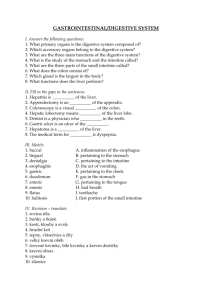
GI System
advertisement

GI System Food Pathway o Mouth Esophagus Stomach Small Intestine (Duodenum Jejunum Ileum) Large Intestine (Ascending Traverse Descending Sigmoid Colon) Rectum Anus Movement of food through the gastrointestinal (GI) tract, from the mouth to the anus involves o Ingestion- Taking food through the mouth o Mastication- Chewing o Deglutition- Swallowing the food o Peristalsis- The process of moving the food through the GI tract via smooth muscle contraction. Function Secretion o Both endocrine and exocrine substances aid in digestion Digestion o This is the processing of ingested foods into molecular forms that can be transferred, along with salts and water, from the external environment to the body’s internal environment, where they can be distributed to cells by the circulatory system. Absorption o The average adult consumes about 800g of food and 1200ml of water. An additional 7000ml of fluid from salivary glands, gastric glands, pancreas, liver, and intestinal glands is secreted in the tract each day. Only about 100ml of water is lost in the feces. The rest is absorbed into the blood. General Anatomy There are two divisions of the GI system o GI Tract This is the tube that begins at the mouth and ends at the anus. o Accessory glands Salivary glands secrete saliva to aid in the digestive process. The liver, pancreas, and gall bladder gland provide hormonal and/or enzymatic support to the entire process. The entire GI tract presents certain common structural characteristics. It is a hollow tube composed of a lumen of variable diameter surrounded by a wall mode of four principle layers. Structures within the GI tract are considered to be on the outside of the body since the lumen of the tract is continuous with the external environment and many layers must be crossed for the GI contents to reach the blood. o Cross section of a typical portion of the GI tract Adventitia/ Serosa This is the outmost layer. It is a thin layer of loose connective tissue containing various vessels and nerves, simple squamous mesothelium, and visceral peritoneum. It may be surrounded by mesentery. Muscularis Muscle Here there is a layer of longitudinal smooth muscle just inside the serosa that produces a shortening movement. A layer of circular muscle runs concentrically around the tube, producing a narrowing of the lumen. Contractions of these muscles provide the forces for moving and mixing the GI contents. Auerbach’s (myenteric) nerve plexus is contained between the two muscle layers. Submucosa This consists of loose connective tissue containing mucous glands, blood and lymph vessels, and a variety of nerves including Meissner’s (mucosal) nerves. Mucosa This is composed of ciliated columnar epithelium, lamina propia (connective tissue containing small blood vessels, nerve fibers, and lymphatic ducts), and muscularis mucosa (smooth muscle). The enteric system is composed of two different nerve plexuses. o The submucosal plexus is located in the submucosa layer, and the myenteric plexus is located between the circular and longitudinal smooth muscle layer. o These are both innervated by both sympathetic and parasympathetic nervous systems. Sympathetic stimulation is inhibitory, and parasympathetic is the opposite. A patient with an overactive digestive system would require a sympathomimetic drug to decrease its activity. Parasympathomimetics are required for patients with an underactive GI system. The muscles in the GI system are single unit types. They have oscillating membrane potentials. When the muscle fibers are stimulated by the parasympathetic nervous system, the degree to which they depolarize is increased, resulting in action potentials that lead to smooth muscle contraction. Gastrointestinal Components Oral Cavity Function o Chewing, production of saliva, and swallowing Histology o The oral mucosa consists of stratified squamous epithelium over a dense layer of connective tissue. The epithelium is usually not keratinized, but may become keratinized under adverse conditions. Anatomy o Lips This is keratinized stratified squamous epithelium which turns into a mucous membrane upon entering the mouth. o Cheeks The cheeks contain considerable fat and are lined with a mucous membrane consisting of non-kertinized squamous epithelium. o Tongue The tongue functions to keep food inside of the mouth as it is being chewed. After it has been chewed, it then assists food by moving it to the back of the throat for swallowing. It is a mass of striated muscle covered with a mucous membrane. The dorsal surface is covered with papillae which contain taste buds, which are specialized sensory structures. These are gustatory receptors and are a type of epithelial cell that is clustered with other cells called supporting and basal cells. The taste buds are somewhat barrel shaped. They have microvilli at the area of the taste pore. o Salivary glands These function to secrete saliva. Functions of Saliva o Saliva lubricates food, making it easier to swallow. o Saliva also helps dissolve some food molecules. It contains amylase, which is an enzyme that can begin the process of digestion. Amylase probably has to do more with freeing up molecules that actually participate more in the actual taste phenomenon, more than it does in the actual digestion. As soon as the food bolus enters the stomach, HCl denatures amylase, terminating any digestive activity of that enzyme. All enzymes are proteins and the low pH of the stomach is going to denature them, except the few that are designed to specifically function in that environment. o Saliva also contains an important antibacterial secretion. Anatomy/ Histology The compound tubuloalveolar glands contain acinar cells that secrete between 1-2 liters of saliva every day. These terminate in an alveolus which may empty into intercalated ducts, forming larger striated ducts. The resting rate of secretion is about 0.5 ml per minute. Basket cells (myoepithelial cells) are involved in the discharge of secretions. Cuboidal cells predominate in the alveoli and secrete saliva containing enzymes, mucous, immunoglobulins (IgA), etc. Types The parotid gland is located in front of and under the ear. This is the largest of the glands and is a branched acinar gland. It contains mostly serous cells which secrete a watery solution containing inorganic ions, IgA, and amylase. The submandibular gland is located in the jaw, below the mandible and mylohyoid muscle. This is a branched tubuloacinar gland that contains mucous cells which secrete mucin and lysozyme. It is mucin that gives a thick viscous characteristic to saliva. The sublingual gland is located under the tongue, in the floor of the mouth. This also a branched tubuloacinar gland that contains mucous cells. Control Both parasympathetic and sympathetic controls exist, with the parasympathetic producing a greater response. In the absence of ingested material, a low rate of salivary secretion keeps the mouth moist. In the presence of food, salivary secretion increases markedly. The response is initiated by chemoreceptors and pressure receptors in the walls of the mouth and on the tongue. CN 7 controls both the sublingual and submandibular glands. CN 9 controls the parotid gland. o Teeth These function to cut food into smaller pieces prior to degluttination. Anatomy The crown is the part of the tooth that extends above the gum or gingiva. The outer part of the tooth is the enamel. It is the hardest substance that our body produces. It is extremely hard, translucent, non-replaceable, and is secreted by the ameloblast during tooth development. Just inside the enamel is a calcified matrix called the dentin, which makes up the bulk of the tooth and surrounds the dental pulp containing the nerves and blood vessels that supply the tooth. The root canal is the central canal in the tooth where blood vessels and nerves run. The dental alveolus is the part of the tooth that is embedded in the bone. Cementum surrounds the root of the tooth and attaches the tooth in its socket via periodontal ligaments to the alveolar bone. Gingiva (gum) has a continuation of the oral mucosa covering the bone in which the teeth are embedded. Organization On each upper and lower half of the mouth there are normally four incisors, two canines, four premolars, and eight molars. o Accessory Structures Frenulum This is a tissue that attaches the lip to the gumline. There are two, one upper and one lower. The lingual frenulum attaches the tongue to the floor of the mouth. Uvula This structure hangs down in the back center of the mouth. Soft palate Palatine tonsils These contain lymphatic aggregates within the submucosa, but are not directly in the lymphatic circulation. They are covered with an invaginating stratified squamous epithelium. Lingual tonsils These are located on the posterior 1/3 of the tongue. The mucous membrane is thick and moves freely. Its submucosa contains an aggregate of lymph nodules. Oral pharynx Behind the teeth is the oral cavity, which leads to the oral pharynx. Food travels this path into the esophagus while air goes through the glottis in the nasal pharynx into the respiratory system. Pathology o Apthous Ulcer (Chancre Sore) These lesions are very common and take the form of a shallow, painful ulcer. They are self-limited, and although the cause remains unknown, they are clearly affected by trauma (stress, viral, fungal, bacterial, and autoimmune). Treatment is not very effective. Topical steroids, antibiotics, and oral hygiene are possible solutions. o Herpes Cold Sores 80% are HSV Type I, and 20% are HSV Type II. This is the opposite of genital cold sores. Greater than 75% of the population has these by middle age. Treatment includes antivirals. o Leukoplakia and cancer Leukoplakia is a whitish patch on the mucosa caused by epidermal thickening or hyperkeratosis. This is a dysplastic condition, so it is proliferative, but it is not a neoplastic disorder. It can be potentially cancerous. There is a 5-15% chance of transformation to squamous cell carcinoma. There is an association with tobacco use, chronic friction (i.e., with ill-fitting dentures), and alcohol abuse. Most oral cancers are squamous cell variety, and these have a 50% five-year mortality rate due to metastasis at time of diagnosis. Treatment includes local excision and radiation. o Oral Cancer The lips and tongue are the most frequent sites of involvement. Squamous cell carcinoma is the most common. The cause is unknown, but risk increases with tobacco and alcohol. o Thrush (Candida) This is a fungal infection in the oral cavity related to many other diseases, such as those that are immunocompromised. Esophagus Function o It functions to conduct food and fluids from the pharynx to the stomach and to prevent reflux of gastric contents into the esophagus. o It also secretes mucous to aid in lubrication of the food. o There is no enzymatic contribution towards the digestion of food. Anatomy o This is a soft, hollow, highly distensible muscular tube, about 25cm long, which extends from the pharynx to the gastroesophageal junction