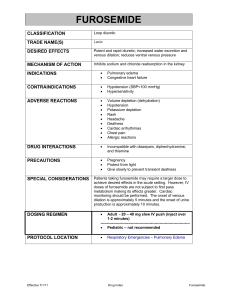
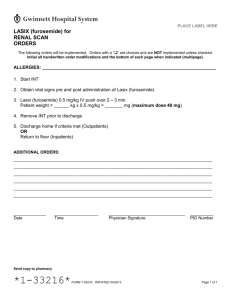
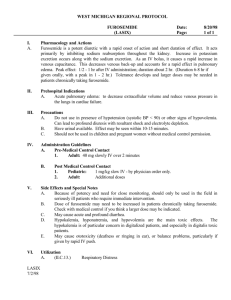
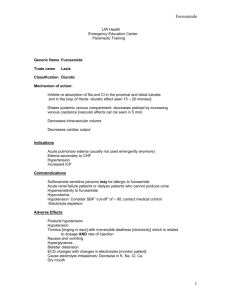
Pharmaceutical care
advertisement

Module 3. Pharmaceutical care during OTC medications vacation. Text test questions: 1. The drug applied at the case of hypersusceptibility to nitroglycerine for removing attack of angina pectoris A. Aspirin B. Atropine C. Piracetame D. Papaverine E. * Molsidomine 2. All of the following statements concerning nitroglycerin are correct EXCEPT: A. It causes an elevation of intracellular cGMP. B. It undergoes significant first-pass metabolism in the liver. C. It may cause significant reflex tachycardia. D. * It significantly decrease AV conduction. E. It can cause postural hypotension. 3. The clot aggregation blocker oppressing the adenosine absorption and reducing its enzyme destruction A. Papaverine B. Propranolol C. Reserpine D. * Dipiridamole E. Trental 4. What group does Trimetazidine belong to? A. Adrenomimetics B. Cholinoblockers C. * Cardioprotectors D. Sympatholitics E. Diuretics 5. The cardioselective beta-adrenoblocker A. * Bisoprolol B. Adrenalin C. Riboxinum D. Enalapril E. Nifedipine 6. The drug applied for the medical treatment of ischemic heart disease A. Sympatholitics B. * beta-adrenoblockers C. alpha-adrenoblockers D. Myorelaxants E. M-cholinomimetics 7. Which of the following adverse effects is associated with nitroglycerin? A. Hypertension B. * Throbbing headache C. Bradycardia D. Sexual dysfunction. E. Anemia. 8. Which drug belongs to the beta-adrenoblockers’ group? A. Nitroglycerine B. * Metoprolol C. Captopril D. Nifedipine E. Furosemidum 9. All of the following mechanisms of action correctly match a drug EXCEPT: A. Quinidine: Blocks Na+ channels B. Brethylium: Blocks K+ channels C. Verapamil: Blocks Ca++ channels D. Propranolol: Blocks beta-adrenoreceptors E. * Procainamide: Blocks K+ channels. 10. The action of nitroglycerine and others organic nitrates is caused by A. The blockade of potassium channels B. The blockade of sodium channels C. The blockade of calcium channels D. * The release of nitrogen oxyde in the vessel walls E. The excitation of beta2 -adrenoreceptors vessels 11. The efficiency of Nifedipine at arterial hypertension is caused by A. * The dilation of vessels B. The rise of myocardium contractility C. The decline of renine production D. The decline of diuresis E. The rise of diuresis 12. Which drug belongs to the Calcium-channel blocker group? A. Papaverinum B. Atenolol C. * Verapamil D. Furosemidum E. Anaprilinum 13. The drug applied for the medical treatment of ischemic heart disease A. alpha-adrenoblockers B. Sympatholitics C. Diuretics D. M-cholinomimetics E. * Nitrates 14. Which one of the following statements is INCORRECT? A. Lidocaine must be given parenterally. B. * Lidocaine is used mainly for atrial arrhythmias. C. Procainamide is associated with a reversible lupus phenomenon. D. Quinidine is active orally. E. All antiarrhythmic drugs can suppress cardiac contractions. 15. The basic principle of Nifedipine action A. It rises the activity of potassium channels B. It blockades beta2-adrenoreceptors C. The release of nitrogen oxide D. * It blockades the calcium channels L-type E. It blockades beta1 -adrenoreceptors 16. The basic effect of nitroglycerine A. Strengthening diuresis B. * Dilation of arterioles and venules C. Oppression of heart contraction D. Anti-inflammatory action E. Rise of myocardium contractility 17. The drug related to the group of calcium antagonists A. Reserpine B. Apressinum C. * Nifedipine D. Prazosinum E. Papaverini hydrochloridum 18. Which drug decreases the demand in oxygen due to the blockade of the sympathetic innervation? A. Molsidomin B. * Atenolol C. Pentoxiphylline D. Papaverinum E. Nitroglycerine 19. An efficiency of beta-adrenoblockers at angina pectoris is explained by A. * The removal of the sympathetic influences on the heart because of the blockade of the betaadrenoreceptors B. The expansion of the coronal vessels C. The increase of sympathetic influences on the heart D. The increase of cardiac abbreviations E. The decline of thrombocyte aggregation 20. Which one of the following statements is INCORRECT? A. Quinidine prolongs repolarization and the effective refractory period. B. Mexiletine shortens repolarization and decreases the effective refractory period. C. * Propranolol increases phase 4 depolarization. D. Verapamil shortens the duration of the action potential. E. Amiodarone prolongs repolarization. 21. The drug, applied sublingually at the attack of angina pectoris A. Isosorbide dinitrate B. Riboxinum C. Pentoxiphylline D. Atenolol E. * Nitroglycerinum 22. The drug of the group of nitrates with the prolonged action at the ischemic heart disease A. Validolum B. Losartan C. * Sustac D. Magnesium sulfate E. Captopril 23. Which drug belongs to the group of beta-adrenoblockers A. Nitroglycerine, Molsidomine B. * Nebivolol, Atenolol C. Pentoxiphylline, Papaverinum D. Nifedipine, Verapamil E. Captopril, Enalapril 24. Which drug belongs to the group of calcium ions antagonists? A. Molsidomine, Nitroglycerine B. Anaprilinum, Atenolol C. Pentoxiphylline, Papaverinum D. * Amlodipine, Verapamil E. Captopril, Enalapril 25. Which one of the following statements about antiarrhythmic drugs is CORRECT? A. * They may act by converting unidirectional block to a bidirectional block. B. They often cause an increase in cardiac output. C. As a group they have mild side effects. D. They all affect Na+ channels in the cell membrane. E. They are equally useful in atrial and ventricular arrhythmias. 26. Which drug belongs to the inhibitors of ACE A. Nitroglycerine, Molsidomine B. Anaprilinum, Atenolol C. Pentoxiphylline, Papaverinum D. Nifedipine, Verapamil E. * Lisinopril, Enalapril 27. Indicate the antiarrhythmic drug A. Nitroglycerin B. Isosorbiti dinitras C. Sustac D. Validolum E. * Procainamide (Novocainamide) 28. Indicate the antiarrythmic drug which exerts membrane-stabilizing action. A. * Quinidine sulfate B. Isadrinum C. Digoxin D. Nitroglycerin E. Atenolol 29. Indicate the antiarrytmic drug of adrenoblockers group A. Amiodaron B. * Metoprolol C. Verapamil D. Asparcam E. Nitroglycerin. 30. Indicate the peculiarities of the action of quinidine upon heart. A. * Increase of the effective refractory period. B. Decrease of the effective refractory period. C. Increase of the conduction of myocardium. D. Inhibition of the conduction of myocardium. E. Increase of the cardic automatism. 31. The major drawback to antianginal use of propranolol is: A. * Exacerbation of congestive heart failure B. Increased blood pressure C. urine retention D. blurred vision E. diabetes-like hyperglycemia 32. Indicate the mechanism of verapamil action. A. Blockade of beta-adrenoceptors of the heart. B. * Blockade of calcium channels of the cardiomyocyte membranes. C. Blockade of potasium channels of myocytes. D. Inhibition of phosphodiesterase . E. Inhibition cholinesterase. 33. Indicate the pharmacological effect of verapamil. A. Cardiotonic effect. B. Hypertensive effect. C. * Antiarrhythmic effect. D. Diuretic effect. E. Antibacterial effect. 34. Which drug is used for ischemic heart disease, hypertension and cardiac arrhythmias? A. * Bisoprolol B. Sustac C. Nitroglycerine D. Novocainamidum E. Validolum 35. To indicate the possible side effect of Propranolol? A. * Bronchial spasm B. Tachycardia C. Rise of arterial pressure D. Ortostatic collapse E. Development of tolerance 36. What antiarrhythmic drug is paraaminobenzioc acid derevate? A. * Novocainamidum B. Quinidinum C. Verapamilum D. Xycainum E. Dipheninum 37. What antiarrhythmic drug has local anaesthetic activity? A. Novocainamidum B. Quinidinum C. Verapamilum D. * Xycainum E. Dipheninum 38. For treatment of what arrythmias Lidocaine is the most effective? A. * Ventrical tachyarrhythmia B. Atrium tachyarrhythmia C. Atrio-ventrical block D. Sino-auricular block E. Chronic paroxismal arrhythmia 39. For treatmant of what kind of arrythmia cardiac glycosides are contraindicated? A. * Ventricula tachyarrhythmia B. Atrium tachyarrhythmia C. Extrasystolia D. Flutering of atrium E. Chronic paroxismal arrhythmia 40. Isosorbide dinitrate is used: A. Antiarrhythmic action is via alpha-adrenergic blockade B. Ventricular premature depolarizations C. * Angina pectoris prophylaxis D. Conversion of atrial fibrillation to sinus rhythm E. Treatment of ventricular fibrillation 41. What medicine is a drug of choice for treatment of ventricular arrythmia? A. Novocainamidum B. Quinidinum C. * Xycainum D. Dipheninum E. Verapamilum 42. When quinidine is administered to a patient with atrial fibrilation? A. the ventricular rate may increase dangerously B. arterial hypotension usually results if the drug is administered intravenously 43. C. thrombi attached to fibrillating atria may embolize A. * all are correct B. none are correct 44. To indicate medication of Nitroglycerine of prolong action A. * Sustac B. Amoidaronum C. Molsidominum D. Fenigidinum E. Anaprilinum 45. Indicate the side effect of nitroglycerine A. Itching of skin B. Bradicardia C. Rise of arterial pressure D. * Headache E. Intestine atony 46. Which antianginal drug provokes bronchial spasm? A. Sustac B. * Propranolol C. Nitroglycerine D. Fenigidinum E. Molsidominum 47. Why during attack of angina pectoris Sustac is not prescribed orally? A. Brief action B. Causes tachycardia C. * Long latent period D. Causes hypotension E. Causes tolerance 48. Indication to Sustac. A. * Prophylaxis of attacks of angina pectoris B. Removal of attacks of angina pectoris C. Medical treatment of acute heart attack D. Medical treatment of high blood pressure illness E. Medical treatment of paroxismal tachycardia 49. Agents which may lower circulating plasma lipids include: A. Clofibrate B. Nicotinic acid C. Cholestyramine D. Dextrothyroxine E. * All are correct 50. Which medication is drug of choice at attack of angina pectoris? A. Sustac B. Molsidominum C. * Nitroglycerine D. Anaprilinum E. Fenigidinum 51. Which from the antianginal agents can be applying for the removal and for prophylaxis of attacks of angina pectoris? A. * Trinitrolong B. Nitroglycerine C. Sustac D. Corvatonum E. Validolum 52. Why is not it impossible to apply nitroglycerine in case of high intracranial pressure? A. Increase arterial pressure B. Causes bradycardia C. * Increase intracranial pressure D. Decrease intracranial pressure E. Provoke angina pectoris 53. Increases transmembrane action potential duration: A. Lidocaine B. * Quinidine C. Atenolol D. Digoxin E. Esmolol 54. Which from agents is used for ischemic heart disease and hypertension? A. * Nifedipine B. Sustac C. Nitroglycerine D. Novocainamaidum E. Aspirine 55. Indicate possible side effect of propranolol? A. Hypertension