PowerPoint_Chapter19
advertisement

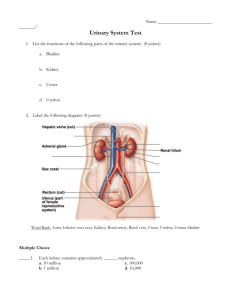
Chapter 19 The Renal System and Drug Therapy © Paradigm Publishing, Inc. 2 Chapter 19 Topics • • • • • • • Anatomy and Physiology of the Renal System Nephrotoxicity and Renal Dosing Urinary Tract Infections Spastic or Overactive Bladder Benign Prostatic Hyperplasia Kidney Failure Herbal and Alternative Therapies © Paradigm Publishing, Inc. 3 Anatomy and Physiology of the Renal System The Renal System • The renal system clears waste products from the blood and maintains proper fluid and electrolyte balance • Kidneys, the primary filter, have several main functions Clear blood flowing through them of metabolic byproducts and waste substances (toxic if not eliminated) Balance fluids and electrolytes, such as sodium, potassium, calcium Affect acidity (blood pH) and BP Produce erythropoietin, which stimulates RBC production © Paradigm Publishing, Inc. 4 Anatomy and Physiology of the Renal System The Renal System (continued) • The ureters transport the waste products and excess fluid to the urinary bladder • The bladder holds the substances until voiding (urination) • Urine exists the body through the urethra The Kidneys • The renal cortex (outer layer) produces hormones • The renal medulla (body of the kidney) is made up of many triangle-shaped sections, or nephrons, that perform filtration © Paradigm Publishing, Inc. 5 Anatomy and Physiology of the Renal System Anatomy of Renal System • The proximity of the kidneys to the abdominal aorta makes these organs sensitive to changes in BP. • High BP damages kidneys’ filtration; low BP can cause acute renal failure © Paradigm Publishing, Inc. 6 Anatomy and Physiology of the Renal System The Nephron and Urine Production • Each triangular section of the kidney contains thousands of microscopic-sized nephrons Nephrons are the functional filtering units • Three steps in urine production process: glomerular filtration, tubular reabsorption, and tubular secretion • Glomerular filtration Blood with fluid and waste products enters the nephron into the Bowman’s capsule, which holds the glomerulus Inside the glomerulus, high pressure forces fluid and small substances (filtrates) out of the blood © Paradigm Publishing, Inc. 7 Anatomy and Physiology of the Renal System The Nephron and Urine Production (continued) The filtered blood leaves glomerulus and continues on • Tubular Reabsorption and Secretion As filtrate passes through tubules and loop of Henle, molecules selectively reenter blood via 3 mechanisms Reabsorption: simple diffusion Active transport process: exchange between blood and urine via secretion Filtration: move across membranes from pressure Substances filtered out or secreted into the urine (but do not reenter the blood) are eliminated © Paradigm Publishing, Inc. 8 Anatomy and Physiology of the Renal System The Nephron and Urine Production • Each part of the nephron performs specific functions: filtration, reabsorption, and secretion of select electrolytes, fluids, and other substances © Paradigm Publishing, Inc. 9 Anatomy and Physiology of the Renal System Urine Production and Elimination • Urine production and maintenance of fluid balance rely on the tubular reabsorption and secretion processes • Hormones such as aldosterone and ADH regulate the rate and volume of urine production • The urinary bladder collects and holds urine until urination External urinary sphincter is a voluntary muscle that holds urine in the bladder before it exits the body • Urinary retention: when the urinary process does not function properly and urine accumulates in the bladder • Incontinence: inability to control external urinary sphincter © Paradigm Publishing, Inc. 10 Anatomy and Physiology of the Renal System The Bladder • Stretch receptors sense pressure when the bladder distends • They cause detrusor muscles in the bladder to contract and the external sphincter to relax • Urine is pushed out; bladder empties © Paradigm Publishing, Inc. 11 Nephrotoxicity and Renal Dosing Drug Accumulation in the Blood • Many drugs are eliminated through the kidneys • Some drugs can directly damage kidney tissue (nephrotoxicity), including NSAIDs, amphotericin B, aminoglycosides, and vancomycin Conditions are usually reversible but