Nursing Assessment of the Gastrointestinal System
advertisement
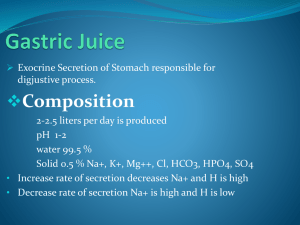
Nursing Assessment of the Gastrointestinal System Sasha Alexis Rarang, RN, MSN The digestive system Structures and Function of the GastroIntestinal System Main Function of the GI System????? Supply Nutrients to body cells Process of Digestion and Elimination A. Ingestion ( Taking In Food) B. Digestion ( Breakdown of Food) C. Absorption ( transfer of food products into the circulation) D. Elimination Concepts of Structures and Functions The GI System consists of the GI tract and its associated organs and glands A. GI tract 1. mouth 2. esophagus 3. stomach 4. small intestines 5. large intestines 6. rectum 7. anus B. Associated organs 1. liver 2. gall bladder 3. pancreas Mouth Mouth Oral or buccal cavity Chewing >> break food products into smaller portions. >> allows digestion and prevent trauma to the mucous lining of the esophagus. >> person exert 25 to 275 lbs during the chewing process. >> Dentures vs. Natural teeth >> poorly chewed foods are not readily digested. Saliva Secreted by the sublingual and submandibular glands. Lubricate and softens the food mass Amylase – breaks down starches to maltose. Swallowing Involves 3 phases >>oral phase >>involuntary pharyngeal phase >>esophageal phase > The time it takes for the bolus to reach the stomach depends on the consistency of the bolus and individual’s position. Esophagus Esophagus A hollow muscular tube Lies posterior to the trachea and larynx Serves as a passage for food from mouth to stomach. >> upper esophageal sphincter >> lower esophageal sphincter Antireflux barrier Act as a vent for increased intragastric pressure. stomach Stomach Structures a.1. fundus a.2. body/central area a.3. antrum/pyloric region a.4. cardiac sphincter a.5. Pyloric sphincter B. Microscopic Glands ( epithelial lining of the stomach) b.1. Cardiac glands – mucus b.2. Peptic (Chief Cells) – mucus and pepsinogen b.3. Parietal (Oxyntic) – HCl acid and water protein digestion intrinsic factor – B12 absorption b.4. Neck cells – mucus b.5. Pyloric glands – gastrin and mucus stimulates HCl acid production A. Stomach C. Functions c.1. storage, mixing and liquefaction of the bolus of food into chyme, control of passage of food into the duodenum. c.2. first stage of protein breakdown c.3. mechanical breakdown of food c.4. absorption of water, alcohol, glucose, and some drugs. c.5. protection Stomach D. Innervation d.1. parasympatehetic – vagus nerve d.1.1. increased gastric secretion of acid, gastrin and pepsin. d.1.2. increased gastric acid motor activity. d.2. sympathetic – inhibit gastric secretion and motility. Stomach E. Secretions – 1.5L to 3.0.L of gastric juice per day. e.1. HCl acid, pepsin, and mucus. e.2. mucin, intrinsic factor, lipase, and pepsinogen. e.3. Gastric acid secretion is directly stimulated by the distention of the stomach and presence of protein. e.4. vagal stimulation, acetylcholine, histamine, and the hormone gastrin. e.5. gastrin is released when the stomach becomes distended with food. Stomach Stomach Small intestines Small Intestine Structure (22 feet long/1 inch in diameter) a.1. duodenum a.2. jejunum a.3. ileum B. Function b.1. completes the digestion of foods b.2. absorbs the products of digestion b.3. secretes hormones – control secretions of bile, pancreatic juice, and intestinal secretions. A. Small Intestine C. Innervation c.1. sympathetic – inhibits motility c.2. parasympathetic – increases intestinal tone and motility. D. Secretions d.1. Brunner’s glands(duodenal) – mucus d.1.1. glucagon, presence of chyme, and vagal stimulation. d.1.2. sympathetic stimulation inhibits secretions of the glands. d.2. Goblet cells – mucus d.3. crypts of Lieberkuhn – secretes an alkaline fluid d.4. epithelial cells – digestive enzymes d.4.1. enterokinase – activates trypsin