Gastro03-RvwGIPhysioPt1
advertisement

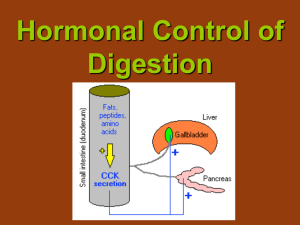
Gastrointestinal2 #03 Monday, February 23, 2004 10:00am Prof: Dr. Gwirtz Scribe: Brandon Zinn Page 1 of 10 Review of GI Physiology, Part 1 Note: This is the first hour of Dr. Gwirtz’s 2-hour review of normal GI physiology (no pathology), and includes powerpoint slides 1-27. The next hour covers slides 28-75. There is no new material presented during this review that wasn’t presented last year. During this hour, her powerpoints in class (but not the slides online) included a table from last year she said is important. Be sure to download this table from the schedule on the website (the link is right under her powerpoint for this hour). I. General Facts: GI Tract A. Mouth Purpose = chew food, break into small particles, mix with saliva, begin digestive process, and swallow the food B. Esophagus Purpose = transport food from mouth to stomach C. Stomach Functions o continue chemical digestion of food acid pepsin IF (Intrinsic Factor) o secretory activity o store chyme and slowly empty into small intestine o motility – breaks down food particles into smaller pieces, mixing with acid and pepsin to continue digestion of material, making into slushy chyme consistency chyme must be <1 mm to fit through pyloric sphincter (yes, that’s 1 mm, not 1 cm) D. Small Intestine (SI) Functions o Digestion pancreatic enzymes continue digestion mixing contractions called segmentations in SI that mix chyme with digestive enzymes o Absorption Occurs along varying locations along SI ileocecal valve prevents reflex of colonic material back into SI E. Large Intestine (LI) Functions o Fecal storage until elimination o Absorption of any remaining water and electrolytes Need for adequate blood supply o Absorption of nutrients → bloodstream Gastrointestinal2 #03 Mon 2/23/04 10:00am Page 2 of 10 o Absorption of lipids → lymphatic system o Blood supply brings H2O and electrolytes to secretory cells to form the enzymes and different secretions o O2 provided by blood supply for motility F. Layers of the SI (slide 3) From inside to outside the layers and elements are: Mucosa Mechanoreceptor Endocrine Cells Muscularis muscle Submucosal plexus* Blood vessel Circular muscle Myenteric plexus* Longitudinal muscle layer Serosa *NOTICE THE PLEXUSES ARE INCORRECTLY SWITCHED IN THE PPT DIAGRAM! THEY ARE IN THE CORRECT ORDER ABOVE Notes on the different layers: Interplay between both muscle layers (circular and longitudinal) occurs o to change the diameter of the canal o to achieve segmentation (mixing) contractions o to achieve peristaltic contractions Mucosa o Chemoreceptors o Mechanoreceptors o Secretory cells o Glands There are 2 enteric (meaning intrinsic) nervous systems in the gut o Submucosal plexus (between submucosa and circular smooth muscle layer) receives signals from chemoreceptors and mechanoreceptors sends signals to secretory cells to regulate secretions by diff regions of gut o Myenteric plexus (between circular muscle and longitudinal muscle layer) Regulates motility Remember that also innervating gut is the Sympathetic Nervous System (SNS) and Parasympathetic Nervous System (PNS) G. Autonomic Nervous System and the GI Tract (slide 4) PNS stimulation o Innervates with enteric nervous system (myeneteric plexus and submucosal plexus) o Always excitatory Gastrointestinal2 #03 Mon 2/23/04 10:00am Page 3 of 10 II. o ↑ motility and ↑ secretions o vagus n. innervates most regions of the gut except beginning at the transverse distal colon o pelvic n. innervates the colon o enteric nervous system sends signals to smooth muscle, secretory cells, endocrine cells, and blood vessels SNS stimulation o Innervates with enteric nervous system (myeneteric plexus and submucosal plexus) AND with blood vessels o Think of as inhibitory o ↓ motility and hyperpolarize smooth muscle o release of catecholamines and NE (NorEpinephrine) to stimulate α receptors causing vasoconstriction and ↓ blood supply to the gut H. Local and Central GI Reflexes (slide 5) Short arc (local) reflexes o Only intrinsic (enteric) nn. o Leads to contraction o e.g., segmentation contractions in SI (due to distention of SI in presence of chyme) o Food present in stomach → distention → stimulation of mechanoreceptors → short arc reflex → ↑ contraction and ↑ secretions (e.g., G cells releasing gastrin, parietal cells releasing acid, chief cells releasing pepsinogen) Long arc (central) reflexes o Always involves either