Introduction: Training – two separate issues: Transformation
advertisement

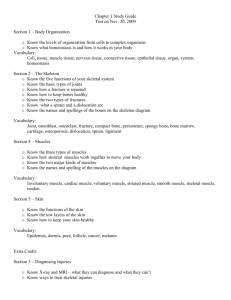
INTRODUCTION: Training – two separate issues: Transformation between fast and slow fibres (plasticity) i.e. some training can turn fast muscle fibres into slow fibres and vice versa, known as plasticity Hypertrophy vs. atrophy i.e. making your muscles bigger or smaller Muscle damage: Stretching contracting muscles cause minor damage e.g. walking downstairs, the quadriceps are used to slow you down while taking the steps below Muscle disease: Muscular dystrophy – caused by the lack of a single cytoskeletal protein in the muscle known as i.e. dystrophin Causes lethal muscle degeneration in males only (in their youth) Training: There are different effects of training on muscles leading to different outcomes e.g. the appearance of muscles – particularly the bulk of muscle e.g. body builder vs. endurance runner Body builders do small numbers of maximal contractions of each muscle group (results include enlarged pectoral muscles, biceps, quadriceps, all the muscles are enlarged because every muscle group is cyclically trained daily) – causes hypertrophy Successful endurance runners do very large numbers of low force (a few % of maximal) contractions – no hypertrophy, this encourages transformation in the direction from fast to slow fibre type E.g. Both will have the same number of quadricep muscle fibres but the endurance runner will have much smaller ones and are will have slower fibres Training Terminology: Two types of training are possible: 1. Transformation between fast and slow fibres. There is probably only a minor effect in humans, but easily produced in experimental animals – since you can train animals 24 hours in a several weeks in ways you can’t do in humans. 2. Hypertrophy and atrophy. Increases or decreases in size of muscle with no change in fibre numbers, simply their diameter. Examples • Inactivity e.g. Plaster cast (stops use of muscles) causes reduction in muscle bulk known as atrophy. There is also a small change from slow towards fast fibre type e.g. in spinal injuries (e.g. paraplegia where there is damage to lower spinal cord and legs muscles do not work at all – there is nothing wrong with the muscles, they are just resting for the rest of the lifetime) where muscles are permanently inactive. Fast phenotype (i.e. the fast fibre) is the default i.e. observed in the absence of muscle activity whereby regular training at the low level would produce slow fibre types • Hypertrophy is caused by about 10-20 maximal contractions of the (targeted) muscle group every day Causes slow increase in fibre size and strength (strength is proportional to cross-sectional area) Isometric contractions (i.e. slow shortening) or eccentric contractions (i.e. slow stretching) are all effective in hypertrophy • Long periods of repeated low force contractions (e.g. running), improves aerobic function i.e. increased cardiac output, improved blood flow to muscles, more muscle capillaries, more mitochondria etc. This is more like slow muscle phenotype. 1|U1L22: training, muscle damage and disease What are cellular and molecular mechanisms? These are areas of intense current research e.g. for drugs that can transform fast to slow fibres to produce strength in persons such as the elderly. (Below) Famous experiment by Eccles in 1960s (NZ/Australian Nobel Prize winner) - He took an animal that had fast muscles innervated by a nerve, and slow muscle innervated by a “slow nerve”. He disconnected the fast nerve from its nerve and shifted it over to the slow muscle and disconnected the slow nerve from its muscle and moved it over to the fast muscle. The fast muscles became gradually slower i.e. from fast fibres to slower fibres and vice versa. Shows that some signal from the nerve determines muscle properties In fast muscles (e.g. arm), nerves fire very infrequently but in rapid bursts action potentials to power the one movement made every so often. In slow muscles (e.g. postural muscles), nerves fire at a low rate but nearly continuously. Later shown that if a permanent stimulator at a low rate (5 Hz) is implanted on a fast nerve (which is firing infrequently), fast muscles gradually becomes slow i.e. it is the firing rate that gradually turns fast fibres into slow fibres. This explains why in paraplegia, where there are no action potentials firing to the leg muscles, the muscles gradually become fast. Slow muscles become slow because they have a regular firing of nerves. Training for a marathon involves this type of stimulation (repetitive low intensity over long periods) and so causes a limited fast-to-slow transformation of the muscle fibre type. Molecular mechanisms: Fast to slow transformation involves a chronic increase in [Ca2+]i inside the fibres (because every time there is an action potential, there is a release of calcium) which causes preferential transcription of the slow genes inside muscles. Hypertrophy is caused by a generalised increase in protein synthesis leading to production of more contractile proteins i.e. muscles fibres are getting larger so there is a need for more myofibrils, thin and thick filaments, more actin and myosin. The pathways that synthesise these proteins are turned on and the breakdown pathways are turned off, and there is an accumulation of these contractile proteins inside muscles making cells larger and muscles stronger. 