3.Pulmonary function testing
advertisement

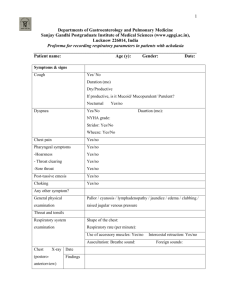
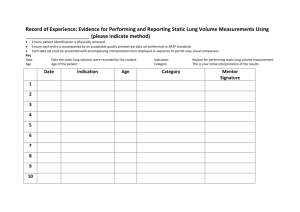
THE KURSK STATE MEDICAL UNIVERSITY DEPARTMENT OF SURGICAL DISEASES № 1 PULMONARY FUNCTION TESTING Information for self-training of English-speaking students The chair of surgical diseases N 1 (Chair-head - prof. S.V.Ivanov) BY ASS. PROFESSOR I.S. IVANOV KURSK-2010 Pulmonary function testing Pulmonary function testing includes both simple spirometry and sophisticated physiologic testing. Pulmonary function abbreviations are explained in Physiology Normally, the volume and pattern of ventilation are initiated by neural output from the respiratory center in the brain stem. This output is influenced by input from carotid (PaO2) and central (PaCO2, [H+]) chemoreceptors; proprioceptive receptors in muscles, tendons, and joints; and impulses from the cerebral cortex. Nerve impulses travel from the respiratory center via the spinal cord and peripheral nerves to the intercostal and diaphragmatic muscles. Normal gas exchange occurs if inspired gas is transmitted through structurally sound, unobstructed airways to patent, adequately perfused alveoli. Normally, alveolar ventilation ( A) and perfusion ( ) are well matched and proportional to the metabolic rate, and arterial blood gas tensions are maintained within a narrow range. Static Lung Volumes and Capacities Static lung volumes reflect the elastic properties of the lungs and chest wall. Vital capacity (VC or "slow VC") is the maximum volume of air that can be expired slowly after a full inspiratory effort. Simple to perform, it is one of the most valuable measurements of pulmonary function. Because VC decreases as a restrictive lung disorder (eg, pulmonary edema, interstitial fibrosis) worsens, it can be used along with the diffusing capacity to follow the course of such a disorder and its response to therapy. The VC also reflects the strength of the respiratory muscles and is often used to monitor the course of neuromuscular disorders. (See also the discussions of maximal voluntary ventilation and maximal inspiratory and maximal expiratory pressures, below.) Forced vital capacity (FVC), similar to VC, is the volume of air expired with maximal force. It is usually measured along with expiratory flow rates in simple spirometry. The VC can be considerably greater than the FVC in patients with airway obstruction. During the FVC maneuver, terminal airways can close prematurely (ie, before the true residual volume is reached), trapping gas distally and preventing its measurement by the spirometer. Total lung capacity (TLC) is the total volume of air within the chest after a maximum inspiration. Functional residual capacity (FRC) is the volume of air in the lungs at the end of a normal expiration when all respiratory muscles are relaxed. Physiologically, it is the most important lung volume because it approximates the normal tidal breathing range. Outward elastic recoil forces of the chest wall tend to increase lung volume but are balanced by the inward elastic recoil of the lungs, which tends to reduce it; these forces are normally equal and opposite at about 40% of TLC. Loss of lung elastic recoil in emphysema increases FRC. Conversely, the increased lung stiffness in pulmonary edema, interstitial fibrosis, and other restrictive disorders decreases FRC. Kyphoscoliosis leads to a decrease in FRC and in other lung volumes because a stiff, noncompliant chest wall restricts lung expansion. Inspiratory capacity is the difference between TLC and FRC. The FRC has two components: residual volume (RV), the volume of air remaining in the lungs at the end of a maximal expiration, and expiratory reserve volume (ERV); ERV = FRC - RV. The RV normally accounts for about 25% of TLC. Changes in RV parallel those in the FRC with two exceptions: In restrictive lung and chest wall disorders, RV decreases less than do the FRC and TLC, and in small airways disease, premature closure during expiration leads to air trapping, so that the RV is elevated while the FRC and FEV1 remain close to normal. In COPD and asthma, the RV increases more than the TLC does, resulting in some decrease in the VC. The characteristic abnormality seen in obesity is a decreased ERV, caused by a markedly decreased FRC with a relatively well-preserved RV. Dynamic Lung Volumes and Flow Rates Dynamic lung volumes reflect the caliber and integrity of the airways. Spirometry records lung volume against time during an FVC maneuver. Forced expiratory volume in 1 sec (FEV1) is the volume of air forcefully expired during the first second after a full breath and normally accounts for > 75% of the FVC. This value is recorded both as an absolute value and as a percentage of the FVC (FEV1 %FVC). The mean forced expiratory flow during the middle half of the FVC (FEF25-75%) is the slope of the line that intersects the spirographic tracing at 25% and 75% of the FVC. The FEF25-75% is less effort-dependent than the FEV1 and is a more sensitive indicator of early airway