of the stomach. Through the course of its travels, the esophagus goes through the mediastenum, piercing the diaphragm. o It is located in three body regions; the neck, thorax, and abdomen. It is anterior to the vertebrae and posterior to the trachea. It adheres to the trachea via fibroelastic membranes and muscle. o The epithelium is stratified squamous. Its walls consist of mucosa, submucosa, muscular propia, and an adventitia. The superficial and deep esophageal glands transverse the mucosa which serves as a lubricant as food is pushed down towards the stomach. Lymphatic tissue is often present within the lamina propia. Mucous glands are present. o The upper 1/3 of the esophagus contains skeletal muscle in the muscularis. The lower 1/3 is involuntary muscle. In the middle, there is a mixed muscularis area of both smooth and skeletal muscle. o There is both an upper and lower esophageal sphincter that keep both ends of the esophagus closed in normal conditions. Physiology o The food bolus is pushed into the back of the mouth by the tongue, pushing the food against the soft palate, activating the reflex swallowing activity. Once the food bolus gets to the back of the throat, swallowing is pretty difficult to prevent. The swallowing center is located in the medulla oblongata. o The food bolus goes to the oral pharynx, and the process of swallowing actually elicits an inhibition of respiration for a period of time. This is designed to prevent the process of swallowing and inspiration simultaneously. When these two activities occur at the same time, it can cause violent eruptions of the diaphragm and abdominal muscles in a choking process trying to get rid of the food particle. Swallowing causes the soft palate to rise and lodge against the back wall of the pharynx, preventing food from entering the nasal cavity. The process of swallowing causes the epiglottis, a flap of tissue, to flap across the glottis, the opening of the trachea. The epiglottis closes the trachea, preventing food from entering the trachea and pushing the food into the esophagus. o As the food enters the esophagus, the upper esophageal sphincter relaxes and opens. It immediately closes after. o The food bolus is going to be moved down the esophagus by peristaltic action. One peristaltic wave can take nine seconds to reach the stomach. There are two components to this. Segmenting action This is a constriction of the tube, narrowing the orifice. It is accomplished primarily by the circular smooth muscles that run circumferentially around the esophagus. So that when they contract, the esophagus essentially pinches. Shortening action The longitudinal muscles contract, shortening the esophagus, which pulls part of it up and essentially helps to move the food bolus down. o At the end of the esophagus, there is a thickening of the muscle forming the gastroesophageal sphincter. This is not a true sphincter, however it acts as a sphincter. o Swallowing is generally accomplished via both somatic nerves to skeletal muscle and autonomic nerves to the smooth muscle. Pathology o Terms Reflux- This is the spilling of the acidic stomach contents into the esophagus. GERD- Gastro Esophageal Reflux Disorder o When the stomach is above the diaphragm, it causes reflow of stomach contents into the esophagus, causing heartburn, burping, etc. o The symptoms are generally from the reflux, not the mechanics. Dysphagia- Difficulty swallowing due to neurological spasms, mechanics, etc. Hematemesis- Vomiting blood, either fresh or digested o Hiatal Hernia This is a very common problem in the US. Only a small percentage of patients have symptoms. On its way down, the esophagus has to pass through a hole in the diaphragm called the esophageal hiatus. A common problem exists in which the esophageal hiatus is expanded, allowing part of the stomach to protrude through the hiatus. This causes problems, particularly when the individual is reclining. It tends to cause acidic stomach juices to move up through the esophagus, producing significant distress, particularly heart burn. Anything that causes reflux from the stomach up the esophagus can significantly irritate the end of the esophageal area and cause a lot of pain. Drugs can decrease hydrochloric acid secretion, decreasing the irritation. Treatments include antacids, prokinetic drugs (cytoprotective, promotility, H2 blockers, and proton pump inhibitors) and antireflux measures. Someone with this problem should not eat at night or eat while lying down. Antispasmodics (Levsin or nitroglycerin) can also be used. In infants, the gastroesophageal sphincter sometimes has not descended into the abdominal cavity and it still resides within the thoracic cavity. The pressure in the thoracic cavity is subatmospheric which tends to allow substances to very easily ascend up the esophagus. Consequently, there is a tendency to empty the stomach contents very simply. Some animals like mice and rats have a much stronger gastrointestinal sphincter than humans. They are incapable of throwing up. This is why they are so easily killed when ingesting toxic substances. o Mallory Weiss Tear This is a tear in the mucosa at the GI junction due to severe retching or vomiting, typically seen in alcoholics. This tear causes blood to be present in the vomit. o Varices These are dilated lower esophageal veins occurring secondary to portal hypertension. This dilation leads to collateral bypass channels and therefore engorged esophageal veins. Dilation of the rectal, umbilical, and lower esophageal veins can all occur. This most commonly occurs due to alcoholic cirrhosis. These are serious, because these vessels can rupture and bleed extensively, which if severe enough can lead to death. This can also be seen in the liver. Treatment includes endoscopy and injection of sclerosing agent or cauterization. Surgery is sometimes required. Tamponades (balloons) are also used. o Esophagitis and Barrett’s Esophagus Inflammation of the esophagus can occur for many different reasons. In the US it is usually due to reflux. Males are affected more than females. Symptoms include pain and a “burning” sensation in the chest. Treatment includes antacids and antireflux measures. Chronic esophagitis can lead to Barrett’s Esophagus, which is the replacement of normal stratified squamous epithelium with abnormal metaplastic columnar epithelium. This leads to a 30-40% increased risk of developing adenocarcinoma of the esophagus. If Barrett’s esophagus is not developed in 5 years, it probably will not. o Cancer Most cases of esophageal cancer are of the squamous cell variety. Risk factors include smoking, drink, esophagitis, etc. It can also spread from the stomach. Men are three times more likely than women to get it, especially over the age of 50. This is less common in the US vs. China and Iran, where there is a female predominance. Stomach Functions o Primarily to temporarily store food o Initiate the digestion of proteins o Move the food into the small intestine as a pasty material called chyme. Anatomy o This is a complex glandular digestive and endocrine organ. It is located on the left side of the abdomen and is relatively fixed at the esophagus and small intestine, but movable in between these structures. o Divisions Cardia This is the part of the stomach adjacent to the esophagus. It contains mainly mucous secreting cells, and the glands are comparatively short in length and depth. There is no sphincter here. Fundus This is the rounded part of the stomach above the gastroesophageal junction. This contains the majority of the chief and parietal cells, along with the body. Body This is the large middle portion. Antrum This is the floor of the stomach. It has a thick layer of smooth muscle. Pylorus This is the narrow lower connection of the stomach to the small intestine. This contains the branched glands with very deep irregular pits that produce gastrin and mucous. The pyloric sphincter is the true sphincter between the pyloris and the intestine. It is a ring of smooth muscle that controls the amount of food entering the small intestine. o The adult stomach is about 25cm long. An empty stomach has the capacity of 50ml, but can hold as much as 4L (1 gallon). The stomach can increase to as much as 1.5L without any increase in pressure, due to receptive relaxation. This is mediated by parasympathetic nerves with coordination by the swallowing center in the brain. o The stomach is innervated by the submucosal plexus and myenteric plexus. These have both parasympathetic and sympathetic innervation, with sympathetic innervation possessing inhibitory functions. o The mucosa has simple columnar cells and is folded into rugae when empty. The submucosa has circular and longitudinal muscles, where the muscularis is smooth muscle serosa. The muscle arrangement allows food to be moved, churned, mixed, and broken down into smaller pieces. The rugae contain openings called gastric pits, where a variety of substances are secreted by the cells here. These cells secrete about 2500ml of gastric juices daily. Most of this juice is produced by exocrine glands located in the body and fundus of the stomach. Contents of the normal gastric juice (fasting state) include cations (Na, K, Mg, H), anions (Cl, HPO3, SO4), pepsins, gelatinase, mucus, intrinsic factor, and water. o Parietal (Oxyntic) cells Secretes hydrochloric acid (HCl) The stomach secretes about 2L of HCl per day, with the majority occurring at the time of meals. The neuronal pathways and duodenal hormones involved act directly on the parietal cells and/or indirectly by influencing gastrin secretion, which in turn directly influences parietal cells. HCl acts by converting pepsinogen secreted by the chief cells into pepsin. Pepsin is a proteolytic enzyme which will begin the digestion of the proteins by cleaving larger chains of polypeptides into smaller chains. This is done most effectively at a pH of 1.4. Between 1 and 4, there is less digestion, and around 6-7, there is no digestion. This is an autocatalytic, positive-feedback process. HCl also plays an important role against bacteria or other ingested organisms. The extremely low pH (1-3) kills an enormous amount of organisms. Those that get past the stomach will cause significant intestinal distress. This also stimulates the flow of bile and pancreatic juices, as well as breaking down muscle fibers and connective tissue. Secretes intrinsic factor This is required for the absorption of vitamin B12 which occurs in the small intestine. In fact, it is the only hormone that is absolutely required in the process of digestion. o Chief (Zymogenic/Peptic) cells These are located in the basal glands of the antrum. They secrete pepsinogen, along with endorphins, serotonin, and cholecytokinin in response to nerve plexuses. Its secretion parallels that of HCl. Pepsinogen is an example of a zymogen that refers to any enzyme that is synthesized in an inactive form. This is done so that the enzymes are not digested in the process of digestion. They only act once inside a cell. o Goblet cells (Mucous Neck Cells) These cells are located in the glands of the