SNS or PNS nn. o Food present in stomach → distention → long arc reflex → activation of vagal fibers → stimulate myenteric and submucosal plexuses→ ↑ motility and ↑ secretions in stomach o Cephalic phase of digestion is mediated by long arc reflexes via the vagus n. Beginning Digestion A. Interdigestive period (slide 6) About 12-15 hours/day is spent in the interdigestive period SI is empty; the only chyme is present in the colon ↓ secretions, ↓ vagal stimulation of gut, ↓ levels of salivary glands, ↓ stomach volume, ↓ acidic secretions, ↓ levels pancreatic enzymes, ↑ rate of synthesis of bile salts in liver (i.e., sphincter of Oddi will be constricted), concentration of bile in gall bladder haustral contractions in colon, also some absorption in colon periodically, a burst of activity and motility (peristaltic contractions beginning at the stomach) o correlated with surge of plasma motilin levels from SI and IMMC (Interdigestive Migrating Motor Complex) one peristaltic contraction goes through the entire gut due to interstitial cells of Cajal (the gastric pacemaker cells) located throughout the gut Gastrointestinal2 #03 Mon 2/23/04 10:00am Page 4 of 10 o IMMC rate = 3/minute (i.e., 1 every 20 sec), set by interstitial cells of Cajal o Recall that the IMMC is a “housekeeping function” things moving during the interdigestive period B. Cephalic Phase (slide 7) Begins when you start thinking about a meal (smelling, seeing, and then chewing the food causes vagal stimulation) Ends when you begin the swallow Mediated solely by PNS function; if you abolish PNS function, then you abolish everything that happens in the cephalic phase Consequences of cephalic phase o salivary secretions o stimulation of parietal cells o stimulation of G cells in antrum of stomach → release gastrin o ↑ pancreatic exocrine secretions (mostly ↑ in pancreatic enzymes, very little HCO3 at this point) o contraction of gall bladder begins o gastrin circulates as a hormone and travels to parietal cells → release IF chief cells → release pepsinogen C. Saliva Composition of saliva (slide 8) o Water - 97-99.5%; hypotonic/hypoosmotic relative to plasma Recall osmolality of plasma = 280-290 mOsm Saliva is the only secretion that is hypotonic/hypoosmotic relative to plasma o Electrolytes: Na, K, Cl, PO4, HCO3 o Digestive enzymes: amylase, lipase amylase begins starch digestion recall starch = a long chain of glucose; amylase breaks it down into oligosaccharides o Proteins: mucin, lysozymes, IgA o Metabolic wastes: urea, uric acid o Volume: 1-1.5 liters daily o Rate: Basal = 30 ml/hr (interdigestive period, keeps mouth clean) Maximal = 400-600 ml/hr (during eating) Secretion of Saliva (slide 9) o Greatest salivation is during cephalic phase o secretion of saliva mediated by PNS o amylase-containing primary secretion occurs in acinar cells o modification of ionic contents occurs in the striated and excretory ducts (ducts that are impermeable to H2O) active absorption of Na active secretion of K (↓ rate than Na absorption) Gastrointestinal2 #03 Mon 2/23/04 10:00am Page 5 of 10 III. passive absorption of Cl active secretion of HCO3 (caused by vagal stimulation) maximum vagal stimulation of saliva secretion means less time for modification in the ducts → ionic concentration of saliva varies with the rate of secretion Esophageal Phase A. Swallowing reflex (slide 10) central (long arc) reflex Up to this point, you can voluntarily stop swallowing (buccal phase), but after this point the reflex is involuntary (pharyngeal phase) Swallowing reflex initiated by pharyngeal receptors in the back of the throat; swallow cannot stop once it goes beyond the skeletal muscle portion of the esophagus Once the smooth muscle portion of esophagus is reached = the esophageal primary peristaltic reflex B. Traveling of food bolus down esophagus (slide 11) Relaxation in front of bolus, constriction behind bolus (requires vagal stimulation) Circular muscles contract behind the bolus to constrict and push bolus down Longitudinal muscles contract in front of the bolus to shorten passageway ahead of bolus LES (Lower Esophageal Sphincter) is constricted when the bolus is on its way down (adaptive relaxation of stomach) LES relaxes when bolus gets there, and constricts again once bolus has passed (slide 12) C. LES (Lower Esophageal Sphincter) (slide 13) Prevents reflux of acid into esophagus Below level of diaphragm, nonspecific group of cells When Pabdominal > Pthoracic it causes LES