B. Tachycardia C. * Bradycardia D. Оrtostatic collapse E. Development of tolerance 56. The patient suffers on the ischemic heart disease. Which from the adopted antianginal drugs has coronary dilation and antiplatelet action? A. * Dipiridamolum B. Acetylsalicylic acid C. Validolum D. Nitroglycerine E. Molsidominum 57. Extensively metabolized by circulating enzymes: A. Quinidine B. Lidocaine C. Nicotinic acid D. Cholestyramine E. * Neither 58. To indicate mechanism of Са2+ antagonists hypotensive action A. Decrease the tonus of vasomotor centers B. Block the postsynaptic beta-adrenoreceptors C. Block the sympathetic ganglions D. * Block the calcium channels E. Stimulate the production of prostaglandins 59. Which one of the following is the most common side effect of antihyperlipidemic drug therapy ? A. Elevated blood pressure B. * Gastrointestinal disturbance C. Neurological problems D. Heart palpitations E. Migraine headaches 60. To indicate side effect of Clophellinum (Clonidine) A. Increasing of arterial pressure B. Increasing of intraocular pressure C. * Dryness in the mouth D. Increasing of glands secretion E. Increasing of intestine motility 61. To indicate the antihypertensive drug used for the medical treatment of hypertensive disease with tachycardia and extrasystoles. A. Methyldopa B. Reserpinum C. * Bisoprolol D. Clophelinum E. Dibazolum 62. What diuretic is used for the removal of hypertensive crisis? A. * Furosemide B. Mannitum C. Triamteren D. Dichlothiazide E. Spironolactonum 63. To indicate the drug – blocker of angiotensin converting enzyme. A. Anaprilinum B. * Lisinopril C. Methyldopa D. Reserpinum E. Dibazolum 64. To indicate– calcium channels blocker hypotensive drug A. * Nifedepine B. Captopril C. Reserpinum D. Anaprilinum E. Dibazolum 65. Mechanism of enalapril action A. Blocks alpha-adrenoreceptors B. * Blocks carboxypeptidase C. Blocks M-cholinoreceptors D. Has diuretic action E. Has sympatholytic action 66. Which one of the following drugs decreases de novo cholesterol synthesis by inhibiting the enzyme 3-hydroxy-3-methylglutaryl CoA reductase? A. Clofibrate B. Niacin C. Cholestyramine D. * Lovastatin E. Gemfibrozil 67. To indicate diuretic drug that is used for the removal of hypertensive crisis. A. Oxytocine B. Dichlothiazide C. Triamteren D. Spironolactonum E. * Furosemide 68. To indicate what diuretics is used in the complex therapy of hypertensive crisis. A. Spironolactonum B. * Furosemide C. Manit D. Dichlothiazide E. Triamterene 69. Which is a NOT a common side effect of nitroglycerin? A. * Blurred vision B. Flushing C. Headache D. Hypotension E. Hypertension 70. Calcium channel blockers reduce myocardial oxygen demand by reducing afterload, which is: A. Blood volume within the heart B. Pressure within the heart C. * Pressure against which the heart must pump D. Contractility of the heart muscle E. Oxygen demand of the heart 71. Which of the following nitrate preparations or dosage forms has the longest duration of action? A. Sublingual nitroglycerin B. Sublingual isosorbide dinitrate C. Oral isosorbide dinitrate D. * Transdermal nitroglycerin patch E. Validolum 72. In order to prevent the development of tolerance, the pharmacist instructs the patient to: A. Apply the nitroglycerin patch every other day B. Switch to sublingual nitroglycerin when the patient's systolic blood pressure elevates to >140 mm Hg> C. * Apply the nitroglycerin patch for 14 hours each and remove for 10 hours at night D. Use the nitroglycerin patch for acute episodes of angina only E. Apply the nitroglycerin patch 2 times per day 73. Binds bile acids in the intestine, thus preventing their return to the liver via the enterohepatic circulation: A. Niacin B. * Clofibrate C. Cholestyramine D. Probucol E. Lovastatin 74. Before administering isosorbide mononitrate, a priority assessment would include: A. Serum electrolytes B. Blood urea nitrogen (BUN) and creatinine C. * Blood pressure D. Level of consciousness E. Pressure within the heart 75. Cause a decrease in liver triacylglycerol synthesis by limiting available free fatty acids needed as building blocks for this pathway: A. Cholestyramine B. * Niacin C. Clofibrate D. Probucol E. Lovastatin 76. The patient asks how nitroglycerin should be stored while traveling. The pharmacist's best response would be: A. "You can protect it from heat by placing the bottle in an ice chest." B. * "It's best to keep it in its original container away from heat and light." C. "You can put a few tablets in a resealable bag and carry in your pant's pocket." D. "It's best to lock them in the glove compartment of your car to keep them away from heat and light." E. "Keep the tablets locked in a safe place until you need them." 77. Patient teaching regarding sublingual nitroglycerin should include which of the following statements: A. "You can take up to five doses every 3 minutes for chest pain." B. "Chew the tablet for the quickest effect." C. "Keep the tablets locked in a safe place until you need them." D. * "Sit or lie down after you take a nitroglycerin tablet to prevent dizziness." E. "You can protect it from heat by placing the bottle in an ice chest." 78. What is the best way to prevent tolerance to nitrates when using the transdermal patches? A. Leave the old patch on for 2 hours when applying a new patch B. Apply a new patch off for 24 hours once a week C. Leave the patch off for 24 hours once a week D. * Remove the patch at night for 8 hours, and then apply a new patch in the morning E. Leave the patch off for 12 hours once a week 79. An annoying side effect of ACE inhibitors that may be minimized by switching to an angiotensin receptor blocking agent includes: A. Orthostatic hypotension B. * A dry, nonproductive cough C. Fatigue D. Hypokalemia E. Hyperkalemia 80. Which of the following should not be taken concurrently with ACE inhibitors? A. Lasix B. Morphine C. * Potassium D. Natrium E. Vicasolum 81. Inhibits 3-hydroxy-3-methylglutaryl CoA reductase, the rate-limiting step in cholesterol synthesis: A. * Lovastatin B. Niacin C. Cholestyramine D. Clofibrate E. Probucol 82. The doctor would plan to administer which of the following calcium channel blocking agents to a patient with cerebral arterial spasms following a subarachnoid hemorrhage? A. amlodipine (Norvasc) B. diltiazem (Cardizem) C. * nimodipine (Nimotop) D. verapamil (Calan) E. furosemidum 83. When explaining different medication regimens to treat hypertension during a community education program, it would be accurate to state that African-Americans probably respond best to which combination of medications? A. ACE inhibitors and diuretics. B. * Diuretics and calcium antagonists C. Diuretics and beta-blockers D. ACE inhibitors and beta-blockers E. All of the above 84. Labetalol and carvedilol are classified as: A. Beta-blocking agents B. Alpha1-blocking agents C. * Combined alpha- and beta-blocking agents D. Calcium channel blockers E. Fibrinolytics 85. The pharmacist would monitor for reflex tachycardia in a patient receiving which classification of antihypertensive agents? A. Calcium channel blockers B. Cardioselective beta-blockers C. Nonselective beta-blockers D. * Direct-acting vasodilators E. Neuroleptics 86. ACE inhibitors and angiotensin receptor blockers both work to decrease blood pressure by: A. Preventing the formation of angiotensin II B. Enhancing sodium and water resorption C. Increasing the breakdown of bradykinin D. * Inhibiting aldosterone secretion E. All of the above 87. Which one of the following drugs is useful in treating tachycardia? A. Phenoxybenzamine B. Isoproterenol C. Phentolamine D. * Propranolol E. Prazosin 88. What diuretic has potassium-sparing action? A. Furosemide B. Mannitol C. Dihlothiazid D. * Triamterene E. Urea 89. Equilibrium between plasma and tissue levels for quinidine is reached: A. * in 1 or 2 days B. in approximately 1 wk C. in 1–3 wk D. in just a few minutes E. in 2 h 90. What diuretic is used for forced diuresis? A. Dihlothiazid B. Triamterene C. Spironolactone D. * Furosemide E. Diacarb 91. What diuretic is belonging to osmotic diuretics? A. Spironolactone B. * Mannitol C. Furosemide D. Dihlothiazid E. Triamterene 92. Equilibrium between plasma and tissue levels for amiodarone is reached: A. * in 1–3 wk B. in 1 or 2 d C. in approximately 1 wk D. in just a few minutes E. in 2 h 93. Equilibrium between plasma and tissue levels for IV lidocaine is reached: A. * in just a few minutes B. in 1 or 2 d C. in approximately 1 wk D. in 1–3 wk E. in 2 h 94. Drowsiness, paresthesias, muscle twitching, convulsions, changes in mental status (eg, confusion), hypersensitivity reactions (eg, urticaria, edema, anaphylaxis) – adverse effects of: A. * Lidocaine B. Phenytoin C. Propranolol D. Disopyramide E. Verapamil 95. Adverse effects of nitrates are: A. * hypotension, dizziness, tachycardia B. bradycardia, bronchospasm, heart failure C. peripheral edema, headache, heart failure D. nausea and constipation E. lightheadedness, weakness, peripheral edema 96. GI problems—nausea, vomiting, flatulence, constipation or diarrhea, abdominal discomfort are the most common adverse effects of: A. * dyslipidemic drugs B. calcium channel blockers C. beta-adrenergic blocking agents D. nitrates E. all of the above 97. Which of the following adverse effects is associated with nitroglycerin? A. Bronchospasm B. * Throbbing headache C. Bradycardia D. Sexual dysfunction. E. Anemia. 98. All of the following statements concerning nitroglycerin are correct EXCEPT: A. It causes an elevation of intracellular cGMP. B. It undergoes significant first-pass metabolism in the liver. C. It may cause significant reflex tachycardia. D. * It can not cause throbbing headache. E. It can cause postural hypotension. 99. Which of the following adverse effects is associated with nitroglycerin? A. Hypertension B. * Increasing of intracranial pressure C. Bradycardia D. Sexual dysfunction. E. Anemia. 