Respiratory - gastonlpnspring
advertisement

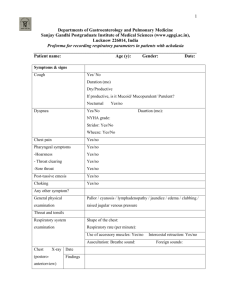
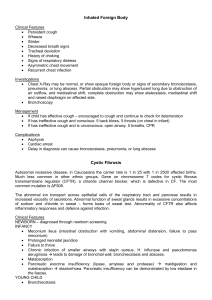
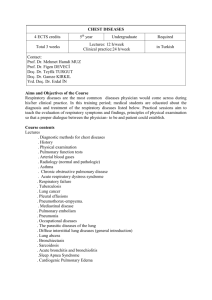
Respiratory Structure and Function The primary function- bring oxygen into the body so that it can reach all body tissues via the blood stream To remove carbon dioxide To maintain acid-base balance To protect the airway from infection Upper Respiratory System Mouth Nose Pharynx Larynx Epiglottis closes during swallowing to prevent aspiration and opens to allow air passage Trachea (can be upper or lower) - protected by hard cartilage- Carinaii at the bottom of the trachea where it splits. If hit during suctioning will have to back out Lower Respiratory System Trachea Lungs Bronchi and bronchioles Alveoli- basic functioning units of the lung Pulmonary capillary network- brings deoxygenated blood from the right ventricle of the heart to the tip of the alveoli and the oxygen will diffuse into the capillary bed and carbon dioxide will go out of the capillary into the alveoli. This newly oxygenated blood will go into the pulmonary vein back into the left atria of the heart to be sent out of the aorta to the body. Plural membranes Outside- parietal Inside- visceral Alveolus Basic functioning unit of the lung and are more than 300 million per lung Outer layer contains surfactant that helps keep the alveoli open and elastic- surfactant missing in preemies, alveoli will not stay open, can’t breathe on their own Chemo-receptors Aortic and Carotid bodies (computer chips) Detect Carbon Dioxide and when level is too high it sends chemical stimulus to the medulla oblongata and is the stimulus breathe in most people Intact nervous system required to work In COPD, Oxygen is the stimulus to breath and is called the oxygen deprivation drive. Oxygen therapy must be limited to 2-4 LPM. External Respiration Ventilation: air moves in and out of the lungs External Respiration: Oxygen and carbon dioxide are exchanged- alveoli and blood Perfusion: Transportation through the blood Internal Respiration When the oxygen and carbon dioxide are exchanged between the blood cell and the target body cell Diaphragm and Atmospheric Pressure When the diaphragm contracts and pushes downward causing the lung space to become larger and facilitating inspiration. When the diaphragm relaxes, it moves upward and decreases the lung space and causes exhalation. Slight negative pressure- sub atmospheric- exists in the pleural space- just enough to keep the lungs open Inspiration increases the vacuum or negative pressure- inhale When pressure is equal or slightly greater, then the diaphragm contracts Greater pressure must be exhaled Tests for oxygenation Arterial Blood Gases Watch for signs of bleeding, apply at least 3 minutes of pressure About 3% of inspired oxygen is absorbed into the plasma PaO2- 80-100 mmHg PaCo2- 34-45 mm Hg pH= 7.35-7.45 Oxygen Saturation- O2 sats 95-100% below 70 life is threatened Oxygen Saturation Room Air: 21% oxygen- 78% nitrogen- 1% other gases fiO2- 21% 97% oxygen bound to hemoglobin SaO2- 94-95% if below 90% then PaO2 less than 60 mmHg- hypoxia Oxygen Supplementation Low flow and High Flow- low flow is less accurate delivery than a high flow system Low: Nasal cannula- most commonly used- 2-4 LPM COPD patients- only 40-44% at 6 lpm, maybe Simple face mask Non-rebreather- has disk that allows CO2 to escape so that it is not breathed back instill influenceable and low flow High: Venturi mask- accurate delivery flow at 24% or 44%. Hypoxemia Decreased amount of oxygen in the blood Results in decreased oxygen at the cellular level (called hypoxia) Also results in increased levels of carbon dioxide (hypercapnia or hypercarbia) and may progress to respiratory acidosis Onset may be rapid or gradual Patient is post op and appears to be sleeping. Respiratory rate is 6. – Hypoventilation leading to hypoxia and respiratory acidosis and respiratory arrest. Signs Restless, irritability, confusion in the beginning Dyspnea Tachypnea, stridor (normal 12-20) Abnormal lungs sounds Cyanosis, retractions, arrhythmias Acid-base balance disturbances Orthopnea Decreased O2 sats Clubbing of the fingers