obstruction. Prolongation of expiratory flow rates is increased by bronchospasm (in asthma), impacted secretions (in bronchitis), and loss of lung elastic recoil (in emphysema). In fixed obstruction of the upper airway, flow is limited by the caliber of the narrowed segment rather than by dynamic compression, resulting in equal reduction of inspiratory and expiratory flow rates. In restrictive lung disorders, increased tissue elastic recoil tends to maintain the caliber of the larger airways so that at comparable lung volumes, flow rates are often higher than normal. (Tests of small airways function, however, may be abnormal.) Retesting pulmonary function after the patient inhales a bronchodilator aerosol (eg, albuterol, ipratropium) provides information about the reversibility of an obstructive process (ie, the asthmatic component). Improvement in FVC or FEV1(L) of > 15 to 20% is usually considered a significant response. In patients with airway obstruction, absence of a response to a single exposure to a bronchodilator, however, does not preclude a beneficial response to maintenance therapy. In bronchoprovocation testing, a significant decrease in flow rates after inhaling methacholine (a cholinergic drug) may indicate asthma. Maximal voluntary ventilation (MVV) is determined by encouraging the patient to breathe at maximal tidal volume and respiratory rate for 12 sec; the volume of air expired is expressed in L/min. The MVV generally parallels the FEV 1 and can be used to test internal consistency and estimate patient cooperation. The MVV can be estimated from the spirogram by multiplying the FEV1(L) × 40. When the MVV is disproportionately low in a patient who seems to be cooperating, neuromuscular weakness should be suspected. Except in advanced neuromuscular disease, most patients can generate fairly good single-breath efforts (eg, FVC). Because the MVV is much more demanding, it can reveal the diminished reserves of weak respiratory muscles. The MVV decreases progressively with increasing weakness of the respiratory muscles and, along with maximum inspiratory and expiratory pressures, may be the only demonstrable pulmonary function abnormality in patients with moderately severe neuromuscular disease. The MVV is important preoperatively because it reflects the severity of airway obstruction as well as the patient's respiratory reserves, muscle strength, and motivation. Flow-Volume Loop The flow-volume loop is generated by continuously recording flow and volume with an electronic spirometer during a forced inspiratory and expiratory VC maneuver. The shape of the loop reflects the status of the lung volumes and airways throughout the respiratory cycle. Characteristic changes occur in restrictive and in obstructive disorders. The loop is especially helpful in detecting laryngeal and tracheal lesions. It can distinguish between fixed obstruction (eg, tracheal stenosis) and variable obstruction (eg, tracheomalacia, vocal cord paralysis) of the upper airway. Lung Mechanics Airway resistance (Raw) can be directly measured with a body plethysmograph, which determines the pressure required to produce a given flow. More commonly, however, Raw is inferred from dynamic lung volumes and expiratory flow rates, which can be obtained more easily. Maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) measure the strength of the respiratory muscles as the patient forcibly inhales and exhales, respectively, through a closed mouthpiece attached to a pressure gauge. Like the MVV, maximal pressures are reduced in neuromuscular disorders (eg, myasthenia gravis, muscular dystrophy, Guillain-Barré syndrome). These pressures, along with the VC, are often measured at the bedside of an intubated patient to predict the success of weaning from ventilatory support. Diffusing Capacity The diffusing capacity for carbon monoxide (DLCO) can be determined from a single breath (DLCOSB). The patient inspires a known small amount of carbon monoxide (CO), holds his breath for 10 sec, then exhales. A sample of alveolar (end-expired) gas is analyzed for CO, and the amount absorbed during that breath is then calculated and expressed as mL/min/mm Hg. A low DLCO probably reflects abnormal ventilation/perfusion ratios ( / ) in diseased lungs rather than physical thickening of the alveolar-capillary membrane. However, this test relies on the avidity of Hb for CO and thus is affected by the volume of blood and the quantity of desaturated Hb in the lungs at the time of testing. The DLCO is low in processes that destroy alveolar-capillary membranes (eg, emphysema and interstitial inflammatory or fibrotic processes) and in severe anemia, in which less Hb is available to bind the inhaled CO. The DL CO is artifactually low if the patient's Hb is already occupied by CO (eg, if he smokes within several hours of the test). The DLCO increases with polycythemia and with increased pulmonary blood flow, as may occur in early heart failure. Small Airways Studies In the normal lung, bronchi < 2 mm in diameter constitute < 