antrum and scattered throughout the gastric epithelial lining. They have irregular shapes and produce a less viscous, more acidic mucous secretion than mucous secreting cells. o Surface mucosa cells These secrete HCO3 and mucus to form an unstirred layer that has a pH of about 7.0. This layer, along with the surface membranes of the mucosal cells and the tight junctions between them, constitute the mucosal bicarbonate barrier that coats the gastric wall and protects the mucosal surface from damage by gastric acid and HCl. Substances that tend to disrupt the barrier and cause gastric irritation include ethanol, vinegar, bile salts, aspirin, and other NSAIDs. Prostaglandins stimulate mucus secretion while aspirin and related drugs inhibit prostaglandin synthesis. The fluid also protects against mechanical injury by acting as a lubricant. o G-cells (Enteroendocrine cells) These are found in the pits of the pylorus and secrete the hormone gastrin into the portal blood, which is necessary for protein digestion. Gastrin secretion can be stimulated by the vagus nerve via acetylcholine, as well as being stimulated by many of the same components that stimulate HCl. It is inhibited by the high acidity of duodenal chyme, distension, hypertonic solutions, and solutions containing amino acids, fatty acids, and monosaccharides. The hormones that inhibit gastric activity are collectively known as enterogastrones, and include secretin, CCK, and additional unidentified hormones. o Enterochromofin-like cells These cells are stimulated by gastrin to secrete histamine which directly stimulates the parietal cells to release HCl. Tagamet, zantac, and pepsid AC specifically blocks the histamine receptors, causing decreased acidity in the gastric juice. o D-cells These secrete the hormone somatostatin which inhibits parietal, chief and G cells. Physiology o Gastric motility As with the esophagus, the stomach utilizes peristaltic waves to move food. These waves begin higher in the body as weak movements so that the contents are not mixed too much with acid and pepsin. The waves become stronger towards the antrum, where they mix the contents and close the pyloric sphincter. The waves are produced by pacemaker cells in the longitudinal smooth muscle layer that undergo spontaneous depolarizationrepolarization cycles known as the basic electrical rhythm of the stomach. This determines the frequency of the contractions, which is about three per minute. The force is determined by the neural and hormonal input to the antral smooth muscle, which depends on the contents of the stomach. Decreased parasympathetic or increased sympathetic activity inhibits motility. Pathology o Gastritis This is an inflammation of the stomach mucosa. It is a vague, descriptive term for self-limiting illness characterized by nausea, anorexia, epigastric distress with or without vomiting, as well as some systemic symptoms. There is also the presence of inflammatory cells, acute or chronic, in the gastric mucosa. Risk factors include NSAIDs, prescription medications, alcohol, physical stress, smoking, stress, aging, idiopathic, postgastrectomy, bile reflux, and infections. o Vomiting This is the forceful expulsion of the contents of the stomach and upper intestinal tract through the mouth. It is regulated in the medulla oblongata in an area known as the vomiting center and can be caused by neural input to the vomiting center via extensive distension of the stomach or small intestine, substances acting on chemoreceptors, increased pressure in the skull, rotating movements of the head as in motion sickness, intense pain, or tactile stimuli of the back of the throat. Vomiting is generally preceded by increased salivation, sweating, increased heart rate, pallor, and feelings of nausea. During vomiting, the abdominal muscles contract, raising the abdominal pressure, forcing the stomach contents into the esophagus. When this all occurs without the expulsion of stomach contents, it is called retching. Excessive vomiting can lead to large losses of the water and salts, which could result in severe dehydration, disruption of the body’s salt balance, and create circulatory problems because of the decrease in plasma volume. o Ulcers These are sores or erosions in the mucosa that extend through the muscularis mucosa into the submucosa or deeper. There is a strong association with H. pylori infection. Ulcers can also arise from stress, NSAIDs, steroids, spicy foods, etc. An acute or chronic benign ulceration occurs in a portion of the digestive tract that is accessible to gastric secretions. It does not occur in the absence of peptic gastric secretions. A penetrating ulcer refers to an ulcer that has gone to another organ. Diagnosis is done via biopsy or “breath test.” Antibiotic tests are not as good, because there are many false positives. Symptoms include pain, nausea, bloating, weight loss, and other symptoms due to blood loss. Blood in the stomach quickly congeals and turns brown and when vomited, looks like coffee grounds. Treatment Proton pump inhibitors inhibit HCl secretion. Same as GERD, but treat the H. Pylori with antibiotics as well. o Gastric Ulcer This is an ulcer due to decreased tissue resistance more than hypersecretion. This is demonstrated by x-ray or gastroscopy. Symptoms include epigastric distress or an empty stomach, epigastric tenderness and voluntary muscle guarding. o Zollinger-Ellison Syndrome (Gastrinoma) This is the increased production of stomach acid, causing increased ulcers. The major cause is a gastrin secreting tumor in the pancreas, while few have tumors in the submucosa of the duodenum and stomach, the hilum of the spleen, and the regional lymph nodes. This is a metabolic condition, and there is no association with H. pylori. Symptoms include severe peptic ulcer disease, gastric hypersecretion, and elevated serum gastrin. o Cancer This cancer has a survival rate of <10%, due to a high rate of metastasis. It is decreasing in incidence in the US. It is seen more in patients over 40. A favorite location is the lesser curvature of the stomach, and therefore any ulcer seen there on an upper GI x-ray deserves further investigation by endoscopy. Lesions are irregular with raised borders. Symptoms mimic sores or ulcers and include upper GI symptoms with weight loss including a palpable abdominal mass, anemia, and blood in stool. Small Intestine (Bowel) Function o This is the major digestive organ of the body. Almost all absorption occurs here, except for water and ethyl alcohol, which is absorbed in the stomach. o Secretions including water and mineral ions. Anatomy o This extends from the pyloric sphincter of the stomach to the ileocecal valve and is the longest part of the alimentary canal. o Dimensions 1 inch in diameter. 2m in length in situ due to muscle tone. 6m in length in a cadaver. o This is held in place by the mesentery, which contains arteries and veins. The mesentery is very movable so it allows for a lot of movement of the intestine while at the same time not allowing for twists or folds. The lamina propia is usually loose reticular connective tissue. o The inner wall of the intestine tract is folded into plica circularis, which are deep mucosal folds involving the mucosa and submucosa called villi that appear as fingerlike projections in the intestinal walls. These villi cause further microscopic folds of the entire mucosa of the intestine called microvilli or a brushborder. This serves to increase the small intestine’s surface area for absorption about 600-fold. o Structure of the Villi The epithelium is simple columnar with a brush border. The epithelial cells here have a large rate of mitosis, so there is a large turnover. They are released into the intestinal lumen, contributing to the digestive process. It is because of this rapid cell turnover that the lining of the intestinal tract is so susceptible to damage by agents that inhibit cell division, such as radiation and anticancer drugs. In the interior of the villus there is a lymphatic vessel called a lacteal. The lacteals are very thin-walled structures and are very difficult to see except when they are full of lymph, particularly when that lymph is full of fat. This is the only mechanism in which fat can be absorbed into the body. Near the lacteals are arteries and veins that are going to participate in absorption. The villi also contain Goblet cells secrete mucous. Intestinal crypts Brunner’s glands are found in the submucosa of the duodenum and secrete alkaline mucus that protects the duodenal mucus membrane against damage from the acidic gastric juice. Lymphoid aggregation known as Peyer’s patches may be present within the lamina propia. Paneth cells are serous cells in the basal portion of the intestinal glands and may play a role in controlling intestinal flora. o Segments of the Small Intestine Duodenum This is 10 inches-1 foot in length. It is the shortest and widest segment in the upper abdominal cavity. It is located mostly to the right and is retroperitoneal, i.e., not suspended by the peritoneum. It curves around the head of the pancreas and terminates at the duodenojejunal flexure. The sphincter of Oddi (hepatopancreatic sphincter), a ring of smooth muscle at the duodenum, controls entry of bile and pancreatic juice. Glands in the submucosa of the duodenum secrete an alkaline mucous that protects the duodenal mucosa from the very acidic chyme as it comes from the stomach. There are some enzymes that are secreted by the duodenum that participate in the digestion of sugars. o Sucrase digests glucose and fructose. o Maltase digests maltose to glucose. o Lactase digests lactose to glucose and galactose. 