Lung Sounds Rales- heard on inspiration generally- bubbly Rhonchi- better heard on expiration- more musical crackles Tracheostomy Reasons Tube inserted in the trachea to provide and maintain a patent airway To remove secretions from clients unable to cough Replace endotracheal tubes Use positive pressure ventilation Prevent aspiration Signs that Suction is Needed Restlessness, gurgling/rattling sounds Unable to expectorate secretions Unable to swallow Adventitious breath sounds when auscultated Change in LOC Skin color- cyanotic/dyspneic Rate and pattern of respirations Pulse rate/rhythm Parts of Tracheostomy Outer cannula with flange- placed by Md. Will be held in place with straps. Inner cannula- goes inside the outer cannula. Can be removed and cleaned Obturator- helps get it through the skin. Will want to hang on to it Tracheostomy Tubes Curved tube inserted into a tracheostomy, a surgical incision in the trachea just below the first or second tracheal cartilage The tube extends through the tracheostomy stoma Metal-plastic-foam Outer cannula-inner cannula-Obturator Single cannula Cuffed Tracheostomy Have an inflatable cuff that produces an airtight seal between the tube and the trachea Seal prevents aspiration of oropharyngeal secretions and air leakage between the tube and the trachea Limit to 20 cm. of pressure in the cuff to prevent tissue necrosis of the trachea. Uncuff policy must be followed Procedure Wash hands and gather supplies. Don gloves and mask with eye shield Check suction at 80-120 mm Hg. Pressure Hyper-oxygenate by: 100% O2 flush- 15 lpm Deep breaths 3-5 Prepare 2-5 mL of sterile saline for lavage if needed Open sterile suction tray first and keep it closest to your patient #12-14 Fr Open cleaning tray Open sterile saline and Hydrogen Peroxide Fill suction container with sterile saline Lubricate and insert catheter without suction approximately 5-6 inches in the adult Meet resistance at carina- pull back 1 centimeter Suction 5-10 seconds Remove and rotate catheter with suction If not successful use 2 mL of saline and suction again (infants- 0.5 mL) Suction stat with saline lavage If not using the saline allow 2-3 minutes between suctions Hyper-oxygenate Remove dressing and inner cannula and put cannula in hydrogen peroxide Documentation: Excessive, white thin mucous from the tracheostomy, cyanotic lips, jerking at covers, trying to sit up in bed. Crackles notes in right upper love, dyspnea, RR28 and shallow. Suctioned large amount of with thin mucous from trach X2 Trach care done. Hyperoygenation and hyperventilation done. LS clear bilaterally, skin pink, RR 24 and regular Other assessment tests Pulmonary function test: Breathe through a machine with nose pinched by clamp Measures lung capacity Tidal volume: total air exchange with normal breathing Total lung capacity: total volume of lungs at a maximum inflation pg. 509 Chest Drainage Tubes Used to remove air from the patient with a pneumothorax or hemothorax or after chest surgery Connected to a drainage device that allows air or drainage to escape and not enter the cavity May require suction to operate or may use gravity drainage Tubes are removed and an occlusive dressing is applied when the air is removed from the plural space. Tall, skinny, young adults may spontaneously have pneumothorax This drains the cavity of air, blood, fluid, whatever, so that the negative pressure can be reestablished, the lungs can reinflate, and oxygen exchange can resume Water Seal Drainage 1st part will be drainage collection- no more than 100 cc per 24 hour period, but can be more 2nd part will be the water seal- tip end of tube needs to be under 2 cm of water at all time- keeps air from reentering the chest cavity 3rd part will be for suction- will fill with Md. Prescribed water to create the amount of suction. When you have water seal, when the patient breathes the water will move up and down with each breath. But, you should never see bubbling in the 2nd chamber, because that is a leak and has to be found before the lung collapses again If two tubes, the upper tube will be to drain air, the lower tube will be to drain fluid or blood. NO dependant loops, kinks or clamps (clamp only for seconds changing bottles or looking for leaks) as can cause tension pneumothorax and Mediastinal shift Empymea Pus in the pleural space caused by bacteria Do thoracentesis not chest drainage Thoracentesis: removal of fluid or pus by needle aspiration in the pleural space Over the bedside table Hold breath Antibiotics and chest x-ray needed Respiratory Acidosis- Hypercapnia Abnormal decrease in the pH of the blood due to decreased ventilation of the alveoli leading to elevated CO2 Hypoventilation- decreased ventilation- holding the CO2 in. Decreased respirations. Acute: CO2 over 47 mm Hg and pH <7.35 Chronic- near normal pH (renal compensation) and elevated CO2 and elevated Na Bicarb Or HCO3 > 30 mm Hg- this is the body trying to compensate Respiratory Alkalosis Caused by hyperventilation of the alveoli resulting in CO2 being blown off by the lungs Acid is lost resulting in respiratory alkalosis pH is higher end of spectrum 7.45 Disrupts the calcium balance Causes: Anxiety Labor Hysteria Fever Caffeine Symptoms Numbness and tingling Tetany or twitching/convulsions Person faints Pneumonia Three Groups: 1. Community Acquired, due to a number of organisms, namely Streptococcus pneumonia 2. Hospital or nursing home acquired (nosocomial) due to a gram negative (Klebsiella) bacilli and staphylococci 3. Immunocompromised person like person on chemo or steroids- increases likelihood of overwhelming infection. Factors Any condition that interferes with normal drainage of the lung- example: cancer Postoperative patients may develop pneumonia since anesthesia impairs respiratory defenses and decreases diaphragmatic movement Depression of the CNS examples: drugs, heart trauma, alcohol Person over 65 have a high mortality rate, even with appropriate antimicrobial therapy Natural resistance should be maintained: nutrition, rest, exercise Avoid people with URT infections Avoid obliteration of the cough reflex and aspiration of secretions prevented. Immobilized clients should be turned every 2 hours Susceptible persons (elderly and chronically ill) should be immunized against influenza and pneumonia Signs and Symptoms Sudden Onset Shaking chills Leukocytosis- WBC’s increased Rapidly rising fever- 101-105F Cough productive of purulent sputum Color sputum depends on infectious agent- Brown, rusty colored sputum in 48 hours if Streptococcus Pleuritic chest pain, aggravated by respiration or coughing Tachypnea (25-45/min) accompanied by grunting, nasal flaring, use of accessory muscles Rapid, bounding pulse Skin is hot and dry Mucous membranes dry N/V/D Restless Delirium Streptococcal Pneumonia May be Hx of previous respiratory infection Sudden onset with shaking and chills Rapidly rising fever Tachypnea Productive rusty brown or green purulent sputum Pleuritic pain aggravated by cough Chest sounds dull to percussion Chest sounds: crackles, bronchial breath sounds Confusion may be the only symptom presenting in the elderly Herpes simplex lesions often present on face or lips Penicillin G or Erythromycin, clindamycin, cephalosporins, trimethoprim-sulfa-methoxazole Complications: Septic shock Pleural Effusion: escape of fluid into the pleural linings of the lungs Pericarditis Otitis Media Staphylococcal Pneumonia Often prior history of viral respiratory tract infection Insidious onset of cough with yellow, blood streaked mucous Fever, pleuritic chest pain, progressive dyspnea Pulse varies may be slow in proportion to temperature Must be isolated! Infections often lead to necrosis and destruction of lung tissue Treatment must be vigorous and prolonged May develop drug resistance Penicillin Staph Complications Effusion/Pneumothorax Lung Abscess Empymea Meningitis Viral Pneumonias Viral Pneumonia- influenza viruses Viral sx: cough, severe headache, anorexia, fever, and myalgia Often begins as acute coryza, bronchitis, pleurisy, or GI symptoms Treat symptomatically- Amantadine relieves symptoms Use vaccines if client is at risk Complications: Risk of secondary bacterial pneumonia Pericarditis Endocarditis Pneumocystis Carinii pneumonia Lowly virulent fungal pneumonia Fungal Pneumonia High mortality rate- destroys lung tissues Complications: Pleural Effusion Hypotension and shock Superinfection: Pericarditis, Bacteremia, meningitis Delirium- this is considered a medical emergency Atelectasis- due to mucous plugs (pockets of dead air space) Assessment History of recent respiratory illness- symptoms Presence of chills Description of chest pain Any family illness Any recent antimicrobial drugs Alcohol, tobacco, drug abuse Splinting of the affected side Confusion/Disorientation Shallow respirations/dyspnea Flushed appearance/Anxious Auscultate crackles over affected region and bronchial breathing when consolidation is present Interventions- lots of questions on these Allow client to sit upright for greater lung expansion and more oxygen Administer oxygen per order- low level for client for COPD Obtain sputum culture and sensitivity Encourage fluids to 3-4,000 mL/day if within limits for client’s cardiac reserve- thins the mucous Encourage coughing Humidify air to loosen secretions Employ chest wall percussion- “cupping” and postural drainage- cupping comes first and then have them upside down to drain the mucous Continue to auscultate lung sounds Relieve pleuritic chest pain by semi-Fowler’s position, splinting of chest with pillows Coughing- do not suppress productive cough- only dry hacking nocturnal cough Sedatives, narcotics, and cough suppressants are generally contraindicated for the elderly. These meds suppress cough, gag reflex, and respiratory drive Apply heat to the chest as prescribed Watch for paralytic ileus or abdominal distention from swallowing too much air- NG possible Patient Education Fatigue, weakness, and depression may be prolonged after pneumonia Encourage gradual increase in activities Explain need for follow up exams and x-rays It is wise to stop smoking. Smoking destroys cillial action which is one of the first lines of defense for the lungs Smoking irritates lung tissue which is already irritated by the infection Smoking inhibits the function of lung macrophages which seek out any bacteria that enters the lung and tries to destroy it Take antibiotics as prescribed Any itching or rash, contact physician Other Conditions Care of a client with Pleurisy Inflammation of the pleura Can occur from pneumonia, TB, Pulmonary embolism, URT infections, Pulmonary neoplasms Chest pain-Pleuritic, char, knifelike on inspiration Intercostal tenderness Pleural friction rub- grating or leathery sounds heard on both phases of respiration Evidence of an infection: fever, malaise, increased WBC’s especially with empyema- pus in the linings Interventions for Pleurisy Treat cause of pleurisy like cancer or pneumonia Relieve the pain by auto splint on the affected side, apply prescribed heat and analgesics Watch for pleural effusion which is a collection of fluid in the pleural space Shortness of breath Pain Local decreased excursion of the chest wall Cough absent breath sounds Treatment of Pleural effusion Treat underlying cause Same as pleurisy Thoracentesis- aspiration for fluid removal and relief of dyspnea- chest x-ray post procedure Pleurodesis- production of adhesions between the parietal and visceral pleura by use of tubes and tetracycline for sclerosing agent COPD COPD is a term that refers to a group of conditions characterized by continued increased resistance to expiratory airflow Emphysema Chronic Bronchitis Chronic asthma Excessive secretion of mucous and chronic infection within the airways Increase in size of air spaces as terminal bronchioles with loss of alveolar walls and elastic recoil Distention of the alveoli with mixture of oxygen and carbon dioxide Causes: Cigarette smoking Air pollution Occupational exposure Allergy Autoimmunity Infection Genetic predisposition and aging Pulmonary Emphysema Slowly progressive deterioration of lung function for many years before development of the illness 1 out of 4 wage-earners are disabled due to the disease More common in men Oxygen is inhaled but CO2 is retained Symptoms of Emphysema Dyspnea Cough Sputum expectorant Digital Clubbing Weight loss and anorexia Abnormal lung sounds Barrel shaped chest- increased anterior-posterior diameter Respiratory acidosis- nervous, headaches, confusion Cyanosis Weakness