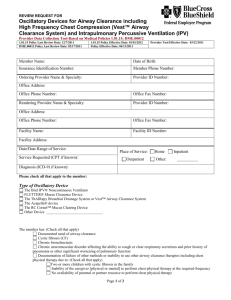
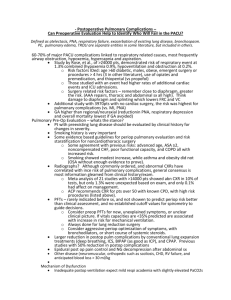
Patient's Cost
advertisement

Reducing The Cost Of Pulmonary Impairment In Children With Neuromuscular Disease Chris Landon, MD, FAAP, FCCP Ventura County Medical Center Ventura, California Audrius Plioplys, MD, CMD,FRCPC, FAAP Mercy Hospital Chicago, Illinois Objectives 1. Provide an overview of neuromuscular diseases and complications that predispose patients to frequent respiratory exacerbations. 2. Identify treatment strategies/medically appropriate care to meet needs of this difficult patient population to promote improvements in quality of life, and positive clinical outcomes. 3. Discuss evidence supporting the effect of airway clearance with The Vest system on reducing costs associated with pulmonary complications/exacerbations. Neuromuscular Diseases: Overview Children who experience varying degrees of neurological/neuromuscular dysfunction Diagnoses include: cerebral palsy, muscular dystrophy, spinal muscular atrophy, brain injury, consequences of infectious disease, inherited metabolic disorders, etc. – One child in 1000 is institutionalized as a result of profound disability Neuromuscular Diseases: Overview Multi-system assessment necessary to determine risk of pulmonary involvement: Neuromuscular Gastroesophageal Immune system Respiratory Psychosocial Neuromuscular Diseases Assessment of complications that predispose to pulmonary involvement Neuro – – – – – – – assessment Skeletal muscle control Respiratory and ventilatory muscle abnormalities Weak/absent cough Weak/absent gag reflex Upper airway control and coordination Seizure activity Spasticity Neuromuscular Diseases Assessment of complications that predispose to pulmonary involvement Neuro – – – – – assessment – Dysphagia Oral motor dyskinesia/pseudobulbar palsy True bulbar palsy Dysfunctional arousal Oral motor weakness Increased secretions Neuromuscular Diseases Assessment of complications that predispose to pulmonary involvement Neuro assessment – Oral motor weakness Typical symptoms – Muscular dystrophies – Too weak to swallow – Myopathies – Too weak to cough – Neuromuscular junction disorders – Easily fatigued – Anterior horn cell disorders – Head position dependent Neuromuscular Diseases Assessment of complications that predispose to pulmonary involvement Neuro assessment – Increased secretions Typical symptoms – Autonomic dysfunction – Constant drooling – Medication effects – Worse with stress or infection – Frequent seizures – Drowning in drool Poor Swallow Control (Dysphagia) Oral motor dyskinesia / pseudobulbar palsy True bulbar palsy Dysfunctional arousal Oral motor weakness Increased secretions Oral Motor Dyskinesia / Pseudobulbar Palsy Diffuse or bilateral cortical damage Basal ganglia damage Cerebellar – brainstem damage Oral Motor Dyskinesia / Pseudobulbar Palsy Typical symptoms: – – – – Increased gag, choking, vomiting Nasal regurgitation Tonguing – pushing Poor tolerance of liquids and chunks True Bulbar Palsy Cranial nerves 9, 10, 12 Pontine-medullary damage Arnold-Chiari malformation Bulbar syrinx Moebius syndrome True Bulbar Palsy Typical symptoms – – – – – Decreased gag, poor palate movement Pocketing of food Rumination Drooling “O” sign Dysfunctional Arousal Disorder of excessive somnolence Toxic encephalopathy Drug induced stupor Autistic disorder Dysfunctional Arousal Typical symptoms – – – – Must be reminded to swallow Falls asleep while eating Poor cough reflex “Q” sign, string bean sign Oral Motor Weakness Myopathies Muscular dystrophies Neuromuscular junction disorders Anterior horn cell disorders Oral Motor Weakness Typical symptoms – – – – Too weak to swallow Too weak to cough Easily fatigued Head position dependent Increased Secretions Autonomic dysfunction Medication effects Frequent seizures Increased Secretions Typical symptoms – Constant drooling – Worse with stress or infection – Drowning in drool Poor Breathing Control Central neurogenic hypoventilation Periodic breathing patterns Ondine’s curse Stupor and coma Thoracic weakness Central Neurogenic Hypoventilation Diffuse cortical damage Poor hypoxic response Poor hypercarbic response Worse with stress or infection Periodic Breathing Patterns Cheyne-Stokes respiration Biot’s respiration Rett’s syndrome Apneustic breathing Ondine’s Curse Waking versus sleeping centers Defect in shift to automatic breathing “… if I should die before I wake…” Stupor and Coma Brainstem dysfunction from pressure Brainstem dysfunction from ischemia Brainstem suppression from drugs Brainstem degeneration Thoracic Weakness Myopathies Muscular dystrophies Neuromuscular