and extreme heat. Label the dry film with a grease pencil by writing across the thicker portion of the thin film the patient’s name or number and date. Materials and reagents Microscope Clean glass microscope slides Sterile blood lancets Cotton wool Grease pencil Methanol 70% Ethanol. Measuring cylinders, 10, 50 and 100ml Beakers, 50 and 250ml Staining troughs Glass rods Wash bottle Slide forceps Slide racks 229 | P a g e Timer Giemsa stain Methanol in a drop bottle Buffered water, pH 7.2 or distilled water Staining blood films with Giemsa stain Principle During staining of the blood film, the haemoglobin in the erythrocytes dissolves(de haemoglobin ization) and is removed by the water in the staining solution. All that remain are the parasites and the leukocytes, which can be seen under the microscope. First method: Rapid method for staining thick and thin blood films This method is suitable for rapid staining of thick films when urgent results are required. It uses much more stain than the regular method 1. Using forceps, place the slides back to back in a staining trough 2- Prepare a 3% Giemsa solution in buffered or distilled water, pH 7.2, in sufficient quantity to fill the number of staining troughs being used, mix the stain well. 3- Pour the stain gently into the staining trough, until all the slides are totally covered. Stain for 30–45 minutes out of sunlight. 4. Pour clean water gently into the trough to remove the deposit on the surface of the staining solution 5. Gently pour off the remaining stain), and rinse again in clean water for a few seconds. Pour the water off. Second method 1. Allow the thick film to dry thoroughly; if results are required urgently, drying may be hastened by fanning, or briefly exposing the slide to gentle heat such as that from a microscope lamp. Care should be taken to avoid overheating, otherwise the thick film will be heat-fixed 2. Fix the thin film by adding three drops of methanol, or by dipping it into a container of ethanol for a few seconds. To permit dehaemoglobinization, the thick film should not be fixed; therefore avoid exposure of the thick film to methanol or methanol vapour 3. Prepare a 10% Giemsa solution in buffered or distilled water, pH 7.2; if a small quantity is being used, three drops of stain per ml of buffered water will give the correct concentration of Giemsa solution. One slide requires about 3ml of madeup stain. Mix the stain well with a glass rod. 4. Gently pour the stain on to the slides or use a pipette. Stain for 5–10 minutes. 5. Gently flush the stain off the slides by adding drops of clean water. Do not tip off the stain and then wash, as this will leave a deposit of scum over the smears. 230 | P a g e 6. Place the slides in the slide rack to drain and dry, film side downwards; making sure that the film does not touch the slide rack. Microscopic examination Examine the slide under the microscope using the ¥100 objective. Malaria parasites found in the blood are at different stages of development Some malaria parasites have granules of pigments in their cytoplasm Thin blood films: In thin blood films, the infected erythrocytes may remain unchanged or have a different colors or shape, or may contain pink (“Schüffner’s”) or red (“James”) thin films can be used to identify the species of malaria parasite Note: In patients who have been suffering from malaria for a long time, monocytes may be seen in the thin blood film; the cytoplasm often contains brown or greenish black bodies (siderophils). In patients who have recently received an injection of an antimalarial drug, the parasites stain poorly and appear distorted and indistinct. Thick blood films: In thick blood films, the background should be clean and free from debris, as the infected erythrocytes are lysed. The malaria parasites should have deep red chromatin and blue or pale purplish-blue cytoplasm. In thick films stained with Giemsa, the nuclei of leukocytes should be stained dark purple. Schüffner’s dots may be seen around the malaria parasites. Thick blood films are used for estimating the parasite density, as described below. Reporting results If the result of the examination of the stained blood films is positive, specify: the species of parasite found the stage of development of the parasite the parasite density. Blood films containing P. ovale and P. vivax may contain few parasites and therefore take more time to examine under the microscope. However, it is necessary to differentiate the two species, since they may reappear in the blood without reinfection. Patients infected with P. ovale or P. vivax require additional treatment to eradicate the liver stages of these parasites. A patient can harbour more than one species of malaria parasite at the same time(e.g. P. falciparum and P. malariae or P. falciparum and P. vivax). If the result is negative, report as “no parasites found”. 231 | P a g e Figure 30: P. Falciparum 1: Normal red cell , 2-18:Trophozoites (among these) , 2-10:correspond to ring stage trophozoites , 19-26:Schizonts (26 is ruptured schizont), 27&28: Mature macrogametocytes , 29&30:Mature microgametocytes (male) 232 | P a g e Figure 31: P. Ovale 1: Normal red cell , 2-5: Young trophozoites (Rings) , 6-15:Trophozoites , 1623:Schizonts , 24:Macrogametocytes( female) , 25: Microgametocytes (male) 233 | P a g e Figure 32: P. Vivax 1: Normal red cell , 2-6: Young trophozoites (Ring stage parasites) , 718:Trophozoites , 19-27:Schizonts , 28&29:Macrogametocytes( female) , 30: Microgametocytes (male) 234 | P a g e Module 5 Session 2: Biochemistry Objectives At the end of this session participants will be able to: 1. Estimate blood glucose level 2. Estimate ALT 3. Estimate AST 4. Estimate Alkaline Phosphatase 5. Estimate total serum bilirubin 6. Estimate renal function test (blood urea, serum creatinine, uric acid) 7. Estimate total cholesterol and triglycerides 8. Estimate HDL Cholesterol LDL Cholesterol Trainers Preparation: Review the reading material and the session plan. Prepare the presentation as appropriate and as recommended in the method column of the session plan, or write the information on a flipchart or board where all participants can see it. Prepare copies of the reference materials/handouts and exercises. Arrange the training room. Methods and activities Mini-lecture, question & answers, discussion, discussion-lecture Evaluation/assessment Questions and answers, trainer’s observation Estimated Time 280 minutes 235 | P a g e Session plan -2- Objectives 5.2.1.Estimate blood glucose level Content 5.2.2.Estimate ALT 5.2.3. Estimate AST 5.2.4. Estimate Alkaline Phosphatase Causes of Hyperglycemia Causes of hypoglycemia Reagents and materials Procedure Reference intervals Causes of high ALT Principle Specimen Reagents and materials Reference value Limitation Causes of high AST Principle Specimen Reagents and materials Reference value Limitation Principle Specimen Reagents and materials Procedure Methodology Question &answers 30 minutes Mini-lecture 30 minutes Question & answer 20 minutes Question & answer 20 minutes 236 | P a g e 5.2.5. Estimate total serum bilirubin 5.2.6. Estimate renal function test (blood urea, serum creatinine, uric acid) 5.2.7. Estimate total cholesterol and triglycerides 5.2.8. Estimate HDL Cholesterol and LDL Cholesterol Reference value Discussion Principle Specimen Reagents and materials Procedure Reference value Limitation Blood urea Serum creatinine Uric acid Discussion- lecture Lipid profile - Total cholesterol - Triglycerides Lipid profile - HDL Cholesterol - LDL Cholesterol 30 minutes 60 minutes Question & answers 45 minutes Question & answers 45 minutes 237 | P a g e 238 | P a g e 8. Biochemistry 8.1 Blood glucose Glucose is the chief source of energy in the body. The levels of this compound are balanced by digestion and absorption of carbohydrates in the intestine, its storage and release in the liver and its utilisation in the muscle. Causes of Hyperglycemia: Insulin – dependent type (IDDM) Non – insulin dependent type (NIDDM) non obese NIDDM obese NIDDM Gestational diabetes Impaired glucose tolerance: Glucose intolerance associated with certain conditions and syndrome such as (chronic pancreatitis with endocrine and exocrine insufficiency, cushing syndrome , acromegaly ) Causes of hypoglycemia: Deficient glucose production Ketotic hypoglycemia Glycogen storage disorder Deficiency of gluconeogenic enzyme Galactosemia Hereditary fructose intolerance Leucine hypersensitivity Endogenous hyperinsulinism Glucose is determined after enzymatic oxidation in the presence of glucose oxidase. The hydrogen peroxide formed reacts, under catalysis