2|U1L22: training, muscle damage and disease Muscle damage: If you walk up a mountain, your muscles become painful and weak but recover after a few minutes rest i.e. muscle fatigue. Conversely, if you walk down a mountain it is relatively painless but the next day your muscles are weaker and feel stiff, sore and swollen. This known as Delayed Onset Muscle Soreness (DOMS) and is a form of (mild) muscle damage. Recovers completely in a week. Why does this form of exercise (particularly walking down mountains) which utilises eccentric contractions – using muscles to break movement, why does that cause this form of muscle damage - DOMS? Characteristics of DOMS: The force is reduced immediately, it takes (3 to 4) days to recover (different from muscle fatigue whereby recovery is around 10minutes) Loss of muscle enzymes into the blood (membrane damage) i.e. because proteins that are normally soluble but inside the muscle are leaking out into the plasma and blood Mainly occurs in eccentric contractions (stretched movement) i.e. when muscles are stretched onto the descending limb of the tension length curve There is a characteristic EM appearance – where there are overstretched and understretched sarcomeres jumbled together In understanding stretch induced muscle damage e.g. DOMS, we will use the length-tension curve: (remember – due to the overlap of thick and thin filaments, there is an ascending region, a flat plateau at the top and a descending region and we work at the flat plateau at the top) - (right) Sarcomeres are unstable on the descending limb of the tension-length curve Imagine two sarcomeres on the descending limb (i.e. there isn’t a complete overlap of their thin and thick filaments) – muscles are at normal length and are being stretched during a contraction so we go down on the descending limb (since we stretch starting from the peak) If sacromere A gets slightly longer than B (and B gets shorter), A will become weaker while B will become stronger (because there are more cross-bridges in the overlap zone) Consequently A will get longer and exacerbates the length difference. For this reason sarcomeres are fundamentally unstable on the descending limb of the TL curve. i.e. If there is contraction, A will still get longer, and B will get still shorter. whereby when any sacromere gets slightly longer than its neighbour, it will be stronger and therefore shorten more and therefore stretch its neighbour more. 3|U1L22: training, muscle damage and disease Typical EM Appearances: Note regions of overstretched and understretched sarcomeres Note the orange bar is a normal sarcomere length; the blue bars are examples of one sarcomere and its neighbouring sarcomere. One is shorter than average and other is longer than average, i.e. because there is shortening on the descending limb where sarcomere are fundamentally unstable due to the negative slope of the LT relationship. These areas propagate through the muscle due to short and longer sarcomeres producing regions of disorganisation but till take a few days to recover. Regular pattern of stability and uniformity is lost due to these eccentric contractions. Regions of damaged sarcomeres cause membrane damage (e.g. membrane can get torn) resulting in the loss of intracellular proteins (leaking out to the blood) and cause inflammation which is why muscles become sore & tender. Skeletal muscles contain satellite cells (resident stem cells) which can divide, form new muscle cells which fuse to form a replacement multinucleate muscle fibre for damaged muscle cells i.e. muscles repair themselves. 4|U1L22: training, muscle damage and disease Muscle Diseases: Remember from previous: muscles are controlled from the brain, one neuron down to the spinal cord, another neuron whose cell body is in the spinal cord and sends its nerve out to wherever the muscle is. i.e. there are problems anywhere in the chain-of-command that can cause failure of muscle function: E.g. ischaemic damage in the motor cortex – strokes in the elderly damage to spinal cord causes paraplegia e.g. complete loss of function in legs, bladder, sexual organs, rectum i.e. because the spinal cord transects all the neurons coming down to your lower muscles motor neuron disease affecting the lower motor neuron e.g. Stephen Hawkings cutting a motor nerve paralyses the muscles supplied (i.e. all the downstream muscles are paralysed) btw, sewing the nerves together is possible (and yes, I just typed btw) diseases affecting the neuromuscular junction diseases affecting muscle can affect muscle function (will be the focus) Muscular dystrophy It is a devastating disease of muscle affecting 1 in 3500 boys (only males due to mutation on X chromosome since males have XY chromosomes and since there is a mutation on the X, there is no normal X to balance it – girls are carriers and can carry the disease onto their male offspring) Boys have normal muscles at birth They gradually get weaker and are wheel chair at around 10 years of age They die in early 20s of respiratory failure In late 1980’s, a mutation causing the disease was found in a previously unknown protein which was then called dystrophin. Boys with muscular dystrophy lack dystrophin (i.e. boys have a mutation in the gene that should produce the protein dystrophin). (right) Unnecessary image – don’t need to know showing where the protein is. Dystrophin is a cytoskeletal protein which connects the contractile proteins to a group of proteins in the cell membrane (we don’t need to know these proteins in the group however, mutation to these proteins will cause other muscle diseases). 