can cause kidney failure if not addressed quickly • Doses are kept low to avoid negative effects © Paradigm Publishing, Inc. 12 Nephrotoxicity and Renal Dosing Renal Dosing Calculations • Dosing calculations must take into account the reduced renal function in patients with kidney problems Doses for such patients must be adjusted because drugs require good renal function for elimination Adjustment depends on degree of renal dysfunction • Technicians may help in gathering kidney function laboratory tests © Paradigm Publishing, Inc. 13 Urinary Tract Infections UTIs and Drug Therapy • UTIs usually occur in the bladder • Cystitis: lower UTI involving the bladder; pyelonephritis: upper UTI affecting the kidneys • Prostatitis is a prostate infection in men; bladder infections in men are rare and difficult to treat • UTIs occur most often in sexually active women • Symptoms: pain or burning during urination, frequent urge to urinate, abdominal pain, fever, chills, cloudy urine • Treatment: antibiotics (penicillins, nitrofurantoin, sulfamethoxazole-trimethoprim, ciprofloxacin) © Paradigm Publishing, Inc. 14 Spastic or Overactive Bladder Spastic or Overactive Bladder and Drug Therapy • Malfunction of the detrusor muscles in the bladder; causes contraction and frequent urination • Drug Therapy: urinary antispasmodics; mostly oral • Mechanism of Action: inhibit ACh in the autonomic nerves that control involuntary bladder contraction and emptying • Side Effects (common): dry mouth, constipation, blurred vision, urine retention; (other): drowsiness, stomach upset • Side Effects (rare): allergic reactions • Cautions: phenazopyridine can turn urine orange and stain clothing; methenamine can turn urine blue © Paradigm Publishing, Inc. 15 Your Turn Question 1: What is the function of the bladder? Answer: The bladder collects and holds urine until urination. Question 2: A patient feels the urge to urinate often. She jokingly tells the physician that she knows where all the restrooms are when she runs errands or is out with family or friends. This is also causing problems for her at work. What drug therapy is the physician likely to prescribe? Answer: The physician will likely prescribe an urinary antispasmodic. © Paradigm Publishing, Inc. 16 Benign Prostatic Hyperplasia (BPH) About BPH • Chronic condition that occurs in men as prostate gland enlarges with age (common from ages 60 to 85) • Condition itself is not harmful, but the enlarged gland can impinge on the urethra and obstruct urine flow • Symptoms: weak or slow urine stream, delayed start of urination, straining to urinate Feel need to urinate often, but void only small amounts • PSA is a lab test to screen for BPH and other prostate problems, such as prostate cancer • Some drugs cause urine retention; do not use with BPH © Paradigm Publishing, Inc. 17 Benign Prostatic Hyperplasia (BPH) Agents to Avoid for Patients with BPH Avoid Instead Try… Anticholinergics H2 blockers, sucralfate, antacids Oral bronchodilators Inhaled bronchodilators Tricyclic antidepressants (TCAs) Calcium-channel blockers Selective serotonin reuptake inhibitors (SSRIs) Alpha blockers Disopyramide Quinidine © Paradigm Publishing, Inc. 18 Benign Prostatic Hyperplasia (BPH) Male Urinary System •Unvoided urine can promote infection •Men with BPH may have bladder infections frequently © Paradigm Publishing, Inc. 19 Benign Prostatic Hyperplasia (BPH) Prostate Cancer • Prostate tissue growth can become a malignant process • Prostate cancer is the second most common type of cancer in men (just behind skin cancer) Approximately 1 in 6 men will be diagnosed with prostate cancer • Prostate cancer is highly treatable, especially when caught early • Symptoms: difficulty starting or stopping urination, frequent urination, painful urination, blood in the urine © Paradigm Publishing, Inc. 20 Benign Prostatic Hyperplasia (BPH) Drugs for BPH: Alpha Blockers • Indication: BPH, especially if accompanied by high BP • Indication (other): passage of kidney stones • Mechanism of Action: inhibit alpha-1 receptors that relax smooth muscle in the prostate and bladder • Side Effects (common): dizziness, drowsiness, fatigue, headache, fainting, orthostatic hypotension • Side Effects (rare, severe): priapism • Cautions: interact with