10% of the total airway resistance, but their aggregate surface area is large. Disease affecting primarily the small (peripheral) airways can be extensive yet not affect the Raw or any tests dependent on it (eg, FEV1). This is true of early obstructive lung disease and interstitial granulomatous, fibrotic, or inflammatory disorders. The status of the small airways is reflected by the FEF 25-75% and by expiratory flow rates in the last 25 to 50% of the FVC, best determined from the flow-volume loop . More sophisticated tests of small airways function have been devised--eg, frequency-dependent changes in lung compliance (dynamic compliance), closing volume, and closing capacity. In general, such tests add little to those more readily available and have little place in the clinical laboratory. Monitoring Respiration During Sleep Central and obstructive sleep apnea can be distinguished by monitoring respiration during sleep. An oximeter on the ear or finger monitors O2 saturation. A catheter placed in a nostril measures end-tidal PCO2 (PETCO2) and monitors airflow. Chest wall motion is monitored by a strain gauge or impedance electrodes. In obstructive sleep apnea, airflow at the nose ceases despite continued excursion of the chest wall, O2 saturation drops, and PETCO2 increases. In central apnea, chest wall motion and airflow cease simultaneously. Ordering Pulmonary Function Tests As a general preoperative screen, determination of the FVC, FEV 1, FEV1 %FVC, and MVV usually suffices. Testing should be performed before chest or abdominal surgery in smokers > 40 yr old and in patients with respiratory symptoms. In patients with suspected laryngeal or tracheal disorders, a flow-volume loop should be requested. If weakness of the respiratory muscles is suspected, the MVV, MIP, MEP, and VC are the appropriate tests. A complete set of pulmonary function tests should be requested when the clinical picture does not coincide with the data obtained by simple spirometry or when more complete characterization of an abnormal pulmonary process is desired. A complete set includes determination of static and dynamic lung volumes, DLCO, flow-volume loop, MVV, MIP, and MEP. However, extensive testing is tiring, time-consuming, expensive, and unnecessary for adequate clinical assessment of most patients. Periodic determinations of VC and DLCO usually suffice to monitor patients with interstitial lung disease. Measurements of Arterial Blood Gases The PaO2 and PaCO2 reflect the adequacy and efficiency of gas exchange between the lungs and venous blood. The PaCO2 is normally maintained in the narrow range of 35 to 45 mm Hg. An increase in CO2 production ( CO2) normally results in an appropriate increase in ventilatory drive and in alveolar ventilation ( A), preventing any increase in PaCO2. The A and PaCO2 are inversely proportional at any given level of CO2 (ie, A × PaCO2 = k × CO2). The PaO2 is considerably lower than the inspired PO2 (PIO2) and somewhat lower than the PaO2. The PO2 in inspired gas is calculated as the fractional percentage of inspired O2 (FIO2) times barometric pressure (PB). For room air at sea level, PI O2 = 0.21 × 760 mm Hg ~= 160 mm Hg. As inspired gas enters the upper airway, it becomes saturated with water vapor. At sea level and at normal body temperature (37° C [98.6° F]), water exerts a partial pressure of 47 mm Hg. After saturation with water vapor, the PO2 is slightly diluted; PO2 = 0.21 (760 - 47) ~= 149 mm Hg. For practical purposes, the PO2 of inspired gas as it enters the alveoli can be approximated by multiplying the FIO2 × 7 (eg, for room air, 21 × 7 = 147 mm Hg; for 40% O2, 40 × 7 = 280 mm Hg). Because total gas tension in the alveoli must remain constant, the greater the amount of CO2 entering the alveoli, the lower the PAO2 must be. In a patient on a normal diet, the respiratory quotient (ie, the ratio CO2/ O2) is not unity but is about 0.8, thus every 1 mm PACO2 effectively displaces 1.25 mm PAO2. (Respiratory quotient is affected by the relative quantity of fat and carbohydrate in the diet, increasing to about 1 with a high-carbohydrate diet and decreasing to about 0.7 with a high-fat diet.) For clinical purposes, the PACO2 can be assumed to equal the PaCO2. Thus, the PAO2 can be calculated by the equation PAO2 = FIO2 (PB - PH2O) - 1.25 PaCO2. For room air, with a PaCO2 of 40 mm Hg, the PAO2 = 147-50 = 97 mm Hg. Normal A is about 5 L/min, as is perfusion ( ). If A and were perfectly matched (ie, / = 1), PAO2 and PaO2 would be equal. The overall / ratio of normal lungs is, however, about 0.8. This degree of / mismatch results in a PaO2 that is 5 to 15 mm Hg lower than the PAO2, equivalent to shunting 2% of pulmonary arterial (mixed venous) blood directly into the pulmonary venous circulation without participation in gas exchange. The difference between PAO2 and PaO2 (A - aDO2) directly reflects the degree of mismatching of and , ie, the severity of intrinsic lung disease. The PaO2 for a healthy 20-yr-old breathing room air is about 90 mm Hg. The normal PaO2 