Management of Emphysema Smoking Cessation Bronchodilators Sympathomimetics: albuterol-Alupent-Buterol-Proventyl-protect against bronchospasm Methylxanthines-theophylline-TheoDur- is given orally- don’t give if pulse is over 100 Theoophylline- Breathine- aminophylline- very important in treating- will make jittery, and nervous, elevates pulse- check pulse and do not give if pulse under 100 Antimicrobial agents for infections Steroids for acute exacerbations- Prednisone Chest therapy- cupping and postural drainage IPPB treatments- intermediate positive pressure breathing, nebulizer treatment Low-flow oxygen by nasal cannula Complications of Emphysema Respiratory failure Pneumonia Right sided heart failure called Cor Pulmonale Nursing Interventions for emphysema Eliminate all pulmonary irritants- perfumes, cooking foods, cigarette smoke, etc. Keep client’s room dust free Add moisture- humidifier or vaporizer Control bronchospasm by bronchodilators- watch side effects Monitor lung sounds Do cupping and postural drainage before eating Small frequent meals Teach use of controlled coughing- exhaling through pursed lips or pursed lip breathing, and “huffing” Inhale slowly Keep secretions liquid- avoid dairy products Teach breathing exercises Follow-up care Avoid RTI- most frequent cause of emphysema attack Relaxation exercises- avoid stress Position of comfort Discuss regular exercises like walking Balance activity and sleep Nocturnal oxygen use Understand SOB and fatigue Encourage verbalization of feelings Sexual dysfunction is common Avoid extremely hot/cold temperatures Shower in warm not hot water Obtain influenza and pneumococcal vaccines Care of a Client with Pulmonary Embolism The obstruction of one or more pulmonary arteries by a thrombus originating in the deep veins of the legs Predisposing factors: Stasis; prolonged immobilization Phlebitis Previous heart or lung disease Coagulation disorders Metabolic, endocrine, vascular or collagen disorders Malignancy Advancing age Estrogen therapy including birth control pills Prevention and Health Maintenance of Pulmonary Embolism Be aware of high risk clients- pelvic surgery, immobilization, trauma to the pelvis, obesity, history of emboli, pregnancy, CHF, MI, malignancy, elderly, post-op client Prevent stasis of blood in legs due to position, prolonged sitting or standing Prevent wearing constrictive clothing Encourage early mobility and weight bearing if allowed Elevate legs 15-20 degrees at intervals to increase venous return to the heart Apply TED if ordered Instruct to wiggle toes, move feet, raise and lower legs frequently Don’t let patients legs dangle without support to the back of the legs Sequential Compression Device- SCD if ordered Avoid crossing legs Encourage fluids- avoid hemoconcentration Avoid leaving IV catheter past 3 days Examine client’s legs daily for evidence of thrombosis- Homan’s sign Filters used or umbrellas Signs and Symptoms of Pulmonary Embolism Sudden pleuritic chest pain is the most common Dyspnea- increased shallow respirations Tachypnea Apprehension Sense of impending doom Cyanosis Arrhythmias Syncope Blood tinged sputum/hemoptysis Circulatory collapse- shock Pleural friction rub is heard on lung sounds Presence of venous thrombosis in leg Diagnosis of Pulmonary Embolism Arterial blood gases Radioscopic lung scans Pulmonary angiogram is most definitive CT scan Treatment of Pulmonary Embolism Oxygen IV Dopamine drip- Inotropic agent, for shock Anti- arrhythmic drugs Small doses of morphine Thrombolytic agents-urokinase-streptokinase- and tpa- tissue plasminogen affector Surgical intervention like vena cava filter or prevent migration of emboli Embolectomy Anticoagulation therapy by Heparin (IV) progressing to Warfarin or Coumadin- (PO) Monitor Heparin by PTT- Partial Thromboplastin Time PTT- 30-45 sec. >90 is critical Antidote for Heparin is Protamine Sulfate 1% solution Heparin’s effect unlike that of Warfarin is immediate. Heparin can also be given SC after surgery to prevent leg clots Warfarin or Coumadin is monitored by the PT- prothrombin time or protime Warfarin may take 1-2 weeks to produce therapeutic effect Normal is 11-12.5 seconds Critical