the PowerPoint Presentation
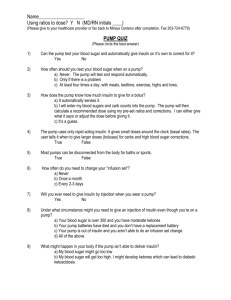
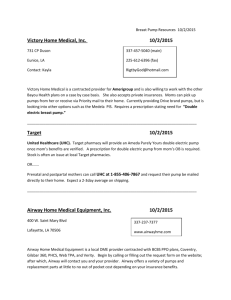
advertisement

Pumping How Do I Start? John Walsh, P.A. Author: Pumping Insulin, Using Insulin (619) 497-0900 www.diabetesnet.com What We’ll Cover Introduction to pumps Advantages of pumping Am I a candidate? How to choose a pump and infusion set What is needed to start Importance of data Site preparation Troubleshooting Formulas that help Smart features Where Pumps Began Started ~1978 with conversion of portable chemotherapy pumps to delivery of insulin The Autosyringe AS2C and Harvard Apparatus Mill Hill Infuser were first Single basal, no memory 50 ml syringe on pump exterior Required dilution of insulin to U-36 or U-18 1976 Biostator (top) and 1978 Autosyringe AS2C –> The Basal-Bolus Concept Advantages Flexibility in meal timing & size Eat when you want to Faster adjustment of insulin for exercise Family activities are no longer tied to one person’s needs Easier handling of illness, travel, or camping Advantages More Consistent Insulin Action The same dose of NPH insulin given to the same individual varies by 25% from day to day Order of variablility: NPH > Lente > Lantus > Detemir A pump has less variable insulin delivery at 3% Advantages Precise doses, as small as 0.025 u, can be given Manages the Dawn Phenomenon Improves control during growth spurts and adolescence Reminders Who Is A Good Pump Candidate? Why Choose A Pump? A freer lifestyle Easier dose determinations Improved blood sugars Flexibility in meal timing and size Ability to exercise without losing control Peace of mind When To Consider A Pump More than 3 injections per day Tired of multiple injections Frequent or severe hypoglycemia Hypoglycemia unawareness Elevated A1c DKA or ER/hospital admission Strong Dawn Phenomenon Require small, precise doses Less risk of complications Insulin Pump Pro Less work Simplified insulin dosing Precise delivery Greater impact in those with highest starting A1c Slightly less insulin use per day Con More DKA More severe hypoglycemia A1c levels and frequency of DKA & hypoglycemia are similar to ICT What It Takes To Succeed A personal desire for better control Willing to adjust insulin doses to carb count, test results, and activity Willing to monitor at least 4 times a day Willing to keep an accurate record of BGs, boluses, and carb counts Committed to solve problems and adapt lifestyle as needed Success For Kids On Pumps Supervision is required: kids BEGIN to develop self care skills at about age 10 Family support is essential: an adult who can go to school, etc. Communication with a health care team that is committed to pumps Adequate insurance and financial resources Assistance and support from teachers, friends, babysitters, grandparents, siblings Features For Infants & Toddlers Little ones are ideal pump candidates if the parents are Delay or split boluses for fussy eaters Small, user-friendly pumps offer precise dosing (0.05, 0.025, or 0.01 unit increments) Lock out Worn between shoulder blades If a toddler likes to remove the infusion set, let them know what comes out must go right back in Help For Kids & Teens Growth spurts Dawn Phenomenon Easy coverage of snacks TDD and bolus history can be checked to ensure consistent dosing Faster adjustment of basals and boluses for changes in activity, etc Special Teen Concerns Dating Wearing, sharing Alcohol Eating disorders Fast foods Fabrication Sleeping-in Personal Effort Those who expect a pump to manage their diabetes for them will fail to optimize their own therapy. Learn how to adjust your basals and boluses for an excellent A1c! First Steps Toward A Pump Keep detailed records Consider your (and your child’s) motivation Peer group, acceptance issues, family support Look at available pumps Which pump(s) does your insurance cover? Talk with your doctor about a prescription Visit a dietician to learn carb counting What To Learn How your pump works How to count carbs How to interpret BG results and see BG patterns When to increase and decrease basals and boluses How to adjust for high GI foods, extra activity How To Choose A Pump Pump Companies Who sell or plan to sell pumps in the US: Animas R1200 Dana Diabecare III Deltec Cozmo Medtronic Paradigm Nipro Amigo Roche/Disetronic Visit www.diabetesnet.com/diabetes_technology/ Things To Consider Look, feel, color Features: reminders, child block, waterproofing Size of basal and bolus increments Infusion set choices Safety and reliability Customer support History Ease of data analysis Add-ons: meters, covers, cases Today’s Smart Pumps Easy dose calculations with Carb Factor and Correction Factor Precise insulin dosing (0.05 units or better) to allow basal rates to be set up for Dawn Phenomenon, etc. Tracks BOB to avoid insulin stacking Reminders Today’s Pumps When control is poor or varies greatly on one of today’s pumps, the pump settings are incorrect. Test and reset basal rates, carb and correction factors until you have good control. Garbage in….. How To Choose An Infusion Set Infusion Sets Straight-In Teflon: Cleo, Inset, Ultraflex, Quik-Set Angled Teflon (Comfort, Tender, Easy, Silhouette): Easier to insert, variety of depths (6, 8, 9 mm) Fewer failures Insertion site is visible Longer is more secure Adjust angle to reach fat Metal needles (Rapid-D or bent needle) As comfortable and often more reliable Very short, multi-needle infusion sets expected soon Infusion Sets And Inserters Disetronic Rapid-D Smith’s Medical Cleo Medtronic Sil-serter Animas Inset Quik-serter Site Supplies Emla cream (Rx, 30 min wait) or ice cube Set inserter: Cleo and Inset are self-contained, ezSerter, Quick-Serter, Sil-Serter, Sof-Serter Adhesive: IV-3000, Hypafix, Tegaderm Stickies: Skin Tac-H, Skin Prep Tape: Micropore, Durapore, Band-Aid Blister Relief (wicking) Sweating aid: Mastisol Spray (Detachol for removal), Skin Tac, Tincture of Benzoin, Skin Prep Adhesive removal: Uni-Solve, Allkare School Supplies Meter, lancets, test strips Glucagon, glucose tablets, or crackers for lows Spare insulin, syringes or insulin pen Spare infusion set and pump batteries Ketostix or Precision Xtra to test for ketones Information card with insulin-to-carb ratio, formula for corrections Telephone numbers of parents, health care providers, and pump manufacturer's help line How To Start Starting On A Pump Everyone is nervous Read, read, read • Pumping Insulin, Kids Insulin Pumps And You (Animas), www.childrenwithdiabetes.com, www.pumps4kids.ca, etc, etc Do lots of recording before and after start Start to play with pump as soon as it arrives Saline practice helps Get telephone contacts: MD, CDE, pump company, pump rep, other parents Helpful Attitudes And Habits Be blatant about your diabetes A pump is a tool, not a cure Take a bolus for every bite Change site as directed Look for a solution for every problem Write down a reason for every low and high Test often John’s Pump Rules • Total Daily Dose = weight in lbs / 4 • Basal Dose = 50% to 60% of TDD • Carb Factor = 500 / TDD • Correction Factor = 2000 / TDD • BG target = 90 to 120 mg/dl • Basal target = +/- 30 mg/dl • BOB = 20% per hour • Correction boluses = < 8% of TDD J Walsh and R Roberts: Pumping Insulin, 2005 Starting Insulin Doses J Walsh and R Roberts: Pumping Insulin, 2005 Carb Counting And Recording As Ways To Lower The A1c Steps For A Better A1c Carb counting – 0.6% Givivg boluses based on an accurate carb count – 0.3% Recording test results, carb intake, insulin doses, & activity – 0.5% Monitoring often – 0.5-2.0% Bolusing often – 0.5-2.0% Contacting your doctor or adjusting your own doses when you encounter unwanted BGs Carb Counting Allows precise matching of carbs with boluses Glycemic index, saturated fat, and high protein all play a role, but grams of carb is what controls the blood sugar after a meal Easy! Where Carbs Come From fruit/fruit juice breads/bagels cereals crackers 1 gram of carb grains raises the BG muffins 4 to 7 points! rice potatoes/yams vegetables dessert/cookies/cake/pie ice cream/frozen dessert sweetened beverages milk/yogurt (not cheese) beer/wine honey/syrup/molasses jams/jellys/preserves -ose foods like sucrose (table sugar) How To Count Carbs Food labels Check portion size Books Dr’s Pocket Guide, Health Cheques A gram scale plus carb factors Carb factors are available in Pumping Insulin and are built into scales like the Salter computer gram scale Blood Sugar Testing – 1921 Blood Sugar Testing – 2004 Blood Sugar Testing – 2004 “I just don't write down (log) anything. I hate to take the time to do it. I'd rather have a machine talk for me. I think it revolves around partial general laziness, as