several prescription medications; should be used with caution in patients with GI disorders, liver disease, kidney impairment © Paradigm Publishing, Inc. 21 Benign Prostatic Hyperplasia (BPH) Drugs for BPH: 5-Alpha Reductase Inhibitors • Indications: BPH; male-pattern hair loss • Mechanism of Action: inhibit conversion of testosterone into DHT Restricting this active form of testosterone reduces the size of the prostate • Side Effects (common): decreased libido, erectile dysfunction, ejaculation disorders, breast enlargement • Cautions: could be harmful to a developing fetus in utero Women of childbearing age must not handle these agents with bare skin © Paradigm Publishing, Inc. 22 Kidney Failure Acute and Chronic Kidney Failure • Acute renal failure is due to physical or chemical damage or to lack of blood supply to the kidneys Temporary or short-lived; can return to normal status Life threatening if severe; possible permanent damage • CKD is progressive damage or results in the death of kidney tissue over time Irreversible condition © Paradigm Publishing, Inc. 23 Kidney Failure Renal Function Tests • BUN and SCr are lab blood tests used to diagnose and monitor renal function • When renal function is impaired, the elimination of urea, nitrogen, and creatinine is also impaired; elements accumulate in blood Normal range for SCr is 0.5–1.5 mg/dL SCr is used to calculate CrCl which estimates GFR • CrCl and GFR estimate the level of kidney function while taking into account such factors as age and gender © Paradigm Publishing, Inc. 24 Kidney Failure Renal Function Tests (continued) • Most common formula to calculate CrCl is the Cockcroft and Gault equation CrCl (mL/min) = [(140 – age) × IBW] SCr x 72 For females, multiply the result of right side by 0.85 Where IBW is ideal body weight in kg and SCr is in mg/dL • Example: if CrCl drops below 30 or 60 mL/min, the dose is decreased or the interval between doses is increased • Technician: retrieve lab results and perform calculations © Paradigm Publishing, Inc. 25 Kidney Failure Stages of CKD • CKD is more common than acute renal failure; common cases for CKD include diabetes and untreated hypertension • As it worsens, CKD is categorized into four stages that guide treatment (see Table 19.5) • Diuretics and other renal-protective medications can help slow the progression of the disease in early stages • Eventually, dialysis and kidney transplant are the only means of treatment (Stage IV) © Paradigm Publishing, Inc. 26 Kidney Failure Dialysis • Artificial method of filtering blood and correcting the electrolyte imbalances caused by renal failure • Two common methods are hemodialysis and peritoneal dialysis Hemodialysis: a machine mechanically filters the blood and returns it to the body; occurs every 2 to 4 days Peritoneal dialysis: dialysate is put into the abdominal cavity and left for a few days, then drained The dialysate fluid is changed at home Risk of infection and other complications is greater © Paradigm Publishing, Inc. 27 Kidney Failure Hemodialysis Peritoneal Dialysis © Paradigm Publishing, Inc. 28 Kidney Failure Drugs for Renal Failure • Acute renal failure improves or reverses; drug treatment is limited and short term • CKD is more frequently treated with medication Diuretics are used to improve urine output In advanced stages of CKD Dialysis and various drugs are needed Imbalances of various micronutrients and vitamin D become problematic Anemia occurs, requiring hemopoietic therapy and iron supplementation © Paradigm Publishing, Inc. 29 Kidney Failure Drugs for Renal Failure: Diuretics • Thiazides and potassium-sparing diuretics are used for hypertension • Loop diuretics are used for renal failure or reducing edema • See Table 19.6 for commonly used diuretics by class • Routes: all are oral; some are IV; bumetanide is also IM © Paradigm Publishing, Inc. 30 Kidney Failure Diuretic Sites of Action • Thiazide diuretics work in the distal convoluted tubule • Loop diuretics work in the loop of Henle © Paradigm Publishing, Inc. 31 Kidney Failure Drugs for Renal Failure: Thiazide Diuretics • Mechanism of Action: inhibit reabsorption of sodium and chloride ions in the distal tubule of the nephron; water is pulled into urine and eliminated, thus reducing blood volume