value is >20 Goal is 1 ½ times normal Vitamin K: Synkavite is the antidote Newer SC drug called Lovenox- enoxaparin- give SC only to prevent clots postHeparin and Lovenox are given deep SC with a tuberculin syringe Give in the abd at a 90 degree angle Do not aspirate or massage Use ice to numb area before administration Side effects with Anticoagulants Hypersensitivity Increased risk of bleeding from the gums, kidneys, GI tract, petechial on the skin or ecchymosis, brain Fever N/V Edema Care with Anticoagulants Soft bristle toothbrushes Use and electric razor Observation of bleeding Observe for low back pain, melena, urine color Instruction on not taking aspirin, NSAID, or other antiplatelet meds- Plavix Monitor respiratory rate and watch for failure Listen to lung sounds Auscultate heart sounds- listen for splitting of second heart beat Perform stool guaiac test Monitor platelet count for DIC- decrease in the clotting platelet mechanism of the body. All clotting mechanisms will release and there will be a lack of the mechanism, they will start clumping together and make microclots all over the body. Normal platelet count 150,000- 400,000 in Heparin induced DIC they are reduced RBC’s- 45-54 million- less in women Medic alert bracelet Follow up PT’s Avoid sports/activities that injure Lose weight Lung Cancer 14% survival rate 85% caused by smoking The more cigarettes smoked per day, the higher the risk Genetic link not found Diet low in Vitamin A, C, E Antioxidants protect against cell change Small Cell Lung Cancer Small cell lung cancer occurs in 20% of patients Aggressive and spreads bilaterally Both sides affected at time of diagnosis in 75% of patients Bones, Liver, Brain Non small cell lung cancer Adenocarcinoma- most common 40% Squamous cell carcinoma- 30%- grows slower better to resect Large cell carcinoma- 10% Symptoms of Lung Cancer Cough—hidden by chronic smoker cough Blood tinged sputum- hemoptysis Thick and purulent sputum Recurrent RTI’s Dyspnea Hoarseness Chest pain or tightness Dysphagia Head and neck swelling Pleural Effusion Weakness and anemia Weight Loss and anorexia Diagnosis- Lung Cancer Bronchoscopy: NPO past midnight Fiber optic bronchoscopy will enable doctor to view tracheobronchial tree Biopsy by: bronchial washing or brushing cells to analyze Numb throat and spray Valium NPO until gag reflex returns Monitor sputum post procedure for blood Lung Biopsy Needed if tumor on lung periphery Percutaneous fine needle aspiration guided by fluoroscopy or CAT Complications: bleeding; pneumothorax, spread of cancer cells- metastasis Chest X-ray Treatment for Lung Cancer Pneumonectomy- removes whole lung Lobectomy- removes lobe of lung Segmental Wedge Resection- takes a triangular section of the lung out Chemotherapy Radiation Pneumonectomy All post op care previously studied Turn on affected/operative side only for fluid to drain down and not collapse lung to prevent Mediastinal shift Lobectomy- turn either side Wedge resection: turn on unaffected/non operative side Other measures for Lung Cancer Surgery Splint incision for turn cough and deep breath Leg exercises Pain medication Nicotine patch Oxygen administration/patent airway Chemotherapy side effects Emotional support Cancer of the Larynx Permanent Tracheostomy Loss of taste Loss of speech Dealing with emotional aspect Symptoms of Laryngeal Cancer Hoarseness/voice change most common Lump/fullness in throat Tickling in throat Coughing on swallowing Pain radiating to the ear Dyspnea Coughing Smell to breath Care of Client with Larynx Cancer Trach care and suctioning Suctioning will be required every 5 minutes due to large amounts of mucous from the throat and lungs Maintain patent airway and oxygenation Speech Rehab Client teaching regarding trach Client with ARDS Adult Respiratory Distress Syndrome Emergency Causes: Near drowning experience Flu Shock Overdose Head or chest trauma Cancer Radiation Definition of ARDS Lung failure due to a noncardiogenic life threatening event Lung capillaries and the alveoli cell wall membranes become weak and porous Tiny lung blood vessels leak into the alveoli Alveoli fill up with blood Risk Factors for ARDS Cigarette Smoking