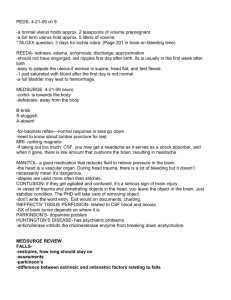
CSF dynamics - Rackcdn.com
advertisement

CSF flow imaging in Chiari 1 malformation Wende Gibbs, MD, Department of Neuroradiology Gabriel Zada, MD, Department of Neurosurgery John Liu, MD, Department of Neurosurgery Patrick Hsieh, MD, Department of Neurosurgery Meng Law, MD, MBBS, Department of Neuroradiology University of Southern California, Keck School of Medicine Control # 1775 eEdE-227 Disclosures Wende Gibbs: none Gabriel Zada: none John Liu: none Patrick Hsieh: none Meng Law: Toshiba Grant Speakers Bureau; Bracco speaker and consultant; Guerbet Medical Advisory Board; Prism Stock; Fuji speaker and consultant Purpose Chiari 1 malformation (CM1) has traditionally been defined by morphologic criteria: cerebellar tonsil herniation 3-6mm below the foramen magnum It is increasingly clear that CM1 is a complex disorder resulting from not only abnormal anatomy, but disordered CSF flow This exhibit will review static and dynamic imaging tools applied to the study of CM1, including new techniques that may improve diagnostic accuracy, patient management and surgical outcome Approach Review theories of pathogenesis of CM1, focusing on the interplay of anatomy and CSF flow dynamics Describe established and recently developed neuroimaging tools used to study CM1: traditional MRI sequences and dynamic techniques including phase contrast MR and Time-spatial labeling inversion pulse technique (Time-SLIP) Demonstrate the utility of Time-SLIP in providing a rapid, individualized assessment of CSF flow before and after surgical treatment Introduction CM1 has historically been described as a change in hindbrain morphology characterized by cerebellar tonsil herniation 3-6mm* below the foramen magnum on sagittal MRI or CT images1-3 However, 30 - 50% of individuals with tonsillar herniation greater than 5mm are asymptomatic4 In those individuals with symptoms, the degree of herniation does not correlate well with symptom severity5 Further, a subset of patients with CM1 symptoms have no tonsillar herniation, suggesting abnormal morphology alone cannot explain CM1 symptomatology6 *The degree of herniation is not universally agreed upon, and depends upon age Introduction Both abnormal anatomy and aberrant CSF flow dynamics contribute to the pathophysiology of CM1 Anatomy/Morphology Posterior fossa anatomy Tonsillar herniation Spinal canal geometry CSF dynamics Complex CSF flow patterns Resistance to flow Abnormal flow velocity Pressure gradients Craniospinal compliance Pathology/Symptoms Syrinx Suboccipital headache Motor or sensory dysfunction Fatigue Pain Introduction Suboccipital decompressive surgery is a standard treatment for CM1 35-45% of patients have minimal or no relief years after surgery7,8 The search for a noninvasive method of selecting patients with CM1 symptoms who will benefit from surgical intervention is an active area of research across many fields CM1 Imaging The observation of cerebellar tonsillar ectopia in the absence of syrinx, hydrocephalus, or suggestive signs and symptoms has uncertain clinical significance When signs and symptoms are present, neuroimaging is vital to diagnosis and management Symptoms Headache (typically suboccipital) Neck, back, face pain “Cape” pain: neck, upper back, shoulders Nonradicular limb pain Weakness Dizziness Vertigo Slurred speech Syncope Difficulty swallowing Tinnitus Signs Cranial nerve: Dysphagia Dysarthria Hoarseness Cough Nystagmus Cerebellar Ataxia Dysmetria Brainstem Nystagmus Sleep apnea Sensorineural hearing loss Hypertension Sinus bradycardia/tachy cardia Syncope Spinal cord Hyperactive reflexes Babinski, Hoffman reflex Spastic gait Urinary incontinence, frequency Extremity weakness CM1 Imaging Routine imaging sequences are obtained to evaluate for hydrocephalus, syrinx, or other craniocervical junction (CCJ) pathology The midline sagittal image is used to quantify cerebellar tonsillar ectopia in relation to a line connecting the basion and opisthion (McRae’s line, foramen magnum) CM1 Imaging: Classification Chiari 0: Tonsils descend 3mm or less below the foramen magnum Syrinx +/- crowding at foramen magnum Chiari 1: Greater than 5mm tonsillar descent in age >15 year Greater than 6mm tonsillar descent in age < 15 years 3-5 mm is borderline, and abnormal if syrinx or symptoms 4th