The Integumentary System
advertisement

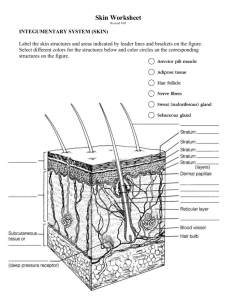
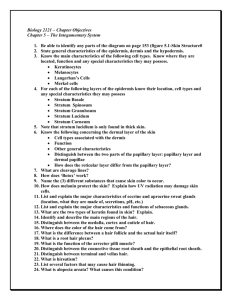
The Integumentary System Skin, Hair, Nails, and Glands Do Now: Calculate the weight of your skin: For average adult skin accounts for 7% of body weight! Thickness ranges from 1.5mm – 4.0mm Where on the body is it thickest? Thinnest? Integumentary Structure 2 Components: Cutaneous Membrane Epidermis Dermis Hypodermis aka subcutaneous layer Superficial fascia Accessory Structures Hair Nails Exocrine Glands Integumentary Function Protection Temperature maintenance Synthesis and storage of nutrients Sensory reception Excretion and secretion Epidermis Avascular & Keratinized Thick skin – 5 layers Thin skin – 4 layers New epidermis every 25-45 days Cells: Keratinocytes (most cells) – produce keratin Melanocytes – (spider shaped) produce melanin Tightly connected by desmosomes Callus – accelerated keratin formation Melanin taken in by keratinocytes Shields nucleus from UV Merkel cells – sense skin curvature Langerhans’ cells – star shaped phagocytes Layers of Epidermis Layers (starting from basement membrane): Stratum Germinativum (Basale) 3 Intermediate layers Stratum Spinosum Stratum Granulosum Stratum Lucidum** Stratum Corneum (superficial) Stratum Germinativum (aka stratum basal) Newly synthesized keratinocytes attached to basement by hemi-desmosomes Forms ridge contours at interface of epidermal ridges and papillae of underlying dermis Ridge contours are developmentally determined and visible in palmer, plantar, and digits 1 layer of Stem cells or germinative cells dominate the stratum germintivum Undergoing mitosis 10-25% melanocytes, some merkel cells Receives nourishment from dermis Fingerprint Activity Psoriasis •Very common between 15-35 •Autoimmune disease • increased rate of mitosis despite same rate of shedding •Non-contagious •Treated w/topically or phototherapy Intermediate Strata Stratum Spinosum spiny or prickly layer Newly synthesized keratinocytes (several layers) Cells continue to divide Langerhans cells abundant Stratum Granulosum 3-5 flattened grainy cell layers Stopped dividing, nuclei 7 organelles break down Produce keratin (durable, water resistant protein) Produce glycolipids –reduces water loss Stratum Lucidum Thin layer clear layer Found in thick skin Densely packed cells filled with keratin Stratum Corneum Most Superficial layer ¾ of epidermis 20-30 layers of flat dead keratinized or cornified cells Held tightly together by desmosomes Relatively dry (prevents microorganism growth) Lasts about 2 weeks before shed Avg person sheds 40lbs of skin in a lifetime! Pigmentation: Skin Color Melanin (yellow, brown or black pigment) Freckles & moles are areas of heavy melanin production Carotene (orange-yellow pigment) Converted to vitamin A for epithelial maintenance Accumulates in stratum corneum Dermal Circulation Oxygenated Hemoglobin - reddish tint Constricted blood vessels – pale Cyanosis – Sustained constriction bluish color in Caucasian, only visible in nail beds of dark skin Produced by melanocytes in epidermis Production increases in response to sun exposure Prevents skin damage by absorbing UV rays All humans have same number of melanocytes What causes the appearance of wrinkled, leathery skin? Sun Exposure UV stimulates production of vitamin D3 D3 is modified by liver and converted to calcitrol by kidneys Calcitrol essential for absorption of calcium and phosphorus Too much UV clumps elastin fibers causing leathery appearance UV destroys folate needed for DNA synthesis Too much UV can also cause chromosomal damage in stem cells of stratum germinativum causing skin cancer Skin Cancer Most common form of cancer (and most preventable) Basal Cell Carcinoma – originates in stratum germanitivum Squamous Cell Carcinomas – superficial layers Malignant Melanomas Extremely dangerous Begins as a mole Melanocytes grow rapidly and metastasize through lymphatic system Know the ABCD