100. Nitroderm is used: A. Antiarrhythmic action is via (-adrenergic blockade B. Ventricular premature depolarizations C. * Angina pectoris prophylaxis D. Conversion of atrial fibrillation to sinus rhythm E. Treatment of ventricular fibrillation 101. Which one of the following is a specific alpha-adrenergic antagonist: A. Atenolol B. Timolol C. Labetalol D. * Terazosin E. Sotalol 102. Agent, that inhibits 3-hydroxy-3-methylglutaryl CoA reductase, the rate-limiting step in cholesterol synthesis: A. * Pravastatin B. Niacin C. Cholestyramine D. Clofibrate E. Probucol 103. Adverse effects of organic nitrates are: A. nausea and constipation B. bradycardia, bronchospasm, heart failure C. peripheral edema, headache, heart failure D. * throbbing headache, dizziness, tachycardia E. lightheadedness, weakness, peripheral edema 104. What diuretic is used for the removal of hypertensive crisis? A. Dichlothiazide B. * Furosemide C. Spironolactonum D. Mannitum E. Triamteren 105. Indicate the antiarrytmic drug from of adrenoblockers group A. Nitroglycerin B. Amiodaron C. * Metoprolol D. Verapamil E. Asparcam 106. The drug related to the group of calcium antagonists A. Apressinum B. Prazosinum C. * Amlodipine D. Reserpine E. Papaverini hydrochloridum 107. Factors causing a susceptibility to urinary tract infect include: A. urinary tract obstruction B. diabetes mellitus C. pregnancy D. * All of the above E. None of the above 108. In the nephrotic syndrome: A. the prognosis is better in males than in female patients B. * a generalized edema is present, favourable treatment includes the management of any underlying disease C. an intermittent microscopic hematuria suggests advanced parenchymal damage D. the administration of steroids is always ineffective E. All of the above 109. Mechanism of action of cardiac glycosides A. Block the activity of COX2 B. Cause the dilatation of coronary vessels C. Block the beta-adrenoreceptors D. Block the calcium channels E. * Block the activity of adenosine-tryphosphatase (ATP-ase) 110. Dose of which of the following may not be altered with deranged value of GFR? A. * Cefipime B. Cefoperazone C. Cefuroxime D. Tetracycline E. All of the above 111. A drug that can selectively supress automaticity in Purkinje fibers compared to the sinus node: A. verapamil B. atenolol C. diltiazem D. propranolol E. * lidocaine 112. Carbonic anhydrase inhibitor A. furosemide (Lasix) B. bumetanide (Bumex) C. * acetazolamide (Diamox) D. chlorothiazide (Diuril) E. spironolactone (Aldactone) 113. About 35% of the filtered load of sodium chloride is reabsorbed here: A. thin limb -- --loop of Henle B. collecting duct C. distal convoluted tubule D. * thick ascending limb -- loop of Henle E. cortical collecting tubule 114. A drug, or class of drugs, that has been documented to reduce mortality following a myocardial infarction: A. Class Ia antiarrhythmics B. Class Ic antiarrhythmics C. * Class II antiarrhythmics D. Class III antiarrhythmics E. digoxin 115. Mechanism of action: spironolactone (Aldactone) A. through osmotic effects B. through enzyme inhibition C. * through interaction with hormonal receptors D. all of the above E. none of the above 116. GI upset, tinnitus and cinchonism are common side effects of: A. lidocaine B. digoxin C. propranolol D. * quinidine E. amiodarone 117. Diuretics acting on specific membrane transport proteins: A. loop diuretics B. thiazides C. amiloride (Midamor) D. triamterene (Dyrenium) E. * all of the above 118. An antiarrhythmic drug with the most "non-selective" mechanism of action: A. lidocaine B. Quinidine C. Propranolol D. Sotalol E. * amiodarone 119. Diuretic mechanism(s): A. through osmotic effects (preventing water reabsorption) B. enzyme inhibition C. interaction with hormonal receptors D. * all of the above E. none of the above 120. Loop diuretics -- effects on ionic excretion: A. * increased sodium excretion, increased calcium loss B. decreased magnesium loss C. decreased potassium loss D. all of the above E. none of the above 121. A primary mechanism by which Class I antiarrhythmic drugs produce their therapeutic effect in patients with ventricular arrhythmias: A. Block L-type Ca channels B. Block beta-adrenergic receptors C. * Increase the Effective Refractory Period D. Increase vagal tone to the AV node E. Increase the dispersion of refractoriness 122. Primary indications for treatment of cardiac arrhythmias include all of the following EXCEPT: A. * Arrhythmias that reduce cardiac output B. Arrhythmias that are prone to degenerate into more serious arrhythmias C. Arrhythmias that cause vascular stasis D. Arrhythmias that increase the risk of stroke E. Monomorphic premature ventricular beats 123. A side effect of furosemide that can increase the automaticity of ectopic cardiac pacemakers: A. hypercalcemia B. hyperkalemia C. * hypokalemia D. hyponatremia E. hypothyroidism 124. In the treatment of exertional angina: A. * nitroglycerin reduces O2 demand by decreasing preload B. nitroglycerin increases O2 supply by dilating atherosclerotic vessels C. attacks frequently occur during sleep D. nitroglycerin increases cardiac myocyte cAMP levels E. beta blocking agents have no beneficial action 125. Diltiazem: A. * decreases calcium entry through L type channels B. increases total peripheral resistance C. increases cardiac output D. increases heart rate E. increases gastrointestinal motility 126. A drug effect that is produced by therapeutic doses of both propranolol and amiodarone is blockade of: A. cardiac Na channels B. cardiac K channels C. * beta-adrenoceptors D. alpha-adrenoceptors E. L-type Ca channels 127. The most common cellular mechanism responsible for production of cardiac arrhythmias in patients with ischemic heart disease: A. * Hypokalemia B. depressed automaticity C. sick sinus syndrome D. reentrant excitation E. hormonal imbalance 128. Mechanism of action: acetazolamide (Diamox) A. through osmotic effects B. * through enzyme inhibition C. interacting with hormonal receptors D. all of the above E. none of the above 129. In a patient with a high risk for coronary artery disease (LDL cholesterol 200 mg/dL, normal tryglycerides), the best lipid lowering drug would be: A. nicotinic acid B. gemfibrozil C. atorvastatin D. colestipol E. * cholestyramine 130. Pharmacological blockade of sodium and chloride cotransport at the distal convoluted tubule: A. bumetanide (Bumex) B. furosemide (Lasix) C. * chlorothiazide (Diuril) D. triamterene (Dyrenium) E. none of the above 131. What diuretic has potassium-sparing action? A. Urea B. Furosemide C. Mannitol D. Dihlothiazid E. * Triamterene 132. Indicate the antiarrythmic drug which exerts membrane-stabilizing action. A. Atenolol B. * Quinidine sulfate C. Nitroglycerin D. Digoxin E. Isadrinum 133. What diuretic is used for forced diuresis? A. Dihlothiazid B. Triamterene C. Spironolactone D. * Furosemide E. Diacarb 134. Nitrates relieve angina pain by reducing preload, which is: A. * Oxygen demand of the heart B. Pressure within the heart C. Blood volume within the heart D. Pressure against which the heart must pump E. Contractility of the heart muscle 135. What diuretic is belonging to thiazide diuretics? A. Spironolactone B. Mannitol C. Furosemide D. E. 136. A. B. C. D. E. 137. A. B. C. D. E. 138. A. B. C. D. E. 139. A. B. C. D. 140. A. B. C. D. E. 141. A. B. C. D. E. 142. A. B. C. D. E. 143. A. B. C. D. E. 144. A. B. * Dihlothiazid Triamterene Acetazolamide (Diamox) inhibits carbonic anhydrase may produce metabolic acidosis increases potassium secretion * all of the above none of the above Indicate the Verapamil possible side effect, as antiarrhythmic drug Tachycardia Bronchospasm Stenocardia Mouth dryness * Decrease of artery pressure (hypotension) Osmotic diuretic is furosemide (Lasix) bumetanide (Bumex) * mannitol (Osmitrol) thiazides None of the above Nifedipine and verapamil both * cause coronary vasodilation depress atrioventricular nodal conduction cause reflex tachycardia stimulate calcium entry into cells Primary site of action of loop diuretics: distal tubule collecting duct thin descending limb of the loop of Henle * thick ascending limb of the loop of Henle at the site of glomerular filtration Loop diuretics are: * rapidly absorbed eliminated by renal secretion only eliminated by glomerular filtration only loop diuretics act on the interstitial side of the principal cell indomethacin (Indocin) increases loop diuretic clearance Which of the following agents is selective for beta1-adrenergic receptor? Metaproterenol Propranolol * Metoprolol Terbutalin Timolol Loop diuretics: Effects on magnesium and calcium excretion increase in magnesium secretion increase in calcium secretion hypomagnesemia in patients (prolonged loop diuretic use) No hypocalcemia in patients (prolonged loop diuretic use) * all of the above Selective blockade of beta1-adrenergic receptors: Labetalol Prazosin C. D. E. 145. A. B. C. D. E. 146. A. B. C. D. E. 147. A. B. C. D. E. 148. A. B. C. D. E. 149. A. B. C. D. E. 150. A. B. C. D. E. 151. A. B. C. D. E. 152. A. B. C. D. E. 153. Timolol * Atenolol Sotalol Furosemide (Lasix) toxicity: * ototoxicity hypouricemia hypermagnesemia severe fluid overload hypernatremia Agent is a specific alpha-adrenergic antagonist: * Prazosin Timolol Labetalol Atenolol Sotalol Indicate the peculiarility of Furosemide action Slow effect development * Fast effect development The duration of action (10-14 days) Low diuretic activity It doesn’t influence K concentration in the blood Indicate the diuretic of immediate diuretic action influencing the ascending part of Henle loop: Euphyllinum Spironolactonum * Furosemidum Triamterenum Diacarbum Labetalol is: * a selective alpha-adrenergic antagonist as well as a nonspecific beta-adrenergic antagonist is a specific alpha-adrenergic antagonist is a nonspecific beta-adrenergic antagonist is a selective beta1-adrenergic blocker Neither To indicate marching 8-oxychinoline for the medical treatment of urinary infections. Rifampine * Nitroxoline Biseptol Ampicilline Furosemide Which of the following agents is pure beta1-adrenergic agonists? Albuterol Propranolol * Bisoprolol Isoproterenol Timolol To indicate quinolone derivated , which is used mainly at infections of urinary tract. * Nalidixic Acid Biseptol Furosemide Aspirine All of the above Weakness or dizziness, especially with activity or exercise – adverse effects of: A. B. C. D. E. 154. A. B. C. D. E. 155. A. B. C. D. E. 156. A. B. C. D. E. 157. A. B. C. D. E. 158. A. B. C. D. E. 159. A. B. C. D. 160. A. B. C. D. E. 161. A. B. C. D. E. * Propranolol Phenytoin Lidocaine Disopyramide Verapamil Adverse effects of beta-adrenergic blocking agents are: * bradycardia, bronchospasm, heart failure hypotension, dizziness, lightheadedness headache, heart failure, pulmonary edema, nausea and constipation hypotension, dizziness, tachycardia Adverse effects of calcium channel blockers are: * dizziness, lightheadedness, peripheral edema, constipation bradycardia, bronchospasm, heart failure hypotension, tachycardia, headache palpitations and headache hypotension, dizziness Calcium channel blockers with prolong action: Nifedipine Verapamil Diltiazem * Amlodipine Nebivolol Which of the following agents is selective for beta1-adrenergic receptor? Metaproterenol Propranolol * Nebivolol Terbutalin Esmolol Call calcium channel blockers with prolong action: * Felodipine Verapamil Diltiazem Nifedipine Nebivolol Amlodipine and verapamil both * cause coronary vasodilation depress atrioventricular nodal conduction cause reflex tachycardia stimulate calcium entry into cells Which of the following agents is selective for beta1-adrenergic receptor? Salmeterol Propranolol * Bisoprolol Terbutalin Timolol