of peroxidase, with phenol and 4aminophenazone to form a red-violet quinoneimine dye. The intensity of the colour produced is directly proportional to the concentration of glucose in the sample. Glucose + O2+H2O --------------GOD H2O2 + Gluconate 2H2O2+ Phenol+ 4-Amino-antipyrine H2O+ Quinonimine SPECIMEN Serum, heparin plasma, or fluoride plasma may be used. Plasma or serum samples without preservatives should be separated from the cells or clot within a half hour of being drawn. Glucose in separated, un-hemolyzed serum is stable up to four hours at 25°C and up to 24 hours at 4°C. REAGENTS AND MATERIALS 239 | P a g e 1- Full automated auto analyzer or Spectrophotometer 2- Centrifuge 3- Gel tube (clot activator) 4- Spectrophotometer cuvettes 5- Deionized water 6- Pipettes 7- Glucose standards 20 mg/dL 100 mg/dL, 200 mg/dL, 400 mg/dL 8- Heating block or water bath 37°C 9- Timer 10- Reagents : Reagent 1 Buffer solution Reagent 2 tris buffer pH 7 Phenol glucose oxidase Peroxidase 4-amino-antipyrine Reagent 3 standard glucose Preparation: Dissolve the powder R2 with the Buffer R1 100 mmol/l 0.3 mmol 10 000 u/l 1 000 u/l 2.6 mmol/l 100 mg/dl PROCEDURE Wave length ………… 505 nm ( 490 – 550) Temperature………….37 ċ Blank Standard Sample Standard 10 µl Sample 10µl Working reagent 1 ml 1ml 1ml Mix incubate 10 minutes at 37 ċ or 30 minutes at room temperature ( 20 ċ – 30 ċ ) The color is stable 30 minutes Linearity : up to 500 mg / dl Calculation: Glucose concentration =O. D. sample / O.D. standard * concentration of standard . QUALITY CONTROL Level one and level two serum controls are tested with each patient run. The level one control range is 70-85 mg/dL and the level two range is 271-306 mg/dL. RESULTS Using graph paper, plot the Absorbance on the vertical (y axis) against the concentration on the horizontal (x axis) for each of the glucose standards. 240 | P a g e 1- Draw a "best fit line" and use this standard curve to determine the glucose concentration for the controls and patient specimens. 2- Verify that the control results are acceptable before reporting patient results. 3REFERENCE INTERVALS The reference range for glucose is as follows: Cord 45-96 mg/dL Premature 20-60 mg/dL Newborn 40-60 mg/dL 1 wk 50-80 mg/dL Child 60-100 mg/dL Adult 74-100 mg/dL >60 yr 82-115 mg/dL >90 yr 75-121 mg/dL LIMITATIONS 1- Serum and plasma must be separated from the red blood cells promptly to prevent glycolysis. Glucose will decrease approximately 7% per hour when left in contact with red cells. 2- Whole blood glucose is 12-15% less than serum glucose. 3- Venous blood glucose is approximately 5 mg/dL less than arterial or capillary blood glucose. 8.2 Liver Function Test 8.2.1 Alanine Aminotransferase (ALT) Is found mainly in the liver, but also in smaller amounts in the kidneys , heart , muscles, and pancreas. ALT is measured to see if the liver is damaged or diseased. Low levels of ALT are normally found in the blood. But when the liver is damaged or diseased, it releases ALT into the bloodstream, which makes ALT levels go up. Most increases in ALT levels are caused by liver damage. The ALT test is often done along with other tests that check for liver damage, including aspartate aminotransferase (AST), alkaline phosphatase, lactate dehydrogenase (LDH), and bilirubin. Both ALT and AST levels are reliable tests for liver damage. Causes of high ALT: Alcohol abuse 241 | P a g e Medications Acute and Chronic hepatitis Principle: Kinetic determination of ALT activity , method recommended by IFCC 2-oxoglutarate +l-alanine-----ALT-------- glutamate + pyruvate Pyruvate + NADH + H+-----------LDH------- l-lactate + NAD+ The rate of NADH consumption is determined photometrically and is direct proportional to the ALT activity in the sample SPECIMEN A. Recommended specimen: 100 μl of serum or heparinised plasma or EDTA plasma. Collect specimens by standard venipuncture technique. Heparin may be used as an anticoagulant for plasma specimens. Handle specimens in stoppered containers to avoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or other serum-based products. Discard contaminated materials with infectious waste. B. Remove serum promptly from the clot. Haemolysed specimens should not be used because ALT contamination from red cells will occur. DO NOT freeze the sample; this will cause a loss of ALT activity. C. If concentration is greater than the analyser range, dilute with an equal volume of isotonic saline and re-analyses. Multiply the result by 2 to obtain the original ALT activity. REAGENTS AND MATERIALS A. full automated autoanalyzer or spectrophotometer B. Centrifuge C. Gel tube (clot activator) D. Reagents : Reagent 1 tris buffer P H 7.5 Buffer reagent L-alalnine Reagent 2 NADH Substrate LDH Oxoglutarate 100mmol/l 500 mmol/l 0.18 mmol/l 1200u/l 15 mmol/l Preparation: Dissolve one vial of reagent 2 with 3 ml of R 1 buffer, this working reagent stable 13 days at 2 – 8 ċ or 24 hours at 20 – 25 days. Procedure: Wave length ----------340 nm Working reagent 1 ml mixed with sample 100 µl and wait 1 minute 242 | P a g e Measure the extinction decrease per minute for 1 – 3 minutes Calculation : Δ OD/min * 1750 = u/l QUALITY CONTROL 1. Run quality control materials in normal and abnormal ranges (low and high controls) at the beginning of each day. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. 2. Variability is expressed as standard deviation (SD) and coefficient of variation CV) and plotted on a Levy-Jennings graph. Reference value: Women up to 31 u/l at 37 ċ Men up to 40 u/l at 37 ċ RESULTS 1- Panic values: are double or triple to the normal value. 2- Becareful . Reference value for the end point procedure is differed from the reference value for the kinetic procedure. LIMITATIONS A. High total protein samples that are predominantly gamma globulins can increase ALT results. The sample should be diluted with an equal volume of isotonic saline and then reanalysed. B. In sera with very high activities, the initial absorbance may be very low because most of the NADH may have been consumed before the first readings. In this case, return the sample after dilution as described above. 8.2.2 Aspartate Aminotransferase (AST) AST (Aspartate transaminase ): AST is normally found in red blood cells, liver, heart, muscle tissue, pancreas, and kidneys. AST formerly was called serum glutamic oxaloacetic transaminase. Low levels of AST are normally found in the blood. When body tissue or an organ such as the heart or liver is diseased or damaged, additional AST is released into the bloodstream. The amount of AST in the blood is directly related to the extent of the tissue damage. After severe damage, AST levels rise in 6 to 10 hours and remain high for about 4 days. 243 | P a g e The AST test may be done at the same time as a test for alanine aminotransferase, or ALT. The ratio of AST to ALT sometimes can help determine whether the liver or another organ has been damaged. Both ALT and AST levels can test for liver damage. Causes of increase AST: Alcohol abuse . viral hepatitis, acute MI Principle: Kinetic determination of ALT activity , method recommended by IFCC 2-oxoglutarate +l-aspartate-----AST-------- glutamate + oxaloacetate oxaloacetate + NADH + H+-----------MDH------- malate + NAD+ The rate of NADH consumption is determined photometrically and is direct proportional to the ALT activity in the sample. SPECIMEN A. Recommended specimen: 100 μl of serum or heparinised plasma or EDTA plasma. Collect specimens by standard venipuncture technique. Heparin may be used as an anticoagulant for plasma specimens. Handle specimens in stoppered containers to avoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or other serum-based products. Discard contaminated materials with infectious waste. B. Remove serum promptly from the clot. Haemolysed specimens should not be used because AST contamination from red blood cells will occur. Refrigerate specimens if analysis is not performed immediately. Freeze specimens if analysis is not performed within 48 hours. C. If concentration is greater than the analyser range, dilute with an equal volume of isotonic saline and reanalyse. Multiply the result by 2 to obtain the original AST activity. REAGENTS AND MATERIALS 1- full automated auto analyzer or spectrophotometer 2- Gel tube (clot activator) 3- Centrifuge 4- Reagents : Reagent 1 tris buffer P H 7.8 80mmol/l Buffer reagent L-aspartate 200 mmol/l Reagent 2 NADH 0.18 mmol/l Substrate LDH 800u/l Oxoglutarate 12 mmol/l MDH 600 u/l Preparation: 244 | P a g e Dissolve one vial of reagent 2 with 3 ml of R 1 buffer , this working reagent stable 21 days at 2 – 8 ċ or 24 hours at 20 – 25 days . Procedure: Wave length ----------340 nm Working reagent 1 ml mixed with sample 100 µl and wait 1 minute Measure the extinction decrease per minute for 1 – 3 minutes Calculation: Δ OD/min * 1750 = u/l Reference value: Women up to 31 u/l at 37 ċ Men up to 38 u/l at 37 ċ QUALITY CONTROL A. Run quality control materials in normal and abnormal ranges (low and high controls) at the beginning of each shift. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. B. Variability is expressed as standard deviation (SD) and coefficient of variation (CV) and plotted on a Levy-Jennings graph. LIMITATIONS A. High total protein samples that are predominantly gamma globulins can increase AST results. The sample should be diluted with an equal volume of isotonic saline and reanalysed. Highly active sera can have a very low initial absorbance because much of the NADH is already consumed prior to measurement. In such cases, dilute sample as specified. B. Analyser range: ≤ 150 U/L 8.2.3 Alkaline Phosphatase Alkaline phosphatase is an enzyme used by the cells to speed up the time of a reaction. It is found in the bone, placenta, kidneys, small intestines and liver, but is primarily associated with liver disease and the obstruction of bile flow. Within the liver, alkaline phosphatase is located near or within the tubes that collect bile. Principle: Phenyl phosphate-----------ALP-------- phenol + phosphate Free phenol liberate by hydrolysis of substrate reacts then with 4-amino-antipyrine in the presence of alkaline. Potassium ferricyanide to form a red – colored complex which absorbance measured at 510 nm is directly proportional to ALP activity . sodium arsenate incorporated in the reagent abolishes further enzyme activity and prevent the dilution of the color inherent in earlier methods . SPECIMEN 245 | P a g e Recommended specimen: 20 μl of serum or heparinised plasma. Collect specimens by standard venipuncture technique. Handle specimens in stoppered containers to avoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or other serum-based products. Discard contaminated materials with infectious waste. Haemolysed specimens should not be used and samples more than 7 days old should not be used due to loss of the enzyme activity in 7 days. If absorbance change per minute exceeds 0.250, dilute 0.1 ml of the sample with 0.5 ml of normal saline and repeat the assay using this dilution. Multiply the results by 6 to obtain the alkaline phosphatase activity. REAGENTS AND MATERIALS A. full automated autoanalyzer or spectrophotometer . B. Gel tube (clot activator) C. Centrifuge D. Reagents : reagent 1 substrate buffer disodium phenylphosphate carbonate-biocarbonate buffer P H 10 stabilizer Reagent 2 phenol Standard Reagent 3 4- aminoantipyrine Blocking reagent sodium arsenate Reagent 4 potassium ferricyanide Dye reagent 5 mmol/l 50 mmol/l 20u/l 60 mmol/l 240 g/l 150 mmol/l CALIBRATION A. Empty and wash flow-through cuvette by pressing [WASH] on the LCD display. An automatic return to the select menu will occur. B. Push sip by pressing lever [P] to drain the tube system. Do not sip any solution. C. Measure exactly 1,000 μl of distilled water into a sample cup and sip distilled water by pushing sip-press lever [P]. The sipping volume of 1,000 μl is automatically measured in the flow-through cuvette. D. The length of transportation of the air and water will be displayed on the screen. E. Press [↵] to finish calibration. The program will return to method select menu. QUALITY CONTROL 246 | P a g e A. Run quality control materials in normal and abnormal ranges (low and high controls) at the beginning of each shift. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. B. Variability is expressed as standard deviation (SD) and coefficient of variation (CV) and plotted on a Levy-Jennings graph. PROCEDURE Serum blank R1 2 ml Incubate for 5 minutes at 37 ċ Serum R2 Incubate for 15 minutes at 37 ċ R3 0.5 ml Mix well R4 0.5 ml Serum 0.5µl D.W. - Serum sample 2ml Standard 2ml Regent blank 2ml 50 µl - 50 µl - 0.5 ml 0.5 ml 0.5 ml 0.5 ml - 0.5 ml - 0.5 ml 50 µL Mix well wait for 10 minutes in dark place, read at 510 nm against blank . Calculation: Conc.of ALP = O.D of serum / O.D. of standard * concentration of standard Linearity: up to 285 u /l Reference value: children 17 – 142 u / l Adult 21 – 92 u /l Conv F.: kau/dl * 7.09 = u/l 8.2.4 Total Serum Bilirubin bilirubin is formed from the haem fragment of haemoglobin released by damaged or aged RBC . bone marrow , liver and spleen are the sites of bilirubin production . Causes for an increase in total bilirubin may be divided into 3 categories: Pre- hepatic: resulting from various haemolytic states; Hepatic: resulting from hepatitis, cirrhosis, and other causes of hepatic necrosis;\ Post-hepatic: resulting from an obstruction of the common bile or hepatic duct. Principle: 247 | P a g e Sulfanilic acid react with sodium nitrate to form diazotized sulfanilic acid . in the presence of dimethyl sulfoxide . total bilirubin react with dizotized sulfanilic acid form azobilirubin . SPECIMEN A. Recommended specimen is 100 μl of serum or heparinised plasma. Collect specimens by standard venipuncture technique. Handle specimens in stoppered containers to avoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or other serum-based products. Discard contaminated materials with infectious waste. B. Protect specimens from light and analyse as soon as possible after collection. Direct exposure to sunlight is reported to cause as much as 50% loss of bilirubin in one hour, especially when the specimen is kept in a capillary tube. Exposure to normal room light can result in a significant loss of serum bilirubin after 2 to 3 hours. C. If analysis is not performed immediately, samples can be refrigerated for up to 24 hours at (2–5)°C. D. Samples that come in contact with alcohol from sterile wipes may become haemolysed, which will increase the value of bilirubin. E. If concentration is greater than the analyser range, dilute with 5 volumes of normal saline and reanalyse. Multiply the result by 6 to obtain the original total bilirubin concentration. The results may show a positive bias of up to 30%. REAGENTS AND MATERIALS A. spectrophotometer and bilirubimnometer for neonate . B. Centrifuge C. Gel tube (clot activator) D. Reagents : Reagent 1 sulfanilic acid 30 mmol/l Hydrochloric acid 150 mmol/l Dimethylsulfoxide 7 mol/l Reagent 3 sodium nitrate 20 mmol/l Reagent 4 Standard Procedure: Working reagent: Mix Reagent 1 20 volumes Reagent 3 1 volume Stability in absence of light 6 hours at 20-25 ċ 2 days at + 4 ċ 248 | P a g e Wave length -------------- 555nm Temperature ------------- 37 ċ Read against R1 sample blank Read against R1 + R3 (working reagent ) sample and standard CALIBRATION A. Empty and wash flow-through cuvette by pressing [WASH] on the LCD display. An automatic return to the select menu will occur. B. Push sip by pressing lever [P] to drain the tube system. Do not sip any solution. C. Measure exactly 1,000 μl of distilled water into a sample cup and sip distilled water by pushing sip-press lever [P]. The sipping volume of 1,000 μl is automatically measured in the flow-through cuvette. D. The length of transportation of the air and water will be displayed on the screen. E. Press [↵] to finish calibration. The program will return to method select menu. QUALITY CONTROL A. Run quality control materials in normal and abnormal ranges (low and high controls) at the beginning of each shift. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. B. Variability is expressed as standard deviation (SD) and coefficient of variation (CV) and plotted on a Levy-Jennings graph. PROCEDURE CALCULATIONS Sample Calibrator(R4) Reagent(R1) Working reagent Sample blank 50 µl 1 ml - Sample 50 µl 1 ml Standard blank 50 µl 1 ml - Standard 50 µl 1 ml Mix and read the extinction after incubation for 5 minutes at 37 ċ Stability of color is 1 hour ( ovoid direct sunlight ) Calculation: ( O.D sample – O. D. sample blank ) / ( O. D. calibrator – O. D. calibrator blank ) * n N = calibrator concentration Linearity: linear up to 20 mg / dl , 340 µmol/l 249 | P a g e Reference value: Serum total bilirubin: < 1 mg/dl, < 17 µmol / l Conv. F. : mg / dl * 17.1 = µmol/l LIMITATIONS A. Specimens from haemodialysis patients should not be analysed for total bilirubin. B. Haemoglobin affects bilirubin results. C. Compounds that discolour serum, such as 4-aminosalicylic acid and phenazopyridine, may falsely increase bilirubin results. D. Results for predominantly unconjugated bilirubin (e.g., for neonates) may be up to 10% higher than the reference method. 