ventricle remains in normal position Chiari 1.5: Herniation of tonsils Elongation and displacement of 4th ventricle and brainstem Chiari 0 and Chiari 1.5 are controversial classifications CM1 Imaging Static features of CM1 - anatomy and morphology – are studied with traditional MRI and CT sequences Degree of tonsillar herniation Tonsillar shape Posterior fossa volume Posterior fossa crowdedness Linear Posterior Fossa Measures: Clivus Supraocciut Twining line McRae Line Dynamic aspects of CM1 are evaluated with CSF flow techniques and computational fluid dynamic simulations CSF velocity CSF stroke volume Tonsil and cord movement Pressure Resistance to flow Craniospinal compliance CM1 Imaging: Morphology The morphologic abnormality in CM1 is diverse In general, CM1 is characterized by: Pointed configuration of the tonsils More vertically oriented cerebellar folia Crowded foramen magnum Narrowed retrocerebellar and premedullary subarachnoid space Lower limits of normal or small posterior fossa Short clivus Inferior elongation of the 4th ventricle with mildly low-lying nucleus gracilis (the demarcation of obex and central canal) 40-80% of symptomatic CM1 have a syrinx4 CM1 Imaging: Morphology Posterior cranial fossa (PCF) volumetry is a potential predictor of surgical outcome9,10 Alpern et. al. studied 20 morphologic and physiologic measures, of which 10 were found to discriminate CM1 from healthy controls better than tonsillar herniation alone The three parameters that best characerized CM1: Cord displacement Posterior cranial fossa crowdedness Normalized posterior cranial fossa volume Using these three parameters, 37 healthy subjects and 35/36 CM1 subjects were correctly classified10 CM1 Imaging: Morphology Complex CMI (cCMI) has recently been described in the neurosurgical literature as a CMI variant with more severe clinical phenotype Recognition by the radiologist is useful as cCMI may require more extensive or repeat neurosurgical procedures Moore and Moore evaluated a number of morphologic measures and found that obex level was the most important differentiating factor between CMI and cCMI11 Inferior herniation of the obex below the foramen magnum (FM) and a prominent dorsal bump was observed in all patients with cCMI in their study Typical CMI is characterized by obex above or at the FM Complex CMI: The obex lies just below the FM (arrow). CM1 Imaging: Dynamic CSF dynamics in the cranial and spinal subarachnoid space may be equally important to morphology in the pathophysiology of CM1 CSF velocity, resistance to flow, pressure, and craniospinal compliance cannot be measured with static MR techniques Dynamic evaluation of CSF flow has primarily been studied with 2D phase contrast MRI New techniques developed to study flow include 4D PC MRI and Time inversion recovery pulse (TimeSLIP) Morphology Abnormal morphology of cerebellar tonsils at the FM: -crowding of neural structures -narrowed subarachnoid space Obstruction of CSF pulsations Cranial arterial driving pressure forces same volume of CSF against obstruction Increased pressure: may further displace or damage neural structures Hydrodynamics Increased pressure gradient Elevated CSF velocity Altered craniospinal compliance Increased resistance to CSF flow Increased pressure: over time may alter neural elasticity, permeability, water content Surgical decompression alleviates crowding, results in decreased peak CSF velocity, and alters craniocervical CSF compliance CM1 Imaging: Phase Contrast 2D PC MRI in axial and/or sagittal orientation has been used to quantitatively and qualitatively evaluate dynamic CSF features such as: Direction of flow Peak CSF velocity Pulse wave velocity in the subarachnoid space Relative timing of CSF and arterial pulsations Before PC MR images are acquired, maximum CSF velocity must be anticipated in order to set the Venc (velocity encoding) To optimize signal, CSF velocity should be the same or slightly below the venc Velocities above the Venc produce aliasing artifact Velocities significantly below the Venc have weak signal CM1 Imaging: Phase Contrast Magnitude and phase images provide information about anatomy and velocity The phase image, reflecting spin phase shifts, is the most sensitive to flow Quantitative information is acquired with images in the axial plane with through-plane