Which one of the following drugs is useful in treating tachycardia? * Bisoprolol Isoproterenol Phentolamine Phenoxybenzamine Prazosin 162. Weight gain & edema occur in patients with congestive heart failure in response to: A. * increased aldosterone levels B. increased diuresis C. decreased renin levels decreased total peripheral resistance D. decreased venous capacitance 163. The mechanism by which digoxin causes a positive inotropic effect on heart tissue is by: A. increasing ATP hydrolysis B. stimulating the Na/K pump C. * increasing intracellular Na and Ca D. sensitizing the heart to catecholamines E. inhibiting the Na/H exchanger 164. A drug that is NOT known to increase the effect or toxicity of digoxin when given concominantly: A. furosemide B. verapamil C. amiodarone D. * propranolol E. quinidine 165. A drug used in the treatment of systolic congestive heart failure and produces its effects by inhibiting the cardiac Na/K pump: A. Furosemide B. Nifedipine C. captopril D. clonidine E. * digoxin 166. In the treatment of congestive heart failure, choose a drug that would reduce dyspnea and pulmonary edema by decreasing the left ventricular preload: A. Hydralazine B. propranolol C. * isosorbide dinitrate D. Dobutamine E. digoxin 167. Sodium nitroprusside: A. * is used to lower blood pressure in a hypertensive emergency B. increases smooth muscle cAMP levels C. has a slow onset and long duration of action D. is given orally E. inhibits nitric oxide formation 168. To indicate the antihypertensive drug used for the medical treatment of hypertensive disease with tachycardia and extrasystoles. A. Reserpinum B. Methyldopa C. * Bisoprolol D. Clophelinum E. Dibazolum 169. To indicate the possible side effect of propranolol? A. * Bronchial spasm B. Tachycardia C. Ortostatic collapse D. Rise of АP E. Development of tolerance 170. To indicate an antihypertensive drug from the calcium channels blockers. A. Anaprilinum B. Captopril C. Dibazolum D. * Nifedipine E. Reserpinum 171. Acebutolol is A. * Beta-adrenoreceptor antagonist B. Calcium channel blocker C. Beta-adrenoreceptor agonist D. Angiotensin II receptor antagonists E. ACE inhibitor 172. The patient suffer from hypertensive disease with bradiarrhythmia. What drug is necessary to prescribe? A. Papaverinum B. Platyphyllini hydrotartras C. Ceftriaxone D. * Methyldopa E. Paracetamol 173. Indicate the Verapamil possible side effect, as antiarrhythmic drug A. Tachycardia B. Bronchospasm C. Stenocardia D. Mouth dryness E. * Decrease of artery pressure (hypotension) 174. What diuretic has potassium-sparing action? A. Furosemide B. Mannitol C. Dihlothiazid D. * Triamterene E. Urea 175. What diuretic is used for forced diuresis? A. Dihlothiazid B. Triamterene C. Spironolactone D. * Torasemide E. Diacarb 176. Treatment of digoxin overdose may include all the following EXCEPT A. withdrawal of digoxin B. intravenous injection of Fab fragments of digitalis antibodies C. potassium supplements D. antiarrhythmic drugs E. * cholestyramine to break enterohepatic circulation 177. The administration of digoxin to a patient with congestive heart failure results eventually in a decrease in all of the following parameters EXCEPT A. heart rate B. end-diastolic pressure C. arteriolar resistance D. * AV node refractoriness E. renal sodium and water retention 178. Each of the following agents is useful to treat diastolic heart failure EXCEPT: A. lisinopril B. * digoxin C. verapamil D. furosemide E. carvedilol 179. Which of the following maneuvers is the most likely to improve renal perfusion in a patient treated for acute cardiac failure? A. administration of phenylephrine B. administration of propranolol C. injection of esmolol D. * administration of dopamine E. administration of epinephrine 180. The drugs whose international common name ends in - sentan such as bosentan, are: A. ACE (angiotensin converting enzyme) inhibitors B. progestogens C. * antagonists of endothelin receptors D. agonists of adenosine receptors E. directly acting cholinomimetic drugs 181. Clonidine lowers blood pressure: A. by inhibiting alpha-1 adrenergic receptors B. by inhibiting angiotensin converting enzyme C. * by stimulating central alpha-2 adrenergic receptors D. by inhibiting endothelin receptors E. by inhibiting beta-adrenergic receptors 182. Sartan: the drugs whose international common name ends by the suffix - sartan are: A. antineoplastic agents B. antiemetic agents C. antihypertensive drugs D. * angiotensin II receptor antagonists E. enkephalin receptor antagonists 183. Pril: the drugs whose international common name ends in the suffix – pril are: A. anorectics B. inhibitors of type V phosphodiesterases C. * ACE (angiotensin converting enzyme) inhibitors D. agonists of alpha- adrenergic receptors E. antidiarrheal drugs 184. During treatment, a patient develops a drug-induced dry cough. The drugs possibly responsible for this cough are: A. codeine B. diclofenac C. * perindopril D. Acetaminophen E. All of the above 185. A side effect of furosemide that can increase the automaticity of ectopic cardiac pacemakers: A. hypercalcemia B. hyperkalemia C. * hypokalemia D. hyponatremia E. hypothyroidism 186. Antihypertensive drug belonging to the same class: A. Doxazosin (Cardura), prazosin (Minipress), metoprolol (Lopressor) B. * nifedipine (Procardia, Adalat), verapamil (Isoptin, Calan), diltiazem (Cardiazem) C. Clonidine (Catapres), guanabenz (Wytensin),terazosin (Hytrin) D. Lisinopril (Prinvivil, Zestril), fosinopril (Monopril), guanadrel (Hylorel) E. None of the above 187. Mechanism of action: prasosin (Minipress) A. * alpha-1 receptor blocker B. beta receptor blocker C. phosphodiesterase inhibitor D. calcium channel blocker E. none of the above 188. Side effects of this antihypertensive agent includes tachycardia, angina, reversible lupus-like syndrome A. propranolol (Inderal) B. mecamylamine (Inversine) C. * hydralazine (Apresoline) D. Diazoxide (hyperstat) 189. Vasoconstriction, aldosterone secretion, and renin release suppression occur upon activation of the renin-angiotensin-aldosterone system. How would captopril (Capoten) affect these responses? A. * blocks all three B. blocks only vasoconstriction C. blocks all except vasoconstriction D. no effect E. Block renin release 190. Antihypertensive drug LEAST likely to elevate serum lipids: A. propranolol (Inderal) B. metoprolol (Lopressor) C. chlorothiazide (Diuril) D. * diltiazem (Cardiazem) E. Both chlorothiazide and propranolol 191. Mechanism of action: prazosin (Minipress) A. * alpha-1 receptor blocker B. beta receptor blocker C. phosphodiesterase inhibitor D. calcium channel blocker E. none of the above 192. Mechanism of action: diltiazem (Cardiazem) A. phosphodiesterase inhibitor B. * blockade of calcium channels C. alpha-1 receptor antagonists D. beta-1 receptor antagonist E. all of the above 193. I.v. route of administration; few side effects; effective in treating hypertensive crisis: A. nifedipine (Procardia, Adalat) B. * nitroprusside sodium (Nipride) C. nicardipine (Cardene) D. all of the above E. none of the above 194. Ganglionic blocker A. prazosin (Minipress) B. hydralazine (Apresoline) C. * mecamylamine (Inversine) D. nicardipine (Cardene) E. None of the above 195. Blocks both alpha and beta receptors: A. timolol (Blocadren) B. * labetalol (Trandate, Normodyne) C. propranolol (Inderal) D. diazoxide (Hyperstat) E. all of the above 196. Hypertensive emergencies: indicated using of A. diltiazem (Cardiazem) B. * nitroprusside sodium (Nipride) C. reserpine D. phenylephrine (Neo-Synephrine) E. all of the above 197. ACE inhibitor is A. nifedipine (Procardia, Adalat) B. * captopril (Capoten) C. timolol (Blocadren) D. methyldopa (Aldomet) E. None of the above 198. Antihypertensive: action based on inhibition of norepinephrine release from adrenergic nerve endings: A. propranolol (Inderal) B. * guanadrel (Hylorel) C. mecamylamine (Inversine) D. phentolamine (Regitine) E. None of the above 199. Causes of hypertension: A. Cushing's disease B. oral contraceptives C. acromegaly D. polycystic kidney disease E. * all of the above 200. The most specific agent for prevention of asthma is: A. * Salbutamolum B. Libexinum C. Adrenalini hydrochloridum D. Pertussinum E. Mucaltinum 201. Drugs that may decrease theophylline clearance include: A. * Cimetidine, ciprofloxacin B. ranitidine C. phenytoin D. None of the above E. All of the above 202. Theophylline clearance may be reduced by: A. phenobarbital B. warfarin C. tobacco smoking D. phenytoin E. * ciprofloxacin 203. Factors which are important to consider in selecting a maintenance dose of theophylline in a patient include all of the following EXCEPT: A. smoking history B. concomitant medication administration C. presence of congestive heart failure or cor pulmonale D. presence of hepatic failure E. * presence of renal insufficiency 204. Manifestations of theophylline toxicity may include all of the following EXCEPT: A. tremors B. seizures C. tachyarrhythmias D. vomiting E. * hyperkalemia 205. In the case of an oral overdose of theophylline, clearance may be enhanced by: induction of emesis A. * oral pulse dose charcoal B. administration of cimetidine C. lavage of nasogastric contents D. forced diuresis E. None of the above 206. Regarding its actions, cromolyn is best described as: A. bronchodilator B. anticholinergic C. beta agonist D. * inhibitor of mast cell degranulation E. glucocorticoid 207. Beta-2 selective adrenergic agonists include all EXCEPT: A. terbutaline B. albuterol C. metaproterenol D. * isoproterenol E. pirbuterol 208. Adverse effects of beta-2 adrenergic bronchodilators include all of the following EXCEPT: A. nervousness B. headache C. tachycardia D. tremulousness E. * lethargy 209. Which of the following work through cholinergic receptor antagonism? A. isoetharine B. cromolyn C. ephedrine D. * ipratropium E. salmeterol 210. Which of the following pharmacologic agents antagonize adenosine? A. * theophylline B. glucocorticoids C. cromolyn sodium D. propranolol E. terbutaline 211. Theophylline, ethacrynic acid, and furosemide: A. interfere with active renal tubular reabsorption of sodium B. * increase urine volume C. are not effective in the treatment of congestive heart failure D. decrease excretion of sodium in the urine E. may precipitate in renal tubules and cause acute angiospastic necrosis 212. The agent with immune boosting activity yet recently implicated with causing severe depression and suicidal ideation is A. echinacea B. * interferon C. dronabinol (Marinol) D. megestrol (Megace) E. all of the above 213. Examples of autoimmune diseases A. rheumatoid arthritis B. insulin-dependent diabetes mellitus C. systemic lupus erythematosis D. rheumatoid arthritis & systemic lupus erythematosis E. * all of the above 214. Which of the following asthma