Anatomy and Physiology with Integrated Study Guide Third Edition
advertisement

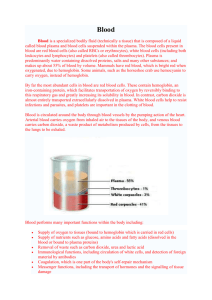
BLOOD AND DISORDERS BIO 238 Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Blood is confined within the heart and blood vessels Functions of blood Carry substances throughout the body Examples: oxygen and wastes Regulate pH of body tissues Prevent excessive blood loss due to hemorrhage Fight infections GENERAL CHARACTERISTICS OF BLOOD Blood is a fluid connective tissue It is heavier and more viscous then water Blood pH ranges between 7.35 and 7.45 Male blood volume: 5-6L Female blood volume: 4-5L Blood is ~8% of body weight 55% of blood volume consists of plasma Liquid matrix of blood 45% of blood volume consists of formed elements Most are red blood cells 1% are white blood cells and platelets RED BLOOD CELLS Also called erythrocytes Transports oxygen and carbon dioxide Biconcave shape allows for maximal surface area for gas diffusion Mature RBCs lack a nucleus Most numerous formed element HEMOGLOBIN Forms 33% of RBC volume Red pigment Components Heme: iron containing pigment Globin: protein Binds oxygen (to a small degree carbon dioxide) Oxygen-carrying hemoglobin is called oxyhemoglobin Bright red color Oxygen-deficient hemoglobin is called deoxyhemoglobin Dark red color CONCENTRATION OF RBCS Most abundant formed element Red blood cell count: clinical test to determine RBC number in a mm3 of blood Adult males>Adult females Males have higher metabolism; needs more O2 Increases with higher altitude Hematocrit: the percentage of RBC per volume of blood PRODUCTION Prior to birth, RBCs are produced by liver and spleen After birth, RBCs are produced by red bone marrow If blood oxygen level is low, erythropoietin is released by liver and kidneys Stimulates red bone marrow to make more RBCs Other factors required for production Iron is required for hemoglobin production Folic acid and vitamin B12 are needed for DNA synthesis during RBC formation B12 absorption from diet requires intrinsic factor secreted by the stomach lining All RBCs develop from hemocytoblasts in red bone marrow LIFE SPAN AND DESTRUCTION Live ~120 days Worn out RBCs are removed by phagocytes in liver and spleen Break down of heme Breaks into iron-containing compound and bilirubin Iron is recycled to form more hemoglobin Bilirubin is secreted by liver into bile, which enters the small intestine WHITE BLOOD CELLS Also called leukocytes Formed from hemocytoblasts in bone marrow Cells retain their nuclei ~4,500 to 10,000 per mm3 of blood WBC count increases whenever the cells encounter disease causing organisms or chemicals Function Provide defense against disease organisms or promote and decrease inflammatory responses Cells perform their functions within tissues Cells can migrate from blood into tissue Cells then follow a chemical trail to the site of damage TYPES OF LEUKOCYTES Grouped into two broad categories Granulocytes: possess cytoplasmic granules Neutrophils, eosinophils, basophils Agranulocytes: lack cytoplasmic granules Lymphocytes, monocytes Neutrophils Most abundant First WBCs to respond to tissue damage Number increases with acute bacterial infections Eosinophils Functions Perform phagocytosis and release the enzyme lysozyme Neutralize histamine released during allergic reactions Destroy parasitic worms Number increases during allergic reactions and parasitic worm infections Basophils Those that move into tissues are called mast cells Functions in damaged tissues and during allergic reactions Release histamine, which dilates blood vessels to increase blood flow Release heparin, which inhibits clot formation Lymphocytes Two types T lymphocytes Attack and destroy pathogens B lymphocytes Produce antibodies that attack bacteria and bacterial toxins Monocytes Function Phagocytosis of bacteria and cellular debris Once in tissues, they are called macrophages PLATELETS Also called thrombocytes Cytoplasmic fragments of megakaryocytes that develop from hemocytoblasts ~150,000 to 400,000 per mm3 of blood Functions Plug breaks in blood vessels Begin the clotting process PLASMA Straw-colored fluid portion of blood 90% water containing dissolved solutes and formed elements Contains a variety of solutes that are kept in a state of dynamic balance Plasma Proteins Most abundant solutes Most are produced by the liver Three types of plasma proteins Albumins Globulins Fibrinogen Albumins Most abundant protein Buffers to maintain pH of blood Maintain osmotic pressure of blood Globulins Alpha and beta globulins carry lipids and fat soluble