to squeeze down on esophagus (P=Pressure) Receptors from vagus n. and myenteric plexus keep LES constricted o ACh on α → depolarization of smooth muscle → constriction of smooth muscle (ACh = AcetylCholine) ↑ LES tone o Acetylcholine o α-agonists o Gastrin, motilin (depolarize smooth muscle) o Protein, coffee o Antacids, prostaglandins ↓ LES tone (promotes GERD = Gastro Esophageal Reflux Disease) o Purinergic, β-agonists o CCK, secretin, histamine, VIP, progesterone o Fat, CHO, chocolate o Anticholinergics, nicotine, alcohol, peppermint Gastrointestinal2 #03 Mon 2/23/04 10:00am Page 6 of 10 Q: Is coffee not contraindicated in GERD? A: Yes it is, but not according to this list (coffee → ↓ LES is not by the same type of mechanism as the others on the list above…basically don’t worry about it for the test). IV. Gastric Phase A. Digestive period (slide 14) Food is in the stomach Salivary secretions down to baseline levels with absence of chewing Active secretions are mostly due to gastrin (PNS stimulation drops, but hormonal effects ↑) Distention of stomach → ↑ gastrin (via G cells) ACh and gastrin cause: o vagal stimulation still induces pancreas to release enzymes and HCO3 (still more enzymes than HCO3 in this phase) o gall bladder contraction the release of enzymes and bile into SI prepare SI for chyme coming from stomach much colonic activity; haustral contractions within 15 minutes, the gastrocolic reflex starts – a lot of chyme is moved across the transverse colon into the distal colon and rectum, initiating the defecation reflex another strong initiation of the defecation reflex occurs when you first stand up in morning B. Muscles of stomach (slide 15) stomach has 3 layers of muscle: o longitudinal o circular o oblique muscle layers are thinner in the body of the stomach (weaker mixing) muscle layers are thicker toward pyloric antrum region (stronger mixing) pyloric sphincter is tonically constricted C. Layers of the stomach wall (slides 16, 17) Glands in stomach o parietal glands o pyloric antral glands body and fundus of stomach have the majority of glands in the stomach – gastric pits gastric mucosal cell o secrete thick mucus ↑ in HCO3 mucus neck cells o secrete pepsinogen (inactive proteolytic enzyme) o acid environment induces pepsinogen → pepsin chief cells o release acid, IF Gastrointestinal2 #03 Mon 2/23/04 10:00am Page 7 of 10 pyloric antrum o G cells → release gastrin o D cells → release somatostatin considered paracrine; it acts locally when pH<2, somatostatin release is accompanied by ↓ gastrin secretion and ↓ parietal cell stimulation—a protection mechanism to keep the stomach from getting too acidic D. Stimulatory events of stomach (slide 18) cephalic phase is mediated by vagus n. only o Signals to cerebral cortex and hypothalamus → vagus n. → motor activity in stomach and release of gastrin and acid o administration of atropine → all events in cephalic phase would be eliminated since everything in the cephalic phase is mediated by the vagus n. gastric phase o Distention → stretch receptors → vasovagal reflexes → brainstem vagus n. → motor activity G cell → release gastrin parietal cell → release acid o direct stimulation by chemicals in food o also local reflex mediated by myenteric and submucosal plexuses ↑ motor activity and ↑ secretions intestinal phase o G cells → release gastrin E. Inhibitory events of the stomach (slide 18) Excess acidity → somatostatin → inhibit G cells If emotionally upset, SNS will override PNS During digestion o Distention of SI, presence of food chemicals → local reflexes → enterogastric reflex → ↓ motor activity and secretions o Also long arc vagal enterogastric reflex = constriction of pyloric sphincter o fats = release of CCK o acid and hypo- or hyper- osmotic chyme = release of secretin o carbohydrates = release GIP or VIP o secretin, GIP, CCK, VIP – when in blood will feed back to the stomach to ↓ motility and secretions F. Receptors on parietal cell (slide 19) 1 Gastrin receptor 2 ACh receptor 3 Histamine receptor Stimulation of any of the 3 will activate protein kinase → production of HCl Gastrointestinal2 #03 Mon 2/23/04 10:00am Page 8 of 10 o HCl transported by proton pump via gastrin gland duct to lumen of stomach H+ ion formed by combination of CO2 and H2O → HCO3 o H+ ion then pumped out of cell o venous blood draining stomach during digestion = alkaline tide To block or reduce acid secretion chemically o Can block any of the 3 receptors o Or, you can block