junction disorders Anterior horn cell disorders Recognition of Neurogenic Pulmonary Clearance Problems Recognize the possible brain region involved Perform a careful history Perform a careful examination Sleep study / Life Shirt MRI – attention to brainstem ? muscle studies ? Gastroesophageal Function and Complications The Upper AirwaySwallowing and Aspiration Aspiration Associated Pneumonias Lower Esophageal Aspiration, Gastric Distention and Airway Remodeling Gastroesophageal Reflux Disease (GERD) Fundoplication Versus Medication and Airway Clearance Nutrition and the Immune System The Faces of Dysfunction Arching Failure To Thrive Irritability Gagging and Choking Regurgitation Refusing Feedings Sandifer’s Syndrome Characterized by arching and turning the head to the side (opisthotonos) may give the appearance of a seizure. Functions to clear the esophagus of acid reflux by increasing intrathoracic pressure. Cardiorespiratory Reflexes Cardiorespiratory Reflexes Refluxate Refluxate Protection The Immune System Genetic Abnormalities Nutritional Compromise of the Immune System Stress and Immune Response Recurrent Infection and Frequent Use of Antibiotics: The Impacts Allergies Reactive Airway Disease (RAD) Airway Clearance Therapy Respiratory Medical History – Number of Pulmonary Infections Annually – Number of Hospital Admissions Annually – Number of ER Admissions Annually – Number of Courses of Antibiotics for Respiratory Infections Annually – Immunization History – History of Recurrent Infections with Respiratory Syncytial Virus (RSV) Quality Airway Clearance Therapy Should •Clear secretions effectively and consistently •Preserve lung function •Reduce infectious exacerbations •Reduce dependence on antibiotic therapy and other medications •Reduce need for hospitalization and auxiliary medical services •Delay disease progression •Reduce the burden of care •Enhance the quality of life Neuromuscular Disease - Perioperative Care High Risk For Post-Operative Complications Atelectasis Pneumonia Respiratory Failure Need for prolonged ventilation Tracheostomy Death Problems Weak cough Dyscoordinated swallow Aspiration Difficulty clearing secretions Increased lower respiratory tract infections Respiratory Weakness May not be apparent on physical exam Respiratory failure when work of breathing is increased Chronic Respiratory Muscle Weakness Reduced lung volumes Microatelectasis V/Q mismatch Scoliosis Decreased compliance of the chest wall Decreased pulmonary compliance Hypoxemia only during sleep Hypoventilation due to muscle weakness Hypoventilation due to central hypoventilation Preoperative Assessment Thorough history Physical examination Laboratory studies Thorough History Frequency and severity of respiratory tract infections Pulmonary complications of previous surgeries History suggestive of reactive airways disease – Even mildly increased airway obstruction may lead to respiratory failure in the postoperative period in a patient with severe respiratory muscle weakness Physical Examination Gag reflex Cough Adequacy of aeration Presence of adventitial lung sounds Ability To Cooperate With PostOperative Pulmonary Therapy General muscle strength Physical and intellectual capacity Laboratory Examinations Chest x-ray Arterial blood gases or mixed venous gas measurements and oximetry Complete blood count Pulmonary Function Tests All children who are capable of performing them – Lung volumes – Pre and post bronchodilator – Maximal inspiratory and expiratory mouth pressures »frequently decreased more than lung volumes and flows »do not correlate with general muscle strength Alternative/Competitive Airway Clearance Modalities Chest Physiotherapy Mechanical techniques for the noninvasive clearance of excessive secretions and aspirated materials from the airway Prevent, Treat, or At Least Delay The Effects of Mechanical,Infectious, and Biochemical Sequelae prevent resistance to airflow work of breathing hyperinflation atelectasis maldistribution of ventilation ventilation-perfusion mismatch Microorganisms and Host -Mediated Inflammatory Mediators intrabronchial accumulation of secretions – vicious circle of infection – impaired clearance – progressive airway damage Improve Access To The Bronchial Surface Allow inhaled medications to penetrate Effectiveness and Safety Easy to teach to patients and caregivers Should not fatigue the patient Time efficient and practical Whenever possible patient should be participant Mechanical Percussors Mechanical Percussors •Theory: Shock waves transmit through chest loosening secretions in the airways—often dependant on positioning to drain mucus into upper airways •Technique: Patient is positioned for optimal drainage of lobe to be percussed with each area being treated for 2-5 minutes •Considerations: Patient’s mental and physical limitations may impede, technique dependant, labor intensive, and positioning tolerance •Patient’s Cost: $80-150 Positive Expiratory Pressure (PEP) Manufacturers: DHD Healthcare & Pari Respiratory Equipment, Inc. Positive Expiratory Pressure (PEP) •Theory: Prolonged exhalation with positive pressure stabilizes smaller airways open allowing inhaled air to pass and then on exhalation move secretions into larger airways •Technique: Patient exhales through flow restrictor via mask or mouth piece and then performs “huff” cough—typical treatment last about 15-20 minutes •Considerations: Patient’s mental and physical limitations may impede, technique dependant, for ages >4, unit is portable, and maybe self administered •Patient’s Cost: $30 Flutter Valve Manufacturer: Scandipharm Flutter Valve •Theory: Intermittent positive pressure breaths with airway oscillation vibrates the airway walls and loosens secretions— accelerated expiratory flow rates move secretions to larger airways •Technique: Patient exhales through the device causing the steel ball to oscillate rapidly for 5-6 breaths than coughs and repeats for a minimum of 15 minutes—the position/angle of the device determines intensity of vibration •Considerations: For ages > 5, technique dependant, requires cognitive and physical function, portable, and may be self administered •Patient’s Cost: $90 Acapella Manufacturer: DHD Healthcare Acapella •Theory: Intermittent positive pressure breaths with airway oscillation vibrates the airway walls and loosens secretions— accelerated expiratory flow rates move secretions to larger airways •Technique: Patient actively exhales through the device causing rapid oscillation for 10-20 breaths than coughs and repeats for between 15-25 minutes—the dial on the end of the device determines intensity of vibration •Considerations: May not be appropriate for younger patients (<5y/o), technique dependant, requires cognitive and physical function, portable, is not position dependant, and may be self administered •Patient’s Cost: $88 Intrapulmonary Percussive Ventilation (IPV) Manufacturer: Percussionaire Intrapulmonary Percussive Ventilation (IPV) •Theory: High Frequency positive pressure air puffs are thought to open collapsed areas with in the lung and help air get behind mucus plugs aiding in clearance •Technique: During inspiration the patient/caregiver depresses button that triggers delivery of up to 300 bursts of air per minute— the button is released during exhalation and the cycle repeated for 20 minutes, followed by coughing to clear secretions •Considerations: May be used by vent patients, technique dependant, requires adequate cognitive and physical abilities, for ages >5, increased chances of air swallowing, position independent, may be self administered, and may be used for nebulized meds. •Patient’s Cost: $8,200--??warranty PercussiveNeb Manufacturer: Vortran Medical Technology1, Inc. PercussiveNeb •Theory: High Frequency positive pressure air puffs are thought to open collapsed areas with in the lung and help air get behind mucus plugs aiding in clearance •Technique: During inhalation the patient receives nebulized medication/saline, while on exhalation the unit delivers positive pressure burst up to 800 times per minute—typical treatment lasts between 10-20 minutes followed by coughing to clear secretions • Considerations: Technique dependant, requires adequate cognitive and physical abilities, for ages >5, increased chances of air swallowing, position independent, may be self administered, and may be used for nebulized meds. •Patient’s Cost: $140 Cough Assist (InExsufflator) Manufacturer: J. H. Emerson Co. Cough Assist (InExsufflator) •Theory: Positive pressure to the airway, followed by a rapid transition to negative pressure produces cough like expiratory flows aiding in secretion clearance from larger airways •Technique: Via facemask, mouth piece, or trach adaptor , positive pressure is delivered to the airway and then shifted rapidly to a negative pressure for 4-5 breaths, followed by a resting period— typical treatment time is between 10-15 minutes followed by coughing to clear secretions •Considerations: Technique dependant, requires caregiver/patient cooperation, geared towards patients with weak cough function, and may be self administered by some users •Patient’s Cost: $6,000—2 year warranty MedPulse Manufacturer: ElectroMed, Inc. Med Pulse •Theory: High frequency chest wall oscillation clears secretions by both