severity categories has a treatment including inhaled low-dose steroid, cromolyn, nedocromil, zafirlukast or zileuton? A. Mild intermittent asthma B. * Mild persistent asthma C. Moderated persistent asthma D. Severe persistent asthma E. Exercise-induced asthma 215. Which of the following drugs acts through a cytosolic receptor? A. Cromolyn sodium B. * Beclomethasone C. Zafirlukast D. Omalizumab E. None of the above 216. Which of the following corticosteroids is used for quick relief from asthma? A. Triamcinolone B. * Dexamethasone C. Budesonide D. Beclomethasone E. Fluticasone 217. Which of the following is not true about Salmeterol? A. administered by inhalation B. long acting anti-asthmatic with a duration of 12 hour C. * can lead to transient increase in PaO2, especially in poorly ventilated lung tissue D. associated with improvement in patients homozygous for glycine at the B-16 locus of the betareceptor E. none of the above 218. Which of the following is not true about Ipratropium bromide: A. Anticholinergic agent administered by inhalation B. better bronchodilator than Atropine C. * better anti-asthmatic than Epinephrine D. has no effect on mucocilliary clearance E. none of the above 219. Which of the following is not a quick relief medication for asthma? A. Epinephrine B. Ipratropium bromide C. Prednisolone D. * Flunisolide E. All of the above 220. The following is not true of beta-2 adrenergic agonists: A. cause bronchodilation by decreasing cytosolic Ca2+ B. cause hypotension C. * decrease mucocilliary activity D. decrease bronchial vascular permeability E. increase heart rate 221. Which of the following can be administered orally and by inhalation? A. Epinephrine B. Albuterol C. Pirbuterol D. * Terbutaline E. Isoproterenol 222. Which of the following drug combinations would produce a synergistic effect A. Amoxicillin+ ampicillin B. Cephalexin+ penicillin V C. Sulfamethoxazole+ trimethoprim D. Vancomycin+ gentamicin E. * Sulfamethoxazole+ trimethoprim and Vancomycin+ gentamicin 223. The drug of choice for methicillin-resistant Staphylococcus aureus is: A. oxacillin B. gentamicin C. * vancomycin D. piperacillin E. None of the above 224. Tetracyclines: A. are bacteriostatic in vitro B. are bactericidal in vitro C. are effective against rickettsiae D. * are bacteriostatic in vitro, are effective against rickettsiae E. interfere primarily with cell wall synthesis 225. The drug of choice for Streptococcus pneumonia (pneumococcus) in a patient with no drug allergies is: A. erythromycin B. * penicillin C. vancomycin D. ceftriaxone E. gentamicin 226. Aminoglycosides are: A. excreted renally B. bactericidal C. potentially toxic to the auditory and vestibular portions of the eighth cranial nerve D. potentially nephrotoxic E. * All of the above 227. The route by which isoniazid is usually administered is: A. * oral B. intramuscular injection of solution C. intramuscular injection of suspension D. subcutaneous injection of solution E. intravenous 228. Rifampin is used mainly in the treatment of: A. cholera B. typhoid fever C. * tuberculosis D. rickettsial diseases E. pseudomonas infections 229. Impaired vision is an adverse effect of: A. carbenicillin B. * ethambutol C. rifampin D. colistin E. cycloserine 230. Various drugs may induce vitamin deficient states as an undesirable side effect. Vitam B6 (pyridoxine) deficiency may be related to taking: A. estrogen-containing oral contraceptives B. colchicine C. * isoniazid D. All of the above E. None of the above 231. Most adults who are at high risk of developing pulmonary tuberculosis should be treated with: A. isoniazid 100 mg/day for 6 months B. * isoniazid 300 mg/day for 12 months C. ethambutol 400 mg/day for 12 months D. rifampin 600 mg/day for 24 months E. No treatment is necessary 232. An antitubercular agent which is associated with the development of ocular toxicity is: A. rifampin B. * ethambutol C. isoniazid D. streptomycin E. para-aminosalicylic acid 233. Which of the following antitubercular agents is associated with the development of ototoxicity? A. rifampin B. ethambutol C. isoniazid D. * streptomycin E. para-aminosalicylic acid 234. Which of the following antibiotics is most closely associated with the development of ocular toxicity? A. kanamycin B. penicillin G C. tetracycline D. isoniazid E. * ethambutol 235. Which of the following antibiotics is most closely associated with the development of hepatitis? A. kanamycin B. penicillin G C. tetracycline D. * isoniazid E. ethambutol 236. Which of the following antibiotics is most closely associated with the development of renal and ototoxicity? A. * kanamycin B. penicillin G C. tetracycline D. isoniazid E. ethambutol 237. A. B. C. D. E. 238. A. B. C. D. E. 239. A. B. C. D. E. 240. A. B. C. D. E. 241. A. B. C. D. E. 242. A. B. C. D. E. 243. A. B. C. D. E. 244. A. B. C. D. E. 245. A. B. Patients having a history of a severe, immediate reaction to penicillin: may be given a cephalosporin without concern have a definite risk of reaction to any cephalosporin have a low risk of having a reaction to a broad spectrum antipseudomonal penicillin have a high risk of hypersensitivity to a broad spectrum antipseudomonal penicillin * have a definite risk of reaction to any cephalosporin & have a high risk of hypersensitivity to a broad spectrum antipseudomonal penicillin What agents are antiviral: Interferonum Biochinolum Oxolinum Remantadinum * Interferonum, Oxolinum & Remantadinum Choose the necessary component of therapy of pneumonia complicated by pleurisy with effusion: Inhibitors of proteinases; Diuretic; * Antibiotics; Antiviral therapy; Cardiac glycosides. Most common fungal infection in HIV patients Cryptococcosis * candidiasis histoplasmosis Neither All of the above Agents useful in treating mycobacterial infections in HIV patients: clarithromycin (Biaxin) ethambutol (Myambutol) amikacin (Amikin) * all of the above may be useful None of the above Suitable for treatment of bacterial meningitis caused by H. Influenzae: * cefotaxime (Claforan) cephalexin (Keflex) cephalothin (Keflin) cefadroxil (Duricef, Ultracef) None of the above Antibiotic's clearance from the body most likely influenced by severe hepatic disease: Penicillins clindamycin (Cleocin) rifampin (Rimactane) * clindamycin & rifampin None of the above Associated with "gray baby syndrome" which is characterized by pallor, cyanosis, and even death. Tetracyclines * chloramphenicol (Chloromycetin) third-generation cephalosporins Tetracyclines & chloramphenicol None of the above Special concerns in using antimicrobials in newborns and young children: Sulfonamides can be safely given to newborns Tetracyclines should not be administered to children betlow the age of eight C. Newborns should not be given chloramphenical because they are unable to metabolize the drug adequately. D. * Tetracyclines should not be administered to children betlow the age of eight & Newborns should not be given chloramphenical because they are unable to metabolize the drug adequately E. None of the above 246. Antibacterials regarded as generally safe to prescribe in pregnancy. A. Erythromycins B. Cephalosporins C. Tetracyclines D. * Erythromycins & Cephalosporins E. All of the above 247. Ototoxicity and nephrotoxicity associated with this antibiotic: A. cefotaxime (Claforan) B. * amikacin (Amikin) C. aztreonam (Azactan) D. ceftriaxone (Rocephin) E. cefotaxime & amikacin 248. Aminoglycosides antibacterial is A. Hetacillin B. Aztreonam C. * gentamicin (Garamycin) D. vancomycin (Vancocin) E. gentamicin & aztreonam 249. FALSE statement about penicillin G A. treatment of choice for viridans group streptococcal endocarditis. B. Pen G and Pen V are the two natural penicillins. C. Pen G can be combined with procaine, extending drug half-life D. * Pen G most effective when given orally E. All of the above 250. Inhibits bacterial cell wall synthesis: A. Streptomycin B. * vancomycin (Vancocin) C. doxycycline (Vibramycin, Doryx) D. gentamicin (Garamycin) E. None of the above 251. Mechanism of action: amoxicillin (Amoxil) A. inhibits bacterial cell wal biosynthesis B. interferes with transpeptidation preventing peptidoglycan chain crosslinking. C. Inhibits protein synthesis D. * inhibits bacterial cell wal biosynthesis & interferes with transpeptidation preventing peptidoglycan chain crosslinking E. interferes with transpeptidation preventing peptidoglycan chain crosslinking & Inhibits protein synthesis 252. Combination of metronidazole (Flagyl) and penicillin in treating an abscess caused by betalactamase producing Bacteriodes and anaerobic streptococci is an example of: A. synergistic drug treatment B. antagonistic drug effects C. * additive drug effects D. none of the above E. synergistic drug treatment & additive drug effects 253. Beta-lactamase inhibitor: A. vancomycin (Vancocin) B. sulbactam C. clavulanate D. * sulbactam & clavulanate E. None of the above 254. Antifungal polyene macrolide that preferentially binds to fungal ergosterol which alters cellular permeability. A. Ketoconazole B. * amphotericin B C. Flucytosine D. Grisefulvin E. Clotrimazole 255. An azole most commonly used for topical treatment of candidiasis: A. amphotericin B B. * clotrimazole C. Griseofulvin D. Flucytosine E. none of the above 256. Polyene macrolide only used topically, due to systemic toxicity; active against most Candida species--most commonly used for suppression of local candidal infection. A. Miconazole B. Terbinafine C. * Nystatin D. Fluconazole E. Flucytosine 257. Inhibition of fungal squalene epoxidase is this antifungal drug's mechanism of action: A. Ketoconazole B. Fluconazole C. * Terbinafine D. Nystatin E. Ketoconazole & Fluconazole 258. Most potent of the presently available anti-fungal azoles: A. Fluconazole B. * Itraconazole C. Ketoconazole D. Both Fluconazole & Ketoconazole E. None of the above 259. Azole most likely to get into the cerebral spinal fluid: A. Ketoconazole B. Itraconazole C. * Fluconazole D. Both Ketoconazole & Itraconazole E. None of the above 260. Given by i.v. administration, the drug of choice for nearly all life-threatening mycotic infections-usually used as the initial induction regimen A. Ketoconazole B. Itraconazole C. Flucytosine D. * amphotericin B E. nystatin 261. Properties of tetracycline: A. inhibitor of bacterial cell wall synthesis B. * dug of choice in treating typhus C. cleared primarily by the liver D. All of the above E. none of the above 262. Females often complaine: odorless, white or yellow cheesy discharge with itching A. Chalymida B. Syphilis C. Chalmdyia D. * Candidias E. none of the above 263. A bacteriostatic antimicrobial that inhibits protein synthesis by blocking attachment of aminoacyi t-RNA to the A site on the 30S bacterial ribosome A. Aminoglycosides B. Fluoroquinolones C. Metronidazole D. Sulfonamide