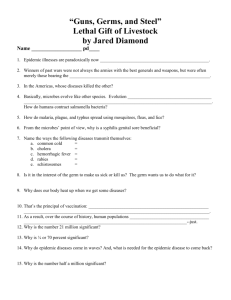
Disease detectives Notes - Raleigh Charter High School
advertisement

Disease detectives Notes Epidemiology- study of how disease is distrubuted is population’s abd the factors that inluence or determine this distrubution Objectives: -identify cause and risk factors of a disease -how is it transmitted -determine extent of disease in community -study natural history and prognosis of disease -identify high risk groups: find specific factors/change -Primary Prevention: (ultimate goal) prevent in healthy people beofre Secondary Prevention: already developed disease in early stages intervene Population based approach: preventative measure applied to population High-risk approach: applied to high-risk group of people -Diagnosis and prognosis are often population based- “what’s going around” (helpful- not always occur) 1) Determne whether association is b/w factor (ie environmental exposure) or Characterisitic and development of disease in question=study characteristic of groups and individual a) find differences- make sure c comparable data and try to find why (high risk people? Ethnicity?) disease is almost always based on interactiony, even if genetic. -Clinical disease- characterized by signs and symptoms -Host must be susceptible -Disease tranmitted directly (person to person) or indirectly (water supply) -Non-clinical disease: prechricail disease- not yet clinically apparent subclinical disease- not clinically apparent and never will be presistant (chronic)- persists for years -Latent: infection with no active mult. Of virus -Horizontal transmission: person to person -Vertical tansmission: generation to generation (usually genetic) -Host: ie person Agent: bacteria Environment: contaminating water supply Vector: ie mosquito -Carrier state: person harbors organism but is not know to be infected and can infect others (usually not very many) -Endemic: habitual presence of disease in given geographic area Epidemic: occurance in a community or region of a group of illnesses of a similar nature -Pandemic: worldwide epidemic -Single or multiple exposures -Periodic or continuous contamination -Common vehicle exposure: ie people sick from eating same food -Single exposure, common vehicle outbreak- explosive (all increase at once) and limited to people sharing exposure -Determinants of disease outbreaks: depends on the numble of people susceptible or number immune -Herd immunity: resistance of a group to an attack by disease because a large proportion of group members are immune- if a large percentage of the population is immune, everyone is usually protected not just the immune because disease spreads from person to person (must have random mixing of people, constant mixing, can’t have reservoir outside human host for disease -Incubation period: interval from receipt of infection to onset of the clinical illness -Epidemic circle: distribution of the times of onset of the disease -When did the exposure take place? -When did the disease begin? -What was the incubation period? -attack rate = # at risk that develop illness # at risk -Primary case: person aquires disease from exposure -Secondary case: person aquires disease from primary case -Sources of data: -interviews -physician records -hospital records -Incidence: number of new cases of disease that occur during specified period of time in population at risk (measure of risk) -Cumulative incidence: when entire population is at risk -Determines incidence: # of new cases occuring in a population during a specified period of time x 1,000 = incidence per 1,000 # of people at risk of developing it during that time -Incidence rate: denominator is sum of different times individuals were at risk -Prevalence (per 1,000): determines the number that have the disease -point (specific point in time) vs. period (any time in a certain period) prevalence -prevalence = incidence x duration of disease number of affected people in population at a specific time number of people in population at that time x 1,000 -Spot map: map, each point is case -Annual mortality rate (per 1,000 in population) = total # of death from --x 1,000 (-can make it age, disease, # of people at risk at a specific time cause, etc. specific) -Case fatality rate (%) = # of people dying during a specific time after the disease onset/ diagnosis # of people with disease x 1,000 -Proportionate mortality = # of death from ---- to ---- x 100 total # of deaths from ---- to ----Mortality rate is a good reflection of incidence rate when: case/ fatality rate is high and duration of the disease is short. -Stardardized mortality ratios = observed # of deaths per year expected # of deaths per year -Cohort: group of people who share the same experience -Mortality changes may be due to: quality of life -Median survival time: length of time that ½ the study population survives -Relative survival rate = observed survival in people with disease expected survival if disease was absent -Randomized Trial: -Case study: need a control -Historical controls: look at records of past patients treated differently -Simultaneous non-randomized controls, randomization -Cohort studies: group of exposed and group of non-exposed individuals and follows up to compare incidence of the disease, incidence of exposed: a/a + b not: c/c + d -Concurrent prospective study: investigator identifies original population at the beginning and follows through time… takes at least 20 years retrospecitve cohort study- use historical data -Must have an idea of possible cause / exposure to do cohort- easier when time b/w exp. and outcome is short -Case-control study: people with disease and people without disease determine proportion exp. and not (& controls) a/a + c > b/b + d -Group matching: proportion of controls of certain characteristics are identical to proportion of cases with same -Individual matching: control selected of similar variables of concern (age, race, etc.) -Problem: limitation of recall and recall bias cross-sectional studies- both disease and exp. are determined simultaneously (snapshot of population) -Outbreak: more cases of a disease than expected in an area, group of people or period of time (epidemic = large # of people and large area) -Cluster: aggregation of cases public health surveillance investigate for control and prevention, severity and risk to others research and training if cases continue occurring- control cases extent and pop’n @ risk to prevent if almost over- investigate to ID source Steps: 1. prepare for field work 2. establish existence 3. verify diagnosis 4. define identify cases 5. orient data: time, place, person 6. develop hypotheses 7. evaluate hypotheses 8. refine hypotheses and carry out additional studies 9. control and prevention measures 10. communicate findings #1: Research disease and gather equip, and supplies, make arrangements, consult all parties for role in invest. And local contacts #2. determine expected # of cases for area in the time frame (compare current and previous comparable data) health dept. surveillance records local sources (death records etc.) estimates from neighboring states/ national data or telephone survey # reported cases greater than expected may not mean an out break (change in reporting case def. nat. local awareness population size) #3. Ensure problem was properly diagnosed, review clinical findings and lab results and lab tech, look at techniques being used, visit ill people and ask questions #4. establish case der (standard criteria) includes: clinical information, characteristics of affected people, info about location/places, specification of time when it occurred; confirmed, probable or possible c= lab verification prob= clinical identify and count cases, determine size and geographic extent, look at health care facilities (calling/ visiting = actual surveillance), alert public through media, conduct survey of population, collect info for line listing (11= table, each column representing variable), identifying info, demographic info, clinical info, risk factor info #5. Descriptive epidemiology- describe what has occurred in population under study characterizing by time: epidemic curve (tells where you are in course of epidemic, maybe future, maybe estimate time period of exposure, infer: common source exposure? Person to person spread? Must know: time of onset of illness for each person -consider overall shape, period of time people are exposed, unit ¼ to 1/3 incubation period, minimum, average, max incubation period -steep slope and gradual climb = point/ single source epidemic (all cases with incubation period) if exp is prolonged = continuous common source epidemic = plateau - person to person spread = series of progressively taller peaks 1 incubation period apart, outliers and information! Characterizing by place: “spot map” of area- clustering indicates focal source or personto-person spread; scattering = common source (can be misleading- # distribution, use attack rate) Characterizing by person: use characteristics (age and sex esp) of population , summarize #6. hypothesize- source of agent, mode (vehicle/vector) of transmission, exposures causing disease – should be able to be tested – talk to a few people, use descriptions, epidemiology