creating shear forces between air and secretions in the lungs, moving mucus towards larger airways, and decreasing the viscosity, allowing for easier clearance •Technique: Patient places vest around chest setting prescribed pressure and frequency then turns unit on pausing at 5-10 minute intervals to cough and clear secretions—treatment typically lasts 1530 minutes •Considerations: For ages >2, technique independent, provides passive therapy, may be used on patients with cognitive/physical impairments, and treats all lobes simultaneously •Patient’s Cost: $11,999 with vests costing $500 each—2 year warranty Hayek Oscillator Manufacturer: Breasy Medical Equipment, Ltd. Hayek Oscillator •Theory: High frequency chest wall oscillation clears secretions by both creating shear forces between air and secretions in the lungs, moving mucus towards larger airways, and decreasing the viscosity, allowing for easier clearance—the Hayek is primarily designed as a non-invasive ventilator with a airway clearance mode and uses both positive and negative pressure during oscillation •Technique: Patient places shell snuggly around chest setting prescribed pressure and frequency then turns unit on—we are unaware of a standard protocol for use in airway clearance •Considerations: Shell fit may be difficult with abnormally shaped chests, little offered in the way of product information/support, for use on neonates to adults, and weighs 110 pounds •Patient’s Cost: Last reported around $20,000 Airway Clearance Percussion and Postural Drainage -Mechanical percussors Expiratory Pressure Modalities -Positive Expiratory Pressure (PEP) -Flutter Valve -Acapella High-Frequency Intrapulmonary Positive Pressure -Intrapulmonary Percussive Ventilation (IPV) -PercussiveNeb Intrapulmonary Positive/Negative Pressure -Cough Assist (InExsufflator) High-Frequency Chest Wall Oscillation -MedPulse -Hayek Oscillator The Aristotelian tradition, defined tragedy as a drama which concerns better than average people (heroes, kings, gods) who suffer a transition from good fortune to bad fortune, and who speak in an elevated language. Tragedy, in the Aristotelean tradition, serves the purpose of purging the soul of the "fear and pity" which most of us carry around (Aristotle called this catharsis ). In some ancient Greek drama, an apparently insoluble crisis was solved by the intervention of a god, often brought on stage by an elaborate piece of equipment. This "god from the machine" was literally a deus ex machina. We have a group of 5 patients for whom chest physiotherapy did not achieve effective airway clearance and who where to small to be effectively fit with Advanced Respiratory (formerly American Biosystems) child-medium vest for oscillatory therapy. We changed the configuration of the vest to a "belt" without occluding any of the surface features of the vest. The Model 103 generator from Advanced Respiratory was used. We were able to achieve an effective fit for each of these children without significant changes in pressure transmitted to the chest (.30 psig(vest) versus .38 psig(belt)). Pressures for therapy were adjusted downward and no child received therapy at a pressure setting higher than 4 (range 0 to 10) on the 103 Model Generator. Frequencies for therapy were kept in the range of 10-16 Hz (range 0-25 Hz). Therapy with the "belt" was well tolerated by this group of children and effective therapy could be delivered. There were no adverse events related to this modification. This simple modification may be a helpful adjunct to achieving effective airway clearance therapy in this unique group when chest physiotherapy fails to achieve the desired results. Risk For Anesthetic Complications Malignant hypothermia Cardiac arrhythmia Excessive potassium release Myoglobinuria Prolonged skeletal muscle contraction in muscular dystrophy – succinylcholine With Care We Can Minimize PostOp Risk Even In Severe Neuromuscular Disease Ventilatory support planned for 24-48 hours post surgery But avoiding more prolonged ventilation – disuse atrophy – respiratory muscle weakness Chest Physiotherapy Is The Keystone To Success Unable to perform incentive spirometry Clearance of secretions and prevention of atelectasis Every 2 to 4 hours after surgery Frequency May Be Reduced If Tolerates Extubation For 24 Hours Without Complication IPPB may be helpful in severe neurologic disease' Oxygen saturation should be >95% Hematocrit over 35% Careful Attention To Fluid Balance Decreased pulmonary compliance and hypoxemia if lung water is increased Scoliosis repair even more critical setting Careful Attention To Even Minimal Bronchospasm Bronchodilator