well as the constant reminder of being different from everyone else. I know other diabetics who won't even test when they're out with friends. They hate ….” The Artiste 6/28/04 Charting Improves Control Smart Charts Needed to solve problems Basis for better diabetes health care ~0.5% drop in A1c Blood sugar, insulin, food, activity, stress Better Charts, Better A1c Charts Software My Other CheckBook Meter companies Internet: myhealthchannel.com Pump Control Software Meters, PDAs & Pumps Pump: Deltec, Disetronic, Animas, Medtronic Meter: BD, Therasense, Lifescan, Boerhinger Analyze Carb Boluses 1. Count carbs 2. Give carb bolus 3. Eat 4. Record BGs 5. Analyze BGs 6. Balance better next time Match Your Carbs With Boluses for HALF the day’s control! Keeps blood sugar normal after meals Requires accurate carb counting and an accurate carb factor 500 Rule provides a close estimate of carb factor if the TDD is accurate Accounts 500 Rule To Find Carb Factor Gives grams of carb covered by one unit of Humalog or Novolog 500 / TDD = grams of carb per unit of insulin Example: Person’s TDD = 50 units 500/50 = 10 grams of carb covered by 1 unit of Humalog or Novolog Postmeal readings stay normal! 2000 Rule To Find Correction Factor Gives how far your blood glucose is likely to fall per unit of insulin over 5 hours 2000 / TDD = # mg/dl your BG will fall per unit Example: Person’s TDD = 25 units 2000/25 = an 80 mg/dl drop per unit of H or Nov Adapted from 1500 Rule by Dr. Paul Davidson, Atlanta, GA 2000 Rule Total Daily Dose 20 units 25 units 30 units 35 units 40 units 50 units 60 units 75 units Point drop per unit 90 pts 72 pts 1600, 1800, 2000, 60 pts or 2200 may be divided by TDD to 51 pts get point drop per 45 pts unit 36 pts 30 pts 24 pts 1800 provides a good average --- 1600 Rule is more aggressive and gives more insulin, while a 2000 or 2200 Rule gives less insulin New Devices Data storage and download Easy recording of BGs, insulin, carbs, activity Automatic carb counting Pattern recognition Insulin dose guidance Data analysis to improve control Feedback that encourages use Pump — Meter Combos CozMonitor from Deltec and Therasense Disetronic and Roche Medtronic 512 and BD Paradigm Link Animas and Lifescan Dana Diabecare III and Dana meter Troubleshooting Most Pump Problems Occur In First First week month First 6 months Problems are most likely when unexpected or inconvenient Occasional Pump Problems Setup tips Leaks Allergies Bleeding O-rings Hub Line Clogs Site infections and abscesses onto skin inside needle under skin Pump bumps Hypertrophy DKA Some frustration at times is normal! Set And Site Issues Dislodged infusion set Tunnelling Rapid-D and slanted Teflon sets work better for mobile kids Metal may be better than teflon Infection Hematoma Site Preparation Prevents pump bumps, infection, and abscess Steps Wash the hands Sterilize the skin – IV Prep Use bio-occlusive adhesive – IV 3000 Insert the set Use safety tape Will Your Pump Alarm? Low battery Mechanical problem Empty reservoir Clog Forgotten bolus Leak Bleeding Bad programming Dislodged infusion set Yes Yes Yes Yes Yes No No No No How To Check Mechanical Problems Check from skin to pump: Skin and site Infusion set Connection Line Hub Reservoir Pump High BG Checklist See a leak or smell insulin? Infusion set in place? Was infusion set primed? Are connections at hub and O-rings tight? Bubbles in the tubing? One inch = a half unit Clog in line? Alarms? Errors? If no cause is found, replace everything! Check Ketones Early Test for all BGs over 300 Always test when nauseous Test urine with Ketodiastix Test blood with Precision Xtra meter Earlier detection No need to collect urine Keep currently dated strips available Go to ER at 1st sign of vomiting! More Insulin For Unexplained High BGs When a blood glucose test is unexpectedly high, the correction bolus needed to lower this will be much higher than normally required Loss of basal insulin delivery for several hours Insulin resistance from length of hyperglycemia Insulin resistance from presence of ketones Conclusion A pump offers the latest technology for precise insulin delivery Requires commitment and responsibility Benefits include more flexibility, less hypoglycemia, improved control, and a longer, healthier lifespan Make the commitment and start pumping! Questions ???