velocity encoding in the craniocaudal direction Qualitative features of flow are observed in the sagittal plane with in-plane velocity encoding Peripheral cardiac gating allows for collection of 12-24 phases during the repetition interval, depending on HR By convention, bright signal reflects caudal motion during systole and dark signal represents cranial motion during diastole CM1 Imaging: Phase Contrast Phase images in sagittal orientation in cine mode “White” flow is moving caudally during systole “Black” flow is moving cranially during diastole In this patient with CMI, there is craniocaudal flow ventral to the brainstem and upper cervical cord Craniocaudal flow dorsal to the tonsils and cord is minimal. Click to play cine clip. CM1 Imaging: Phase Contrast The majority of studies utilizing 2D PC MRI show that CM1 is characterized by elevated peak CSF flow velocity at the foramen magnum, and that peak velocity decreases after decompression However, there is not an established correlation between change in velocity and the degree of clinical improvement CM1 is characterized by inhomogeneous flow patterns and simultaneous bidirectional flow: important findings confirmed in subsequent studies using different techniques, including 4D PC MRI and computation flow models5,12,13 CM1 Imaging: Phase Contrast McGirt et al. found that pediatric CM1 patients with normal CSF flow at the FM as assessed by PC MR were 4.8-fold more likely to experience symptom recurrence following surgery regardless of the degree of tonsillar herniation or presence of syrinx8 Abnormal ventral and dorsal flow was associated with a 2.6-fold reduction in risk of symptom recurrence after surgery These findings support the role of inhomogeneous flow patterns in CM1 pathophysiology CM1 Imaging: Phase Contrast Time-resolved three directional velocity encoded phase contrast MRI (4D PC MRI) is a recent advance that can better assess the three dimensional complexities of the CSF flow field Using 4D PC MRI, Bunck et al. showed that in CM1, the anterior subarachnoid space (SAS) is markedly narrowed, with CSF flow diversion to the anterolateral SAS This results in flow jets with elevated velocities and flow vortices14 A B Coronal 4D PC MRI images in control (A) and CM1 (B). Compare uniform, homogeneous flow in A, with lateral flow diversion and left sided flow jet in B. Bunck et al, Eur Radiology (2012) 22:1860-1870. CM1 Imaging: Phase Contrast Peak CSF velocities were significantly greater at the craniocervical junction in CM1 patients than in controls, a finding in most, but not all prior studies using the 2D PC MR technique The volumetric measurement facilitated by the 4D technique demonstrated variability among patients as to the level where peak systolic flow was found Inconsistent results in prior studies may relate to the inability of the 2D technique to capture the correct level for peak flow measurement CM1 Imaging: Time-SLIP Another recently developed MR technique applied to the study of CSF flow dynamics is Time-spatial labeling inversion pulse (Time-SLIP) Time-SLIP is based upon the arterial spin labeling concept In this case, instead of flowing blood, CSF is used as an endogenous tracer Advantages over phase contrast include: Superior anatomic detail Shorter acquisition time Improved evaluation of non periodic or turbulent flow CM1 Imaging: Time-SLIP First the background signal is suppressed with a non selective inversion recovery pulse This is followed by a second, spatially selective pulse perpendicular to the direction of flow When images are acquired, the labeled CSF flows into regions of suppressed background with high conspicuity CSF bulk flow can be observed for up to 5 seconds before contrast between tagged and non tagged CSF is lost Time-SLIP A nonselective IR pulse is applied, inverting all signal in the field of view A second, spatially selective inversion pulse is applied to the region of interest After a short period of time, tagged CSF is seen moving into the nontagged background (red arrow) CM1 Imaging: Time-SLIP A B Time-SLIP in CM1 after surgical decompression. The initial image (A) shows the location of the selective pulse (gold lines). Tagged CSF is bright in this slice. All other CSF is suppressed (dark). After several seconds (B) tagged CSF is seen above and below the slice (gold lines), ventral to the brainstem and cord and dorsal to the cerebellum and cord (orange arrows). *Note the exquisite anatomic detail of the images allowing precise localization of CSF flow, a significant advantage over PC MR images. CM1 imaging: Time-SLIP In this cine clip, we watch the movement of CSF over 5 seconds. Gold lines mark the selective pulse with tagged (bright) CSF Notice the movement of CSF above and below the slice with time We observe features of flow not possible by any other technique: CSF moves from the 4th ventricle superiorly into the aqueduct Turbulent flow is seen in the 4th ventricle (moving dark lines in the midst of bright CSF) CSF moves within the cervical syrinx At the end of 5 seconds, contrast between Click to play cine clip. tagged and untagged CSF is lost CM1 Imaging: Time-SLIP Click to play cine clip. 2D Phase Contrast Click to play cine clip. Time-SLIP 2D PC demonstrates the presence and direction of flow. Time-SLIP allows better visualization of location of flow, as well as periodic and turbulent flow. Case 1: 35 year-old man with 2 years of worsening headache, facial pain, and developing slurred speech. MRI demonstrated tonsillar herniation 16mm below the foramen magnum. After decompression with C1 and partial C2 laminectomies and duraplasty, the patient had marked improvement of his headaches and resolution of his facial pain. A. Initial imaging. Sagittal T1-W image shows ectopic, pointed cerebellar tonsils and crowding at the foramen magnum (FM). A B B. The preoperative Time-SLIP image demonstrates flow ventral the cervical cord (blue arrow). No flow is seen dorsal to the cord below the FM (gold arrow). Yellow lines indicate the tagged slice. All bright CSF above and below the lines has flowed from the tagged slice. C. Post decompression sagittal T2-W image reveals relief of crowding at the FM. More CSF is seen dorsal and inferior to the tonsils. A small amount of fluid is seen posterior to the duraplasty. C D D. Post operative Time-SLIP image again shows CSF flow ventral to cervical cord (blue arrow). There is now flow dorsal to the cord at this level (gold arrow). Case 2: 43-year-old man with 10 year history of upper and lower extremity weakness and numbness, ataxia, increasing difficulty with fine motor control. Click to play cine clip. A The pre-operative Time-SLIP image demonstrates flow ventral to the cord, but only trace flow dorsal to the cord at the tagged level (level marked by gold dots). A small amount of flow is also seen within the syrinx. Click to play cine clip. B The post-decompression study reveals increased flow dorsal to the cord. Craniocaudal flow within the syrinx has also increased. Interestingly, there is a small amount of cranial flow of fluid within the pseudomeningocele. This may relate to respiration. The high intrinsic signal to noise and temporal resolution of Time-SLIP in comparison to 2D PC MRI allows visualization of CSF movement in response to respiration. Respiratory motion may have a greater effect on CSF flow than cardiac pulsation.15 Case 3: 58-year-old man with complicated history of cervical stenosis with myelopathy post C6-T1 laminectomy and fusion one year ago. Increasing difficulty with gait, balance, and left leg weakness prompted imaging. He was found to have an increase in his preexisting tonsillar ectopia. He underwent posterior fossa decompression, C1 laminectomy, and duraplasty. A 5/2014. The preoperative image shows crowding at the FM, increased from prior studies. The focus of abnormal T2 signal in the cord at C7/T1 reflects myelomalacia. The post decompression image shows relief of crowding. There is a large pseudomeningocele. B Click to play cine clip. C Click to play cine clip. D 8/2014 and 12/2014. The patient had only partial improvement in symptoms. Time-SLIP shows that there is no flow dorsally at the FM. The brisk ventral flow is already apparent on the first image. 4 months later, the pseudomeningocele is noted to be larger. There is no change in CSF flow pattern. There is no cranial flow in the fourth ventricle, an abnormal finding. Case 4. 