8.3 Renal Function test 8.3.1 Blood Urea The liver produces urea in the urea cycle as a waste product of the digestion of protein , Elevated levels of blood urea are most commonly associated with renal disease, but may also result from dehydration, a high-protein diet, excess destruction of body proteins, and gastrointestinal diseases, especially with intestinal obstruction. Principle: Urea + H2O --------urease------ CO2 + 2NH3 Salicylate and hypochlorite in the reagent react with the ammonium ions to form 2.2dicarboxy –indophenol . the quantity of green compound is proportional to the urea concentration. SPECIMEN A. Recommended specimen is 10 μl of serum or EDTA plasma. Collect specimens by standard venipuncture technique. Heparin may be used as an anticoagulant for plasma specimens. Handle specimens in stoppered containers to avoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or other serum-based products. Discard contaminated materials with infectious waste. B. Refrigerate specimens up to 3 days at 4°C if analysis is not performed immediately. C. If concentration is greater than the analyser range, dilute with 9 volumes of isotonic saline or distilled water and reanalyse. Multiply the result by 10 to obtain the original urea nitrogen concentration. REAGENTS AND MATERIALS A. full automated auto analyzer or spectrophotometer B. Gel tube (clot activator) C. Centrifuge D. Reagent : 250 | P a g e R1a R1b R2 CAL urease phosphate buffer Sodium salicylate Sodium nitroprusside EDTA sodium hypochloride Sodium hydroxide standard >5000 u/l 120 mmol/l p H 7 63.4 mmol/l 5 mmol/l 1.5 mmol/l 18 mmol/l 750 mmol/l 8.05 mmol/l Preparation: Add 1 vial of of urease R1a to one bottle of phosphate buffer R1b Procedure : Wave length …….600 nm Temperature ……25 ċ – 37 ċ CALIBRATION A. Empty and wash flow-through cuvette by pressing [WASH] on the LCD display. An automatic return to the select menu will occur. B. Push sip by pressing lever [P] to drain the tube system. Do not sip any solution. C. Measure exactly 1,000 μl of distilled water into a sample cup and sip distilled water by pushing sip-press lever [P]. The sipping volume of 1,000 μl is automatically measured in the flow-through cuvette. D. The length of transportation of the air and water will be displayed on the screen. E. Press [↵] to finish calibration. The program will return to method select menu. QUALITY CONTROL A. Run quality control materials in normal and abnormal ranges (low and high controls) at the beginning of each shift. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. B. Variability is expressed as standard deviation (SD) and coefficient of variation (CV) and plotted on a Levy-Jennings graph. PROCEDURE 251 | P a g e Blank Standard standard 10µl sample Working reagent 1 ml 1 ml Mixture incubated for at least 3 minutes at 37 ċ or 5 min. at 20-25 ċ sample 10µl 1 ml Sodium 200 µl 200 µl 200 µl hypochloride mix. incubate for at least 5 min. at 37 ċ or 10 min. at 20-25 ċ , measurement is against reagent blank . Calculation: O.D.sample / O.D. standard * concentration of standard CALCULATIONS The results are reported in mmol/L. No further calculation is necessary unless the specimen has been diluted. Conversion Urea = 2.14 × BUN BUN = 0.466 × Urea RESULTS A. Expected values: (urea) 1.7–8.3 mmol/L B. Panic values: <1.07 mmol/L and >37.1 mmol/L C. Each laboratory should confirm these values. LIMITATIONS A. Do not use plasma collected with sodium fluoride. B. Specimens that contain haemoglobin increase urea nitrogen. Haemoglobin of 50 mg/dL (slightly haemolysed) increases BUN levels below 28 mg/dL by 1 mg/dL. C. Ammonium ions have shown an increase in urea nitrogen equivalent to their nitrogen content. 8.3.2 Serum Creatinine Creatinine measurement is used in the diagnosis and treatment of renal diseases and in monitoring patients on renal dialysis. Analysis of creatinine activity in 100 μl of serum or plasma is based on an enzymatic method that produces a coloured product. A. The 100 μl of patient sample mixed with picrate in alkaline medium produces a coloured complex with creatinine. The rate of formation of the complex is then measured. 252 | P a g e B. The creatinine present in the sample reacts with the picrate at 37°C, and the rate of complex formation is measured and is proportional to the creatinine concentration. SPECIMEN A. Recommended specimen is 100 μl of serum or heparinized plasma. Collect specimens by standard venipuncture technique. Heparin may be used as an anticoagulant for plasma specimens. Handle specimens in stoppered containers to avoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or other serum-based products. Discard contaminated infectious waste. B. Refrigerate specimens at 4°C for 24 hours if analysis is not done immediately. REAGENTS AND MATERIALS A. Photometer B. Gel tube (clot activator) C. Centrifuge D. Picric acid 26 mmol/L E. NaOH 1.6 mmol/L F. Creatinine 2 mg/dL or 176.8 μmol/L CALIBRATION A. Empty and wash flow-through cuvette by pressing [WASH] on the LCD display. An automatic return to the select menu will occur. B. Push sip by pressing lever [P] to drain the tube system. Do not sip any solution. C. Measure exactly 1,000 μl of distilled water into a sample cup and sip distilled water by pushing sip-press lever [P]. The sipping volume of 1,000 μl is automatically measured in the flow-through cuvette. D. The length of transportation of the air and water will be displayed on the screen. E. Press [↵] to finish calibration. The program will return to method select menu. QUALITY CONTROL A. Run quality control materials in normal and abnormal ranges (low and high controls) at the beginning of each shift. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. B. Variability is expressed as standard deviation (SD) and coefficient of variation (CV) and plotted on a Levy-Jennings graph. PROCEDURE A. Mix reagents according to manufacturer’s recommendations. 253 | P a g e B. Label 2 tubes: in tube or standard tube pipette 1,000 μl of reagents solution and 100 μl of creatinine standard reagent; and in tube 2 or sample tube pipette 1,000 μl of reagents solution and 100 μl of sample. C. Mix them well and measure them immediately as indicated. D. Press ZERO and then push sip by pressing lever [P] to sip water and drain the system. E. When the screen displays MEASURE STANDARD, place cuvette with the standard solution into cuvette holder and aspirate the standard solution by pushing lever [P]. F. When the screen displays MEASURE SAMPLE, place cuvette with the sample solution into cuvette holder and aspirate the sample solution by pushing lever [P]. G. Press [RESULT] and await possible delay while measuring the sample solution. The result will be displayed on top line. H. Print or write out the results. Press [WASH] to sip rinse solution or press [MEASURE] to measure the next sample by pushing sip lever [P]. CALCULATIONS The results are reported in μmol/L. No further calculation is necessary unless the specimen has been diluted. RESULTS A. Expected values: Males: 53–97 μmol/L Females: 44–80 μmol/L B. Panic values: < 27 μmol/L and > 663 μmol/L C. Each laboratory should confirm these values. LIMITATIONS A. EDTA and fluoride/oxalate anticoagulants will cause low creatinine results. B. Lidocaine: Patients on long-term lidocaine therapy may show an increase of up to 1.0 mg/dL. Ninety percent of patients receiving intravenous lidocaine will show less than a 0.3 mg/dL increase. C. Proline: Patients receiving hyperalimentation fluid that contains proline may show an increase of up to 2.0 mg/dL. D. TRIS buffer (control fluid) causes an approximate 50% decrease in results. E. Dipyrone (Metamizol) at 40 mg/dL shows a –0.6 mg/dL bias at a creatinine concentration of 1.0 mg/dL. F. N-acetylcysteine: Patients receiving N-acetylcysteine (Fluimucil, Mucomyst) intravenously have been reported to show a large negative bias. 8.3.3 Uric acid Uric acid is a chemical created when the body breaks down substances called purines. Purines are found in some foods and drinks ,Most uric acid dissolves in blood and 254 | P a g e travels to the kidneys, where it passes out in urine. High levels of uric acid in the body is called hyperuricemia. Principle : Uric acid +O2 +H2O---------uricase -------- allantoine + CO2 + H2O2 2H2O2 +4-aminophenazone+ 2-4dichloro- phenol-sulfonate -----------peroxidase------- quinonemine Reagents: Reagent 1 phosphate buffer P H 7.4 50mmol/l Buffer solution 2-4 DCPS 4 mmol/l Reagent 2 uricase 7o u/l Vial of enzyme peroxidase 660 u/l 4-aminophenazone 1 mmol/l uric acid 6 mg/dl Reagent 3 Standard Preparation : Dissolve the content of one bottle R 2 with the content of one bottle buffer R 1 Procedure : Wave length---------------------510 nm (490 – 550) Blank Standard Sample Working reagent 1 ml 1 ml 1 ml Standard - 20µl - Sample - - 20 µl mix. incubate 5 minutes at 37 ċ or 10 minutes at 20-25 ċ the colour is stable for 30 minutes . 