rule! Do Now: What are Stretch Marks? Damage to the dermis (collagen & elastin fibers) due to rapid stretching of the skin due to rapid growth or weight gain Appear reddish- purple at first then fade to a lighter color over time Tend to occur in regions of the body where fat is stored Hormonal changes, genetics, and diet can all affect development of stretch marks Dermis “hide” Dermis – contains network of blood vessels, lymph vessels, and nerve fibers Papillary Layer (thin superficial) Loose connective tissue Dermal Papillae indent epidermis Supports and nourishes epidermis Capillaries and nerves Meissners corpsucles – touch receptors Reticular Layer (80% of dermis) fibroblasts., macrphages, mast cells Meshwork of dense irregular connective tissue Elastic fibers provide stretch & recoil Collagen fibers provide rigidity & strength BV, sweat and oil glands Phagocytes Striae – stretch marks Blisters Cutis hyperelastica Mechanoreceptors of Skin Merkel’s disk Meissner Corpuscle Pain Chemicals Ruffini’s ending Light Touch Free Nerve Endings Skin Curvature Heat Stretch Pacinian Corpuscle Deep Pressure Vibrations Sensory Homunculus What causes a decubitus ulcer or bed sore? Caused by an interruption of blood supply to a tissue causing necrosis. These develop in patients that have been bed ridden for long periods of time. They are caused by the weight of the body on the skin overlying a bony area compressing the blood supply. Do Now: List & describe layers of the Integument Epidermis Dermis Stratum corneum Stratum lucidum Stratum granulosum Stratum spinosum Stratum germanitivum (Basale) Papillary Layer Reticular Layer Hypodermis Subcutaneous Layer Not actually part of integument, blurred boundary Anchors skin to muscles, but loosely so it can slide Loose connective tissue with many adipocytes Fat distribution changes as grow and mature (shock absorption & insulation) Females thighs & breasts Males abdomen “beer belly” Contains no vital organs and few capillaries Subcutaneous injection useful method of administering drugs with hypodermic needle Accessory Structures: Hair and Hair Follicles 2.5 million hairs on human body!! Hair Growth Cycle Hair grows for 2-5 years about .3mm per day then pushed to surface to be shed for new cycle to begin (scalp 6-10 yr cycle, eyebrows 3-4 months) Function Protect scalp from UV, cushion head, and insulate skull Prevent entry of foreign particles in nostrils, ears, and eyes Respond to stress or cold (arrector pili smooth muscle in dermis forces hair to stand up) Structure Walls of follicle contain cells of epidermis Hair Papilla – peg of connective tissue containing capillaries and nerves, cell division occurs Hair Root – anchors hair in to skin Hair Shaft – 3 layers of dead keratinized cells Medulla – core of hair (soft keratin) Absent in fine hair Cortex – surrounds medulla (hard keratin) Cuticle – surface single layer made of overlapping shingles of cells Hair Texture Oval – silky & wavy Flat & ribbonlike – curly Round – straight Conditioners – smooth out rough cuticles making it shiny Split ends – cuticle wears away at ends Hair Types: Cuticle Coronal Crown like (stacked paper cups) Small rodents & bats Spinous Petal or triangular shaped Mink, cats and seals Imbricate Flattened, overlapping scales Humans and other animals Medulla Fragmentary (trace) Discontinuous (broken) Continuous Cortex Human pigment granules distributed by cuticle (except red-hair) Cattle, dogs and some humans have ovoid bodies Human Hairs vs. Animals Consistent color & pigmentation throughout shaft (see banding in animals) Animal pigmentation is centrally located Humans 2 types of hair: Vellus hair – fine body hair Terminal hair – coarser, darker hair (increased testosterone increases growth) Hair Color Genetically determined by type and amount of pigment produced by melanocytes Brown – true melanin Blond - sulfur Red - iron Gray - Pigment production decreases White air bubbles within hair shaft Do Now: What is