Physiology of venous and lymph system
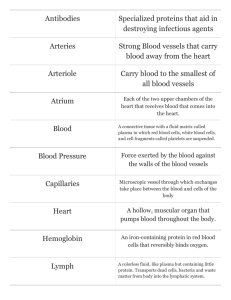
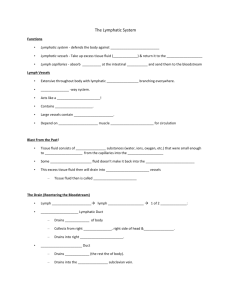
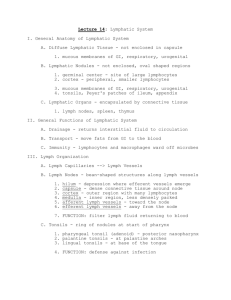
advertisement

PHYSIOLOGY OF VENOUS AND LYMPHATIC SYSTEM. Blood flow in veins Blood flows through the blood vessels, including the veins, primarily, because of the pumping action of the heart, although venous flow is aided by the heartbeat, the increase in the negative intrathoracic pressure during each inspiration, and contractions of skeletal muscles that compress the veins (muscle pump). Morpho-functional properties of venous system Veins are the vessels, which are carry out blood from organs, tissues to heart in right atrium. Only pulmonary vein carry out blood from lungs in left atrium. There are superficial (skin) and deep veins. They are very stretching and have a low elasticity. Valves are present in veins. Plexus venosus are depo of blood. Blood moving in veins under gravity. Mechanism of regulation Difference of pressure in venous system is a cause of blood moving. From the place of high pressure blood moving to the place of low pressure. Negative pressure in chest is a cause of blood moving. Contraction of skeletal muscles, diaphragm pump, peristaltic movement of veins walls are the causes of moving. Venous pressure Venous pressure is pressure of blood, which are circulated in veins. Venous pressure in healthy person is from 50 to 100 mm H2O. Increase of venous pressure in physiological condition may be in the action of physical activity. Determine of venous pressure is called phlebotonometry and give for doctors information about activity of right atrium. Speed of blood stream Speed of vein blood stream depend on diameter of vessels. In venuls speed of blood moving is lower. In veins of middle diameter it 7-14 cm/s, in big veins the speed is near 20 cm/s. In big veins speed of blood moving depend on breathing and heartbeat. Venous pulse Venous pulse is a moving of walls of big veins, which are depend on heartbeat. The cause of it stop of blood flow from vein to heart during atrium systole. At these time pressure in it increase. Methods of investigation of venous pulse are phlebography. Transport of substances through capillary membrane Substances are transported through capillary membrane are lipid soluble as O2 or CO2 and water-soluble as ions or glucose. Substances of molecule size more than 6-7 nm cannot diffuse through intra-endothelial pores. The greater the concentration difference of a given substance on two sides of capillary membrane, the greater will bi net rate of diffusion. Forces that determine fluid movement through capillary membrane are capillary pressure, interstitial fluid pressure, plasma colloid osmotic pressure and interstitial fluid colloid osmotic pressure. At arterial end of capillary pressure is higher than interstitial fluid pressure, which causes filtration. At venous end of capillary plasma colloid osmotic pressure is lower than interstitial pressure, which cause reabsorbtion. Lymph and lymphatic circulation Lymph vessels are present in all tissues, except bones, nervous and superficial layers of skin. Lymphatic capillaries Lymphatic capillaries begin as one side closed capacities, which are drained by smallest lymphatic vessels. Lymphatic capillaries have valves, which prevent opposite movement of lymph. Connective tissue fibers fix outer surface of lymphatic capillary to surrounding intracellular substance and keep it voluminous shape. Pressure of lymph inside the capillary is lower than in intracellular space, which helps to lymph flow. Capillary wall has basal membrane and one layer of endotheliocytes. Morpho-functional properties of lymphatic system Lymph system has capillaries, vessels, where present valves, lymphatic nodes. In lymphatic nodes are lymphopoiesis, depo of lymph, their function is barrier-filter. Lymph flow in vein system through the chest lymph ductus. Functions of lymph: 1. support of constant level of volume and components of tissue fluid; 2. transport of nutritive substances from digestive tract in venous system; 3. barrier-filter function. 4. take place in immunology reactions. Composition and properties of lymph Lymph is tissue fluid that enters the lymphatic vessels. It drains into the venous blood via the thoracic and right lymphatic ducts. It contains clotting factors and clots on standing in vitro. Its protein content is generally lower than that of plasma but varies with the region from which the lymph drains. It should be noted that, in most locations, interstitial fluid is not protein-free; it contains proteins that traverse capillary walls and return to the blood via lymph. Water-insoluble fats are absorbed from the intestine into the lymphatic vessels, and the lymph in the thoracic duct after a meal is milky because of its high fat content Lymphocytes enter the circulation principally through the lymphatic vessels, and there are appreciable numbers of lymphocytes in thoracic duct lymph. Time of clotting – 10-15 minutes. There are 3 kinds of lymph: peripheral, transport, central. The difference between them in cell quantity level. Production of lymph Fluid efflux normally exceeds influx across the capillary walls, but the extra fluid enters the lymph and drains through them back into the blood. This keeps the interstitial fluid pressure from rising and promotes the