255 | P a g e calculation : concentration= O.D.sample / O.D. standard * concentration of standard reference value : women 2.5 – 6 mg/dl,148 – 357 µmol / l men 3.4 – 7 mg/dl , 200 – 416 µmol / l Conv. F. : mg/dl * 60 = µmol / l 8.4 Lipid Profile 8.4.1 Total Cholesterol Cholesterol is a waxy, fat-like substance that occurs naturally in all parts of the body. Your body needs some cholesterol to work properly. But if you have too much in your blood, it can stick to the walls of your arteries. This is called plaque. Plaque can narrow your arteries or even block them. High levels of cholesterol in the blood can increase your risk of heart disease. Your cholesterol levels tend to rise as you get older. There are usually no signs or symptoms that you have high blood cholesterol, but it can be detected with a blood test. You are likely to have high cholesterol if members of your family have it, if you are overweight or if you eat a lot of fatty foods. You can lower your cholesterol by exercising more and eating more fruits and vegetables. You also may need to take medicine to lower your cholesterol. Causes of hypercholesterolemia: 1- familial hypercholesterolaemia (FH) 2- reduced metabolism due to thyroid problems(hypothyroidism) 3-kidney diseases 4- diabetes particularly when poorly controlled 5- alcohol abuse 6- being overweight – this is probably the commonest cause of high cholesterol levels. Causes of hypocholesterolemia : 1-Hyperthyroidism 2-Liver disease 3-Malnutrition 4-Cancer 5-Chronic infections or inflammation Principle: 256 | P a g e Esters of cholesterol +H2O -------chloesterol esterase-------> cholesterol + fatty acids Cholesterol +O2 ---------cholesterol oxidase -----------> cholest-4-en-one +H2O2 H2O2 +phenol+4-aminophenazone ------------peroxidase ------------> quinonimine SPECIMEN A. Recommended specimen 10 μl of serum, heparinised or EDTA plasma. Collect specimens by standard venipuncture technique. Heparin may be used as an anticoagulant for plasma specimens. Handle specimens in stoppered containers to avoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or other serum-based products. Discard contaminated materials with infectious waste. B. If the result is over 19.3 mmol/L, dilute the sample before precipitation 1:2 with normal saline and multiply the results by 3 to obtain the original cholesterol concentration. C. Cholesterol remains stable in serum for 6 days at 4–25°C and up to 4 months at – 20°C. D. Lipemic specimens generate turbidity of the sample/reagent mixture, which leads to falsely elevated results. REAGENTS AND MATERIALS A. spectrophotometer B. Gel tube (clot activator) C. Centrifuge D. Reagents : Reagent 1 pipes p H 6.9 90 mmol/l Buffer solution Phenol 26 mmol/l Reagent 2 cholesterol oxidase 399 u/l Vial of two enzymes Peroxidase 1250 u/l Cholesterol oxidase 300 u/l 4-aminophenazone 0.4 mmol/l Reagent 3 standard 200 mg/dl Preparation: Dissolve the contents of one bottle R2 to the contents of one bottle buffer reagent R1 Sample: serum , heparinized plasma Procedure: Wave length …………… 505nm ( 500 550) Temperature …………... 37 ċ 257 | P a g e Blank Standard standard 10µl sample Working reagent 1 ml 1 ml Mix. incubate 5 minutes at 37 ċ ,the colour is stable for 30 min. Calculation: sample 10µl 1 ml Cholesterol concentration = O.D.sample / O.D. standard * concentration of standard QUALITY CONTROL A. Run quality control materials in normal and abnormal ranges (low and high controls) at the beginning of each shift. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. B. Variability is expressed as standard deviation (SD) and coefficient of variation (CV) and plotted on a Levy-Jennings graph. CALCULATIONS The results are reported in mmol/L. No further calculation is necessary unless the specimen has been diluted. RESULTS A. Expected values: 3.6–5.2 mmol/L. B. Each laboratory should confirm these values. LIMITATIONS A. Bilirubin concentrations above 4 mg/dl interferes with tests B. If results are over 25.9mmol/l dilute the sample and repeat measument C. High concentration of ascorbic acid (> 2.5 mg/dL) will give lower values. D. Haemoglobin levels higher than 200 mg/dL do not interfere with the test. 8.4.2 Triglycerides Triglycerides protein is essential for growth, the production of new tissue, and the repair of injured tissue. An increase in triglycerides levels may be the result of nephrosis, cholestasis, pancreatitis, cirrhosis, diabetes mellitus, and hepatitis. Adecrease is seen with malnutrition. The analysis is based on the enzymatic hydrolysis of triglycerides with lipases in a quinoneimine formed from hydrogen peroxide used as a coloured indicator. The intensity of the colour is proportional to the amount of triglycerides in the sample. 10 μl of patient sample is mixed and incubated with 1,000 μl of solution containing 4- aminoantipyrine and 4-chlorophenol in presence of hydrogen peroxide. After incubation for 10 minutes, a reaction between 4-aminoantipyrine and 4-chlorophenol and hydrogen peroxide takes place, forming quinoneimine, which is a coloured 258 | P a g e product. The amount of coloured compound formed is proportional to the amount of triglycerides in the specimen. SPECIMEN A. Recommended specimen 10 μl of serum, heparinised or EDTA plasma. Collect specimens by standard venipuncture technique. Heparin may be used as an anticoagulant for plasma specimens. Handle specimens in stoppered containers to avoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or other serum-based products. Discard contaminated materials with infectious waste. B. Avoid haemolysed specimens. If analysis is not performed immediately, freeze specimens at −25oC for up to 4 months or refrigerate at 2–8oC for up to 3 days. C. If concentration is greater than the analyser range, dilute 1 part of sample with 4 parts of isotonic saline or distilled water and reanalyse. Multiply the result by 5 to obtain the original triglycerides concentration. REAGENTS AND MATERIALS A. Photometer B. Gel tube (clot activator) C. Centrifuge D. Reagent PIPES buffer (pH 7.5) 50 mmol/L 4-chlorophenol 5 mmol/L 4-aminoantipyrine 0.25 mmol/L Magnesium ion 4.5 mmol/L ATP 2 mmol/L Lipases ≥1.3 U/ml Peroxidase ≥0.5 U/ml Glycerol kinase ≥0.4 U/ml Glycerol-3-phpsphate oxidase ≥1.5 U/ml Standard Triglyceride 2.28 mmol/L CALIBRATION A. Empty and wash flow-through cuvette by pressing [WASH] on the LCD display. An automatic return to the select menu will occur. B. Push sip by pressing lever [P] to drain the tube system. Do not sip any solution. C. Measure exactly 1,000 μl of distilled water into a sample cup and sip distilled water by pushing sip-press lever [P]. The sipping volume of 1,000 μl is automatically measured in the flow-through cuvette. D. The length of transportation of the air and water will be displayed on the screen. E. Press [↵] to finish calibration. The program will return to method select menu. QUALITY CONTROL 259 | P a g e A. Run quality control materials in normal and abnormal ranges (low and highcontrols) at the beginning of each shift. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. B. Variability is expressed as standard deviation (SD) and coefficient of variation (CV) and plotted on a Levy-Jennings graph. PROCEDURE A. Mix 2 tubes: one blank with 1,000 μl of standard reagent, and tube 2 with 10 μl of serum or plasma and 1,000 μl of reagent solution. B. Mix each well and incubate for 5 minutes at 37oC, and measure the absorbance of the standard reagent and sample immediately as indicated. C. Press ZERO and then push sip by pressing lever [P] to sip water and drain the system. D. When the screen displays MEASURE RB, place cuvette with the blank solution into cuvette holder and aspirate the blank solution by pushing lever [P]. E. When the screen displays MEASURE SAMPLE, place cuvette with the sample solution into cuvette holder and aspirate the sample solution by pushing lever [P]. F. Press [RESULT] and await possible delay while measuring the sample solution. The result will be displayed on top line. G. Print or write out the results. Press [WASH] to sip rinse solution or press [MEASURE] to measure the next sample by pushing sip lever [P]. CALCULATIONS The results are reported in mmol/L. No further calculation is necessary unless the specimen has been diluted. RESULTS A. Expected values: 0.11–2.15 mmol/L. B. Each laboratory should confirm these values. LIMITATIONS A. Lipemic specimen usually generates turbidity of the sample reagent mixture, which leads to falsely elevated results. B. Ascorbate gives falsely low values. 