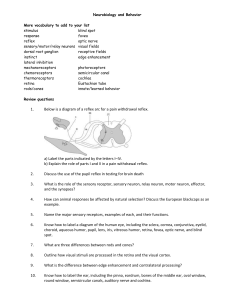
CN Testing
advertisement

CN I Name Olfactory Function Smell Screening Process Ask pt to breath in through nose as PT occludes one nostril at a time. Ask pt to close eyes. Occlude 1 nostril, & introduce a familiar & friendly scent. Ask pt to smell & report what the smell is. Ask pt to compare strength of smell in each nostril. Causes of damage -Head trauma (tearing of olfactory afferents as pass through cribiform plate, or of olfactory tract itself) -Compression of olfactory bulb &/or tract (meningioma of frontal lobe) -Degenerative diseases (Parkinson’s, Alzheimers) -Toxic inhalation -Common cold (temporarily loss) Consequences of damage Anosmia (inability to smell) II Optic Vision Visual acuity: Use Snellen chart 20’ or handheld chart 1’ away. Ask pt to cover 1 eye & read lowest line possible. Repeat for other eye. Test w/ glasses/contacts if normally used 4 fxn. -Optic neuritis (inflammation of the optic nerve, often due to MS) -Central scotoma: visual loss in the center of the field, decreased visual acuity, impaired color vision -Papilledema (optic disc swelling due to elevated intracranial pressure) -Enlargement of the blind spot -Prechiasmal lesions (i.e. to the optic nerve) -Scotomas -Monocular field defect: -lesion to the optic nerve (distal to the chiasm) -Hemianopsia: loss of ½ of the visual field -lesion to the optic tract (proximal to the chiasm) -if lesion to R tract, lose entire L visual field (R retinal field loss) -Damage at the chiasm (often due to pressure from a tumor of the pituitary gland) -visual field defects in BOTH eyes -medial chiasm damage: bitemporal hemianopsia -lateral chiasm damage: nasal hemianopsia Visual fields: Face pt 1’ away, at eye level. Instruct pt to cover 1 eye. PT covers mirrored eye. Instruct pt to look you in the eye & say “now” when they see your finger appear from out of sight. Extend your arm & 1st 2 fingers out of sight at a diagonal, then slowly bring centrally, noticing when fingers enter your field of vision. Pt should say “now” at same time you see your fingers. Repeat for all 4 quadrants. PLR: Parasympathetic: CN II: afferent CN III: efferent III, Oculomotor Pupillary light reflex: Check penlight in your hand for loose parts. Ask pt to put hand up along axis of nose. Slowly bring penlight in towards pt’s eye. Repeat for other eye. Should see bilateral pupil constriction. Ipsilateral response is “direct response”. Contralateral response is “consensual response”. -Motor to: SR, LPS, MR, IR, IO -Parasympathetic efferent limb of PLR Smooth pursuit: Instruct pt to follow fingers w/ their eyes w/o moving head. Move fingers slowly at eye level horizontally, vertically, in an “H” pattern Saccades: Hold fingers 4-6” apart and 18” from pt’s face. Instruct pt to look back & forth between the 2 as quickly as possible. IV, Trochlear -Motor to SO (up & R/L) VI Abducens -Motor to LR (R/L) -Diabetes Palsy (paralysis) Meningeal inflammation Aneurysm to upper basilar artery Sinus infection / thrombosis Aniscoria (pupillary inequality): If R optic nerve damage, neither direct nor consensual pupillary response is seen with light shone in R eye. Light shone in L eye, direct & consensual responses both seen. Opthalmoplegia: paralysis of 1 or more extraocular muscles Strabismus: inability to direct both eyes to same object so that the visual axes of the 2 eyes are misaligned -Results in diplopia Diplopia is the single symptom of opthalmoplegia. Double vision due to image of 1 eye falling on a different spot on the retina than Do horizontally, vertically, & diagonally. -All 3 together = “conjugate movement” V Trigeminal V3 Facial sensation; sensation from cornea (V1- corneal reflex- CN VII is efferent limb) Motor to muscles of mastication, mylohyoid, digastric, tensor veli palatine, tensor tympani (efferent limb of auditory/stapedius reflex) Convergence/Divergence: Instruct pt to hold thumb out & focus on it, then bring it close to face then back out. Ask pt to tell you when there are 2 images (convergence, 2”) & when it’s single again (divergence, 4-6”). About 2” from the nose there is usually double vision or eyestrain that should clear up as pt brings thumb back out. Look for eyes moving medially as thumb gets closer. Sharp and Dull: Test as would on body, with q-tip & pin). Instruct pt to close their eyes & tell you when they feel you touch their face. Randomly touch pt’s face above each temple, next to the nose, & on each side of the chin. Ask pt to compare strength of sensation & whether feels dull or sharp. Resisted jaw closure: Palpate masseter & temporal muscles while instruct patient to bite down hard while you apply downward pressure to chin trying to open mouth. III: aneurysm to PCA, tumor, extradural hematoma VI: rise in intracranial pressure the other eye CN III: Ptosis: eyelid droop due to weakness of levator palpebrae superioris. Lateral strabismus due to MR paralysis. No pupillary light reflex. CN IV: Extortion (outward rotation) due to paralysis of SO CN VI: Medial strabismus due to LR paralysis -Wallenberg’s Syndrome (occlusion of PICA in lower medulla) -Loss of pain/thermal sense in IL face & CL body -Tumor in middle fossa of cranium -Problems with jaw movement -Hyper-acoustic (sensitivity to loud sounds) -LMN damage: muscle atrophy, low tone, dysarthria -UMN damage: problems with chewing & speech; spastic dysarthria; tight and spastic speech -Corticobulbar lesion -Trigeminal neuralgia (no motor or sensory deficits, only pain) Bursts of pain to 1 of the 3 sensory areas Resisted jaw opening: Ask pt to open their mouth as you apply resistance to underneath of pt’s chin. Allow mouth to open slowly. Corneal reflex (wisp of cotton). Afferent = V1; efferent is VII. VII Facial -Motor to muscles of facial expression, stapedius, stylohyoid, digastric Ask pt to perform the following facial expressions: Raise eyebrows, shut eyelids tightly (PT tries to open), puff out cheeks, whistle, wrinkle nose, smile showing their teeth, frown, scowl -Taste from anterior 2/3 of tongue -Parasymp visceral motor to glands VIII Vestibuloco chlear -Paralysis of facial muscles -impaired corneal blink reflex -Hyperacusis (sounds v loud due to paralysis of stapedius) Herpes zoster virus -impairment of taste Compression due to blood vessel -Herpes: Facial palsy & rash in/around external auditory meatus Stroke -Hemifacial spasm: Continual twitching movements around mouth & eye due to compression caused by an aberrant blood vessel Paralysis of Stapedius muscle -Sensory from external ear -Efferent limb of corneal reflex Hearing Bell’s palsy (herpes simplex v.) Vestibular Stand behind pt & rub fingers together from 3-6” away from ear. Ask pt to tell you when they hear something & in which ear they hear it. Whisper 3 2-syllable words (snowflake, hot dog, ketchup) beside each ear & ask pt to repeat the words. Cochlear Weber test for lateralization: -Stroke -Partial or complete deafness -Dizziness, vertigo -Nystagmus Rap a tuning fork (256Hz or 512Hz) on your palm, the place the vibrating fork on vertex of cranium or mid-forehead & ask the pt if they hear the sound equally in both ears. (Will be louder on the side with conductive hearing loss) Rinne test for unilateral air to bone conduction: Rap the tuning fork on your palm and place the vibrating fork on mastoid process & ask if person hears the sound. Have pt say “now” when the sound disappears, then place tuning fork next to ear & ask pt if they still hear the sound. Have pt say “now” when they can no longer hear the sound. (pt should still hear it, unless they have conduction loss- could also be physical object obstruction of the ear canal) Equilibrium Afferent limb of Stapedius reflex Vestibular ocular reflex: Instruct pt to hold their thumb out at arms length and rotate head R and L while focusing on thumb. Ask the pt if they experience any dizziness, or if the object goes out of focus (is blurry) or if it moves (should be still). Gaze nystagmus: Have person fix gaze on an object. Balance: Romberg Test: Dynamic Visual Acuity: Have pt read lowest line possible on eye chart, while rotating head side to side. Should see a drop in no more than 1-2 lines, but no blurriness. IX, X Glossophar yngeal Vagus Motor to stylopharyngeus; Taste from post 1/3 of tongue; sensation from skin of external ear; sensation from carotid body & sinus; para motor to parotid gland Motor to pharynx & larynx; para to smooth muscle of digestive tract, cardiac muscle; sensation from ear; Taste from epiglottis & palate; visceral sensation Observe & palpate as the pt swallows, and note any stuttering or delay. -Tumors & infection affecting the meninges Note the quality and sound of the patient’s voice (hoarseness or nasally?) -Lesions due to: herpes zoster, carotid A aneurysm, alcoholic or diabetic neuropathy Analyze ability to cough Vagus: Ask pt to open mouth wide and say “ah”. Using your penlight, look for deviation of the uvula & drooping of soft palate towards unaffected side Glossopharyngeal neuralgia (similar to trigeminal neuralgia) -Dysarthria (difficulty speaking) -Hoarseness of speech -Nasal speech: paralysis of soft palate muscles -Dysphagia: Difficulty swallowing; nasal regurgitation -Deviation of uvula towards unaffected side; soft palate droops on the affected side (droops towards unaffected side) -Sensory loss to skin at back of ear Paralysis of B recurrent laryngeal nerves results in: -Aphonia: inability to give voice -Inspiratory stridor: harsh, high pitched sound on inspiration Afferent & Efferent (along with CN XI) limbs of swallowing reflex XI Spinal Accessory -Motor to trapezius, SCM, striated muscles of soft palate, pharynx & larynx Fxn is for “head turning” XII Hypoglossa l Instrinsic & extrinsic tongue muscles Observe patient for muscle wasting &/or droopy shoulder(s). Ask pt to shrug their shoulders as strong as possible while you press down on their shoulders. Ask pt to turn their head to side while you resist with your hands (CL SCM) If supine, can have lift head for bilateral SCM contraction. Lesions due to: -Surgical procedures of the neck -Trauma -Herpes zoster virus Trap reflex: only if person can’t follow commands. Place your thumb on muscle belly & tap nailbed. Whiplash Tongue protrusion: Instruct pt to stick out their tongue & move it side to side. -Pathologies to the basal meninges -Tongue deviates towards side of lesion -Neck operations -Tongue atrophy Speech articulation: Listen for dysarthria- have pt repeat “Late Night Down Town” -Ipsilateral SCM & trap weakness -Drooping of shoulder -Scapular winging when arms at sides Tumors near jugular foramen -Dysarthria