negative symptoms
advertisement

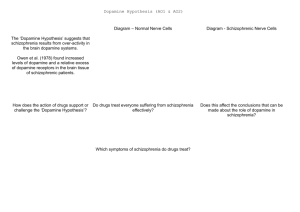
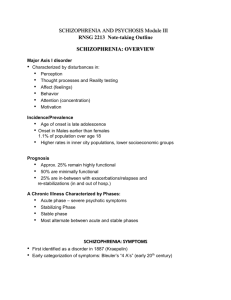
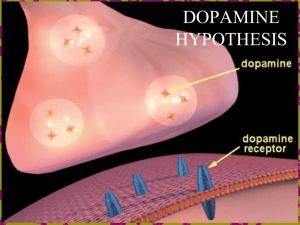
Announcement The following material related to the visual system will not be tested on the December exam: Lecture slides: Lecture 28, slides 15-24 (on- and off-center cells, simple cortical cells, complex cortical cells). Textbook: Bottom half of p. 294; bottom half of p. 300; figure 10.15; bottom half of p. 302 and top half of p. 303; the spatial-frequency filter model, presented on p. 303-305 of the textbook. Guest Lecturer: Naghmeh Shafiei Biopsychology of Psychiatric Disorders Schizophrenia, Affective disorders, & Anxiety disorders Psychiatric disorders • What are Psychiatric disorders (Symptoms)? • What are some causal contributors? • What are some hypothesis about why & how they develop? • What are some treatment options? Outline • Schizophrenia • Symptoms • Epidemiology • Causes • Heredity • Cognitive deficiencies • Neural abnormalities • • • • • • • Cognitive abnormalities in schizophrenia The dopamine hypothesis Problems with typical antipsychotics Problems with the dopamine hypothesis The Glutamate hypothesis Neural Circuitry Implicated in Schizophrenia A new hypothesis Schizophrenia • Schizophrenia • Paranoid Schizophrenic • Disorganized schizophrenic • Catatonic schizophrenic • There are also: • Schizoaffective disorder • Schizophreniform disorder Symptoms • Schizophrenia as defined by DSM IV • Delusions • Incoherence Catatonic • Negative symptom Hallucinations Disorganized or • 6 months duration, psychotic for 1 month • Course: • Continuous • Episodic, with or without residuals • Single episode, partial or full remission Schizophrenia Symptoms • Negative Symptoms: Behavioral deficits • • • • • Social withdrawal Flat affect, Apathy Anhedonia, lack of pleasure Reduced focus and motivation Catatonia Schizophrenia Epidemiology • Onset • Late teenage years-early adulthood • Earlier onset in males (20-28) than in females (26-32) • Rare onset in childhood and late adulthood • Lifetime prevalence of ∼1%. Causes Causes causes • Heredity • Twin studies • Family studies • Adoption Studies Causes causes • These findings indicate • There is a strong genetic component to schizophrenia, but • Altered genes are NOT the only cause of the disease • Genetic component not linked to just one gene, there may be dozens that are altered. • So why some and not others? • Birth complications, Early infections, Autoimmune reactions, Toxins, Traumatic injuries, Stress CausesCausescauses • Alterations throughout development • In utero influence includes Poor nutrition during pregnancy, Premature birth/low birth weight Physical and immune stressors during pregnancy 65 Average number of schizophrenic births • • • 60 55 50 1 2 3 4 5 6 7 8 9 Months after start of flu epidemic 10 Cognitive deficiencies • Cognitive functioning is the #1 predictor of long term outcome (better function= better prognosis) • Seven primary domains of cognition that are affected: • Speed of Processing • Working Memory • Visual Learning/Memory • Social Cognition Attention/Vigilance Verbal Learning/Memory Reasoning/Problem Solving Neural abnormalities • Enlarged Ventricles • Hippocampus: brain region in temporal lobe critical for memory formation. • Some schizophrenics have enlarged lateral ventricles, due to smaller hippocampus and other temporal lobe regions Neural abnormalities • Closer inspection reveals organization of hippocampal neurons is altered in the schizophrenic brain (neural organization occurs during development) Neural abnormalities Neural abnormalities Neural abnormalities Normal Individual Patient with Schizophrenia • Not brain damage per se: changes in the neural organization can disrupt the way brain regions process information Neural abnormalities • Prefrontal Cortex (PFC): frontal lobe region critical for higher order cognition (short term memory, planning, behavioural flexibility, abstract thinking) • Neurons in the PFC of schizophrenics have reduced number of dendrites, which in turn reduces processing power of these cells. Neural abnormalities • Cortical gray matter loss in adolescence in the case of early onset Schizophrenia • No major structural abnormalities in the frontal lobes. Cognitive Abnormalities in Schizophrenia Sort by number Sort by shape Sort by colour Wisconsin Card Sorting Task: A classic PFC task Test behavioural flexibility (ability to change strategies) Cognitive Abnormalities in Schizophrenia • Subjects initially sort cards by one dimension (e.g., number) • Then task switches, subjects must ignore old strategy and switch to new one (e.g., shape) • Damage to PFC impairs switching strategies, patients keep sorting cards by first dimension (keep sorting by number) • Schizophrenics also impaired on this task Cognitive Abnormalities in Schizophrenia • Brain activation studies: schizophrenics and discordant identical twin controls performed Wisconsin Card Sort • Schizophrenics had activation of the PFC at rest; showed no increase when performing task, unlike controls • Other brain regions were activated similarly in both groups • Schizophrenics show a dramatic decrease in PFC function, but not other cortical regions Cognitive Abnormalities in Schizophrenia At Rest During card sorting task Normal Schiz • Hypofrontality (reduced PFC function) is a characteristic negative symptom of schizophrenia Treatments • Most of the dopamine in the brain is produced in small nuclei in the midbrain • 1950s: Chlorpromazine found to be antipsychotic; causes Parkinson’s symptoms in healthy subjects • Brains of Parkinson’s patients