E. * Tetracycline 264. Bactericidal drugs that act by inhibiting DNA gyrase A. Aminoglycoside B. * Fluoroquinolones C. Macrolides D. Rifamycins E. Sulfonamides 265. Binds to the 50 s bacterial ribosome and prevents the translocation step in protein synthesis A. Aminoglycosides B. Daptomycin C. Linezolid D. * Macrolides E. Metronidazole 266. Binds to the 30s bacterial ribosome and blocks the initiation step in protein synthesis. May cause miscoding A. * Aminoglycosides B. Daptomysin C. Linezolid D. Metronidazole E. Rifampin 267. Inhibits the formation of folic acid by competing with PABA for dihydropteroate synthase A. Metronidazole B. Rifampin C. * Sulfamethoxazole D. Trimethoprin E. Linezolid 268. Binds to specific receptors located in the bacterial cytoplasmic cell membrane and inhibits transpeptidase enzymes, preventing cross linking of peptidoglycan chains in the cell wall A. * Cephalosporins B. Daptomycin C. Linezolid D. Metronidazole E. Rifampin 269. Binds to the D-Ala-D-Ala terminal end of peptidoglycan side chains, resulting in inhibition of transglycosylation and disruption of cross-linking in the cell wall A. Chloramphenicol B. Clavulanic C. Imipenem D. * Vancomycin E. Metronidazole 270. Combination of these two drugs would produce an antagonistic (undesirable) antimicrobial effect when treating an infection A. Amoxicillin+ gentamicin B. Cephalexin+ gentamicin C. Sulfamethoxazole+ trimethoprim D. * Tetracycline+ amoxicillin E. Vancomycin+ gentamicin 271. Which form of resistance to the effect of antimicrobial drugs is specific to beta-lactam type antibiotics A. Decreased drug uptake B. Methylation of the antibiotic’s receptor C. Decreased metabolic activation D. Altered amount of drug receptor E. * Increased enzymatic destruction of the antibiotic 272. The combination of sulfamethoxazole and trimethoprim is a useful drug for treating urinary tract infections. Bacterial resistance to trimethoprim occurs primarily by A. Acetylation of trimethoprim B. Acetylation of the drug receptor C. Decreased bacterial uptake D. * Upregulation of dihydrofolate reductase E. Upregulation of beta-lactamase 273. Bacterial resistance to this drug results from a plasmid mediated mechanism that results in an altered ribosomal binding site within the bacteria A. Ampicillin B. * Azithromycin C. Penicillin D. Piperacillin E. Vancomycin 274. Which of the following antimicrobial drugs is bactericidal A. Azithromycin B. Doxycycline C. Erythromycin D. * Gentamicin E. Tetracycyline 275. Which of the following antimicrobials is taken up into bacteria by an oxygen-dependent mechanim and is therefore ineffective against anaerobic organisms A. Cefoxitin B. Clindamycin C. * Gentamicin D. Metronidazole E. Ticarcillin 276. The drug of choice for methicillin-resistant Staphylococcus aureus is: A. oxacillin B. gentamicin C. * vancomycin D. piperacillin E. None of the above 277. The drug of choice for Streptococcus pneumonia (pneumococcus) in a patient with no drug allergies is A. erythromycin B. * penicillin C. vancomycin D. ceftriaxone E. gentamicin 278. Which of the following is the general mechanism of action for erythromycin? A. Inhibition of a metabolic enzyme B. Inhibition of cell wall synthesis C. * Disruption of protein synthesis D. Inhibition of nucleic acid transcription and replication E. None of the above 279. Which of the following is the general mechanism of action for fluoroquinolones? A. Inhibition of a metabolic enzyme B. Inhibition of cell wall synthesis C. Disruption of protein synthesis D. * Inhibition of nucleic acid transcription and replication E. None of the above 280. Trimethoprim is often administered alongside a sulfonamide as a preparation known as cotrimoxazole. Which of the following sulfonamides is used? A. * Sulfamethoxazole B. Sulfathiazole C. Sulfadoxine D. Sulfadiazine E. None of the above 281. Which of the following statements is true regarding the properties of benzylpenicillin? A. It is a bacteriostatic agent. B. It is active over a wide range of bacterial species. C. It is resistant to beta-lactamases. D. * Certain individuals may have an allergic response to it. E. All of the above 282. What crucial feature of a penicillin is involved in its mechanism of action? A. Carboxylic acid B. * beta-lactam ring C. Acyl side chain D. Thiazolidine ring E. All of the above 283. The following structure is a first generation cephalosporin. What is the name of the structure? A. Cefazolin B. Cefoxitin C. Cefuroxime D. * Cefalexin E. All of the above 284. What drugs are present in the preparation Augmentin? A. Ticarcillin and clavulanic acid B. Ampicillin and sulbactam C. Ampicillin and clavulanic acid D. * Amoxicillin and clavulanic acid E. None of the above 285. Which of the following antibiotics is a macrolide? A. Chloramphenicol B. Doxycycline C. * Erythromycin D. Streptomycin E. None of the above 286. Which of the following antibiotics is a tetracycline? A. Chloramphenicol B. * Doxycycline C. Streptomycin D. Erythromycin E. None of the above 287. Which of the following drugs is associated with the reaction of hepatitis? A. Valproic acid B. Quinidine C. * Isoniazid D. Ethosuximide E. All of the above 288. Which of the following drugs (including metabolites) would achieve steady state blood level concentrations earliest assuming a loading dose is not given? A. phenytoin B. primidone C. * valproate D. phenobarbital E. ethosuximide 289. Which one of following is an appropriate therapeutic use for imipramine? A. Insomnia. B. Epilepsy C. * Bed—wetting in children D. Glaucoma. E. Mania 290. MAO inhibitors are contraindicated with all of the following EXCEPT: A. Indirect adrenergic agents, such as ephedrine. B. Tricyclic antidepressants. C. Beer and cheese. D. * Aspirin. E. Dopamine. 291. All of the following are observed in patients taking neuroleptic agents EXCEPT: A. Sexual dysfunction. B. * Increased blood pressure. C. Altered endocrine function. D. Constipation. E. Orthostatic hypotension. 292. In the treatment of acute diarrhea A. antibiotics are worst avoided in non-pathogenic diarrhea B. antibiotics are worst avoided in viral gastroenteritis C. oral rehydration should not be used for initial therapy D. electrolytes and glucose should not be supplemented for initial therapy E. * oral rehydration and electrolytes supplementation are required particularly in children and in the elderly 293. Neostigmine will effectively antagonize skeletal muscle relaxation produced by: A. * Tubocurarine B. Succinylcholine C. Diazepam D. Baclofen E. Nicotine 294. The reversible cholinesterase inhibitor indicated in the treatment of Alzheimer disease is: A. * Rivastigmine B. Levodopa C. Neostigmine D. Pyridostigmine E. Acetylcholine 295. Direct-acting cholinomimetic drug that is lipid-soluble and often used in the treatment of glaucoma is: A. Acetylcholine B. Timolol C. Betaxolol D. * Pilocarpine E. Physostigmine 296. Atropine and scopolamine will block all the effects of acetylcholine listed below EXCEPT: A. bradycardia B. salivary secretion C. bronchoconstriction D. * skeletal muscle relaxation E. miosis 297. Of the many types of adrenergic receptors found throughout the body, which is most likely responsible for the cardiac stimulation observed following an intravenous injection (IV) of epinephrine? A. beta1-adrenergic receptors B. * alpha1-adrenergic receptors C. alpha2-adrenergic receptors D. alpha3-adrenergic receptors E. None of the above 298. Which of the following drugs is a selective inhibitor of MAO type B? A. Neostigmine B. Selegiline C. * Bromocriptine D. Carbidopa E. Entacapone 299. The drug of choice for the treatment of anaphylactic shock is: A. * Epinephrine B. Norepinephrine C. Isoproterenol D. Orciprenaline E. Atropine 300. All the following statements are true concerning dobutamine EXCEPT that it: A. is a selective agonist at alpha1-adrenergic receptors B. * activates dopaminergic receptors in renal and mesenteric vascular beds C. is used to increase cardiac output in patients with severe cardiac failure D. must be given by IV administration E. may cause tachycardia and anginal pain 301. Which one of the following drugs is a selective beta2-agonist? A. Epinephrine B. Norepinephrine C. * Salbutamol D. Isoproterenol E. Dobutamine 302. The nonselective beta-adrenergic blocking agent that is also a competitive antagonist at alpha1- adrenoreceptors is: A. Timolol B. Atenolol C. Propranolol D. Pindolol E. * Carvedilol 303. Propranolol is indicated for use in patients with all the following conditions EXCEPT: A. hypertension B. angina pectoris C. * bronchial asthma D. migraine headache E. supraventricular and ventricular arrhythmias 304. Which one of the following statements best describes the mechanism of action of benzodiazepines? A. Benzodiazepines block GABA uptake B. Their inhibition of GABA transaminase leads to increase of GABA C. Benzodiazepines block glutamate receptors in the brain D. * They increase frequency of opening of chloride ion channels that are coupled to GABAA receptors E. They are direct-acting GABA receptor agonists in the CNS 305. The hypnotic drug facilitates the inhibitory action of GABA, but it lacks of anticonvulsant or muscle relaxing properties, is: A. Buspirone B. Diazepam C. Flurazepam D. Phenobarbital E. * Zolpidem 306. All the following benzodiazepines are biotransformed to active metabolites EXCEPT: A. Alprazolam B. Diazepam C. * Oxazepam D. Clorazepate E. Chlordiazepoxide 307. Which one of the following is described as a competitive benzodiazepine receptor antagonist? A. Pralidoxime B. Bromazepam C. Midazolam D. Triazolam E. * Flumazenil 308. All the following compounds are indicated for the treatment of psychoses EXCEPT: A. Chlorpromazine B. Risperidone C. * Fluoxetine D. Haloperidol E. Clozapine 309. The preferred treatment of status epilepticus is IV administration of: A. Chlorpromazine B. * Diazepam C. Succinylcholine D. Ethosuximide E. Selegiline 310. Carbidopa is useful in the treatment of Parkinson’s disease because it: A. is a precursor of levodopa B. is a dopaminergic receptor agonist C. * prevents peripheral decarboxylation of levodopa D. prevents breakdown of dopamine E. promotes a decreased concentration of levodopa in the nigrostriatum 311. Which one of the following is an antidepressant agent that selectively inhibits serotonin (5HT) uptake? A. Selegiline B. * Fluoxetine C. Maprotiline D. Desipramine E. Amitriptyline 312. Aspirin may be fatal in taken in sufficient quantity. The syndrome of fatal salicyate overdose in children is characterized by A. marked hypotermia secondary to an antipyretic effect B. * fever, tinnitus C. peripheral oedema D. None of the above E. All of the above 313. Common adverse reactions of corticosteroidal therapy are: A. bradycardia, mental dullness B. anorexia, polyuria C. tachycardia, insomnia D. * “moon