49-year-old woman with history of suboccipital headaches. Click to play cine clip. Note the short clivus, small posterior fossa, and superiorly oriented straight sinus, typical of CM1. Crowding at the FM is minimal but there is a large cervical syrinx (Chiari 0?) Click to play cine clip. Note the change in shape of the syrinx in relation to the flow in the ventral and dorsal SAS at that level. No flow is seen dorsally at the FM. Note the cranially-directed flow through the aquaduct into the third ventricle, a normal finding. Selective tagging pulses can be performed at multiple levels and in different orientations, as long as the slice is perpendicular to the flow direction of interest. A coronal orientation can evaluate flow between the lateral and third ventricles. Time-SLIP Investigators are currently devising methods to quantify flow velocity on Time-SLIP16 PC MR and Time-SLIP provide complementary information for the characterization of pathologies with aberrant CSF flow dynamics CSF dynamics visualized with Time-SLIP differ from classic CSF circulation theories, and the development of this method has advanced knowledge of CSF physiology A better understanding of CSF dynamics in health and disease may lead to increased diagnostic accuracy and better patient selection for surgical interventions Summary Historically and currently, neuroimaging is vital to diagnosis and management of CM1 The search for a noninvasive method of selecting patients with CM1 symptoms who will benefit from surgical intervention is an active area of research across many fields Emerging techniques such as 4D PC MRI and TimeSLIP are providing unique insights into CSF flow dynamics in CM1 and other pathologies resulting from disordered CSF flow dynamics References 1. Barkovich AJ, Wippold FJ, Sherman JL, Citrin CM. Significance of cerebellar tonsillar position on MR. AJNR Am J Neuroradiol. 1986;7(5):795-9. 2. Elster AD, Chen MY. Chiari I malformations: clinical and radiologic reappraisal. Radiology. 1992;183(2):347-53. 3. Milhorat TH, Chou MW, Trinidad EM, et al. Chiari I malformation redefined: clinical and radiographic findings for 364 symptomatic patients. Neurosurgery. 1999;44(5):1005-17. 4. Osborn AG. Osborn's Brain, Imaging, Pathology, and Anatomy. Lippincott Williams & Wilkins; 2012. 5. Iskandar BJ, Quigley M, Haughton VM. Foramen magnum cerebrospinal fluid flow characteristics in children with Chiari I malformation before and after craniocervical decompression. J Neurosurg. 2004;101(2 Suppl):169-78. 6. Sekula RF, Jannetta PJ, Casey KF, Marchan EM, Sekula LK, Mccrady CS. Dimensions of the posterior fossa in patients symptomatic for Chiari I malformation but without cerebellar tonsillar descent. Cerebrospinal Fluid Res. 2005;2:11. 7. Aliaga L, Hekman KE, Yassari R, et al. A novel scoring system for assessing Chiari malformation type I treatment outcomes. Neurosurgery. 2012;70(3):656-64. 8. Mcgirt MJ, Nimjee SM, Fuchs HE, George TM. Relationship of cine phase-contrast magnetic resonance imaging with outcome after decompression for Chiari I malformations. Neurosurgery. 2006;59(1):140-6. 9. Badie B, Mendoza D, Batzdorf U. Posterior fossa volume and response to suboccipital decompression in patients with Chiari I malformation. Neurosurgery. 1995;37(2):214-8. 10. Alperin N, Loftus JR, Oliu CJ, et al. Magnetic resonance imaging measures of posterior cranial fossa morphology and cerebrospinal fluid physiology in Chiari malformation type I. Neurosurgery. 2014;75(5):515-22. 11. Moore HE, Moore KR. Magnetic resonance imaging features of complex Chiari malformation variant of Chiari 1 malformation. Pediatr Radiol. 2014;44(11):1403-11. 12. Haughton VM, Korosec FR, Medow JE, Dolar MT, Iskandar BJ. Peak systolic and diastolic CSF velocity in the foramen magnum in adult patients with Chiari I malformations and in normal control participants. AJNR Am J Neuroradiol. 2003;24(2):169-76. 13. Haughton V, Mardal KA. Spinal fluid biomechanics and imaging: an update for neuroradiologists. AJNR Am J Neuroradiol. 2014;35(10):1864-9. 14. Bunck AC, Kroeger JR, Juettner A, et al. Magnetic resonance 4D flow analysis of cerebrospinal fluid dynamics in Chiari I malformation with and without syringomyelia. Eur Radiol. 2012;22(9):1860-70. 15. Yamada S, Miyazaki M, Yamashita Y, et al. Influence of respiration on cerebrospinal fluid movement using magnetic resonance spin labeling. Fluids Barriers CNS. 2013;10:36. 16. Shiodera T, Nitta S, Takeguchi T, et al. Automated flow quantification for spin labeling MR imaging. MAGMA. 2014;27(5):425-33.