5|U1L22: training, muscle damage and disease Why does its absence cause muscle degeneration? Hypothesis 1. Dystrophic muscle is more susceptible to stretch-induced muscle damage. Perhaps dystrophin somehow stabilises the membrane i.e. reduces the membrane damage associated with over and understretched sarcomeres. Above is a muscles representation which has Z-lines, thick filaments, thin filaments, thick filaments, other Zlines, and two sarcomeres. Note: in mammals, the T-tubules are at the overlap region, there are two T-tubules for every sarcomere. What happens when you get a stretched sarcomere like above? The T-tubule is going to have trouble, its attached to the membrane “here”, the sarcomere suddenly stretches and it’ll have to “zip” over “there” and have an S shaped bend in it and may get ripped when that happens. Here’s dystrophin connecting the Z-line or some actin filaments to “this” bundle of proteins in the membrane. Maybe that’s just designed to keep the localisation of the thick and thin filaments and the T-tubules together. So if dystrophin was absent, this disparity between the thin and thick filament and the T-tubules would be much worse and there’d be many more T-tubules disrupted and broken like above. That’s the kind of hypothesis people have to try and understand why the loss of one protein makes stretch induced muscle damage much worse in comparison to normal people. 2. Resulting tears in T-tubules/Surface Membrane allow Ca2+ entry into the muscle and activates Ca2+ activated proteases (i.e. the proteases are activated by excess Ca2+). The general idea is that they get too much calcium in the muscles because they have tears in the membrane. There’s a huge gradients from calcium going from outside the cell into the cell, and if there is too much calcium inside the cells, there is activation of the proteases and they start chewing up the enzyme in the muscle. It also allows soluble enzymes to leak out of the muscle fibres. 3. Repair of damage by satellite cells is adequate initially but later fails. Treatment Since only one gene is abnormal and one protein missing (i.e. only mutation, only one protein affected), gene therapy may eventually provide a treatment. Possible approach Isolate the DNA of the normal gene - (we have the dystrophin DNA ready and available) Insert DNA into a virus - (viruses have DNA inside them) Infect patient with virus (viruses insert their own DNA into cells and use the cells genetic apparatus to produce (their) viral proteins) – (tricked the virus by putting DNA of dystrophin into the virus and the idea is that the virus will get into the muscle cells and dystrophin will start to synthesise. – It works on mice however why doesn’t it work on humans? There are three main reasons – (see next section i.e. Problems) Problems 1. Huge mass of muscle to infect. (humans have 40kg of muscle in the human body i.e. every muscle cell will have to have the virus, will have to synthesise dystrophin at multiple points along it – therefore there is a distribution problem even if the genes worked) 6|U1L22: training, muscle damage and disease 2. Dystrophin gene is too large to go into a virus (dystrophin is the largest gene in the human genome and it’s too big to go into any virus. Scientists have cut off unnecessary parts of the dystrophin molecule and have successfully inserted into mice.) 3. When the virus put its DNA into the cell and starts synthesising dystrophin, the dystrophin is a foreign protein as far as the cell is concerned i.e. when produce is a ‘foreign’ protein and protein and attacked by the patient’s immune system. The combination of these problems, gene therapy, although it has been tried, it has not been successful thus far. Summary: Athletes have long discovered by empirical methods the best way to train for particular activities. We are now beginning to understand the cellular and molecular mechanisms involved. Stretch-induced muscle damage occurs during normal activities and may be part of the pathway leading to effective hypertrophy. Skeletal muscle can repair damage (whereas cardiac muscle cannot). Muscle diseases such as the dystrophy may involve the same damage pathway as stretch induced muscle damage but damage may be worse or repair less effective. Muscular dystrophy is an example of a disease which has led to the discovery of a new protein (dystrophin) which has an unrecognised role in muscle. 7|U1L22: training, muscle damage and disease