at age 70 is about 75 mm Hg. This physiologic decrease in Pa O2 with age results from a decrease in lung elastic recoil (senile emphysema), leading to closure of small airways in the tidal volume range, with a further decrease in the overall / ratio of the lungs. A lower-than-normal PIO2 necessarily leads to hypoxemia, without any alteration in / relationships and without an increase in the A - aDO2. Passenger cabins of commercial aircraft are pressurized to the equivalent of an altitude of 1500 to 2400 m--similar to breathing 17% O2 at sea level. Hypoxemia can be offset somewhat by hyperventilation, but a PaO2 as low as 30 mm Hg has been reported in patients with COPD during commercial flights. Hypoventilation alone can lead to hypoxemia, even without intrinsic lung disease. If the PaCO2 increases from 40 to 80 mm Hg, as might occur with a sedative overdose, the PaO2 must decrease by 50 mm Hg (ie, 40 × 1.25), from 90 to 40 mm Hg. When hypoventilation is identified as the main cause of hypoxemia (ie, hypoxemia with a normal A - aDO2), the diagnoses listed in should be considered. In patients with COPD, loss of tissue elastic recoil, bronchospasm, and inspissated secretions combine to worsen / relationships in the lungs. Areas with low / ratios result in hypoxemia; areas with high ratios lead to wasted ventilation (dead space), increasing the work of breathing and contributing to hypercapnia. As long as the airways are not totally occluded, hypoxemia is readily corrected with small increments in FIO2, because there is a strong gradient of diffusion to the areas of alveolar hypoxia. Characteristically, an FIO2 of 24 to 28% is adequate to correct hypoxemia due to / imbalance. Areas that are not ventilated at all (because the alveoli are totally collapsed or filled with fluid) but that are perfused result in right-to-left shunting of blood. Shunting results in hypoxemia that is more refractory to increases in FI O2 because O2 cannot reach the gas-exchanging surface. Such situations often require mechanical ventilation and positive end-expiratory pressure (PEEP) to increase the FRC and open closed airways. Impaired diffusion of O2 across the alveolar-capillary membrane is probably not a significant cause of resting hypoxemia, except at high altitude. Split-Function Ventilation/Perfusion Scanning Preoperative quantitative ventilation/perfusion lung scanning (split-function scanning) is a noninvasive technique useful for predicting postpneumonectomy lung function. It is most useful in patients with lung cancer, who frequently have asymmetric lung function. A radioactive isotope is injected (perfusion) or inhaled (ventilation) as is done for a conventional lung scan. After equilibration, the percentage of isotope in each lung is determined, usually in the posterior projection with the patient supine. Predicted postpneumonectomy FEV1 equals percentage of radionuclide uptake in the noncancerous lung multiplied by preoperative FEV1 (in liters). A value of < 0.8 L (or < 40% of that predicted for the patient) indicates serious pulmonary disability and the likelihood of unacceptably high perioperative morbidity and mortality. Transdiaphragmatic Pressure Measurement Transdiaphragmatic pressure measurement permits quantitative assessment of the severity of diaphragmatic weakness. This procedure can be used to diagnose bilateral diaphragmatic paralysis. Balloon manometers are placed in the distal esophagus and in the stomach, and pressure across the diaphragm is measured. This procedure indirectly determines tension in the diaphragm during an inspiratory effort. Normally, the gradient across the diaphragm at total lung capacity is > 25 cm of water. The diagnosis of unilateral paralysis, suggested by asymmetric elevation of the affected hemidiaphragm on x-ray, can be confirmed by fluoroscopy. During a forced inspiratory maneuver (the "sniff" test), the unaffected hemidiaphragm descends forcefully, increasing intra-abdominal pressure and pushing the paralyzed hemidiaphragm cephalad (paradoxical motion). However, fluoroscopy is inaccurate for the diagnosis of bilateral paralysis. Exercise Testing Repeating physiologic measurements during or after exercise can help determine the relative roles of heart and lung disorders in the etiology of dyspnea, assist in disability evaluations, and monitor the effectiveness of a rehabilitation program. Patients with suspected asthma but normal resting exams and spirometry may wheeze during exercise, especially when inhaling cooled air. A decrease in VC or FEV1 of > 15% is considered abnormal, indicating hyperactive airways. A decrease in DLCO or oxygenation during exercise indicates abnormal gas exchange and may be the first physiologic indication of pulmonary vascular or interstitial lung disease. In patients with heart disease, stroke volume may not increase appropriately with exercise. Consequently, heart rate increases disproportionately to the O2--a result of increased VD/VT (dead space ventilation), hypoxemia, or fatigue of the respiratory muscles.