face”, obese trunk E. All of the above 314. The chemotherapeutic agent also used orally for severe forms of arthritis is A. 5-fluorouracil (5-FU) B. * methotrexate (Mexate) C. cyclophosphamide (Cytoxan) D. cisplatin (Platinol) E. All of the above 315. What adverse effects are associated with chronic use of systemic corticosteroids? A. Candidosis B. * Gastrointestinal complications C. Hypotension D. Hypoglycemia E. All of the above 316. For a 6-year-old child with fever, what NSAIDs would be preferred? A. aspirin B. * acetaminophen C. indomethacin D. ibuprofen E. All of the above 317. Symptoms of salicylism: A. Tinnitus B. decreased hearing C. vertigo D. None of the above E. * All of the above 318. Released at sites of tissue injury: A. Kinins B. complement components C. cytokines D. neuropeptides E. * all of the above 319. Mediator in acute inflammation, pain A. Histamine B. Serotonin C. Leukotrienes D. * bradykinin E. none of the above 320. Mediator of chronic inflammation (for example rheumatoid arthritis) A. Histamine B. * interleukin-1 C. Bradykinin D. Neuropeptides E. Serotonin 321. Most nonsteroidal antiinflammatory drugs: A. * inhibit prostaglandin biosynthesis B. weak organic bases C. probably increase production of free radicals D. mainly associated with guanylyl cyclase interactions E. all the above 322. Initial drug of choice for treating most articular and musculoskeletal disorders (because of lowcost, safety, and efficacy) A. * Aspirin B. Diclofenac C. Indomethacin D. Phenylbutazone E. Glucocorticoids 323. Concerning salicylates: A. sodium salicylate an aspirin: equally effective as anti-inflammatory agents B. aspirin: maybe more effective for analgesia C. aspirin: hydrolyzed to acetic acid plus salicylate by tissue and blood esterases D. urine alkalinization: increases free salicylate excretion E. * all of the above 324. Acute attacks of gouty arthritis may occur early in treatment with allopurinol because: A. allopurinol increases urate synthesis B. * urate crystals move from tissue to plasma C. allopurinol increases release of chemotactic factors D. None of the above E. All of the above 325. Rational indication(s) for allopurinol (Zyloprim, Purinol) administration: A. chronic tophaceous gout; when tophi reabsorption more rapid with uricosuric agents B. when probenecid or sulfinpyrazone cannot be used C. presence of renal functional impairment D. in a patient with recurrent renal stones E. * all of the above 326. Effective in management of mild to moderate pain, when anti-inflammatory action is not necessary A. penicillamine (Cuprimine) B. sulfasalazine (Azulfidine) C. * acetaminophen (Tylenol, Panadol) D. etodolac (Lodine) E. 327. A. B. C. D. E. 328. A. B. C. D. E. 329. A. B. C. D. E. 330. A. B. C. D. E. 331. A. B. C. D. E. 332. A. B. C. D. E. 333. A. B. C. D. E. 334. A. B. C. D. E. 335. A. piroxicam (Feldene) Probably the initial step in acute gouty arthritis attack: polymorphonuclear leukocytes migration into the joint increased numbers of mononuclear phagocytes (macrophages) * urate crystals phagocytosis by synoviocytes prostaglandin, lysosomal &, interleukin 1 release None of the above Probable direct effect of colchicine (mechanism of action): direct membrane stabilization * binds to intracellular tubulin -- preventing/reducing microtubule formation decreases purine synthesis directly prevents IL-1 release directly none of the above Reduces uric acid synthesis: for management of gout colchicine probenecid sulfinpyrazone (Anturane) * allopurinol oxaprozin Aspirin mechanism of action: anti-platelet effects: promotes platelet aggregation activates thromboxane synthesis * snhibits thromboxane synthesis all of the above none of the above Factors accounting for rheumatoid arthritis incidence: Genetics Climate Urbanization * All of the above None of the above At low doses required to inhibition of thymidylate synthase, an enhanced adenosine release Chloroquine Gold * methotrexate cyclophosphamide ketorolac Aspirin and antipyresis: aspirin -- best available drug for reducing fever (in the absence of contraindications to its use recurrent aspirin -- more effective in lowering elevated temperature than normal body temperature aspirin-induced temperature reduction is caused by vasodilation * All of the above None of the above Phases of inflammation: acute inflammation the immune response chronic inflammation * All of the above None of the above Advantages of other NSAIDs compared with aspirin: generally less expensive B. less gastric irritation C. potentially better compliance (e.g. naproxen, sulindac) D. generally less expensive & less gastric irritation E. * less gastric irritation & potentially better compliance (e.g. naproxen, sulindac) 336. Aspirin: A. inhibits prostaglandin synthase B. inhibits cyclooxygenase C. decreases prostaglandin formation D. decreases thromboxane A2 formation E. * All of the above 337. Mediators of chronic inflammation in rheumatoid arthritis: A. IL-1 B. IL-2 C. IL-3 D. TNF alpha E. * All of the above 338. Effective in managing acute gouty arthritis and ankylosing spondylitis; also accelerates closure of patent ductus arteriosus in premature infants: A. Gold B. Ketorolac C. Phenylbutazone D. Methotrexate E. * Indomethacin 339. Approximate prevalence of rheumatoid arthritis: A. * 1 % B. 5 % C. 7 % D. 10 % E. 15 % 340. Analgesic effects of aspirin: A. peripheral action (inflammation) B. subcortical site of action C. activates thromboxane synthesis D. * peripheral action (inflammation) & subcortical site of action E. subcortical site of action & activates thromboxane synthesis 341. NSAID primarily promoted as an analgesic, not as an anti-inflammatory agent: A. Piroxicam B. Ibuprofen C. Naproxen D. * Ketorolac E. Sulindac 342. Drug associated with the hepatic/renal toxic metabolite: N-acetyl-p-benzoquinone A. Diclofenac B. Meclofenamate C. Indomethacin D. * Acetaminophen E. Aspirin 343. Typically associated with B cell proliferation and differentiation into antibody-secreting plasma cells A. tumor necrosis factor beta B. interferon-gamma C. * IL-4 (interleukin 4) D. IL-2 (interleukin 2) E. all of the above 344. Which of the following describes an agonist? A. substance that brings about a change in biologic function through its chemical action B. * A drug that binds to a receptor and stimulates cellular activity C. A drug that binds to a receptor and inhibits or opposes cellular activity D. A drug directed at parasites infecting the patient E. None of the above 345. What determines the degree of movement of a drug between body compartments? A. Partition constant B. Degree of ionization C. pH D. Size E. * All of the above 346. Which of the following is NOT a protein target for drug binding? A. * Side of action (transport) B. Enzymes C. Carrier molecules D. Receptors E. Ion channels 347. Which of the following is an example of a drug acting directly through receptors? A. Protamine binds stoichiometrically to heparin anticoagulants B. Adrenergic beta blockers for thyroid hormone-induced tachycardia C. * Epinephrine for increasing heart rate and blood pressure D. Cancer chemotherapeutic agents E. Mannitol for subarachnoid hemorrhage 348. What type of drug is propranolol (Inderal)? A. Anticonvulsive B. * Antihypertensive C. Antinauseant D. Antihistamine E. Antipyretic 349. What type of drug is amlodipine? A. * Ca++channel blocker B. Adrenergic beta-blocker C. ACE inhibitor D. Blocks beta-receptors in heart myocardium E. Diuretic 350. Which of the following is considered the class? A. Propranolol B. Inderal C. * Adrenergic beta-blocker D. “off label” use E. Blocks beta-receptors in heart myocardium 351. Which of the following cases would be contraindicated for propranolol (Inderal)? A. Hypertension B. Essential tremor C. Angina D. Tachycardia E. * Asthma 352. Which of the following adverse effects (side-effects) is NOT commonly seen with cholinergic antagonists? A. Blurred vision B. Confusion C. * Miosis D. Constipation E. Urinary retention 353. The drug chloramphenicol (Chloromycetin) is risky for which of the following? A. * Neonates B. Geriatric patients C. Adult males D. Obese patients E. Congestive heart failure patients 354. Which of the following are the two modifying factors that contribute to why women have higher blood peak concentrations of alcohol than men when consuming equivalent amounts? A. Lower blood volume & increased hormones B. Lower fat content & more gastric alcohol dehydrogenase (ADH) C. Higher fat content & more gastric alcohol dehydrogenase (ADH) D. Lower fat content & less gastric alcohol dehydrogenase (ADH) E. * Higher fat content & less gastric alcohol dehydrogenase (ADH) 355. Pharmacokinetics is the effect of the ____ and pharmacodynamics is the effect of the ____. A. Drug on a drug; Body on the drug B. Body on the drug; Drug on a drug C. Drug on the body; Body on the drug D. * Body on the drug; Drug on the body E. Drug on a drug; Drug on a drug 356. Which of the following is NOT an action of the body on a drug? A. Absorption B. Distribution C. Metabolism D. Excretion E. * Side effects 357. If a drug is 80% bound to blood elements or plasma proteins, what part is considered the free form? A. * 20% B. 40% C. 50% D. 80% E. 100% 358. If a patient misses three doses of their daily drug, which of the following (in general) is the best solution? A. Take a 4x dose at the next dose time B. Wait 3 more days (week total) then return to normal regimen C. * Do nothing and continue normal regimen D. Setup an appointment to have the patient evaluated E. Prescribe a higher dosage pill so missed doses will have less effect 359. Which of the following is NOT needed for drug bioequivalence? A. Same active ingredients B. Same strength or concentration C. Same dosage form D. Same route of administration E. * Same side effects 360. For intravenous (IV) dosages, what is the bioavailability assumed to be? A. 0% B. 25% C. 50% D. 75% E. * 100% 361. Although morphine is well-absorbed when administered orally, how much of the drug is metabolized on its first pass through the liver? A. * 90% B. 70% C. 50% D. 30% E. 10% 362. Which of the following is NOT a pharmacokinetic process? A. Alteration of the drug by liver enzymes B. Drug metabolites are removed in the urine C. Movement of drug from the gut into general circulation D. * The drug causes dilation of coronary vessels E. The drug is readily deposited in fat tissue 363. Which of the following can produce a therapeutic response? A drug that is: A. Bound to plasma albumin B. Concentrated in the bile C. Concentrated in the urine D. Not absorbed from the GI tract E. * Unbound to plasma proteins 364. A patient presents with an overdose of acidic Aspirin. The drug ____ can be given to ____ the pH of the urine and trap the Aspirin, preventing further metabolism. A. * NaHCO3; Increase