85% of the adult population lacks lactase and is therefore lactose intolerant. The three classes of enzymes synthesized by the duodenal mucosa include peptidases, enterokinase, and phosphatase. o Aminopeptidase cleaves proteins into amino acids, dipeptides, and tripeptides. o Enterokinase primarily acts to activate trypsin. o Phosphatase is an enzyme that participates in the absorption of calcium by removing phosphate groups, along with magnesium, ATPase, and alkaline phosphatase. Jejunum This is 3 feet and is intraperitoneal. It connects the duodenum to the ileum. Ileum This is 7 feet. This is also intraperitoneal and terminates at the ileocecal junction/valve which serves as a sphincter and connects it to the large intestine. The sphincter is normally closed, but after a meal when the gastroileal reflex increases ileal contractions, it relaxes each time the terminal portion of the ileum contracts allowing chyme to enter the large intestine. A reflex contraction prevents fecal material from moving back into the small intestine. Physiology o Here the most common action is a stationary contraction and relaxation of intestinal segments, with little apparent net movement toward the large intestine. This is called segmentation, and its purpose is to mix the chyme, bringing it into contact with the intestinal wall. These movements are generated via pacemaker cells in the longitudinal smooth-muscle layer. More contractions are seen in the upper segments than the lower, forcing chyme along its path. The “Law of Intestine” states that the mild distention of the intestine produces a contraction of the smooth muscle on the oral side of the distension and relaxation of the smooth muscle on the anal side, producing more movement. The intensity of the segmentation can be altered by hormones, the enteric nervous system, and autonomic nerves. Parasympathetic activity increases the force of contraction, and sympathetic stimulation decreases it. After meals, the contractions cease and are replaced by a pattern of peristaltic activity known as the migrating motility complex. This moves in to the large intestine any undigested material still remaining in the small intestine and also prevents bacteria from remaining in the small intestine long enough to grow and multiply. This process is thought to be due to an intestinal hormone called motilin. o Gastroileal reflex Segmentation intensity in the ileum increases during periods of gastric emptying. o Intestinointestinal reflex Large distension of the intestine, injury to the intestinal wall, and various bacterial infections in the intestine lead to a complete cessation of motility. o As much as 500ml of air may be swallowed during a meal. Most of this air travels no further than the esophagus, from which it is eventually expelled by belching. Some of the air reaches the stomach however, and is passed on to the intestines where its percolation through the chyme as the intestinal contents are mixed produces gargling sounds that are often quite loud. o In the small intestine, monosaccharides and amino acids are absorbed by specific carrier-mediated transport processes in the plasma membranes of the intestinal epithelial cells, whereas fatty acids enter these cells by diffusion. Most mineral ions are actively absorbed, and water diffuses passively down osmotic gradients. Digestion and absorption have been largely completed by the middle portion of the small intestine. The small intestine is very permeable to water, so most of this is absorbed here. o Digestion of Fats Fat intake ranges from 25-160g/day in the typical American diet. Most of this is in the form of triglycerides. Lipids are hydrolyzed by the pancreatic lipase at the surface of the fat droplets. These droplets need to be small, increasing their surface area, to be digested quicker. This process is called emulsification. Emulsification requires mechanical disruption of the larger droplets provided by contractile activity, as well as an emulsifying agent in the form of phospholipids and bile salts. The bile salts also form micelles from triglycerides, which are similar in structure to emulsion droplets, but are much smaller. These consist of bile salts, fatty acids, monoglycerides, and phospholipids. These increase absorption by keeping most of the insoluble fat digestion products in solution, while at the same time replenishing the small amount of products that are free in solution as they diffuse into the intestinal epithelium. These can flow into the capillaries. Fatty acids can move across the epithelium into the columnar epithelial cell where they are combined with other monoglycerides back into triglycerides and moved into chylomicrons, which are packages of triglycerides. The chylomicrons are moved by exocytosis out of the epithelial cell and into the lacteal. The lacteal conducts the lymph back into the circulatory system. Most of the lymph empties back into the circulatory system via the thoracic duct, which empties into the subclavian vein. Dietary triglycerides can be taken up into adipose or liver cells by action of lipoprotein lipase (LPL). It is stored in adipose and used in the liver for energy. Fat essentially delays the digestive process, and so the chyme stays in the small intestine for a longer period of time as digestion of fat requires additional time. Carbohydrates are digested much more quickly than are fats. Also, carbohydrates do not have this inhibitory effect on the digestive process. o Digestion of Proteins 40-50g of protein is required by a normal adult to supply essential amino acids and replace the amino acids converted to urea. A typical American diet contains about 125g of protein per day. This is done by the class of enzymes called proteases. This includes pepsin in the stomach, trypsin and chymotrypsin in the small intestine and pancreas, as well as by carboxypeptidase secreted by the pancreas and aminopeptidase in the membrane of the small intestine. These all cleave off amino acids allowing shorter chains of two or three amino acids to be actively absorbed. Small amounts of intact proteins can cross the membrane via endocytosis and exocytosis. o Digestion of Carbohydrates This ranges from about 250-800g in the typical American diet. 2/3 consists of the plant polysaccharide starch, with the remaining being sucrose and lactose. Starch digestion begins in the mouth with the salivary amylase and continues though the small intestine with pancreatic amylase. These are broken down to the monosaccharides glucose, galactose, and fructose which are later transported across the intestinal epithelium into the blood. Fructose crosses the epithelium by facilitated diffusion, while glucose and galactose undergo secondary active transport coupled with sodium. Large polysaccharides, like cellulose referred to as fiber, is not digested by the small intestine and passed onto the large intestine where it is partially metabolized by the bacteria. Large Intestine, aka Large Bowel Function o Water absorption from indigestible food particles and it’s elimination as semisolid feces. This is the area in which constipation and diarrhea occur. If water is absorbed excessively constipation occurs, and if not, diarrhea is the result. o Vitamin absorption Potassium, folic acid, and several B complex vitamins o Storage and concentration of undigested matter. o 4% of absorption Anatomy o This surrounds the small intestine on three sides. It extends from the ileocecal valve of the small intestine to the anus. It is about 4 feet long and 2.5inches in diameter. Even though it has a larger diameter than the small intestine, the surface area is decreased, since there are no villi. o The mucosa is arranged as a series of densely packed parallel straight tubular glands which are continuations of the Crypts of Lieberkuhn of the small intestine. This is a reduced lamina propia. It is composed of tall columnar epithelium with absorptive cells, goblet cells, and lymph nodes. o Parts Cecum This is sac-like structure lying below the ileocecal valve covered by peritoneum. It is the first part of the large intestine. Humans have a very poorly developed cecum compared to animals that eat plants to digest that material. Colon Consisting of, in order, o Ascending Colon This is against the right abdominal wall. It is usually retroperitoneal, not suspended by the peritoneum. o Hepatic Flexure o Transverse Colon This is between the right and left colic flexures, crossing in front of the duodenum. o Splenic Flexure o Descending Colon This extends downward from the left colic flexure, usually retroperitoneal. o Sigmoid Colon This is an S-shaped segment. Appendix This is a blind sac that has no functional significance in the body, located at the junction of the small and large intestine, coming off of the cecum. The epithelium is columnar. It has a greatly increased proportion of lymphoid tissue in the lamina propia. The lumen of the appendix often appears as triangular in cross section. Enteric bacteria tend to enter this and accumulate, causing inflammation. This leads to acute appendicitis in about 10% of all people in the US. The swelling leads to compromised blood flow and further swelling that may rupture if left unchecked. If the appendix ruptures, it can spill large quantities of bacteria into the peritoneum leading to peritonitis which is an extremely dangerous kind of infection. Symptoms are anorexia and pain that starts in the periumbilical area and travels to the right lower quadrant over McBurney’s point (between the pubic bone and superior ileac crest). Treatment is surgical and should be performed immediately. Rectum This extends from the sigmoid colon to a point in front of the tip of the coccyx within the pelvis. There are extensive goblet cells here with a thick, highly vascular mucosa. Anal Canal This is about 3cm long. It opens to the body exterior at the anus. One sees a transition to stratified squamous epithelium from simple columnar. The outer areas contain apocrine and sebaceous glands, which are large sweat glands Sphincters o Internal anal sphincter This is involuntary and composed of smooth muscle. o External anal sphincter (lower 2/3) This is voluntary and composed of skeletal muscle. Pathology o Hematochezia Fresh rectal bleeding o Melena Digested blood in the stool which is tarry and smelly. Physiology o Absorption is done via active transport of sodium. If fecal material remains in the large intestine for a long time, almost all the water is absorbed, leaving behind hard fecal pellets. o Some bacterial products include gas (flatus), which is a mixture of nitrogen and carbon dioxide, with small amounts of hydrogen, methane, and hydrogen sulfide. This rate of gas formation rises when food are eaten that cannot be digested by intestinal enzymes, but are readily metabolized by bacteria in the large intestine. o Motility The contractions of the smooth muscle here are considerably slower than the small intestine, generally occurring once every 30 minutes. This means that the material here stays for longer periods of time. Three to four times a day, generally following a meal, a wave of intense contractions known as a mass movement spreads rapidly over the colon toward the rectum, coinciding with the gastroileal reflex. With this, the muscle stays contracted for some time. o Defecation This mass movement initiates the defecation reflex, relaxing the internal anal sphincter. The conscious urge to defecate is mediated by stretched mechanoreceptors. The brain centers allow the defecation to be delayed, and the smooth muscles relax. The urge to defecate subsides until the next mass movement. Defecation is completed by contraction of the abdominal and thoracic muscles. This produces an increase in abdominal pressure that is transmitted to the contents of the large intestine and rectum, causing a rise in intrathoracic pressure. This leads to a transient rise in blood pressure as the venous return to the heart is decreased. About 150g of feces is eliminated each day. This includes 100g of water and 50g of solid material, which normally contains bacteria, undigested polysaccharides, bile pigments, cholesterol, and small amounts of electrolytes, mainly potassium. Pathology of the Large and Small Intestines Diverticulum o This is a weak spot in the colon that bulges out. This can collect debris and become inflamed if foreign material is caught. o Diverticulosis is the status of having directiculi. These do not go away. o Diverticulitis is the inflammation of the diverticula, which is seen mostly in the sigmoid colon. It