Blood Clotting
advertisement

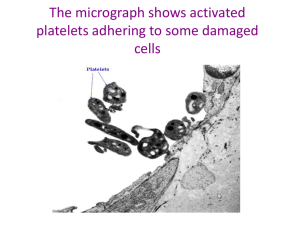
BLOOD CLOTTING 1. Describe the major phases of hemostasis. 2. Describe the mechanisms that stimulate platelet activation. 3. Describe the roles of von Willebrandt factor and Glycoprotein IIb/IIIa in hemostasis. 4. Know the pathway involved in the formation of prostaglandins and thromboxanes and how it affects platelet function. Know where aspirin inhibits this pathway. 5. Describe how thrombin cleavage of fibrinogen converts it to fibrin fibers and facilitates blood clotting. 6. Describe the intrinsic and extrinsic pathways for activating blood clotting. 7. Describe how prothrombin is cleaved by factor X into active thrombin in the final common pathway for blood clotting. 8. Describe the role of vitamin K in hemostasis. 9. Understand how -carboxyglutamate (Gla) resides in prothrombin facilitate its cleavage to thrombin. 10. Describe the actions of warfarin and heparin in inhibiting blood clotting. 11. Describe how protein C and protein S function to limit blood clotting. 12. Understand how plasminogen activators function to dissolve blood clots. BLOOD CLOTTING 1. Hemostasis- stop bleeding from damaged blood vessels a. Rapid constriction of vessel b. Aggregation of platelets to form plug c. Clotting- web forms consisting of fibrin polymers; traps platelets and RBCs; contracts to squeeze out fluid; generates seal 2. Platelet activation a. Aggregation of platelets Produced by splitting off from megakaryocytes; no nucleus or protein synthesis; replaced after 10 days Circulate in blood in inactive state Injury to blood vessel wall exposes extracellular matrix (ECM) components, especially collagen, that bind to receptors on platelets to initiate activation; platelet forms projections; dump secretary granules; contents of granules activates additional platelets Activated platelets adhere strongly to ECM and to each other to form aggregates Von Willebrandt factor (vWf) present in blood plasma; important for associating platelets with ECM; binds collagen and receptors on platelets (integrins and other receptor complexes) Glycoprotein IIb/IIIa (type of integrins) are receptors for fibrinogen; crosslinking of platelets occurs by fibrinogen and other proteins forming complex with these receptors GPIIb/IIIa inhibitors inhibit platelet aggregation; used during angioplasty and for acute coronary syndromes b. Signaling pathways in platelet activation Activation of many signaling pathways; one important pathway involves formation of prostaglandins and thromboxanes Activation of platelets involves activation of phospholipase A2; produces arachidonic acid from cleavage of membrane phospholipids; cyclooxygenase converts arachidonic acid to a prostaglandin (PGG2) In platelets, PGG2 converted to thromboxane A2 (TxA2); TxA2 acts both within cell and released to neighboring cell; causes Ca2+ release in cytosol which promotes dumping of secretary granules, platelet aggregation, vasoconstriction In endothelial cells, PGG2 converted to PGI2 (a prostacyclin); PGI2 released and enters platelets; inhibits platelet aggregation by activating adenylate cyclase; inactivates platelets that leave damaged area; TxA2 inhibits adenylate cyclase which prevents platelets in damaged area from being inactivated c. Inhibiting platelet aggregation with aspirin 1 TxA2 can be bad for some older people because platelet aggregation can interfere with blood flow Aspirin is cyclooxygenase inhibitor; inhibits platelet aggregation by lowering TxA2 levels; also lowers PGI2 levels, but not dramatically because endothelial cells, unlike platelets, have nuclei and continually synthesize more cyclooxygenase 3. Formation of fibrin network a. Conversion of fibrinogen to fibrin fibers Fibrinogen major blood plasma protein; conversion of soluble fibrinogen to insoluble fibrin from proteolytic cleavage by thrombin; fibrin spontaneously associates into long fibers Fibrinogen molecule composed of six polypeptide chains; two each of , , and chains (2,2,2); three-stranded coiled-coil interaction of , , and chains; two complexes linked by disulifde bonds