alopecia? Hairs not replaced as fast as they are shed, begins anteriorly and progresses posteriorly Male pattern baldness – sex linked trait by delayed action gene that when turned on changes response to testosterone Until recently, only cure inhibits testosterone production What are comedones? Acne is caused by blocked sebaceous duct, forming a sebum plug Affects over 85% of adolescents and young adults. Secretions accumulate causing inflammation and possible bacteria infection Blackheads – open comedones, melanin oxidizes turning black Whiteheads – closed comedones Hormonal changes can cause increased oil production Try not to squeeze, scratch, pick, or rub the pimples. Although it might be tempting to do this, it can lead to skin infections and scarring. Accessory Organs: Nails Protect exposed finger tips and limit distortion when exposed to mechanical stress Tools – pick up or scratch itch Free Edge Nail body – dead keratinized cells Nail bed – epidermis covered by nail body Nail root – anchors nail body Nail matrix – nail growth occurs Cuticle – portion of stratum corneum extending over nail Lunula – pale crescent (area of obscured blood vessels) Accessory Structures: Sebaceous Glands Holocrine oil glands Arrector pili muscle contracts squeezes the sebaceous gland forcing oily secretion out Sebum (oily secretion) lubricates hair and skin and inhibits bacteria growth, slows water loss from skin Glands are sensitive to androgens (sex hormones) Cradle Cap – overactive sebaceous glands Accessory Structures: Sudoriferous (sweat) Glands About 3 million per person! Merocrine (eccrine) Sweat Glands Secreted directly onto surface of skin via exocytosis 99% water w/electrolytes, vitamin C, antibodies, metabolic wastes and drugs, pH of 4-6 Cools surface of skin and lowers body temp Too much perspiration may lead to dehydration Flushes microorganisms from surface Apocrine Sweat Glands sweat glands that secrete products into hair follicles in armpits, nipples, and groin Sticky, cloudy secretion released at puberty Odorous as bacteria break it down as food Slides of Scalp vs. Palm Injury and Repair of Skin Inflammatory response – triggered by mast cells increase blood flow to area Scab (fibrin proteins) forms at surface to restrict entry of microorganisms Cells divide rapidly to replace missing cells Macrophages and phagocytes clear debris and patrol area for pathogens Animation: http://www.youtube.com/watch?v=QHzHc9E8kTw&feature=related Deeper wounds Scar tissue – lots of collagen fibers and few blood vessels Fetuses don’t scar Keloid – thickened area of scar tissue with shiny smooth surface (tend to form in adults with dark skin) Damaged hair follicles, sebaceous and sweat glands, muscle cells and nerves are rarely repaired Burns 1st degree – kills superficial epidermal cells, injures papillary dermis 2nd degree – kills epidermis and possible some dermis, injures reticular dermis 3rd degree – kills all epidermal and dermal cells, injures hypodermis and deeper tissues Skin Gun: http://www.youtube.com/watch?v=eXO_ApjKPaI Aging Epidermis thins as stem cell activity decreases increasing skin injuries and infections Number of macrophages and other immune system cells decreases Decline in vitamin D3 production reduces calcium and phosphorus absorption weakening muscles and bones Melanocyte activity decreases causing increases sensitivity to sun Gland activity decreases causing dry scaly skin Follicles decrease function creating thin light hair Elastic fibers decrease resulting in wrinkling Reduced blood supply to dermis – less thermoregulation Repairs are slow…6-8 weeks Write an analogy for our skin…. Human skin is like __________ because _______________. Skeletal System Complete web showing how Integumentary system interconnected w/other organ systems! Reproductive System Muscular System Nervous System Urinary System Integumentary System Digestive System Endocrine System Respiratory System Cardiovascular System Lymphatic System