can lead to an obstruction or perforation which can rupture. The inflammation comes and goes, and it may behave like appendicitis. There may be pain or localized tenderness. A palpable mass is often present. Treatment includes antibiotics and a liquid diet. Surgery is required if bad, but much of the colon needs to be removed. Duodenal Ulcer o These are about 10 times more likely to occur than gastric ulcers. They affect about 10% of the US population. Symptoms include epigastric distress 45-60 minutes after meals, nocturnal pain, epigastric tenderness and guarding. Acid is seen in all cases and hypersecretion in some. An ulcer crater or deformity of the duodenal bulb is seen on x-ray or with endoscopy. Stromal (Marginal) Ulcer/ Jejunal Ulcer o This is suspected when there is a history of operation for an ulcer followed by recurrence of abdominal symptoms after a symptom-free interval of months to years. Symptoms include burning, abdominal pain, nausea, vomiting, weight loss, hematemesis (ejection of blood by vomiting), anemia, and occult blood in stool. Pain occurs sooner because of faster emptying time. Gastroenteritis o This is the term used commonly to describe a diarrheal illness (sometimes vomiting). There are roughly 76 million food poisonings/year, with 325,000 hospitalizations and 5,000 deaths. Refrigeration and the proper handing of food are essential. o There are many causes. Viral This is seen more in kids with poor hygiene. It is rare in the US, but it is the #1 killer for kids in the world. The most common agent is rotavirus. Bacterial Ingestion of toxins such as Staph aureus produces toxins before ingestion. Infection with toxigenic organisms such as E. coli or cholera produces toxins after ingestion. This is seen in travelers in Mexico. Infection by enteroinvasive organisms like Salmonella or Shigella invades the mucosa. Symptoms are seen 24-48 hours after the invasion and can last for weeks. This infection can also be due to an imbalance of bacteria due to antibiotics destroying all of the “good bacteria.” This leads to an overgrowth of clostridium dificile. There is also antibiotic-associated colitis and pseudomembranous colitis. Protozoa (Giardia and Entamoeba) This is common in the water systems of other countries. Regional Enteritis o This is a chronic inflammatory disease that may involve the alimentary tract anywhere from the mouth to the anus. The ileum is the principal site of the disease, whether alone or in conjunction with the colon and jejunum. It usually occurs in young adults and has a variable course with exacerbations and remissions. o Symptoms include insidious onset, nausea and vomiting which occurs 4560 minutes after eating, intermittent bouts of diarrhea, low-grade fever, right quadrant pain, and fistula formation. Constipation o This is the retention of fecal material in the GI tract. The primary factor is due to decreased motility. o Symptoms include headache, loss of appetite, nausea, and abdominal distention. The longer the fecal material remains in the large intestine, the more water gets reabsorbed into the body, and the harder and drier the fecal matter becomes. o Treatment includes dietary fiber or laxatives. Diarrhea o This is increased fecal water content and weight, generally greater than 200 g/day. This is due to decreased fluid absorption, increased fluid secretion, or both. It is generally caused by bacteria, protozoans, or viruses. o This can lead to decreased blood volume, potassium depletion, and metabolic acidosis resulting from the loss of sodium, potassium, and bicarbonate ions. Untreated diarrhea can result in death in underdeveloped countries. Prevention in children is generally via ingestion of solutions containing salt and glucose. Inflammatory Bowel Disease o Includes Ulcerative Colitis and Crohn’s Disease. These are similar clinically. Both are systemic diseases and may be accompanied by abdominal pain, diarrhea which may be bloody, fever, joint pains, etc. The symptoms are variable between patients, but both are long-term and wax and wane. o Ulcerative Colitis This is a non-granulomatous, chronic inflammatory disease that affects mainly the left colon, and carries an increased risk for developing cancer of the colon. It is of unknown etiology and is seen mainly in adolescents and young adults. Symptoms include mild abdominal tenderness, weight loss, fever, anemia, and no stool pathogens. Surgery is the best option, because it is definitive. o Crohn’s Disease This is a granulomatous colitis that may affect any part of the GI tract, but has a predilection for the terminal ileum and the colon. . It is a transmural colitis, meaning that it affects all layers of the bowel wall. It is difficult to distinguish from idiopathic ulcerative colitis, which is purely mucosal. Fistulas can form. Symptoms include abdominal cramping, diarrhea and weight loss, erythema nodosum, spondylitis, polyarthritis, and perirectal disease. Treatment includes systemic steroids, enemas, and chemotherapy agents Ischemic Colitis o This is due to interference of blood flow to the colon. Severe ischemia can lead to gangrene. o Symptoms include lower abdominal pain, fever, vomiting, blood and clots in the rectum. Polyps and Cancer o A polyp is a tumorous mass that protrudes into the lumen of the gut. Some polyps have an abnormal epithelial lining and are termed adenomatous polyps. These are precancerous lesions and should be removed. Both benign and malignant tumors may show no symptoms, but bleeding and obstruction may occur. Bleeding may cause weakness, lassitude, and lightheadedness. Obstruction causes nausea, vomiting, and abdominal pain. Malignant lesions produce weight loss and extraintestinal manifestations. o Colon cancer is very common. It accounts for about 15% of all cancer related deaths in the US every year. Early in the course of the disease there are usually no symptoms. Later there may be fatigue, weakness, and anemia. If one is lucky, there is rectal bleeding early-on. Survival is related to the extent of spread at the time of diagnosis. Males are affected more. Symptoms include altered bowel function, blood in feces, unexplained anemia, weight loss, and a palpable mass involving the colon or rectum. The classifications of this cancer include the Astler-Coller and Dukes classification systems. Dukes Classification A Just mucosa B Muscularis/submucosa without lymph involvement C Lymph involvement D Metastasis o Stages A and B have far better prognosis than stages C or D. 5 year survival o A 98% o B 90% o D 0% Because of this major difference in prognosis, it is standard to screen aggressively for colon cancer, and to treat any rectal bleeding in an adult very seriously. Any anemia in an older male should be considered GI cancer until proven otherwise. Squamous Cell Carcinoma of the Anus o These lesions are often confused with hemorrhoids, another common anal disorder. Tumors tend to be annular, invade the sphincter, and spread upward into the rectum. Accessory Structures Liver Functions o Detoxification of blood via sinusoids Many of the toxic substances that enter our bodies will have methyl groups attached to them, causing them to be polar. These are filtered by the kidney and not reabsorbed, so they are eliminated efficiently in the urine. The liver has the ability to change some ingested, accumulated chemicals to be more polar so that they are removed by the kidney. If not secreted, they would lead to liver damage. Many times the byproducts of protein metabolism produce ammonia, which is an extremely toxic substance. The ammonia is converted by the liver into urea to be less toxic. The liver also converts purines into uric acid. It also serves as a blood reservoir. o Carbohydrate metabolism The liver is one of the two areas in the body that store carbohydrates in the form of glycogen. Excess glucose in the blood can be converted by the liver to glycogen or glucose can also be converted to fat. Under situations where glucose is required, the liver can release glucose by glycogenolysis, the breaking down of glycogen into glucose. The liver is the primary site of gluconeogenesis, the production of glucose from non-carbohydrate precursors, primarily amino acids. o Lipid metabolism Triglycerides and cholesterol are synthesized in the liver. The liver excretes cholesterol into the bile. The liver is also the site of ketone body production during fat metabolism. o Protein synthesis and metabolism Albumins are synthesized in the liver. Plasma transport proteins are synthesized in the liver. These are proteins that transport steroid hormones in particular, along with other hormones and iron. Clotting factors such as fibrinogen, prothrombin, and all of the various other proteins that will contribute to the clotting process are synthesized in the liver. o Formation and secretion of bile The liver secretes one pint of bile a day. Bile contains cholesterol and bile salts, which are important for fat absorption. Bile salts are synthesized in the liver. o Makes and stores vitamin A o Stores iron and copper, along with vitamins B12 and D o Produces blood cells in the embryo Anatomy o This is the largest gland in the body. It is located against the right, inferior surface of the diaphragm. o It consists of two lobes separated by the falciform ligament. The right lobe is larger and contains two smaller lobes, the interiorly placed quadrate lobe and the posterior caudate lobe. o The gall bladder is located on the inferior surface of the liver. o The secretory unit is divided into lobules in which hepatocytes are the functional cells. These are epithelial cells grouped together in interconnected plates. Hepatocytes are radially disposed in the liver lobule forming a layer 1-2 cells thick. These cellular plates are directed from the periphery of the lobule to its center forming a spongelike structure. The space between these cellular plates contains liver sinusoids (aka discontinuous capillary), which are lined with a fenestrated layer of endothelium. These are little passage ways in which blood travels. It is almost like the blood is sieved. This exposes the blood to a lot of tissue. Wherever two hepatocytes abut, they delimit a tubular space between them called the bile canaliculus. o Ducts Bile is secreted into the bile canaliculi, draining into collecting ducts which drain ultimately into the common bile duct. The blood supply includes the right and left hepatic arteries. o Kupffer cells are separated from the underlying hepatocytes by the Space of Disse, which contains microvilli of the hepatocytes. Blood fluids readily percolate through the endothelial wall and make intimate contact with the hepatocyte surface. Kupffer cells are phagocytic cells that are found in the wall of the sinusoids. The removal of RBCs is going to result in the production of bilirubin from the hemoglobin that is in the RBCs. o The Portal System Portal systems connect two capillary beds. The hepatic triad consists of the hepatic artery proper, portal vein, and the common hepatic duct. These are present in the corners of the lobules. The blood flow to the liver is about 