found to be depleted of dopamine • 1960s: Drugs that increase dopamine release (e.g.; amphetamine) could induce psychotic symptoms • Chlorpromazine and other antipsychotics found to block dopamine receptors (Typical antipsychotics) • 1970s: Dopamine receptor subtypes discovered; antipsychotic potency of a drug correlated with binding to D2 receptors (not D1) • THUS, The dopamine hypothesis was born: • Schizophrenia is caused by an abnormal increase in dopamine transmission, leading to overstimulation of D2 receptors The Dopamine hypothesisTreatments How are D2 receptors being overstimulated? •More D2 receptors? –Unlikely: Some post mortem studies report D2 receptors in schizophrenic brains, others failed to find this effect –Changes may be due to chronic antipsychotic medication •More dopamine being produced? –Probably not: Schizophrenics do not show differences in dopamine metabolites in CSF •More dopamine being released? –Study: imaging allows for non-invasive measure of dopamine release in human brain –Give amphetamine to schizophrenics or controls –Greater dopamine release in the Nucleus Accumbens (NAcc) of schizophrenics –More dopamine release = more positive symptoms Problems with typical antipsychotics • Dopamine is heavily involved in motor functions. – Long term treatment with antipsychotics (dopamine blockers) can cause movement (a.k.a extrapyramidal) side effects • Tardive dyskinesia occurs in about one third of patients treated with classical antipsychotics – grimacing, tongue protrusion, lip smacking, rapid limb/trunk movements; symptoms continue after discontinuing medication. – Drugs that are more selective for dopamine vs other receptors usually cause the worst side effects • Antipsychotic drugs treat psychosis (delusions, Problems with the DA hypothesis 1.Antipsychotics block dopamine receptors right away, yet drug treatment takes ~2 weeks to reach full effect If schizophrenia is merely an increase in dopamine, drugs should work right away 2.Not all schizophrenic patients respond to drugs that block dopamine receptors If schizophrenia is merely an increase in dopamine, drugs should work for all patients 3.Dopamine blockers can alleviate psychosis, but do not treat negative symptoms. If cognitive deficits are due to an increase in dopamine, these drugs should alleviate the symptoms Problems with the Dopamine Hypothesis • 4) Some drugs that reduce symptoms do not block D2 receptors very well • Example: Clozapine (atypical antipsychotic) • Not as effective at blocking D2 receptors as classical antipsychotics • Less likely to produce motor side effects • Has a much higher affinity to other receptors, like serotonin (5 HT) • Can improve negative symptoms (possibly via 5 HT blockade) – If positive and negative symptoms are merely due to overstimulation of D2 receptors, atypical antipsychotics shouldn’t work very well • Problems: some patients have an adverse blood reaction to clozapine; not all patients can take it safely 10 9 Controls Schizophrenics 8 7 Errors • 5) Drugs that increase dopamine release can improve performance on cognitive tasks • Study: Schizophrenics and controls tested on a working memory task (dependent on PFC function) • Given either placebo or low dose of amphetamine (dose dopamine release, but not psychotic symptoms) • Under placebo, schizophrenics performed worse than controls • Amphetamine, improved performance in schizophrenics, up to control levels 6 5 4 3 2 1 0 Placebo Amphetamine • If schizophrenia is just an increase in dopamine, then why should a drug that increases dopamine release; – 1) not affect psychosis (even at low doses) – 2) improve cognitive functions? The Glutamate hypothesis • Abuse of phencyclidine (PCP, angeldust) or ketamine (Special K) can cause psychotic symptoms and cognitive deficits resembling schizophrenia – Long lasting effects; can persist after drug use has stopped – Can also cause degeneration of PFC neurons • These drugs block NMDA subtype of glutamate receptors – Block the ion channel: glutamate cannot activate receptor • Glutamate hypothesis: Schizophrenia is caused by decreased glutamate transmission – Neurons in PFC/hippocampus use glutamate as a transmitter – Degeneration of these neurons in schizophrenia disrupts their function, less glutamate released in these areas The Glutamate hypothesis Dopamine levels Working memory performance • Rat/primate studies show that repeated PCP: • 1) decreases dopamine release in PFC • 2) causes cognitive deficits on PFCdependent tasks • These effects persist weeks after drug treatment has stopped • Schizophrenics show decrease dopamine activity in PFC • This model encompasses both positive and negative symptoms of the disorder • Recent finding: these drugs are also potent D2 receptor agonists (stimulate the receptors) – Negative symptoms = decreased glutamate/dopamine transmission in PFC – Positive symptoms = increased D2 receptor stimulation in NAcc Neural Circuitry Implicated in Schizophrenia PFC projects back to VTA Prefrontal cortex Cognitive functions impaired in schizophrenia (decreased glutamate, dopamine?) Dopamine (VTA) VTA sends dopamine input to PFC and accumbens Nucleus Accumbens Increased dopamine release in schizophrenia; related to psychotic symptoms • This connectivity suggests that prefrontal cortex can modulate dopamine release in the NAcc A New Hypothesis 2 PFC 1 Dopamine (VTA) 3 Nucleus Accumbens 1) Decreased PFC dopamine/glutamate reduces activity, (negative symptoms) 2) Decreased PFC activation reduces inhibition of dopamine system 3) Release from this inhibition leads to increased dopamine transmission in NAcc (positive symptoms)