the proton pump at the end G. Gastric emptying Promotion of gastric emptying o Pressure gradient in stomach (Pstomach > Pduodenum) o Distention of stomach – ↑ motility or force of contraction o Gastrin – ↑ force of contraction o Vagal stimulation – ↑ force of contraction o Large meal – ↑ force of contraction Inhibition/Delay of gastric emptying (slide 20) o Any SI signal to stomach: “We have chyme and we need to digest and absorb before you give us any more.” o Acid – hyperpolarizes smooth muscle o Fats – CCK and GIP o Amino acids and peptides – CCK also** **Note the mistake on slide 20: gastrin on the far right will not delay but PROMOTE gastric emptying because gastrin depolarizes smooth muscle. Amino acids and peptides will still have an inhibitory effect on gastric emptying, though, but it is through the release of CCK (as her arrow indicates). H. Gastrin (slide 21) most important acid secretion Secreted by G cells in antrum into blood stream (hormone) Stimulates gastrin receptors on parietal cells Functions o Stimulates HCl secretion o ↑ gastric and intestinal motility o ↑ pancreatic secretions (primarily enzymes) o Necessary for the proper growth of GI mucosa I. Regulation of gastrin secretion (slide 22) Distension Vagal stimulation – ACh, GRP (bombesin) Enterogastrones (secretin, CCK, GIP which feed back from SI to delay) Acidic pH o somatostatin inhibits when pH < 3 Food products (secretagogues) o protein digestion products o alcohol o Ca++ o coffee (caffeinated and decaffeinated) - due to protein, a.a. Gastrointestinal2 #03 Mon 2/23/04 10:00am Page 9 of 10 V. J. Histamine (paracrine agent) (slide 23) mast cells outside of parietal cells histamine will combine with receptor on parietal cell to → acid secretion Stimulate H2 receptors on parietal cells; potentiates secretion produced by ACh & gastrin Stimuli for release o vagal stimulation o gastrin o other (HCl, pepsin) Feedback inhibition: (via inhibition of gastrin by somatostatin) when pH < 3.0) ACh, gastrin, histamine all act synergistically K. Pepsinogen (slide 24) Secreted in an inactive form, pepsinogen (proenzyme) Activated by acid and previously formed pepsin in lumen of stomach Proteolytic enzyme that begins the process of protein digestion; optimal activity at pH 1.8 - 3.5 Cephalic stage: vagally stimulated cholinergic neurons within the enteric nervous system directly stimulate chief cells to release pepsinogen Gastric phase: low pH activates local reflexes that enhance pepsinogen secretion (vagal stimulation and gastrin secretion) Intestinal phase: Secretin enhances pepsinogen release L. Intrinsic Factor (slide 25) Secreted by parietal cells along with acid Essential for absorption of vitamin B12 in the terminal ileum If parietal cells destroyed (e.g., chronic gastritis), will develop hypochlorhydria (low acid secretion) or achlorhydria (no acid) and macrocytic/pernicious anemia due to failure of maturation of RBCs Early Intestinal Phase (slide 26) A. Occurrences in digestive period of early intestinal phase stomach slowly emptying into SI no salivary secretions continue with motility in stomach (both mixing contractions and periodic peristalsis) gastrin volume ↓ as empty stomach acid secretion at peak in gastric phase, starts to ↓ here in response to chemical feedback due to secretin, CCK (these 2 are at peak during this early intestinal phase) secretin, CCK also stimulate pancreatic secretions o CCK is main signal o Secretin, CCK on pancreas potentiate each other plasma gastrin levels ↓ → ↓ distention stomach → ↓ signals from chemicals in chyme of stomach secretin → HCO3 secretion in the pancreas (from ductal cells) o major stimulation is acid in duodenum Gastrointestinal2 #03 Mon 2/23/04 10:00am Page 10 of 10 Enzymes needed for CHO, fats, and protein digestion CCK = cause contraction of gall bladder and releases bile with relaxation of sphincter of Oddi o Need bile for emulsification, digestion, and absorption of fats Material in colon = haustral contractions + periodic peristaltic contractions B. SI mucosa and villi (slide 27) Main function in SI = digestion and absorption o Surface Area for absorption = 2 million cm2 = adaptation to ↑ mixing Adequate arterial blood important removal by hepatic portal v. countercurrent mechanism around central lacteal Absorption of nutrients across mucosal brush border into villus from epithelial cell Contents taken up by blood capillary → liver Lipids being absorbed into central lacteal → vena cava → liver