biochem 45 [4-20
advertisement
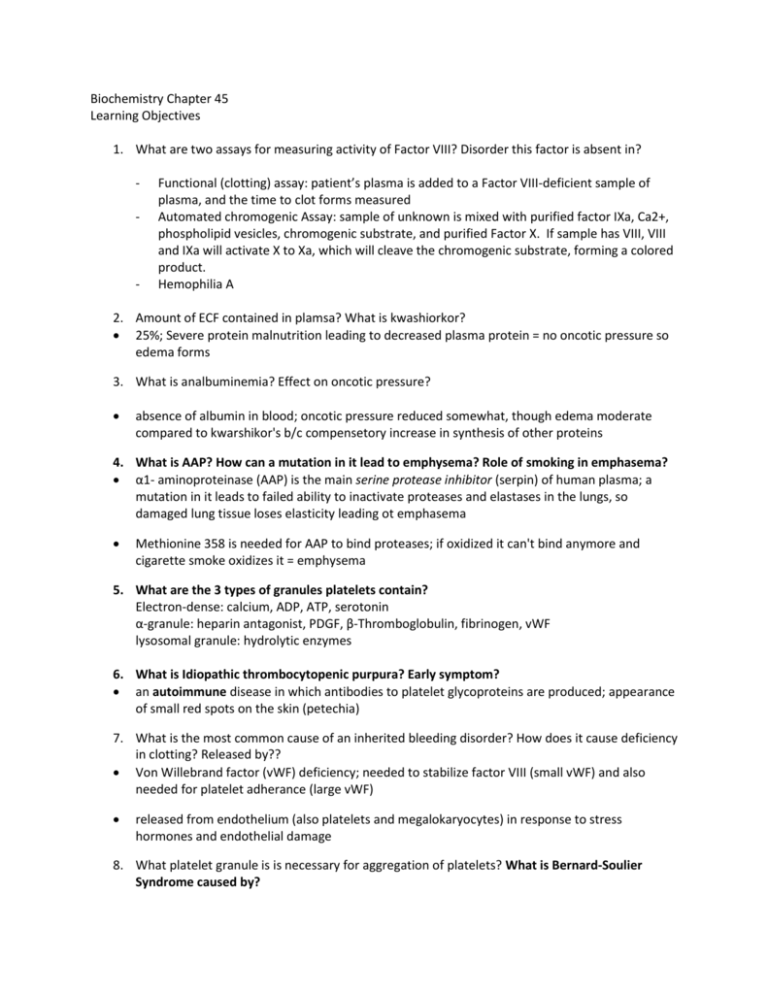
Biochemistry Chapter 45 Learning Objectives 1. What are two assays for measuring activity of Factor VIII? Disorder this factor is absent in? - - Functional (clotting) assay: patient’s plasma is added to a Factor VIII-deficient sample of plasma, and the time to clot forms measured Automated chromogenic Assay: sample of unknown is mixed with purified factor IXa, Ca2+, phospholipid vesicles, chromogenic substrate, and purified Factor X. If sample has VIII, VIII and IXa will activate X to Xa, which will cleave the chromogenic substrate, forming a colored product. Hemophilia A 2. Amount of ECF contained in plamsa? What is kwashiorkor? 25%; Severe protein malnutrition leading to decreased plasma protein = no oncotic pressure so edema forms 3. What is analbuminemia? Effect on oncotic pressure? absence of albumin in blood; oncotic pressure reduced somewhat, though edema moderate compared to kwarshikor's b/c compensetory increase in synthesis of other proteins 4. What is AAP? How can a mutation in it lead to emphysema? Role of smoking in emphasema? α1- aminoproteinase (AAP) is the main serine protease inhibitor (serpin) of human plasma; a mutation in it leads to failed ability to inactivate proteases and elastases in the lungs, so damaged lung tissue loses elasticity leading ot emphasema Methionine 358 is needed for AAP to bind proteases; if oxidized it can't bind anymore and cigarette smoke oxidizes it = emphysema 5. What are the 3 types of granules platelets contain? Electron-dense: calcium, ADP, ATP, serotonin α-granule: heparin antagonist, PDGF, β-Thromboglobulin, fibrinogen, vWF lysosomal granule: hydrolytic enzymes 6. What is Idiopathic thrombocytopenic purpura? Early symptom? an autoimmune disease in which antibodies to platelet glycoproteins are produced; appearance of small red spots on the skin (petechia) 7. What is the most common cause of an inherited bleeding disorder? How does it cause deficiency in clotting? Released by?? Von Willebrand factor (vWF) deficiency; needed to stabilize factor VIII (small vWF) and also needed for platelet adherance (large vWF) released from endothelium (also platelets and megalokaryocytes) in response to stress hormones and endothelial damage 8. What platelet granule is is necessary for aggregation of platelets? What is Bernard-Soulier Syndrome caused by? Electron dense granules=> ADP- needed for platelet activation and aggregation; syndrome caused by defect in GP1b of platelets that is needed to adhere to sub endothelial vWF 9. What is the clinical picture for thrombotic thrombocytopenic purpura ? disease that causes formation ofmicroclots of aggregated platelets, so leads to hemolytic anemia (thrombi damage RBCs) and as platelets are used up from excessive clotting can eventually lead to internal hemorrhage (b/c nothing to protect); sporadically caused by antibody to vWF-metalloprotease, which lyses clots 10. Which pathway of the clotting cascade initiates the clotting response? Sustains it? What is the role of factor XIIIa? extrinsic initiates; intrinsic sustains; XIIIa catalyzes a transamination b/t Gln and Lys forming a COVALENT cross-link (stronger clot) (note XIIIa only enzyme in clotting cascade that is not a serine protease) 11. What amino acids make up the catalytic triad of thrombin, trypsin, and chymotrypsin? all serine proteases w/ triad of aspartate-histidine-serine