8.4.3 HDL Cholesterol High density lipoprotein (HDL) is lipoprotein which is involved in the transport of cholesterol from the cells to the liver. An increase in HDL levels may be the result of nephrosis, cholestasis, pancreatitis, cirrhosis, diabetes mellitus, and hepatitis. A decrease is seen with malnutrition. The analysis is based on the precipitation of chylomicrons, very low-density lipoprotein (VLDL), and low density lipoprotein (LDL) upon addition of phospshotungstic acid and 260 | P a g e magnesium chloride to the sample. The HDL is contained in the supernatant, which can be enzymatically assayed after centrifugation of the supernatant. The absorbance of the sample and the standard reagent is measured against blank reagent. When 200 μl of test sample is mixed with 500 μl of precipitant reagent containing phosphotungstic acid and magnesium chloride at room temperature for 10 minutes chylomicrons, VLDL, and LDL are precipitated . Centrifugation at 10,000 g for 2 minutes leaves only the HDL in the supernatant, where the concentration of HDL in the sample is determined enzymatically. SPECIMEN A. Recommended specimen 200 μl of serum, heparinised or EDTA plasma. Collect specimens by standard venipuncture technique. Heparin may be used as an anticoagulant for plasma specimens. Handle specimens in stoppered containers toavoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or otherbased products. Discard contaminated materials with infectious waste. B. If the supernatant is not clear, dilute the sample before precipitation 1:1 with normal saline and multiply the results by 2 to obtain the original HDL concentration. C. HDL cholesterol remains stable in serum for 6 days at 4–25°C and up to 4 months at –20°C. Serum must be separated from the blood clot as rapidly as possible. REAGENTS AND MATERIALS A. Photometer B. Gel tube (clot activator) C. Centrifuge D. Reagent (Precipitant) Phosphotungstic acid 0.55 mmol/L Magnesium chloride 25 mmol/L Standard Cholesterol 1.29 mmol/L CALIBRATION A. Empty and wash flow-through cuvette by pressing [WASH] on the LCD display. An automatic return to the select menu will occur. B. Push sip by pressing lever [P] to drain the tube system. Do not sip any solution. C. Measure exactly 1,000 μl of distilled water into a sample cup and sip distilled water by pushing sip-press lever “P”. The sipping volume of 1,000 μl is automatically measured in the flow-through cuvette. D. The length of transportation of the air and water will be displayed on the screen. E. Press [↵] to finish calibration. The program will return to method select menu. QUALITY CONTROL 261 | P a g e A. Run quality control materials in normal and abnormal ranges (low and high controls) at the beginning of each shift. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. B. Variability is expressed as standard deviation (SD) and coefficient of variation (CV) and plotted on a Levy-Jennings graph. PROCEDURE A. Into a glass centrifuge tube mix 200 μl of test sample (serum or plasma) 500 μl of precipitant reagent. (Dilute precipitant reagent with distilled water 4 in 1.) B. Mix them well and incubate for 10 minutes at room temperature. C. Centrifuge at 4000 rpm for 10 minutes or 10,000 rpm for 2 minutes. D. After centrifugation remove the clear supernatant and into tube 1 (sample) add 100 μl of supernatant and 1,000 μl of total cholesterol reagent. In tube 2 (reagent blank) add 100 μl of distilled and 1,000 μl of cholesterol reagent. E. Mix them well and incubate for 10 minutes at 20–25°C or 5 minutes at 37°C and measure their absorbance. F. When the screen displays MEASURE BLANK, press ZERO and then push sip by pressing lever [P] to sip water and drain the system. G. When the screen displays MEASURE RB, place cuvette with the blank solution into cuvette holder and aspirate the blank solution by pushing lever [P]. H. When the screen displays MEASURE SAMPLE, place cuvette with the sample solution into cuvette holder and aspirate the sample solution by pushing lever [P]. I. Press [RESULT] and await possible delay while measuring the sample solution. The result will be displayed on top line. J. Print or write out the results. Press [WASH] to sip rinse solution or press [measure] to measure the next sample by pushing sip lever [P]. CALCULATIONS The results are reported in mmol/L. No further calculation is necessary unless the specimen has been diluted. RESULTS A. Expected values: 0–0.9 mmol/L. B. Each laboratory should confirm these values. LIMITATIONS A. High triglyceride level interferes with HDL measure; dilute the sample before precipitation 1:1 with 0.9% saline and multiply the results by 2. B. High concentration of ascorbic acid (> 2.5 mg/dL) will give lower values. C. Haemoglobin levels higher than 100 mg/dL and bilirubin levels higher than 10 mg/dL interfere with the test. 262 | P a g e 8.4.4 LDL Cholesterol Low density lipoprotein (LDL) is lipoprotein which is involved in the transport of cholesterol to the cells. An increase in LDL levels may be the result of altered diet and vascular diseases. A decrease is seen in AIDS, haematological malignancies such as acute myeloid leukaemia (AML) or chronic myeloid leukaemia (CML), and disorders involving splenomegaly. The analysis is based on direct homogenous enzymatic assay for quantitative determination of LDL cholesterol combining two steps. The analysis involves removal of chylomicrons, very low density lipoprotein (VLDL), and high density lipoprotein (HDL), followed by enzymatic determination of LDL in the sample. 10 μl of patient sample is mixed and incubated at 37oC for 5 minutes with 750 μl of enzyme solution containing cholesterol esterase and cholesterol oxidase, which allows the removal of chylomicrons, VLDL, and HDL from the specimen by formation of cholestenone and hydrogen peroxide. The LDL present in the sample is converted to cholestenone and hydrogen peroxide in the presence of cholesterol esterase, cholesterol oxidase, and specific surfactant. The chromogen in presence of hydrogen peroxide peroxidase is converted to a coloured dye (quinine) whose concentration is measured by colorimetric method. SPECIMEN A. Recommended specimen 10 μl of serum or plasma. Collect specimens by standard venipuncture technique. Heparin may be used as an anticoagulant for plasma specimens. Handle specimens in stoppered containers to avoid contamination and evaporation. Follow universal precautions when performing phlebotomy or handling patient specimens, calibrators, or other serum-based products. Discard contaminated materials with infectious waste. B. If the serum concentration of LDL exceeds the measuring range, dilute the sample before precipitation 1:1 with normal saline, repeat the test, and multiply the results by 2 to obtain the original LDL concentration. C. LDL cholesterol remains stable in serum for 6 days at 4–25°C and up to 4 months at –20°C. D. Serum must be separated from the blood clot as rapidly as possible. REAGENTS AND MATERIALS A. Photometer B. Gel tube (clot activator) C. Centrifuge D. Reagent (enzymes) Good’s buffer (pH 7.0) 50 mmol/L Cholesterol esterase 600 U/L Cholesterol esterase 500 U/L 263 | P a g e Catalase 600 kU/L TOOS 2.0 mmol/L Detergents 0.3% w/v Preservatives <0.1% w/v Substrate Peroxidase 4000 U/L 4-Aminoantipyrin 4 mmol/L Good’s buffer (pH 7.0) 50 mmol/L Sodium azide 0.05% Detergents 1% w/v Preservatives <0.1% w/v CALIBRATION A. Empty and wash flow-through cuvette by pressing [WASH] on the LCD display. An automatic return to the select menu will occur. B. Push sip by pressing lever [P] to drain the tube system. Do not sip any solution. C. Measure exactly 1,000 μl of distilled water into a sample cup and sip distilled water by pushing sip-press lever [P]. The sipping volume of 1,000 μl is automatically measured in the flow-through cuvette. The length of transportation of the air and water will be displayed on the screen. D. Press [↵] to finish calibration. The program will return to method select menu. QUALITY CONTROL A. Run quality control materials in normal and abnormal ranges (low and high controls) at the beginning of each shift. Always run a set of controls after calibrating the analyser. If the controls are out of range, do not report patient results until the problem is resolved and the patient samples are repeated with quality control samples within acceptable range. B. Variability is expressed as standard deviation (SD) and coefficient of variation (CV) and plotted on a Levy-Jennings graph. PROCEDURE A. Label 2 tubes and pipette 10 μl water and 750 μl of enzyme solution into tube 1 (blank), and into tube 2 pipette 10 μl of test sample and 750 μl of enzyme solution. Mix gently and incubate at 37oC for 5 minutes. B. Into each tube add 250 μl of substrate solution and mix them well and incubate for 5 minutes at 37°C, then measure absorbance of sample against reagent blank. C. When the screen displays MEASURE BLANK, press ZERO and then push sip by pressing lever [P] to sip water and drain the system. D. When the screen displays MEASURE RB, place cuvette with the blank solution into cuvette holder and aspirate the blank solution by pushing lever [P]. E. When the screen displays MEASURE SAMPLE, place cuvette with the sample solution into cuvette holder and aspirate the sample solution by pushing lever [P]. 