Thrombin cleaves off four small peptides at N-terminus of each and chain known as fibrinopeptides A and B; resulting molecule called fibrin monomer Monomers associate as half-staggered arrays to form fibers; results in unstable “soft clot” Stable “hard clot” formed by cross-linking monomers; transamidation reaction forms isopeptide bonds between side chains at C-termini of chains; catalyzed by factor XIII b. Signaling pathways for stimulating fibrinogen cleavage Cascade of proteases; proteases present in blood plasma as inactive precursors prior to cleavage; most synthesized in liver; each protease cleaves the next protease in pathway, which activates it; results in amplification of signal Two signaling pathways activated by different stimuli; both feed into to common pathway for final steps - Intrinsic- everything needed for pathway contained in blood; stimulated by contact of blood with negatively charged surface, such as glass tube or surface exposed from ruptured vessel; end step is cleavage of factor X to activate it - Extrinsic- requires component from surrounding tissue to stimulate; need tissue factor (thromboplastin) that is normally buried below endothelium; exposed by injury; activates factor VII which cleaves factor X to activate it Common pathway - Activated factor X cleaves inactive prothrombin to generate active thrombrin, which then cleaves fibrinogen - Factor X cleaves at two site on prothrombin; N terminal peptide released; peptides designated A and B linked through disulfide bond in active thrombin c. Role of vitamin K in clotting 2 Various blood clotting factors undergo functionally important posttranslational modification in liver before release; addition of carboxyl group to glutamic acid residues to produce -carboxyglutamate (Gla) Prothrombin has ten Gla residues at N-terminal region; prothrombin cannot be cleaved without Gla modification Vitamin K is cofactor for enzyme that produces Gla modification Dicoumarol (found in spoiled sweet clover) and warfarin (used as rat poison) interfere with vitamin K cycle and inhibit clotting; can be used as blood thinner drugs d. Function of Gla residues in prothrombin cleavage Prothrombin must associate with negatively charged phospholipid membrane to be cleaved by factor X, which occurs at site vessel injury Prothrombin-membrane association requires Ca2+, which forms bridges linking Gla residues to phospholipids Higher negative charge from Gla modification provides stronger attraction for Ca2+ Ca2+ chelating agents prevent clotting of blood samples 4. Blood clotting disorders a. Hemophilia A; inherited deficiency of factor VIII; X-linked b. Von Willebrandt disease; inherited deficiency of vWf Platelet adhesion depends on vWf Factor VIII forms complex with vWf which increases stability of factor VIII; loss of vWf decreases stability of factor VIII 5. Controlling blood clotting a. Inappropriate blood clots major cause of heart attacks and strokes b. Protein C – Protein S Excess thrombin binds to endothelial cell receptor called thrombomodulin Thrombin bound to thrombomodulin activates protein C, which then forms complex with protein S called activated protein C complex (APC) APC anchored by protein S to platelet surface at clot by calcium bridges APC destroys activated factor V and VIII by proteolysis Inherited deficiency of protein C or protein S, or point mutation in APC cleavage site of factor V increase risk of venous thromboembolism c. Heparin Antithrombin is protein present in blood that inhibits clotting by inhibiting most proteases of clotting system; weak activity strongly enhanced by binding glycosaminoglycan heparin 3 Heparin secreted in response to injury by mast cells that line blood vessels to limit spread of clot; useful as blood thinner drug d. Plasminogen activators Plasmin is protease that cleaves fibrin to dissolve blood clots; inactive plasminogen present in blood and cleaved into active plasmin by various proteases known as plasminogen activators Tissue-type plasminogen activator released from endothelial cells; useful drug for dissolving blood clots in stroke and heart attack patients 4