turnover of tissue fluid. The normal 24-hour lymph flow is 2-4 L. Appreciable quantities of protein enter the interstitial fluid in the liver and intestine, and smaller quantities enter from the blood in other tissues. The walls of the lymphatic are permeable to macromolecules, and the proteins are returned to the bloodstream via the lymphatic. The amount of protein returned in this fashion in 1 day is equal to 25-50 % of the total circulating plasma protein. In the kidneys, formation of a maximally concentrated urine depends upon an intact lymphatic circulation; removal of reabsorbed water from the medullar pyramids is essential for the efficient operation of the countercurrent mechanism and water enters the vasa recta only if an appreciable osmotic gradient is maintained between the medullar interstitial and the vasa recta blood by drainage of protein-containing interstitial fluid into the renal lymphatic. Some large enzymes – notably histaminases and lipase – may reach the circulation largely or even exclusively via the lymphatic vessels after their secretion from cells into the interstitial fluid. The transport of absorbed long-chain fatty, for example, cholesterol from the intestine via the lymphatic vessels. Mechanism of lymph flow Lymph flow is due to movements of skeletal muscle, the negative intrathoracic pressure during inspiration, the suction effect of high velocity flow of blood in the veins in which the lymphatic vessels terminate, and rhythmic contractions of the walls of the large lymph ducts. Since lymph vessels have valves that prevent backflow, skeletal muscle contractions push the lymph toward the heart. Pulsations of arteries near lymphatic vessels may have a similar effect. However, the contractions of the walls of the lymphatic ducts are important, and the rate of these contractions increases in direct proportion to the volume of lymph in the vessels. There is evidence that the contractions are the principal factor propelling the lymph. Blood supply of the spleen There are 1,5-2 % of volume circulation in the human spleen. In our organism spleen has a small amount of smooth muscle in the capsule and in pulpe. Activity in the sympathetic nerves caused vasocontriction. Histamine, adenosine caused vasodilatation, adrenaline, serotonine, prostaglandine – vasocontriction. Lympathatic system The lymphatic system has three primary functions. First of all, it returns excess interstitial fluid to the blood. Of the fluid that leaves the capillary, about 90 percent is returned. The 10 percent that does not return becomes part of the interstitial fluid that surrounds the tissue cells. Small protein molecules may "leak" through the capillary wall and increase the osmotic pressure of the interstitial fluid. This further inhibits the return of fluid into the capillaries, and fluid tends to accumulate in the tissue spaces. If this continues, blood volume and blood pressure decrease significantly and the volume of tissue fluid increases, which results in edema (swelling). Lymph capillaries pick up the excess interstitial fluid and proteins and return them to the venous blood. After the fluid enters the lymph capillaries, it is called lymph. The second function of the lymphatic system is the absorption of fats and fat-soluble vitamins from the digestive system and the subsequent transport of these substances to the venous circulation. The mucosa that lines the small intestine is covered with fingerlike projections called villi. There are blood capillaries and special lymph capillaries, called lacteals, in the center of each villus. The blood capillaries absorb most nutrients, but the fats and fat-soluble vitamins are absorbed by the lacteals. The lymph in the lacteals has a milky appearance due to its high fat content and is called chyle. The third and probably most well known function of the lymphatic system is defense against invading microorganisms and disease. Lymph nodes and other lymphatic organs filter the lymph to remove microorganisms and other foreign particles. Lymphatic organs contain lymphocytes that destroy invading organisms. The lymphatic system consists of a fluid (lymph), vessels that transport the lymph, and organs that contain lymphoid tissue. Lymph Lymph is a fluid similar in composition to blood plasma. It is derived from blood plasma as fluids pass through capillary walls at the arterial end. As the interstitial fluid begins to accumulate, it is picked up and removed by tiny lymphatic vessels and returned to the blood. As soon as the interstitial fluid enters the lymph capillaries, it is called lymph. Returning the fluid to the blood prevents edema and helps to maintain normal blood volume and pressure. Lymphatic Vessels Lymphatic vessels, unlike blood vessels, only carry fluid away from the tissues. The smallest lymphatic vessels are the lymph capillaries, which begin in the tissue spaces as blind-ended sacs. Lymph capillaries are found in all regions of the body except the bone marrow, central nervous system, and tissues, such as the epidermis, that lack blood vessels. The wall of the lymph capillary is composed of endothelium in which the simple squamous cells overlap to form a simple one-way valve. This arrangement permits fluid to enter the capillary but prevents lymph from leaving the vessel. The microscopic lymph capillaries merge to form lymphatic vessels. Small lymphatic