25% of the cardiac output. The flow is derived from the portal vein (¾) and the hepatic artery. The position of the liver is optimal for gathering, transforming, and accumulating metabolites and for neutralizing and eliminating toxic substances. In a portal system, unlike other parts of the systemic circulation, the blood passes through two sets of capillaries before it returns to the heart. The first set of capillaries is in the walls of the organs of the digestive tract, and the second set (the sinusoids) are in the liver. The hepatic-portal system consists of veins that drain the blood from the abdominal part of the digestive tract, pancreas, spleen, and gallbladder. These veins go to the portal vein which distributes blood to the capillary-like sinusoids of the liver. The blood then dumps into the central veins, which lead to the hepatic vein, later emptying into the inferior vena cava. The significance of this vascular organization is that blood supplied by the hepatic portal vein is rich in amino acids, simple sugars, and other products of digestion but relatively poor in oxygen. The oxygen required to support the metabolic activity of the liver is supplied by a separate pathway. Arterial blood supplied by the hepatic artery. The liver is unusual in that it has a dual blood supply, both arterial and venous. Pathology o Hepatic dysfunction typically leads to stasis of the bile and therefore jaundice. Liver enzymes are generally looked at to assess liver status, although liver function is better assessed by serum albumin levels. The protime level, which is the bleeding time due to clotting factors not producing properly, is also assessed. Jaundice is a yellow discoloration of the skin and sclera (icterus) that occurs when systemic bilirubin levels rise above normal. Cholestasis is the systemic retention of bilirubin and other solutes (mainly bile salts) that are normally excreted by the liver. o Cirrhosis This is the end stage of chronic liver disease. In western countries, cirrhosis is among the top ten causes of death. Anatomically, the liver becomes hard, shrunken, and nodular due to diffuse fibrous bands replacing normal liver lobules. It displays impaired functions and diminished reserve due to a decreased amount of functioning liver tissue. The hepatic portal vein is diverted around rather than passing through the liver. Once cirrhosis develops, it is irreversible. The most common cause is alcoholic liver disease which accounts for 66-70% of cases. Viral hepatitis is responsible for another 10% of cases. Cirrhosis leads to portal hypertension and all clinical consequences, including hemmorrhoidal bleeding, ammonia buildup in the blood, leading to an abnormal mental state. o Hepatitis This is an inflammation/infection of the liver. Elevated liver enzymes damage liver cells in the bloodstream. It is usually nonsymptomatic (subacute) and recovery is 100%. If symptomatic, 90% of patients experience full recovery and 10% develop chronic hepatitis, leading to inflammation, cirrhosis, and cancer. This needs to be treated. Differentiation Acute vs. chronic o Acute hepatitis causes liver cell necrosis and inflammation. It can occur with resolution of the illness and lifelong immunity. Symptoms include malaise, anorexia, nausea, abdominal pain, jaundice, dark urine, fever, rash, arthritis, and itching. o Fulminant or subacute hepatitis is the cause of acute liver injury. It occurs in an overwhelming manner with massive liver cell death due to hepatic necrosis and decreased liver function. There is a high mortality rate, but if the patient survives, liver function is retuned to normal and there is no residual evidence of liver disease. o Chronic hepatitis is liver injury beyond the initial acute stage. This can either be chronic active hepatitis or chronic persistent hepatitis. o The silent carrier state can have little or no liver damage. 2/3 of these patients are unaware that they have it. Types Each different type is encapsulated with different protein coats. They all present with different clinical symptoms. A- Enteric virus (Enterovirus 72) o The incubation period is about 25 days (2-6 weeks). Since this is so long, it is hard to track the origin. A chronic carrier state does not occur and many infected individuals have an asymptomatic infection. It is rarely fatal unless it affects another organ. o Epidemiology In developing countries, asymptomatic children are the reservoir. With improved sanitation, the disease is seen more in adults. There were 7,600 official cases in 2003. 61,000 are estimated. It accounts for 30% of the acute hepatitis cases. The annual incidence in the US is 3.8-32.6/100.000, with the average being 11. The seroprevalence in the US military is 1525%. It is about 30% in homosexual men and 12% in heterosexuals. o Transmission Fecal-oral spread (rare parenteral cases). It is an infectious hepatitis and is very contagious. The virus is transmitted via contaminated water and food from infected individuals. Hepatitis A may be found in daycare facilities. Young children do not become symptomatic, but they shed high titers. The virus is transmitted through contaminated diapers. Common source outbreaks in food handlers, health care workers, and other institutional settings represent only a small number of total cases. o Prevention Handwashing Safer sexual practices Immune Serum Globulin This is highly efficacious (80-90%) when administered at exposure. Recommended for sexual contacts, household contacts, those exposed in daycare facilities, custodial institutions, and travelers. For common source outbreaks, it is usually too late. Hepatitis A Vaccines Types: two inactivated vaccines o Havrix (SKB) o Vaqta (Merck) Very highly immunogenic and efficacious (>95% after two doses). Adverse reactions are very mild. The CDC recommends routine childhood immunizations. o Diagnosis Elevated liver enzymes Acute hepatitis with positive IgM for HAV. B- Hepadnavirus o This is the most common cause of acute hepatitis in the world. o Epidemiology 200,000-300,000 cases/year in the US through the 1980s. Only 73,000 in 2003. Cases in gay men have dropped in recent years, but are now increasing. Concomitantly, the proportion in heterosexual men is also increasing. In highly endemic areas, the carrier rate can exceed 10% with past evidence of infection in 80-90% of the population. 1-1.25 million are chronic carriers in the US. 300-350 million have chronic HBV infections. Persons with chronic infection are the major reservoir of HBV. 20-25% of persons with chronic HBV infection will die prematurely of cirrhosis or liver cancer. HBV may cause up to 80% of all cases of liver cancer and is second only to tobacco among known human carcinogens. No medical treatment is currently available to reliably eliminate or treat chronic infection. o Transmission Humans are the only reservoir for HBV. Perinatal Child to child through skin lesions, bites, and contaminated medical equipment (IV). Adults through sexual encounters, occupational hazards, and pericutaneous via needle sharing and contaminated medical equipment (IV). Incubation period is 2-6 months. Patients with hepatitis B are at significant risk for primary liver cancer. o Laboratory Diagnosis of HBV Antigen Detection Surface protein, central core, nucleocapsid tells us about the acute infection, DNA/RNA, and viral load (PCR) to see if the treatment is working. Serologic markers Antigen (viral proteins) o Immunized patients will not have a positive result. This tells us of active viruses. o HBsAg- surface protein excreted in the serum. o HBeAg- component of the viral core protein. Antibodies o IgM responds to the core protein of HBV. Histology of liver HBV cannot be cultured in standard laboratory tissue culture Found Surface Ab: have had immunization (passive) or have had an infection (active) Core Ab: had prior infection- not possible with immunization Core Ab without Ab: window period. Takes time to develop surface Abs. Surface Ag in blood: has an infection now. IgE is chronic and IgM is acute. o Prevention Post exposure prophylaxis consists of HBIG (0.06mg/kg) within 24-48 hours of exposure in adults and within 7 days of birth of newborns First dose of HBV vaccine Immune Serum Globulin is not very effective. The asymptomatic conversion rate is 22% vs. 4% for HBIG. Vaccines Heptivax no longer available in US, Recombivax (MSD), and Engerix B (S-KB). All are 80-90% effective in clinical trials. They are available in three doses. The protection duration is not known (14 years). Currently, no booster is recommended. Safe in pregnancy and lactation. Efficacy in HIV infection is around 50%. Those recommended are all neonates, and high risk groups, including health care workers, institutionalized patients, dialysis patients, homosexual males, hemophiliacs and blood product recipients, and sexual contact of carriers. o Treatment Interferon/ riboviran C- Flavivirus o This is the most common cause of chronic hepatitis, cirrhosis, and hepatocellular carcinoma. About 80% develop chronic infection. 20% show signs of cirrhosis within 10 years. Predictors are currently unknown regarding who will progress. There is a low spontaneous remission. Long-term sequelae are similar to HBV. o At least 6 different genotypes have been recognized with type 1 being the most common (72%) o Epidemiology It is difficult to determine, because the screening tests are poorly available. There is also a long lag time before seroconversion (4-32 weeks, with an average of 15). Seroconversion can occur up to a year after the acute illness. The immune response is variable. An estimated 150,000 cases/year in the US through the 1990s, and 30,000 in 2003. There is also an estimated 3,500,000 carriers in the US. HCV infections account for >90% of non-A and non-B hepatitis secondary to blood transfusions, IV, etc. The incidence of HCV infection due to blood transfusions has declined by >95% since 1989. >50% of all cases are community acquired with no known risk factors. o Diagnosis is made by antibodies seen in serology, PCR, viral RNA titers and liver biopsies. There is no test for the antigen itself. The cloned virus was used to develop the immunoassay for anti-HCV antibody detection. o No vaccine is available. D- Defective/Incomplete virus (delta agent) o This is an incomplete virus that requires HBV surface antigen for packaging. It exclusively occurs either simultaneously with HBV (co-infection) or following an HBV infection (superinfection). Superinfection of a HBV carrier with HDV increases the severity of the chronic disease. E- Possibly Calcivirus o This is an enteric virus transmitted by the fecal/oral route. It is mostly water-borne and is spread much like HAV. It is isolated in epidemics from underdeveloped countries like Asia, Africa, and Mexico and is rare in the US. The mortality rate is 1-2%, except in pregnant patients where the rate is >20%. o Incubation is 3-6 weeks. Onset is acute, and there is no chronic carrier state. o Serology is the diagnostic test of choice. Summary Size Acute Acute Chronic Hep Viral Spread (nm) Hep Mortality type 27 Yes 0.2% No RNA