vitamins in blood Gamma globulins are antibodies involved in immunity Fibrinogen Vital role in blood-clotting process Converted into insoluble fibrin to form blood clots Nonprotein Substances Amino acids: nutrients Urea and uric acid: waste products of protein Electrolytes Ions absorbed from intestine or released from cells Most common are Na+, K+, Ca++, Cl-, HCO3-, PO4— Help maintain osmotic pressure and plasma pH HEMOSTASIS Hemostasis is the stoppage of bleeding Involves three processes Vascular Spasm Platelet Plug Formation Platelets are attracted to damage site and adhere to exposed connective tissue Coagulation Constriction of the damaged vessel Restricts blood loss and lasts several minutes Clot formation After clot formation, fibrins contract and pull damaged tissues closer together Fibroblasts migrate into clot and repair the damage Later, tissue plasminogen activator (t-PA) converts plasminogen into plasmin Plasmin breaks down fibrin and dissolves blood clot HUMAN BLOOD TYPES Blood types are determined by specific antigens on RBC plasma membranes Antigen: special protein Common blood types involve the ABO blood group and the Rh factor Antibodies in blood will recognize antigens not found normally on the RBCs of that person Agglutination occurs when the antibodies bind foreign antigens Causes the foreign RBCs to clump together ABO BLOOD GROUP Type depends on the presence of antigen A and antigen B on RBCs Four types of blood are possible A, B, AB, and O Blood type will possess antibodies against the antigens NOT present on the RBCs Type AB blood is considered to be a universal recipient It possesses no antibodies so it will not react with any donated RBCs Type O is considered to be a universal donor It possesses both antibodies and will react with all donated RBCs except those of another type O Transfusion: donation of whole blood to an individual Blood is usually of same type Care must be taken to ensure blood is compatible with recipient blood Incompatible blood can result in widespread agglutination and fatality RH BLOOD TYPE Rh (D) antigen, first discovered in the Rhesus monkey If the antigen is present, blood is Rh+ If the antigen isn’t present, blood is Rh Erythroblastosis Fetalis Disorder in newborn infants resulting from destruction of fetal RBCs by maternal antibodies DISORDERS OF THE BLOOD Disorders can be grouped as Erythrocyte disorders Leukocyte disorders Clotting disorders ERYTHROCYTE DISORDERS Anemia Decreased oxygen-carrying capacity of blood Most common blood disorder Caused by decrease in RBC count or insufficient hemoglobin Nutritional anemia: insufficient iron and vitamin B12 in diet Hemorrhagic anemia: excessive loss of RBCs through bleeding Pernicious anemia: due to deficiency of intrinsic process Prevents absorption of B12 Hemolytic anemia: premature rupture of RBCs Aplastic anemia: due to destruction of red bone marrow or its inability to produce enough RBCs Sickle-cell anemia: due to abnormal hemoglobin that cannot carry enough oxygen Sickled RBCs rupture easily, causing hemolytic anemia Inherited disorder common in African blacks who lived in malarial regions Erythroblastosis fetalis Due to destruction of fetal Rh+ RBCs by a Rh+ mother’s anti-Rh antibodies Causes anemia, jaundice and presence of erythroblasts in fetal blood Polycythemia Excessive numbers of RBCs Increases blood volume and viscosity, which impairs circulation Possibly due to cancer of RBC forming cells LEUKOCYTE DISORDERS Infectious mononucleosis Contagious disease of lymphoid tissue by the EpsteinBarr virus Primarily in young adults Kissing is common mode of transmission Infects B lymphocytes Symptoms include fever and sore throat Lasts from four weeks to months to years Leukemia Cancers of the cells forming WBCs in bone marrow Excessive WBC production that inhibits RBC and platelet production Acute forms: children or young adults Chronic forms: adults Treatments include chemotherapy and bone marrow transplants CLOTTING DISORDERS Hemophilia Inherited diseases that are more common in males Involved spontaneous bleeding and reduced ability to clot blood Due to lack of a clotting factor Treatment involved transfusion containing missing clotting factor Thrombocytopenia Extremely low platelet number that permits spontaneous bleeding to occur Thrombosis Formation of a clot in an unbroken blood vessel If an artery is blocked, tissues are deprived of oxygen In areas roughened or damaged Thrombophlebitis Embolus: clot that breaks free and floats in blood Embolism: free-floating clot lodges in a vessel of the body and blocks blood flow