d.4.2. maltase,lactase, and sucrase – disaccharides Small Intestine E. Absorption e.1. Complex foods are converted into its simplest forms. e.1.1. CHO – monosaccharides e.1.2. CHON – amino acids e.1.3. Fats – fatty acids, monoglycerides, diglycerides and triglycerides. e.2. Water absorption – 8L/day e.3. water-soluble vitamins, electrolytes, minerals. e.4. B12 absorption takes place in the ileum Large intestines Large Intestines Structures ( 5-6 feet long) a.1. Cecum a.2. Colon a.2.1. Ascending a.2.2. Transverse a.2.3. descending a.2.4. Sigmoid colon a.3. Rectum and Anus ( final segments of the large intestine) B. Function b.1. absorb the remaining water, urea,and electrolytes. b.2. secretes mucus b.3. form and store the feces until defecation A. Large Intestine C. Innervation c.1. parasympathetic – vagus nerve increases peristalsis, decrease tone of the sphincter. c.2. sympathetic – reduce peristaltic activity and increase tone of sphincters. D. Secretion d.1. water, mucus, potassium, and bicarbonate – alkaline solution. d.2. Mucus – lubricates, allows passage of the fecal matters, protects the mucosa from injury. Rectum Anus Associated Organs of the GI System Liver Activities of the tract A. Secretion of electrolytes, hormones, and enzymes B. Movement of the Ingested products C. Digestion of food and fluids D. Absorption of end products into the bloodstream. A. Secretion of electrolytes, hormones, and enzymes Hormones – gastrin Electrolytes – H2, Cl, Na, K, Enzymes – pancreatic lipase, enterokinase, ptyalin Movement of the Ingested products Digestion of food and fluids Absorption of end products into the bloodstream Secretions Mucous secretions a. produced throughout the entire length of the tract. b. protects and lubricate the walls of the GI tract. 2. Digestive secretions. a. produced in the mouth, stomach, duodenunum, and jejunum. b. break down ingested food so that it can be absorbed. 1. Secretion: Motility 2 types of movement in the GIT A. Mixing B. Propulsion / Peristalsis ****Soft muscle tissues of the GIT**** Digestion and Absorption Food is broken down into small and simple compounds enough to be absorbed into the bloodstream by diffusion or active transport. Digestion and secretion Effects of Aging on the Gastrointestinal Tract A. B. C. D. E. Teeth may loosen up from the supporting gums and bones. Decreased output of the salivary glands leads to dryness of mucous membranes and increased susceptibility to breakdown, difficulty swallowing and decrease stimulation of the taste buds. Decreased secretion of digestive enzymes and bile – decrease ability to digest and absorb food. >> impaired absorption of fat and fat soluble vitamins Atrophy of gastric mucosa leads to decrease HCl acid production. >>decrease iron and B12 absorption – anemia >>proliferation of bacteria – diarrhea and infection Decrease peristalsis in the large intestine, decrease muscular tone of the intestinal wall and decrease abdominal muscle strength – decrease sensation to defecate and increase incidence of constipation. Teeth may loosen up from the supporting gums Decreased output of the salivary gland Dryness of the mucous membrane Difficulty swallowing Decrease stimulation of the taste buds Effects of aging on the gastrointestinal tract Decreased secretion of digestive enzymes and bile – decrease ability to digest and absorb food. Ex. Impaired absorption of fat and fat soluble vitamins Effects of aging on the GI tract > Atrophy of gastric mucosa leads to decrease HCl acid production Assessment of the GI System Assessment of the GI System A. Past Health History a.1. history or existence of ; > abdominal pain > nausea and > diarrhea > abdominal distention > anemia > dyspepsia > hematemesis > allergies > excessive gas > melena > rectal bleeding vomiting > constipation > jaundice > heartburn > changes in appetite > food intolerance > indigestions > bloating > hemorrhoids Assessment…. B. Medications: b.1. past and current use of medications b.1.1. OTC drugs b.1.2. prescription drugs b.1.3. herbal products and nutritional supplements. b.2. hepatotoxic, diarrhea, GI bleeding C. Surgeries and other treatments c.1. information about hospitalizations for any problems related to GI system Functional Health Assessment Assessment…Objective Data A. Inspection a.1. Lips – symmetry, color and size observe for abnormalities – pallor or cyanosis, cracking, ulcers, or fissures. a.2. Tongue – color, fissures, deviation and lesions a.3. Buccal Mucosa – color and lesions and distinctive breath odors a.4. teeth and gums – caries, loose teeth, abnormal shape and position of the teeth, presence of swelling , bleeding, discoloration. Assessment…. a.5. Abdomen a.5.1. Skin changes ( color, texture, scars, striae, dilated veins, rashes, and lesions.) a.5.2. umbilicus – location and contour a.5.3. symmetry a.5.4. contour – flat, rounded, distended. a.5.5. observable masses – hernias and other masses. a.5.6. movement – observable peristalsis and pulsation. Assessment: Inspection (Skin changes) Assessment Quadrants of the Abdomen AbdominalDraping distention; dilated veins the Abdomen Obese abdomen Hepatomegaly ascites Umbilical Hernia Pregnancy Assessment…. B. Auscultation (done before percussion and palpation) b.1. listening for increased or decreased bowel sounds. b.2. diaphragm of the stethoscope – bowel sounds are high pitched, occur 5-35x per minute. b.3. warm up stethoscope in the hands to prevent abdominal muscle contraction. b.4. listen for BS for 2-5 minutes. Absent BS means no sounds for 5 minutes on each quadrant. C. Percussion c.1. purpose??? Determine the presence of fluid, distention, and masses. Presence of air – tymphany, fluid or masses – dull sounds Auscultation: Listen for……. Increased or decreased bowel sounds Normoactive, hypoactive,hyperactive, or absent Listen with the diaphragm side of the stethoscope BS are high pitched sounds, 3-5x a minute Warm up the stethoscope in the hands to avoid undue abdominalmuscle contraction Listen for BS for 2-5 minutes on each quadrant Absent BS means no sounds for 5 minutes. Assessment: Percussion Purpose????? Determine the presence of fluid, distention, and masses Tymphany is normally present in most areas of the abdomen Dullness!!!!! Ac lue to an underlying mass Assessment: Palpation Light palpation – 1cm deep Look for area of tenderness Look for patient’s facial expression and guarding Deep palpation Delineate body abdominal organs Use two-hand method Diagnostic Studies Upper GI Series or Barrium Swallow > X-ray study with fluoroscopy with contrast medium > used to diagnose structural abnormalities of the esophagus, stomach, and duodenal bulb >NPO for 8-12 hours > pt. will drink contrast medium > give pt. laxatives and fluid to prevent contrast medium impaction. > the stool may be white up to 72 hours after the test B. Small Bowel Series – same as upper GI series A. Diagnostic tests C. Lower GI or Barium Enema > Fluoroscopic examination of the colon using contrast medium w/c is administered rectally. > administer laxatives and enemas the night before the procedure.*****CLEAR**** > clear liquid diet the night before. > NPO for 8 hours before the procedure. > cramping and urge to defecate may occur. > explain that pt will be assuming various position in tilt table. > give laxatives, fluids to assist in expelling barium. Diagnostic tests C. Ultrasound > noninvasive procedure uses high frequency soundwaves to visualize the solid organs. > NPO 8-12 hours D. CT-Scan – > non invasive radiologic examination that combines x-ray machine and computer. E. MRI > non invasive procedure using radiofrequency waves and magnetic field > NPO for 6 hours > C/I in pt with metal implants or who is pregnant Diagnostic tests End of Topic