in active site. AHS 12. Why is Vitamin K necessary for blood coagulation? Why do we use Warfarin? vitamin K is needed for a sort of “pre-activation” in the platelets: the gamma-carboxylation of glutamate residues of factors II, VII, IX, X, protein C, protein S; reaction causes oxidation of Vit. K to an epoxide that must be reduced for reuse by vitamin K epoxide reductase warfarin is structurally similar to vitamin K and competes for the gamma-carboxylation glutamate residues of clotting factors so they cannot bind phospholipid membrane sites of activation (used commonly as a rat poison) ---note that Pharmacology says warfarin goes right after VKORC1! 13. What is the role of proteins S and C? What does a deficiency in these enzyme/cofactor cause? Protein C (with is cofactor/anchor protein S) proteolytically deactivates factors Va and VIIIa and triggers release of prostacyclin (PGI2) that reduces platelet aggregation; deficient in these enzymes = venous thromboembolism 14. What is the Factor V Leiden mutation? PBL case This is a point mutation in the Factor V gene that causes the replacement of an Arg with a Gln in the preferred site for cleavage by activated protein C, rendering Factor Va Leiden resistant to APC. Heterozygotes have a 6-8x higher risk of DVT while homozygotes 30-140 fold increased risk 15. What are serpins? How are they related to heparin? Serpins are Serine Protease Inhibitors that are naturally occurring inhibitory proteins present in high concentration in the plasma. They inhibit proteases involved in coagulation and clot dissolution. They have an active site that is an ideal substrate for serine protease. Once bound, it attacks a peptide bond located within the serpin and forms a tight enzyme-inhibitor complex. The activity of thrombin is controlled by the serpin antithrombin III (ATIII). One molecule of ATIII irreversibly inactivates one molecule of thrombin. Heparin binds to lysyl residues on ATIII and dramatically accelerates its rate of binding to thrombin. 16. What are 3 reasons for the thromboresistance of normal vascular endothelium - Endothelial cells are negatively charged: repels negative platelets - Synthesize prostaglandin I2 (PGI2) and nitric oxide: vasodilators, inhibitors of aggregation - Synthesize heparan sulfate and thrombomodulin that inhibit thrombin 17. What is t-PA? How released? Where is it produced? Tissue plasminogen factor; activated protein C (APC) triggers its release and simultaneously inactivates an inhibitor of plasminogen activator (PAI-1); It has a high binding affinity for fibrin and plays a major role in fibrolysis; produced by vascular endothelial cells 18. What do streptokinase and t-PA have in common? Which has more side effects? Is cheaper? both approved for treatment of myocardial infarction; they restore blood flow to heart by causing clot dissolution streptokinase has more side-effects (produced by beta-hemolytic streptococci) and is substantially cheaper. You are advised to only use it once per patient because of antibodies 19. What is hemophilia A, B? Hemophilia A is the most frequently encountered disorder of blood coagulation in humans. It, and hemophilia B are X-linked and lead to inability to convert prothrombin to thrombin, thus impaired clotting. Hemophilia A is a problem is factor VIII, Hemophilia B is in IX BIOCHEMICAL COMMENTS SECTION BETTER ADDRESSED IN PHARMALOGY 22--> SEE THESE NOTES FOR THIS INFO