264 | P a g e F. Press [RESULT] and await possible delay while measuring the sample solution. The result will be displayed on top line. G. Print or write out the results. Press [WASH] to sip rinse solution or press [MEASURE] to measure the next sample by pushing sip lever [P]. CALCULATIONS The results are reported in mmol/L. No further calculation is necessary unless the specimen has been diluted. RESULTS A. Expected values: 0–0.9 mmol/L. B. Each laboratory should confirm these values. NOTE: Direct measurement of LDL is required instead of the Friedwald, or “calculated”, method whenever triglyceride values exceed 400 mg/dL. The Friedwald or “calculated” method of LDL determination is determined by subtracting HDL and VLDL from the total cholesterol concentration. Total cholesterol = HDL + LDL + VLDL. VLDL is generally estimated by the triglyceride concentration divided by 5, but is inaccurate when triglyceride values exceed 400 mg/dL. LIMITATIONS A. High triglyceride level interferes with LDL measure; dilute the sample before precipitation 1:1 with 0.9% saline and multiply the results by 2. B. High concentration of ascorbic acid (> 2.5 mg/dL) will give lower values. C. Haemoglobin levels higher than 100 mg/dL and bilirubin levels higher than 10 mg/dL interfere with the test. 265 | P a g e Annex 1 TABLE 1 - Outline of the properties of heat decontamination methods. For everyday laboratory purposes, autoclaving is the preferred method, unless the item cannot withstand the heat and/or moisture of autoclaving. Principle/Conditions Advantages Disadvantages Dry Heat Thermal inactivation: Nondestroys by oxidation corrosive Simple design and principle Hot Air Oven · 160-180?C for 2-4 hours · penetrates waterinsoluble materials (e.g., grease and oil) Uses Less effective than moist heat; requires longer times and/or higher temperatures Materials that are damaged by, or are impenetrable to, moist heat · slow diffusion, penetration · anhydrous materials, such as oils, greases and powders · loading, packing critical · laboratory to performance glassware, · less instruments · not suitable corrosive to · closed metals and for reusable plastics containers sharp instruments than steam Red-heat Flame · oxidation to ashes (burning) · rapid · initial contact with flame can · inoculating loops, needles 266 | P a g e produce a viable aerosol · possibility of accidental fire Incineration · oxidation to ashes (burning) · 1-60 minutes: temperatures may exceed 1000?C · reduces volume of waste by up to 95% · improper use may lead to emission of pathogens in smoke · for decontamination of waste items prior to disposal in landfill · requires transport of infectious waste · excess plastic (>20%) content reduces combustibility Moist Heat Irreversible coagulation of (microbial) proteins Pasteurization · heating to below boiling point (generally 77?C) for up to 30 minutes More rapid and more effective than dry heat · can be · not reliably used on heat sporicidal sensitive liquids and medical devices · milk and dairy products · some heatsensitive medical equipment · low cost 267 | P a g e Tyndallization · heating to 80(Fractional 100?C for 30 mins on Sterilization) successive days, with incubation periods in between Boiling autoclaving · resistant spores germinate and are killed on the second and third days · time consuming · not reliably sporicidal · heat sensitive materials such as bacteriologic media, solutions of chemicals, biological materials · maximum · minimal temperature equipment obtainable is required approximately 100?C 10-30 mins · cumbersome: · small not practical instruments and for everyday equipment lab use · steam under pressure · loading and · penetration of packing critical sterile to performance glassware, media and · shielding dirt instruments must first be removed · decontamination · maintenance of reusable and quality supplies and control equipment essential · · damages decontamination heat-sensitive of infectious itmes waste · 121?C/15 psi for 15-90 mins (gravity displacement autoclave) · 132?C/27 psi for 420 minutes (prevacuum autoclave) · minimal time required · most dependable sterilant for lab use · not reliably sporicidal TABLE 2 - Summary of concentrations used, contact times, advantages and disadvantages and uses of some of the halogen-releasing chemical germicides. The wide ranges of effective concentrations and contact times cited are due to a number of factors, including the interdependence of time and concentration, the variability in 268 | P a g e resistance of different microorganisms, the amount of organic material present and the desired effect (e.g., low-level vs high-level disinfection) Effective Concentrations Disadvantage Advantages , Contact s Times Chlorine Compounds: Sodium hypochlorite solution 1 (liquid bleach) · 100-10,000 ppm (.01-1%) free chlorine · broad spectrum · · 10-60 minutes inexpensive (>= 3,000 ppm · widely for broad available spectrum) · bactericidal at low temperature Examples of Uses · toxic, corrosive to skin and metals · general disinfectant · unstable at optimum effective pH of 6 · surface decontaminatio n · inactivated by organic matter · waste liquids · emergency spill clean up · instrument disinfection · deteriorates under light and heat: shelf life of dilutions is less than 1 week Calcium hypochlorite2 granules, powder, tablets · as for liquid bleach NaDCC3 (Sodium · as for liquid dichloroisocyanurate bleach ) powder, granules, tablets · as for liquid bleach but more stable · as for liquid · as for liquid bleach above, bleach except shelf life is longer · more · toxic, stable than corrosive hypochlorite s · as for liquid bleach 269 | P a g e Chloramine-T4 (Sodium tosylchloramide) powder or tablets · as for liquid bleach · stable at pH 6.0 · inactivated by organic matter · more stable, less affected by organic matter than hypochlorite s · deteriorates · as for liquid under bleach humidity, light and heat · longer activity than hypochlorite s Chlorine dioxide5 · demandrelease of chlorine dioxide in situ · longer activity than other chlorine compounds · aqueous solutions decompose under light · instrument disinfection · not consistently sporicidal · germicidal soaps and antiseptics · less corrosive, less toxic than other chlorine compounds · gas sterilization of germ-free animal chambers · effective at pH 6-10 Iodine Preparations: Iodophors6 · 30-1,000 ppm · broad (.003-.1%) free spectrum iodine · germicidal · 10-30 minutes over a wide pH range · efficacy · surface reduced by decontaminatio organic matter n 270 | P a g e · generally nonstaining, less toxic and less irritating than aqueous or alcoholic iodine solutions · some iodophor solutions support growth of Pseudomonas7 · work surface wipedown · instrument disinfection TABLE 3A Summary of recommended concentrations, contact times, advantages and disadvantages of non-halogen chemical germicides. The wide ranges of effective concentrations and contact times cited reflect the interdependence of time and concentration as well as factors such as resistance of the particular class or strain of target microorganism(s) and desired effect. Also, some germicides are available in combinations (e.g., glutaraldehyde/phenol or peracetic acid/alcohol mixtures) which are synergistic whereby the components in combination produce a greater antimicrobial effect than the sum of their individual effects. Effective Concentrations and Contact Times Alcohols · 70-80% ethanol · 60-95% isopropanol · 10-30 minutes Advantages · low toxicity · rapid action · low residue Disadvantages · rapid evaporation limits contact time · non-corrosive · flammable, eye irratant Examples of Laboratory Uses · skin disinfectant (antiseptic) · surface decontamination · benchtop, · may damage cabinet rubber, plastic, wipedown