aerosols Consider theophylline or steroids Careful Attention To Atelectasis Prevention Bronchodilator aerosols Mucolytic aerosols Vigorous CPT and suctioning IPPB Consider bronchoscopy – removing secretions – obtaining culture Direct Antibiotic Therapy Against Specific Pathogens Normal mouth flora and anerobes secondary to aspiration Consider surveillance cultures prior to surgery Posterior pharyngeal cultures "Pulmonary evaluation of rehabilitation and therapy in medically fragile children" which is being submitted in response to the RFA HD#02-027 HYPOTHESIS: Children and adolescents (6 to 18 years of age) with moderate to severe developmental disabilities with an adequate regimen of pulmonary toilet can have an improved quality of life. The development, validation and analysis of the three proposed tools will facilitate the statistical evaluation of specific indicators that correlate to risk of further deterioration in pulmonary function. This study will 1) further define the scope and nature of respiratory failure in children, especially those with special needs, 2) develop and evaluate acute and chronic management strategies to prevent or minimize the development of chronic respiratory failure in children or to ameliorate its effects. Recent scientific and engineering advances, including the availability of innovative approaches and techniques for measuring and treating pulmonary dysfunction open new avenues of exploration to be utilized to enhance the management and quality of life for children with respiratory failure. This study will focus on those children and adolescents with moderate to severe developmental disabilities, who reside in residential care, skilled nursing, domiciliary facilities and their group homes. Subjects will include ethnically diverse, male and female subjects. Standard procedures will be utilized to gather comprehensive baseline and follow-up data, score serial chest x-rays, evaluate quality of life perceptions of caregivers, gather physiologic data related to cardiopulmonary evaluation at rest, exercise and sleep, structured protocols for airway clearance therapy and routine follow-up at 14, 30, 90, 180 days and 1 year and two years at the affiliated institutional clinics routinely caring for these subjects. Because of the negative impact and increased cost of care related to increased risk of pulmonary compromise in this group we are targeting development of broader definition of the medically complex child with a focus on the structural and pathological changes in the thoracopulmonary structures and proposing a chest radiograph scoring system to stage disease progression and evaluate effectiveness of therapy in reducing pulmonary infections and their sequelae. The chest radiograph scoring system is based on currently recognized, landmark based analysis of intrapulmonary evidence and generally recognized radiographic signs of long term changes associated with chronic processes. Validation will be tested across a spectrum of radiology practitioners to determine if there is statistically significant agreement in the interpretation of chest radiographs. Additional data will be gathered to determine if there are general hallmarks of disease progression across the group of children studied and whether there is a correlation between reduced incidence of pulmonary infection and any mode of airway clearance therapy. The definition proposed will recognize the difference amongst the constellation of diagnoses, but focus on the relevant similarities across this group of children as relates to common structural abnormalities, common sources of compromise that increase the risk of pulmonary complications, and risk based analysis associating degree of disability with the prevalence of recurrent pulmonary infection. Baseline data will be collected utilizing a multifactor intake tool that will be completed utilizing the medical record and physical assessment at the time of intake and follow-up assessments at 30, 60, 180 days, 1 year and 2 years. A Caregiver Related Quality of Life tool will be administered at the same intervals as stipulated above. CRQOL will be administered to all caregivers involved in a child’s direct care. This comprehensive evaluation protocol will inform us as to the effectiveness of specific modes of evaluation, measurement and outcome analysis as relates to the special needs child at risk for pulmonary complications and respiratory failure. We will also be able to evaluate the effectiveness of specific therapeutic regimens and the impact of consistently applied airway clearance therapy National Airway Clearance Registry Overview Rationale