Fecal/oral 42 Yes 0.2-1% Yes (2-7%) DNA Blood 30-60 Yes 0.2% Yes (85%) RNA Blood 40 Yes 2-20% Yes (2-70%) RNA Blood 32 Yes 0.2% No RNA Fecal/oral There are probably other viruses yet to be found. Alcoholic Liver Disease Fatty infiltration from chronic alcohol consumption leads to hepatitis then cirrhosis. This is a very large public health issue. Wilson’s Disease This is an inherited disorder of copper metabolism that leads to liver, brain, and eye damage. Copper deposits are the problem here, leaving characteristic Kayser-Fleischer rings in the eyes. Tumors The liver and lungs are the most common organs involved in metastatic cancer. The most common cancers in the liver are metastatic from the colon, lung, and breast. Primary liver cancer is very rare in the US, but common in Asian countries due to an increased rate of hepatitis B carrier states. Prognosis is grim with death usually within 6 months of the diagnosis. Virus A B C D E o o o Gallbladder Function o This stores bile that is produced by the liver and concentrates it 5-10 fold. As digestion occurs, the gallbladder ejects this concentrated bile into the duodenum to aid in the digestion and absorption of fats. o The gallbladder can be surgically removed without impairing bile secretion by the liver and into the intestinal tract. Anatomy o This is a pear-shaped sac 3-4” long located on the under surface of the liver. It has a capacity of 30-35ml. o The walls of the gall bladder have three coats Mucous coat- Tall columnar epithelium Fibromuscular coat- Smooth muscle Serous coat o Ducts The cystic duct from the gall bladder and right and left common hepatic ducts combine to form the common bile duct. This enters the duodenum in the area of the pancreatic duct. The point of entry into the duodenum is called the major duodenal papilla of vater. Occasionally the pancreatic duct enters the common bile duct before entering the pancreas, forming an ampulla of vater. Bile o Bile strongly resembles pancreatic juice. About 500ml is secreted per day. o Bile is secreted by the cells of the liver into bile ducts, which drain into the duodenum. Between meals, the duodenal orifice of this duct is closed and bile flows into the gallbladder, where it is stored. When food enters the mouth, the sphincter around the orifice relaxes. As the gastric contents enter the duodenum, the hormone CCK from the intestinal mucosa causes the gallbladder to contract, emptying the concentrated bile into the small intestine. o Ingredients Human hepatic duct bile is 97% water, 0.7% bile salts, 0.2% bile pigments, 0.06% cholesterol, 0.7% inorganic salts, 0.15% fatty acids, 0.1% lecithin (a phospholipids), 0.1% fat, and trace amounts of alkaline phosphatase to neutralize the acid from the stomach. Small amounts of other metabolic end products and trace metals are also found. Bile salts, cholesterol, lecithin, and bile pigments are secreted by hepatocytes. The bicarbonate is secreted by the epithelial cells lining the bile ducts. Bile salts are the most important. These help participate in enterohepatic circulation. The salts are absorbed into the ileum and are returned via the portal vein to the liver, where they are once again secreted into the bile. Bile salts are synthesized in the liver, then transported to the gall bladder, and stored there until the cholecystokinin stimulates its contraction to dump the bile salts into the duodenum. Bile salts, which are cholesterol derivatives, emulsify fat due to their detergent qualities. They are amphipathic, meaning they have both polar and nonpolar parts, allowing the fat to be more water soluble. This is required for the process of the fat absorption. Bile pigments These are formed when the heme portions of hemoglobin are broken down during the destruction of old or damaged erythrocytes in the spleen and liver. The predominant bile pigment is bilirubin. This gives bile its yellowish color. After entering the intestinal tract via the bile, it is modified by bacterial enzymes to form the brown pigments that give feces its characteristic color. Some are actually excreted in the urine, giving it a yellow color. Pathology o Gall Stones This occurs in 10-20% of adults, generally in females, families, 40s/50s, fat, and fertile. Typically these are cholesterol stones. Most patients with smaller gall stones are asymptomatic, but symptoms of painful cramping and squeezing can occur when a stone obstructs bile flow from the gall bladder. Pain is in the right upper quadrant into the right shoulder blade. Inflammation often occurs with stones trying to pass. This is called cholecystitis, and treatment is mainly surgical. The complications that arise generally appear where the gallstone gets stuck. o The gall bladder and pancreas share a duct, so a small gall stone can obstruct pancreatic flow as well leading to pancreatitis. Acute Pancreatitis and biliary tract disease In patients who do not drink alcohol, about 50% of cases of acute pancreatitis are associated with biliary tract disease. In such cases, the mechanism is obstruction of the common bile duct and the main pancreatic duct when a gallstone becomes lodged at the ampulla of Vater. Reflux of bile or duodenal contents into the pancreatic duct leads to parenchymal injury. Others have proposed that bacterial toxins or free bile acids travel via lymphatics from the gallbladder to the pancreas, giving rise to inflammation. In either case, acute pancreatitis associated with biliary tract disease is more common in women. Chronic Pancreatitis and biliary tract disease Chronic pancreatitis results from recurrent attacks of acute pancreatitis. The two major causes of chronic pancreatitis are chronic alcoholism and biliary tract calculi. o HIV Infection and biliary tract disease The protozoan Cryptosporidium is frequently implicated as the cause of the biliary disease typical of HIV. Cryptosporidial cholangitis may present clinically as cholecystitis, sclerosing cholangitis, or papillary stenosis. Spleen Function o Defense This is part of the lymphatic system. It hypertrophies during infectious disease and atrophies with age. As blood passes through the spleen, macrophages remove microorganisms, old red blood cells, and debris from the blood and destroy them by phagocytosis. While lymph nodes serve as the immunologic filters of lymph, the spleen is the immunologic filter for the blood. Promotes antibodies o Serves as a blood reservoir o Hemopoesis- Makes lymphocytes, monocytes, and plasma cells During fetal life, it makes all blood cell types. Anatomy o This is located between the fundus of the stomach and left inferior surface of the diaphragm, above the left kidney. It is approximately 12cm in length. The hilus contains the splenic artery and splenic vein. o This is a large fibrovascular encapsulated organ with an inner connective tissue trabecular framework supporting a reticular connective tissue meshwork. Inside the organ is a trabecular meshwork which consists of white and red pulp. White pulp This is an aggregate of lymphoid tissue containing T and B lymphocytes. It contains lymphatic nodules called splenic corpuscles or Malpighian bodies. Lymphocytes are formed here. Diffuse lymphoid tissue forms a cuff around the arterial branches composing the periarterial lymphocyte sheath (PALS). Red pulp This contains monocytes, free macrophages, granulocytes (neutrophils, basophils, eosinophils), and erythrocytes (red color of red pulp). It acts as a filtration system for damaged or old red blood cells and microorganisms. It is more abundant than white pulp. It is surrounded by anastomizing venous sinuses. The parenchyma of red pulp is composed of diffuse lymphoid tissue, which is highly infiltrated with blood cells. General Physiology Motility Movements o Movement of food from the mouth into the pharynx is a voluntary act. o Movement of food from the pharynx into the esophagus is a reflex act. o Movement of the food through the esophagus is accomplished via peristalsis. Emptying of the stomach is accomplished by gastric peristalsis. Peristalsis then occurs throughout the colon. o The defecation reflex is initiated by stimulation of the rectal mucosa. Types of motility o Tonus contraction These are continual low grade contractions of smooth muscle. o Rhythmic contractions These are elicited by spike potentials. Two types Segmentation- major mixing movement Peristalsis- major propulsive movement Regulation Neural Control o Motility is regulated by the autonomic nervous system via the enteric nervous system, which is the intestinal muscle pacemaker. This is completely independent of the central nervous system. The enteric brain is an integrated system of nervous plexi in the wall of the digestive tract, containing both the myenteric and submucosal plexus. The neurons either synapse with other neurons or end near smooth muscles or glands. Impulses can be sent either up or down the tracts. This contains both adrenergic and cholinergic neurons, as well as neurons that release other neurotransmitters. Serotonin is the chemical transmitter used by the myenteric plexus, a local network of nerve cells in the walls of the esophagus, stomach, and intestine. The GI reflexes are initiated by Distention of the wall of by the luminal contents Chyme osmolarity (total solute concentration) Chyme acidity Chyme concentration of certain digestion products, such as monosaccharides, fatty acids, peptides, and amino acids. o The parasympathetic autonomic nervous system enters via CN X and innervates most of the upper gut, including the esophagus, stomach, pancreas, and upper large intestine. Constant stimulation on the gut muscle creates the “tonus” of the intestinal muscle. The PANS enhances motility and digestive secretions and relaxes muscle sphincters so food can pass. Acetylcholine is the neurotransmitter that stimulates the gut wall. o The sympathetic nervous system supplies the entire GI tract. Norepinephrine inhibits the enteric nervous system, therefore inhibiting contractions of the smooth muscle. The SANS thus slows and blocks passage of food, decreases contraction and motility, causes loss of tonus, constriction of sphincters, and decreases secretion of digestive juices. Hormonal Control o Endocrine hormones, which last longer than neurotransmitters, reach their target through the circulation. They are produced in the epithelium of the stomach and small intestine. Paracrine hormones are vasoactive intestinal polypeptides, such as somatostatin. Somatostatin reaches target cells by diffusing through intercellular spaces after traveling from the blood. Gut hormones Gastrin o The introduction of a food bolus from the esophagus into the stomach stimulates gastrin, which produces many events, eventually leading to the release of chyme into the small intestine. This is secreted by the stomach and stimulates HCl secretion. o There are three phases of gastric secretion. These do not necessarily occur in this order and one at al time. They may all occur simultaneously. Cephalic Phase The sight, smell, and taste of food stimulate the PNS which activates the initial stage of the whole digestive process. Here