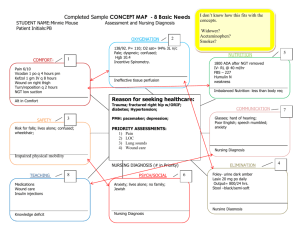
Care Mapping
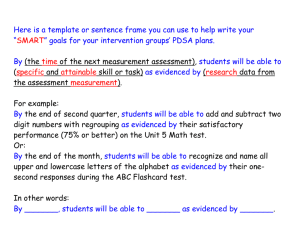
advertisement

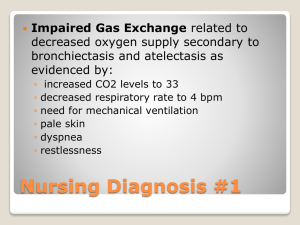
Technologies in Nursing Duquesne University First introduced in 1950. In 1953 Fry proposed the formulation of nursing diagnosis. In 1973, the first national conference was held. In 1982, NANDA was founded. Diagnostic reasoning ◦ A process of using assessment data to create a nursing diagnosis Defining characteristics ◦ Clinical criteria or assessment findings Clinical criteria ◦ Objective or subjective signs and symptoms 1. Medical diagnosis 2. Nursing diagnosis A. Clinical judgment about the client in response to an actual or potential health problem B. The identification of a disease condition based on specific evaluation of signs and symptoms 3. Collaborative problem C. An actual or potential complication that nurses monitor to detect a change in client status 1. Actual Nursing Diagnosis A. Describe human responses 2. Risk Nursing Diagnosis B. Describes human 3. Wellness Nursing Diagnosis C. Describes human to levels of wellness that have a readiness for enhancement responses to health conditions/life processes that may develop responses to health conditions or life processes Problem Etiology Signs and Symptoms By learning to make accurate nursing diagnoses, your care plan will help communicate the client’s health care problems to other professionals. A nursing diagnosis will ensure that you select relevant and appropriate nursing interventions. Problem—the name or diagnostic label identified from the NANDA list. This may be an actual problem, a risk (potential) problem, or a wellness diagnosis. The suspected cause or reason for the response that has been identified from the assessment They are stated “as evidenced by (A.E.B.)” or “as manifested by”, followed by a list of subjective and objective data. “Risk” problems have no evidence statement. Ineffective Airway Clearance, related to increased pulmonary secretions and bronchospasm, evidenced by wheezing, tachypnea, and ineffective cough. Acute pain related to tissue distention and edema as evidenced by reports of severe colicky pain in right flank, elevated pulse and respirations, and restlessness. Hyperthermia related to increased metabolic rate and dehydration as evidenced by elevated temperature, flushed skin, tachycardia, and tachypnea. Risk for infection, related to broken skin, traumatized tissues, decreased hemoglobin, invasive procedures, increased environmental exposure. Risk for skin breakdown related to immobility as evidenced by stage III sacral wound (7 X3 cm) Pain related to myocardial infarction as evidenced by patient’s report of pain at 9 on the 1-10 pain scale Ineffective airway clearance related to pneumonia as evidenced by adventitious breath sounds, sputum production, and abnormal chest x-ray. Fluid volume deficit related to blood loss through wound as evidenced by hemoglobin of 8 and hematocrit of 26% Fluid volume deficit related to NPO status as evidenced by weight loss Diarrhea related to C. Diff as evidenced by 10 stool in one day Risk for infection related to invasive procedure (surgery) Readiness for enhanced knowledge of disease process. Based on a medical diagnosis Examples: ◦ Risk for pneumonia related to immobility ◦ Risk for DVT related to immobility ◦ Risk for myocardial infarction related to inadequate tissue perfusion Written in general terms Not behavioral in nature Patient centered Example: To enhance airway clearance and improve oxygenation Actions that the nurse carries out for the client or encourages the client to do for themselves. Include interdisciplinary actions, but identify them as such. Includes assessment Includes teaching the client Include the rationale for the intervention. Specific Measurable Attainable Realistic Time oriented ◦ The patient will identify four adaptive/protective measures for individual situation by discharge. ◦ The patient will maintain a patent airway, ongoing. (This outcome is stated as “ongoing” and does not include a specific timeframe other than discharge from care. In this example, this is appropriate because the situation may not resolve until the patient’s condition or status changes or discharge has occurred.) ◦ The patient will be free of skin breakdown. (This is another example of an ongoing outcome). ◦ The patient will demonstrate correct insulin administration techniques within 48 hours. The patient will attain pain relief identified as a “3” on the 0-10 pain scale 30 minutes after being medicated with pain medication. The patient will maintain an oxygen saturation of 92 or higher. The patient will not incur a fall. Should refer directly to the nursing diagnosis and to the goal.