Objectives Design NACR Overview Patients with pulmonary disorders often experience a vicious cycle of obstruction, inflammation, infection, and destruction of lung tissue. In many cases, this begins with airway clearance abnormalities. The National Airway Clearance Registry (NACR) is designed to document the epidemiology and impact of airway clearance and hypersecretion disorders, and the associated economic and human costs. Patients identified by participating physicians and healthcare teams will be able to use The Vest™ airway clearance system for a 60-day screening trial. Following the screening trial, patients, with physician input, will select standard medical management, or standard medical management plus the Vest and be followed for up to three years. NACR Rationale Conducting separate clinical trials in numerous patient populations and disease states with airway clearance needs is impractical, time consuming, and extremely expensive. The similarities between the patient profiles and the pulmonary complications associated with impaired airway clearance will allow us to take a different approach. The NACR will allow us to collect clinical data on numerous patient populations and sub-groups while focusing on the key endpoints associated with airway clearance-related problems. The Registry will use the power of large numbers compiled over time to answer key clinical questions. Treatment Registry Observational research program for capturing actual experience in clinical practice in order to gathering additional information on: » Post-market safety/tolerability of treatment(s) » Health and economic outcomes of treatment(s) » Cost-effectiveness of treatment(s) » Epidemiology, e.g the clinical course of disease with and without treatment(s) *A registry typically involves more patients and a longer duration than a clinical trial Randomized Clinical Trial Data Registry Considered the “Gold Standard”, more rigorous methodology, hypothesisdriven Considered observational, less rigor, hypothesisgenerating Randomized Not randomized Control group No concurrent control group Restrictive inclusion/exclusion criteria Broad enrollment criteria Patient visits strictly defined by protocol Recommended visits at specific time intervals NACR Clinical Objectives Document the impact of airway clearance complications and airway clearance therapy (ACT) on pulmonary health, healthcare utilization, and disease progression among different patient populations. Document similarities and differences in clinical outcomes, healthcare utilization, patient-reported treatment satisfaction and usage associated with different forms of ACT. Document and describe the ACT practices among different patient populations in terms of ACTs used, prescribed protocols, and patient-reported treatment satisfaction and usage. Determine predictors of successful outcomes for therapy with The Vest in order to better define patient selection criteria for various patient populations. Medical Advisory Board Frank Accurso, M.D. Children’s Hospital Denver, CO Andrew Gelfand, M.D. Pediatric Pulmonary Specialists, PA Dallas, TX Dean Hess, Ph.D., R.R.T. Massachusetts General Hospital Harvard Medical School Boston, MA Steve JuliusM.D. Scottish Rite Children’s Hospital Atlanta, GA Michael Konstan, M.D. Rainbow Babies and Children’s Hospital Cleveland, OH Ron Morton, M.D. Kosair Children’s Hospital Louisville, KY Virginia Simson Nelson, M.D. University of Michigan C.S. Mott Children’s Hospital Ann Arbor, MI 48109-0242 Kerstin Sobus, M.D. Altru Health Institute Grand Forks, ND 58206 Jean Stansbury, R.N., C.N.P. Gillette Children’s Hospital-Outpatient Clinic St. Paul, MN 55101 NACR Site Eligibility Clinical Centers within the United States that: Regularly see patients that are prone to airway clearance complications Have a strong potential to enroll a minimum of 20 registry patients within one year of participation Have computer and internet access Can designate an individual from their staff, in addition to the site physician(s) that can serve as the key contact/coordinator for their site NACR Patient Outcomes Patient-reported outcomes: – Treatment satisfaction – Treatment adherence – Symptom (cough and sputum) assessment Clinical outcomes: – Pulmonary functions (FEV1, FVC, FEF25-75), tidal volume and vital capacity – Respiratory rate, O2 saturation, end-tidal CO2 Cost-related measures (direct and indirect): – # non-routine physician office visits – # ER visits – # hospitalizations, LOS – # ICU visits, LOS – # Pulmonary exacerbations requiring antibiotics – Reduction in concomitant medications or therapies – Missed days from work or school