and pressure • Indication: first-line therapy for newly diagnosed patients with hypertension • Side Effects (common): hypotension, dizziness, headache, rash, hair loss, stomach upset, diarrhea, constipation • Caution: often must take with potassium supplements; several drug interactions including corticosteroids, lithium, and drugs for diabetes; avoid alcohol © Paradigm Publishing, Inc. 32 Kidney Failure Drugs for Renal Failure: Loop Diuretics • Mechanism of Action: inhibit reabsorption of sodium, chloride, and water in the ascending loop of Henle Pulls fluid out of the body rapidly • Indication: swelling and fluid accumulation due to heart or kidney failure • Side Effects (common): hypotension, dizziness, headache, rash, hair loss, stomach upset, diarrhea, constipation • Caution: often must take with potassium supplements © Paradigm Publishing, Inc. 33 Kidney Failure Drugs for Renal Failure: Potassium-sparing Diuretics • Mechanism of Action: block the exchange of potassium for sodium that takes place in the distal tubule; more sodium and water are excreted while potassium is preserved in body • Indication: hypertension • Side Effects (common): gynecomastia • Side Effects (other): stomach upset, headache, confusion, drowsiness • Caution: possible hyperkalemia; monitor potassium levels © Paradigm Publishing, Inc. 34 Kidney Failure Drugs for Renal Failure: Aldosterone Antagonists • Mechanism of Action: Work by inhibiting a hormone that promotes fluid retention Spironolactone, in particular, inhibits aldosterone, which promotes sodium and water reabsorption in the distal tubule and collecting duct of the nephron • Indication (spironolactone): hypertension; sometimes, hyperaldosteronism • Caution (spironolactone): hyperkalemia; monitor potassium levels © Paradigm Publishing, Inc. 35 Kidney Failure Drugs for Renal Failure: Carbonic Anhydrase Inhibitors • Mechanism of Action: work in the nephron by increasing excretion of bicarbonate ions, which carry sodium, potassium, and water into the urine • Indication: open-angle glaucoma, diuresis in CHF • Side Effects (common): tinnitus, nausea, vomiting, diarrhea, drowsiness, tingling, changes in taste • Side Effects (severe): sulfa allergy, Stevens-Johnson syndrome • Caution: do not take with aspirin © Paradigm Publishing, Inc. 36 Your Turn Question 1: What is the purpose of calculating a patient’s GFR? Answer: The GFR is used as a guide for estimating renal function and dosing for drug therapy. Question 2: A patient has edema due to kidney failure. The physician needs a medication to quickly pull a large amount of fluid out of the patient’s body. What drug therapy is the physician likely to order? Answer: The physician will likely order a loop diuretic. © Paradigm Publishing, Inc. 37 Kidney Failure Drugs for Renal Failure: Potassium Supplements • • • • Indication: potassium deficiency caused by diuretics Route: oral; taken daily Side Effects: nausea, vomiting, diarrhea, stomach upset Caution: do not use salt substitutes Drugs for Renal Failure: Osmotic Diuretics • Indication: severe trauma, cardiac operations, elevated intracranial pressure • Mechanism of Action: increases concentration of filtrate, hindering reabsorption of water; mannitol used most © Paradigm Publishing, Inc. 38 Herbal and Alternative Therapies • Saw palmetto is taken for BPH symptoms such as frequent or painful urination and urination hesitancy and urgency Works by reducing thickness of inner layer of prostate and inhibiting 5-alpha reductase Causes dizziness, headache, nausea, vomiting, constipation, diarrhea Has possible interactions with anticoagulants and some hormone therapies • Cranberry juice is taken for prevention of recurrent UTIs Adheres to bacteria, preventing the cells from attaching to the inner walls of the bladder Can interact with warfarin © Paradigm Publishing, Inc. 39 Summary • Antispasmodics are used for spastic or overactive bladder • Alpha blockers and 5-alpha reductase inhibitors are used for BPH • Diuretics are used to improve kidney function and urine production • Thiazides and potassium-sparing diuretics are used most for high blood pressure • Loop diuretics are used to pull large amounts of fluid from the body in patients with heart or kidney failure © Paradigm Publishing, Inc. 40