Chronic Lung Disease Age over 65 but can happen to anyone over the age of 1 Symptoms of ARDS SOB- hypoxemia Tachypnea Cyanosis- skin and fingernails Rapid pulse Fever, chills, muscle aches Headache Dry cough Treatment of ARDS Usually develops 24-48 hours of the injury Get help quickly! Mechanical ventilation- force oxygen into cells by pressure- PEEP Monitor arterial blood gases and O2 sats Monitor I&O Sedation coma for intubation Anasarca my develop- total body edema TPN used for nutrition Respiratory Distress in Children Costal, sternal, Substernal retraction Use of accessory muscles Stridor Pediatric Respiratory Conditions Rhinitis- common cold- viral verses allergic rhinitis Flu- influenza- virus transmitted by airborne droplets Sinusitis- bacterial Complications can be serious: meningitis, brain abscess, ear infections/hearing loss Worse in morning, better in afternoon Pharyngitis: viral verses streptococcal If streptococcal must have Augmentin or Cefazolin if allergies to Penicillin Untreated: Scarlet fever; Rheumatic Fever; or Glomerulonephritis Treatment for Strep Bacterial: antibiotics Fluids, rest, analgesics/antipyretics, humidity Best way to thin secretions in body so that they can be coughed up and out: encourage fluids May need tonsillectomy Watch for increased swallowing=bleeding Croup Acute respiratory distress in a child or infant Nasal flaring Retractions Dyspnea Barking cough/stridor Tongue blade can cause respiratory arrest Croup Care Relieve hypoxia/O2 sats/ oxygen Hold upright- crying makes worse- parents stay Increase humidity- bathroom with hot water relieves laryngeal spasms Croupette- cool air saturated with microdroplets Keep children dry Steroids if no chickenpoxEpinephrine will relax the smooth muscles of the bronchial tree Asthma Chronic inflammatory disorder with bronchial spasms or constriction alternating with relaxation Results in narrowed bronchioles- less oxygen Airways become edematous and infant’s tiny airways will close shut Copious amounts of mucous produced during and after episode Symptoms of asthma Wheezing, abnormal lung sounds SOB Cyanosis Coughing O2 decreased PCO2 increased Perspires Triggers of Asthma RTI’s Cigarette smoking Stress Dust/molds/allergens Treatment of Asthma If child sit up and over overbed table to breathe better Bronchodilators- increased pulse Steroids: Prednisone= Na retention with fluid retention and causes ulcers IPPB with Isuprel or Bronkosol or Alupent Emergency= Epinephrine 1:1000 sc Child= 0.1-02 mL Adult: 0.3-0.5 mL Cystic Fibrosis Manifestations Salty tears, saliva, and sweat Heat prostration- very prone to heat stroke Distended abdomen Rectal prolapse Meconium Ileus Atrophy of thighs and buttocks Sinusitis Chronic cough, cyanosis Dyspnea, wheezing Barrel shaped chest Obstructed pancreas Deficiency of enzymes, poor digestion Large, foul-smelling stools Clubbing of fingers and toes CF Patho Lungs produce a layer of mucous that protects them. Mucous helps keep bacteria on the move Clients with CF have thicker mucous and more mucous Thick, sticky mucous obstructs the airway Lung damage from dead neutrophils’ waste products Inherited recessive gene disease- both parents CF also affects: Pancreas: thick secretions prevent pancreative and liver enzymes from flowing to aid digestion--poor growth, thin, anorexic, muscle wasting Abnormal loss of electrolytes primarily NaCl in sweat due to abnormal chloride movement Bulky foul smelling stools that are frothy because of undigested fat are classic Thick impacted feces may cause rectal prolapse Skin: loss of sodium and chloride in sweat gives salty skin surface--- electrolytes imbalance Infertility: thick cervical mucus hinders sperm Every mucous secreting cell in the body will be affected Meconium ileus in newborns Diagnosis of CF Analyze sweat---sweat test for sodium chloride- 60 meq/L Cor Pulmonale may develop Treatment of CF Oxygen Antibiotics Inhalers Bronchodilators Cupping and PP IPPB Humidity and liquids Pancrelipase- Pancrease (Oral pancreatic preparation)- given with each meal and snack. Give Vitamins A, D, E, K, iron, and zinc supplements Watch for signs of heat stroke and exhaustion which occurs quickly