shellac · ineffective against 271 | P a g e bacterial spores Phenolic Compounds · 400-50,000 · tolerant of ppm (.05-1.5%) organic load, "hard" dilution · 10-30 water minutes · leaves an active residue (may be desirable on some surfaces) · pungent odour, corrosive, some forms toxic · instruments and equipment disinfection · disinfection of floors and other surfaces · not sporicidal; limited activity · antiseptic against viruses soaps and lotions · biodegradable · leaves a residual film (undesirable in culture systems) · may support growth of bacteria1 Quaternary Ammonium Compounds · 500-15,000 · combined ppm (.05-1.5%) detergent and germicidal · 10-30 activity minutes · stable · working dilutions have low toxicity · non sporicidal, limited activity against viruses, mycobacteria · surface decontamination · most formulations not readily biodegradable · antiseptic formulations available · equipment wipedown · floors and · may support walls growth of bacteria2 272 | P a g e Hydrogen Peroxide · 3-30% aqueous solution · rapid action · 10-60 minutes · low toxicity · 6% for 30 minutes may kill spores · no residue · limited sporicidal activity · corrosive to some metals · surface decontamination · instruments and equipment · environmentally · potentially safe explosive at high concentrations · stock solutions irritating to skin and eyes Peracetic Acid · .001-.3% aqueous (PAA) solution · broad spectrum · pungent odour · gas phase: 24% · sporicidal at low temperatures corrosive to some metals · 5-120 minutes · can tolerate organic load · rapid action · nontoxic decomposition products · leaves no residue · instruments and equipment · gas phase sterilization of chambers for · shelf life of germ-free dilutions is less animals than 1 week · stock solutions irritating to skin and eyes · stock must be protected from heat, light · gas phase: respiratory irritant, fire hazard above 55?C 273 | P a g e Table 3B - Summary of recommended concentrations, contact times, advantages and disadvantages of non-halogen chemical germicides. The wide ranges of effective concentrations and contact times cited reflect the interdependence of time and concentration as well as factors such as resistance of the particular class or strain of target microorganism(s) and desired effect. Also, some germicides are available in combinations (e.g., glutaraldehyde/phenol or peracetic acid/alcohol mixtures) which are synergistic whereby the components in combination produce a greater antimicrobial effect than the sum of their individual effects. Effective Concentrations Advantages Disadvantages and Contact Times Examples of Laboratory Uses Aldehydes: Glutaraldehyde · 0.5-2.5% alkalinized aqueous solution · broad spectrum · expensive · pH, temperature dependent · does not corrode · 2-30 mins; up metal · pungent to 12 hours to · can odour kill all spores tolerate organic load · toxic: skin, eye, respiratory tract irritant · cold sterilant and fixative · surface decontamination · instruments, equipment, glassware · activated solutions have less than 2week shelf life Formalin (37% aqueous formaldehyde) · 3-27% formalin (110% formaldehyde) · broad spectrum · pungent odour · cold sterilant and fixative 274 | P a g e in 70-90% alcohol · 10-30 minutes Formaldehyde (gas) Ethylene Oxide Gas · 1-3 hours · 50-1200 mg/L · 1-12 hours · · skin, eye and inexpensive respiratory tract irritant · does not corrode · potential metal carcinogen (animal · can studies) tolerate organic load · may require 24 hrs or more to kill all spores · surface decontamination · as for formalin · as for formulin · effective penetration · flammable · on site decontamination of biological safety cabinet HEPA filters · broad spectrum · porr penetration of covered surfaces · instruments and equipment · enclosed areas · flammable, reactive · heat or moisture sensitive · no heat or · toxic: supplies, moisture potential instruments and evolved carcinogen and equipment mutagen · penetrates packaging · some materials sterilized items may need more than 24 hours for outgassing 275 | P a g e References: 1. J. vandepitte & J. Verhaegen et al., Basic laboratory procedures in clinical bacteriology,WHO, geneva, 2nd edition, 2003 th 2. John Bernard Henry ,Clin. diagnosis & management by lab methods,19 edition, 1996. 3. Dacie and Lewis: PRACTICAL HAEMATOLOGY Tenth Edition. 4. Blood Cells: A Practical Guide, Fourth Edition. 5. Manual of basic techniques for a health laboratory. 6. Iraqi Ministry of Health\ Al Karkh Directorate SOP manual. 7. Betty a faubs, Daniel F Sahm and Alices S weiss feld. Baily and Scott, Diagnostic microbiology. Twelve edition 2007 Mosby Elsevier 8. Cedric Mims, Hazel M Dockrell, Richard V Goering etal medical Microbiology 3rd edition 2004 Mosby by Elsevier 9. Murray PR , Baron Ej , Pealler MA etal , editors Manual of clinical microbiology ed7,Washington, Dc 1999,ASM press 10.Rose NR, Friedman H., Manual of clinical immunology 2nd editor Washington, DC 1980 ASM press 11.Richard L Guerrant , David H walker and Peter F Weller Tropical infection disease principles, pathogens and practice Vol. 1 .1999 Churchill Livingstone. 276 | P a g e 12.Mandel GL. Bennett JE, Dolin R, editors, Principle and practice of infectious diseases ed5, Philadelphia 2000, Elsevier Churchill Livingstone. 13.Performance standard for antimicrobial susceptibility test M100-S22 VOL32, NO.3 ,2012 14.R.R Gillies ,T.C DODDS bacteriological illustrated 1971 Churchill Livingstone. 15.Vandepitte J., Engbaek K., Rohner P., Piot P. and Heuck C. C. Basic laboratory procedures in clinical bacteriology / 2nd ed. Geneva ,World Health Organization 2003. 16.Mekonnen E. Health Laboratory Management and Quality Assurance Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education.2004 17.Manual for Laboratory Diagnosis of Common Epidemic Prone Diseases at District Public Health Laboratories, National Center for Disease Control (India) .September 2009. 18.Standard Operating Procedures for Laboratory Services Laboratory Department Coast Provincial General Hospital Ministry of Health, Kenya ,March 2005. 19.Perilla M. J., Ajello G., Bopp C., Elliott J., Facklam R., Knapp J. S., Popovic T., Wells J., Scott F. Manual for the Laboratory Identification andAntimicrobial Susceptibility Testing of Bacterial Pathogens of Public Health Importance in the Developing World, Centers for Disease Control and Prevention: National Center for Infectious Diseases and World Health Organization: Department of Communicable Disease Surveillance and Response ,2003. 20.Manual of basic techniques for a health laboratory., 2nd ed. World Health Organization, Geneva ,2003 21.O’Connor, JH., Helicobacter pylori and gastric cancer: a review and hypothesis. Eur. J. Gastro. Hepa. 1992; 6: 103-109. 22.Mcguigan JE., Peptic ulcer and gastritis. In Harrison’s Principles of Internal Medicine, 12th Edition, 1988, Chapter 238, 1229-1248. 23.Cover TL. and Blaser MJ., Helicobacter pylori: A Bacterial Cause of Gastritis, Peptic Ulcer Disease, and Gastric Cancer, ASM News, 1995; 61: 21-26. 24.Podolsky I, Lee E, Cohen R, Peterson WL. Prevalence of H. pylori in healthy subjects and patients with peptic diseases. Gastroenteroloty 1989: 96: Suppl: A394. abstract. 25.Kist M., Immunology of Helicobacter pylori. In Helicobacter pylori in peptic ulceration and gastritis, edited by Marshall BJ., McCallum RW., and Guerrant RL., 1991, Chapter8, 92-110. 277 | P a g e 26.26.Ivanoff B. Typhoid fever, global situation and WHO recommendations. Southeast Asia J. Trop. Med. Public Health, 1995, 26:supp2 1-6 27.Parry CM, Hien TT Dougan G et al., Typhoid fever, N. Eng. J. Med. 2002, 347:177082. 28.Harris, JR., Cavallaro, EC., De Nobrega, AA., Dos S. Barrado, JCB., Bopp, C, Parsons, MB, Djalo, D, Fonseca, FG. dS, Ba, U, Semedo, A, Sobel, J. and Mintz, ED. (2009), Field Evaluation of Crystal VC® Rapid Dipstick Test for Cholera During a Cholera Outbreak in Guinea-Bissau. Trop Med Int Health 2009;14(9):1117-112. 29.Nato F, Boutonnier A, Rajerison M, Grosjean P, Dartevelle S, Guenole A, et al. Onestep immunochromatographic dipstick tests for rapid detection of Vibrio cholerae O1 and O139 in stool samples. Clin Diagn Lab Immunol 2003;10:476–8. 30.Kalluri P, Naheed A, Rahman S, Ansaruzzaman M, Faruque AS, Bird M, et al., Evaluation of three rapid diagnostic tests for cholera: does the skill level of the technician matter? Trop Med Int Health. 2006;11(1):49-55. 31.Mukherjee P, Ghosh S, Ramamurthy T, Bhattacharya MK, Nandy RK, Takeda Y, Nair GB, Mukhopadhyay AK. Evaluation of a rapid immunochromatographic dipstick kit for diagnosis of cholera emphasizes its outbreak utility. Jpn 278 | P a g e 279 | P a g e