vessels join to form larger tributaries, called lymphatic trunks, which drain large regions. Lymphatic trunks merge until the lymph enters the two lymphatic ducts. The right lymphatic duct drains lymph from the upper right quadrant of the body. The thoracic duct drains all the rest. Like veins, the lymphatic tributaries have thin walls and have valves to prevent backflow of blood. There is no pump in the lymphatic system like the heart in the cardiovascular system. The pressure gradients to move lymph through the vessels come from the skeletal muscle action, respiratory movement, and contraction of smooth muscle in vessel walls. Lymphatic Organs Lymphatic organs are characterized by clusters of lymphocytes and other cells, such as macrophages, enmeshed in a framework of short, branching connective tissue fibers. The lymphocytes originate in the red bone marrow with other types of blood cells and are carried in the blood from the bone marrow to the lymphatic organs. When the body is exposed to microorganisms and other foreign substances, the lymphocytes proliferate within the lymphatic organs and are sent in the blood to the site of the invasion. This is part of the immune response that attempts to destroy the invading agent. The four types of lymphatic organs are described below. Lymph Nodes Lymph nodes are small bean-shaped structures that are usually less than 2.5 cm in length. They are widely distributed throughout the body along the lymphatic pathways where they filter the lymph before it is returned to the blood. Lymph nodes are not present in the central nervous system. There are three superficial regions on each side of the body where lymph nodes tend to cluster. These areas are the inguinal nodes in the groin, the axillary nodes in the armpit, and the cervical nodes in the neck. The typical lymph node is surrounded by a connective tissue capsule and divided into compartments called lymph nodules. The lymph nodules are dense masses of lymphocytes and macrophages and are separated by spaces called lymph sinuses. Several afferent lymphatic vessels, which carry lymph into the node, enter the node on the convex side. The lymph moves through the lymph sinuses and enters an efferent lymphatic vessel, which carries the lymph away from the node. Because there are more afferent vessels than efferent vessels, the passage of lymph through the sinuses is slowed down, which allow time for the cleansing process. The efferent vessel leaves the node at an indented region called the hilum. Tonsils Tonsils are clusters of lymphatic tissue just under the mucous membranes that line the nose, mouth, and throat (pharynx). There are three groups of tonsils. The pharyngeal tonsils are located near the opening of the nasal cavity into the pharynx. When these tonsils become enlarged they may interfere with breathing and are called adenoids. The palatine tonsils are the ones that are located near the opening of the oral cavity into the pharynx. Lingual tonsils are located on the posterior surface of the tongue, which also places them near the opening of the oral cavity into the pharynx. Lymphocytes and macrophages in the tonsils provide protection against harmful substances and pathogens that may enter the body through the nose or mouth. Spleen The spleen is located in the upper left abdominal cavity, just beneath the diaphragm, and posterior to the stomach. It is similar to a lymph node in shape and structure but it is much larger. The spleen is the largest lymphatic organ in the body. Surrounded by a connective tissue capsule, which extends inward to divide the organ into lobules, the spleen consists of two types of tissue called white pulp and red pulp. The white pulp is lymphatic tissue consisting mainly of lymphocytes around arteries. The red pulp consists of venous sinuses filled with blood and cords of lymphatic cells, such as lymphocytes and macrophages. Blood enters the spleen through the splenic artery, moves through the sinuses where it is filtered, then leaves through the splenic vein. The spleen filters blood in much the way that the lymph nodes filter lymph. Lymphocytes in the spleen react to pathogens in the blood and attempt to destroy them. Macrophages then engulf the resulting debris, the damaged cells, and the other large particles. The spleen, along with the liver, removes old and damaged erythrocytes from the circulating blood. Like other lymphatic tissue, it produces lymphocytes, especially in response to invading pathogens. The sinuses in the spleen are a reservoir for blood. In emergencies such as hemorrhage, smooth muscle in the vessel walls and in the capsule o Thymus The thymus is a soft organ with two lobes that is located anterior to the ascending aorta and posterior to the sternum. It is relatively large in infants and children but after puberty it begins to decrease in size so that in older adults it is quite small. The primary function of the thymus is the processing and maturation of special lymphocytes called T-lymphocytes or T-cells. While in the thymus, the lymphocytes do not respond to pathogens and foreign agents. After the lymphocytes have matured, they enter the blood and go to other lymphatic organs where they help provide defense against disease. The thymus also produces a hormone, thymosin, which stimulates the maturation of lymphocytes in other lymphatic organs. THANCK YOU!