some gastrin is secreted. Gastric Phase As the food bolus accumulates in the stomach, the distention of the stomach is going to have a stimulatory effect on the PNS. As the peptides are digested, the amino acids that are liberated are also going to have stimulatory effects on acid secretion. When the secretion of acid results in a pH of less than 2.5 in the stomach, further gastrin secretion is inhibited to prevent further HCl secretion. Intestinal Phase Arrival of chyme into the intestine distends the intestine which inhibits the parasympathetic stimulation of motility, which is further inhibited by the presence of fat in the intestine. The gastric motility is inhibited, allowing the chyme to remain in the small intestine so that it can be fully digested and absorption can take place. Here CCK and GIP are involved. Secretin o This is secreted by the small intestine and stimulates water and bicarbonate secretion in the pancreatic juice and potentiates the action of cholecystokinin, which acts on the pancreas. This is stimulated by increased duodenal acidity and gastrin. Cholecystokinin (CCK) o This is secreted by the small intestine in the presence of fatty acids and amino acids. o Its most important action is to stimulate contraction of the gall bladder, but it also stimulates the secretion of pancreatic juice enzymes and inhibits gastric motility. Gastric inhibitory peptide o Glucose-dependent Insulinotropic Peptide (GIP) o This is an inhibitory hormone that inhibits gastric motility and stimulates secretion of insulin from the endocrine portion of the pancreas. This is to prevent additional chyme from being released into the small intestine too quickly. It is stimulated by chime. Glucagon-like-peptide o This is an inhibitory enzyme in the ileum and colon. It is also stimulated by chyme and inhibits gastric motility and the secretion/ stimulation of insulin. Thyroid hormone increases both the rate of secretion of the digestive juices and the motility of the GI tract. Stimulation of the lateral hypothalamic area causes a tremendous increase in appetite. Digestive Enzymes Absorption Most absorption occurs in the small intestine. This is the passage of substances, such as digested foods, water, salts, and vitamins through the intestinal mucosa into the blood or lymph. Absorption may occur though diffusion, osmosis, filtration, or active transport. Absorption of lipids occurs passively as these substances pass through the lipid bilayer of a cell membrane. Water soluble substances like sugars and amino acids use carriers to enter cells. Some absorptive processes require energy (active transport) while others do not (facilitated diffusion). Pancreatic Secretions The exocrine pancreas is the source of an enormous number of digestive enzymes. These secretions go into the pancreatic duct which later joins the common bile duct that enters the duodenum. The pancreatic juice is alkaline and has a high HCO3 content (about 113 meq/L vs. 24 meq/L in the plasma). About 1400ml of pancreatic juice is secreted per day. Composition of normal pancreatic juices include cations (Na, K, Mg, H), anions (HCO3, Cl, HPO3, SO4), albumin, globulin, and digestive enzymes. o The bicarbonate released from the pancreas will neutralize the HCl being released from the stomach. Its release is analogous to the release of HCl, with the directions being reversed. o Digestive Enzymes Amylase digests starch to maltose and glucose Trypsinogen, a precursor to trypsin, is activated by enterokinase. It is present in the brush border of the epithelium, and it acts to cleave peptide bonds to digest protein. Once trypsin is activated, it is going to activate chymotrypsin and elastase. These cleave only internal peptide bonds. Carboxypeptidase cleaves off the carboxyl end of a peptide. Phospholipase cleaves the fatty acids from phospholipids. Lipase cleaves fatty acids from glycerol to digest triglycerides. Cholesterolesterase releases cholesterol from other molecules. Ribonuclease cleaves RNA into shorter chains. Deoxyribonuclease cleaves DNA into shorter chains. Pancreatic juice is the most versatile of the digestive secretions, because its enzymes are capable of nearly completing the digestion of food in the absence of all other digestive secretions. These enzymes require a pH close to neutrality for optimal activity, and this is provided by the alkaline secretion of the pancreatic intercalated duct cells. Its secretion increases directly after a meal, mainly as a result of stimulation by the hormones secretin and CCK. An additional 25% of secretions are controlled by parasympathetic nerves in response to such things as the taste of food, distention of the stomach, etc. The secretory units are compound tubuloacinar glands. Serous cells surround a central lumen which goes on to form an intercalated duct. These are lined with cuboidal epithelial cells. The digestive enzymes secreted are discharged into the intercalated duct which eventually joins to form the pancreatic duct. The pancreatic duct receives branches from lobules and joins the common bile duct to empty into the duodenum. o The blood supply is from the lineal (splenic) artery. Gastrointestinal Drugs Agents Useful in Treating Peptic Ulcers o H2 Blockers/ Receptor Antagonists These can be purchased over the counter. Agents Cimetidine (Tagamet) o This is a short-acting agent that attaches to histamine receptors in parietal cells. o Adverse effects include blockade of testosterone receptors Famotidine (Pepcid) Nizatidine (Axid) Ranitidine (Zantac)- Longer acting Mechanism Decreased gastric acid and pepsin secretion, as well as decreased vasodilation via H+K+ ATP-ase decreasing the H+ in the lumen. Therapeutic Uses Treat peptic ulcer disease Treat gastroesophageal reflux disease (GERD) Treat immediate hypersensitivity response o Proton Pump Inhibitors This is the most effective method of preventing acid secretion. It is converted to the active form by acid. Agents Omeprazole (Prilosec) Lansoprazole Esomeprazole (Nexium) Mechanism- Inhibits H+, K+-ATPase Therapeutic Use- Treats GERD o Antacids These neutralize stomach acids (pH 1.4-4.0) that can cause heartburn in the lower esophagus. Systemic These are highly soluble and are rapidly absorbed in the gut. Sodium bicarbonate (Baking Soda) o This causes bloating, hypertension, and acid rebound. This should not be used with deep ulcers, because it causes perforation and inflammation. These may produce systemic alkalosis, making nonsystemic antacids more desirable. Nonsystemic Constipating agents constrict the sphincter. o Calcium carbonate (Tums, etc) o Aluminum hydroxide gel (Amphogel) o Aluminum phosphate (Alternagel) o Magnesium hydroxide Laxatives o Magnesium hydroxide (Milk of magnesia) This works via an osmotic mechanism o Magnesium trisilicate gel Mixtures o Maalox (magnesium and aluminum oxides) o Creamalin o Mylanta o Beano o Cholinergic blockers Pirenzapine Block M1 receptors on paracrine cells Block M3 receptors on parietal cells Dicyclomine (Bentyl)- Relaxes GI muscles to treat GI spasm. Atropine, Methantheline, Propantheline, Tricyclics o Misoprostol (Cytotec) Mechanisms This is a prostaglandin analog that inhibits cAMP, thus decreasing acid secretion. It also stimulates secretion of mucous. It is used in conjunction with NSAIDs. Adverse effects- Diarrhea and abortion o Sucralfate (Carafate) Mechanism- This coats the ulcer crater by binding to necrotic ulcer tissue, acting as a barrier to HCl and pepsin. o Colloidal bismuth Mechanism- These preparations coat and bind to both gastric and duodenal ulcer tissue. They protect the ulcer from acid and pepsin. o Carbenoxolone and Bismuth subcitrate o Antimicrobials Prokinetc Drugs o These stimulate gut activity and are used to treat pathologies such as diabetic gastroparesis (no churning due to diabetes mellitus) and GERD. o Cholinergic agonists Types Bethanechol Metoclopramide (Reglan) o This is the most widely used antiemetic that blocks D2 receptors. o It increases the tone of the lower esophageal sphincter, increases the force of gastric contractions, improves gastro-duodenal coordination, enhances gastric emptying, as well as sensitizing receptors in the gastric muscles to acetylcholine to increase stomach activity. o Adverse Effect- can develop EPS Mechanism- Stimulate muscarinic receptors in the stomach. Adverse effects- Increased salivation, lacrimation, sweating. o Cholinesterase inhibitors act in a similar manner to cholinergic agonists. o Motilin receptors agonists (GI hormones) Erythromycin (E-mycin) and derivatives enhance GI contractions and increase the rate of gastric emptying. Emetics o These induce vomiting by irritating the stomach lining. They can use used with accidental ingestion of poisons. o Types Apomorphine Syrup of Ipecac Antiemetics o These suppress vomiting. o Types Metoclopramide (Reglan) This is a prokinetic drug that treats gastric hypomotility. Ondansetron (Zofran) This blocks the 5-HT3 receptors that increases the tone of lower esophageal sphincter, increases the force of gastric contractions, improves gastro-duodenal coordination, and increases stomach emptying. Prochlorperazine (Compazine)- most effective This is a major tranquilizer, along with chlorpromazine. It comes in the form of a suppository. Dronabinal (Marinol) and Nabilone are used for cancer patients. H-1 Blockers such as diphenhydramine, dimenhydrinate, and promethazine. Scopolamine- These patches can be used behind the ears. Laxatives (Cathartics) o These are used to treat constipation when other measures such as increased water, fiber, and exercise fail or cannot be used. Other valid uses include preparation for surgery, acute poisoning, severe cardiac problems. A condition called “The Laxative Habit” can be encountered in which the taking of laxatives everyday can make the gut hypotonic and lose tone. This is common with seniors. o Irritants Agents Emodin Castor oil Phenolphthalein (Ex-Lax) Bisacodyl (Dulcolax) Ducosate sodium (Colace) Mechanisms Stimulates the accumulation of electrolytes and water in the lumen of the muscles of the large intestine, increasing intestinal motility. Adverse effects Cramping Intestinal atony o Emollients Agents Mineral oil (Liquid petrolatum) Insoluble dietary fiber (vegetables) Hydrophilic colloids o Agar o Psyllium seed (Metamucil) o Methylcellulose (Citrucel) Mechanisms Decreases fluid absorption, therefore decreasing motility. o Osmotic agents Agents Magnesium sulfate (Epsom salt) Magnesium hydroxide (Milk of magnesia) Lactulose (Cephulac) Glycerin suppositories PEG Electrolyte Solution (GoLYTELY, CoLYTE) o Polyethylene glycol o Cleans out gut pre-surgery Mechanism Increases osmotic pressure in the intestine, thereby increasing the bulk and stimulating the muscles. Antidiarrheal Agents o Opium derivatives (Morphine) Diphenoxylate (in Lomotil)- contains some atropine Codeine Loperamide (Imodium) o Bismuth subsalicylate (Pepto-Bismol) o Clonidine (Catapres) o Kaolin o Pectin o Activated charcoal- absorbs poison o Major tranquilizers, such as trifluoperazine and chlorpromazine. o Antimicrobials Diagnostic Agents- Barium salts