B. NaHCO3; Decrease C. NH4Cl; Increase D. NH4Cl; Decrease E. None of the above 365. A patient presents with an overdose of alkaline Codeine. The drug ____ can be given to ____ the pH of the urine and trap the Codeine, preventing further metabolism. A. NaHCO3; Increase B. NaHCO3; Decrease C. NH4Cl; Increase D. * NH4Cl; Decrease E. None of the above 366. Bioavailability (F) is the fraction or percentage of administered drug that reaches the systemic circulation via a given route as compared to what route? A. Oral B. * IV (intravenous) C. IO (intraosseous) D. CSF (cerebrospinal fluid) E. Whatever route attains the target drug concentration in plasma (CT) 367. What organ is responsible for metabolism in the “first pass effect”? A. Brain B. Heart C. Kidney D. * Liver E. Spleen 368. Which of the following routes of administration is the most convenient, although may have a bioavailability anywhere from 5-100%? A. * PO (oral) B. IV (intravenous) C. IM (intramuscular) D. SQ (subcutaneous) E. Transdermal 369. Which of the following enteral administration routes has the largest first-pass effect? A. SL (sublingual) B. Buccal C. Rectal D. * Oral E. None of the above 370. Which of the following administration routes is not often used, is painful, and has a risk of infection and adhesion? A. EPI (epidural) B. IA (intraarterial) C. * IP (intraperitoneal) D. IV (intravenous) E. IO (intraosseous) 371. Which of the following is NOT an advantage of prolonged release medications? A. Less frequent administration B. Therapeutic effect overnight C. Lower incidence of side effects D. Patient compliance E. * More fluctuation in plasma concentration 372. Which of the following would receive drug slowly? A. Liver B. Brain C. * Fat D. Muscle E. Kidney 373. What type of drugs can cross the blood-brain barrier? A. Large and lipid-soluble B. Large and lipid-insoluble C. * Small and lipid-soluble D. Small and lipid-insoluble E. None of the above 374. Basic drugs, such as lidocaine, bind primarily to which of the following plasma proteins? A. alpha-1-fetoprotein (AFP) B. Gc-Globulin (GcG) C. Albumin D. * alpha 1-acid glycoprotein (AAG) E. Transcortin 375. A decrease in drug-protein binding will lead to which of the following? A. Decrease in the unbound drug concentration B. Increase in free drug C. * Increase in rate of drug elimination D. Decrease in volume of distribution E. None of the above 376. Which of the following locations can accumulate lipid-soluble drugs, has little or no receptors, and can hold distributed drugs like barbiturates? A. Liver B. Kidney C. D. E. 377. A. B. C. D. E. 378. A. B. C. D. E. 379. A. B. C. D. E. 380. A. B. C. D. E. 381. A. B. C. D. E. 382. A. B. C. D. E. 383. A. B. C. D. E. 384. A. B. C. D. E. 385. Brain * Fat Fetus Which of the following locations has high blood flow and is a site of excretion? Liver * Kidney Brain Fat Fetus What is the approximate lag time for equilibration between maternal blood and fetal tissues? 20 mins * 40 mins 1 hour 2 hours 6 hours Elderly patients often have ____ muscle mass and thus a(n) ____ Vd (volume of distribution). More; Increased More; Decreased Less; Increased * Less; Decreased None of the above Most drugs are active in their ____ form and inactive in their ____ form. * Non-polar; Polar Polar; Non-polar Water-soluble; Lipid-soluble Lipid-insoluble; Water-insoluble Neutral; Neutral Which of the following metabolically active tissues is the principle organ for drug metabolism? Skin Kidneys Lungs * Liver GI Tract What is the goal of the P450 system (microsomes pinched off from endoplasmic reticulum)? Metabolism of substances Detoxification of substances Increasing pH of compartments containing substances Decreasing pH of compartments containing substances * Metabolism of substances & Detoxification of substances The direct-acting plasminogen activator is: streptokinase * urokinase epsilon-aminocaproic acid anistreplase heparin The antithrombotic drug which inhibits cyclooxygenase enzymes is: prednisone dipyridamole tranexamic acid * aspirin ticlopidine The mechanism of action of mini-dose heparin is correctly described by: A. factor X is more sensitive to heparin than are other serine protease factors B. mini-dose heparin is useful prophylactically rather than during active clot formation C. by inhibiting factor X activation, a relative block of the clotting cascade develops, with less thrombin formed D. * All of the above E. None of the above 386. The correct statement about fibrinolytic agents is: A. streptokinase acts directly to activate plasminogen B. * urokinase acts directly to activate plasminogen C. tissue-type specific plasminogen activator is more fibrin specific than streptokinase D. side effects of t-PA include skin rash, allergic reactions, and development of antibodies E. have been shown to increase mortality when given in the setting of an acute myocardial infarction 387. Following drugs stimulate erythrogenesis EXCEPT: A. Iron dextran B. Vitamine B12 C. * Methotrexate D. Folic acid E. Aspirin 388. Which drug does not influence leucopoiesis? A. Filgrastim B. * Erythropoetin C. Doxorubicin D. Methotrexate E. All of the above 389. Iron deficiency anemia leads to: A. pallor B. fatigue C. dizziness D. exertional dyspnea E. * All of the above 390. Tick the drug for parenteral iron therapy: A. Ferrous sulfate B. * Fercoven C. Ferrous lactate D. Ferrous fumarate E. All of the above 391. Indicate the drug which increases absorption of iron from intestine: A. Cyanocobalamin B. Folic acid C. * Ascorbic acid D. Erythropoetin E. All of the above 392. The drugs used for oral administration EXCLUDE: A. Ferrous sulfate B. * Fercoven C. Ferrous lactate D. Ferrous fumarate E. None of the above 393. Pernicious anemia is developed due to deficiency of: A. Erythropoetin B. * Vitamin B12 C. Iron D. E. 394. A. B. C. D. E. 395. A. B. C. D. E. 396. A. B. C. D. E. 397. A. B. C. D. E. 398. A. B. C. D. E. 399. A. B. C. D. E. 400. A. B. C. D. E. 401. A. B. C. D. E. 402. A. Vitamin B6 Vitamin C Select the drug used for pernicious anemia: Ferrous lactate * Cyanocobalamin Iron dextran Ferrous gluconate Vitamin E An adverse effect of oral iron therapy is: Anemia Thrombocytopenia Headache * Constipation Hypertension Choose the drug which contains cobalt atom: Folic acid Iron dextran * Cyanocobalamine Ferrous gluconate Furosemid Tick the drug used in aplastic anemia: Fercoven Cyanocobalamine * Epoetin alpha Folic acid Methotrexate Folic acid is recommended for treatment of: * Megaloblastic anemia Shock Hypertension Leukemia None of the above Select the drug of granulocyte colony-stimulating factor: * Filgrastim Methotrexate Erythropoetin Doxorubicin Methotrexate All of the following groups of drugs are for thrombosis treatment EXCEPT: Anticoagulant drugs * Antifibrinolitic drugs Fibrinolitic drugs Antiplatelet drugs None of the above Pick out the drug belonging to anticoagulants of direct action: Aspirin * Heparin Dicumarol Phenprocoumon None of the above Tick the drug used as an oral anticoagulant: Heparin B. C. D. E. 403. A. B. C. D. E. 404. A. B. C. D. E. 405. A. B. C. D. E. 406. A. B. C. D. E. 407. A. B. C. D. E. 408. A. B. C. D. E. 409. A. B. C. D. E. 410. A. B. C. D. Daltreparin * Dicumarol Enoxaparin Fraxiparin Which of the following drugs has low-molecular weight? Dicumarol * Enoxaparin Phenprocoumon Heparin Aspirin Indicate the drug belonging to antagonists of heparin: Aspirin Dicumarol Dalteparin * Protamine sulphate Iron dextran All of the following drugs are indirect acting anticoagulants EXCEPT: Dicumarol Warfarin * Dalteparin Phenindione None of the above Which of the following drugs belongs to coumarin derivatives? Heparin Enoxaparin Dalteparin * Warfarin Aspirin Heparin is effective when administred: Orally * Parenterally Sublingually All of the above None of the above All of these drugs are antiplatelet agents EXCEPT: Aspirin * Urokinase Ticlopidine Clopidogrel Dipiridamol Mechanism of aspirin action is: Converts inactive plasminogen into active plasmin * Inhibits COX and thus thromboxane synthesis Enhances the interaction between antitrombin III and both thrombin and the factors involved in the intrinsic clotting cascade Inhibits the glycoprotein IIb/IIIa complex All of the above Which of the following drugs is an inhibitor of platelet glycoprotein IIb/IIIa receptors? Aspirin Clopidogrel Ticlopidine * Abciximab E. 411. A. B. C. D. E. 412. A. B. C. D. E. 413. A. B. C. D. E. 414. A. B. C. D. E. 415. A. B. C. D. E. 416. A. B. C. D. E. 417. A. B. C. D. E. 418. A. B. C. D. E. 419. A. B. Heparin Which of the following drugs is fiibrinolytic? Ticlopidine * Streptokinase Aspirin Warfarin Heparin Fibrinolytic drugs are used for following EXCEPT: Central deep venous thrombosis Multiple pulmonary emboli * Heart failure Acute myocardial infarction All of the above Indicate the drug belonging to fibrinoliytic inhibitors: * Aminocapronic acid Ticlopidine Streptokinase Vitamin K Vitamin C Aminocapronic acid is a drug of choice for treatment of: Acute myocardial infarction * Bleeding from fibrinolytic therapy Heart failure Multiple pulmonary emboli All of the above Which of the following substances has its major activity as a saline cathartic? sodium bicarbonate methylcellulose * sodium phosphate castor oil mineral oil The correct statement regarding sucralfate: pharmacologic action is to reduce gastric acid secretion by antagonizing gastrin enhances N+-K+ ATPase antagonizes acetylcholine * most common side effects is constipation increases gastric motility Correct statement regarding metoclopramide: central nervous system dopamine receptor agonist peripheral blockage of acetylcholine at muscarinic synapse decreases lower esophageal sphincter pressure * adverse effects include dystonic or extrapyramidal effects increases motility of colon In general, mechanisms of laxation include: adding bulk to the stool increasing peristaltic activity emulsifying aqueous and fatty substances with stool lubricating the passage of stool * All of the above Appropriate indications for and/or uses of laxatives include: prevent straining at the stool in patients with cardiovascular disease bulk forming agents for diverticular disease C. treatment of drug overdose D. * All of the above E. None of the above 420. Which of the following substances is most likely to cause systemic alkalosis? A. * sodium bicarbonate B. methylcellulose C. sodium phosphate D. castor oil E. mineral oil 421. Saline cathartics, such as sodium sulfate or magnesium sulfate: A. are safe in patients with renal failure B. are readily absorbed from the gastrointestinal tract C. are slower acting than bulk-forming laxatives D. * act by increasing intestinal volume, hence stimulating peristaltic action E. lower the surface tension of the feces to facilitate fecal hydration 422. Adverse effect(s) of laxatives: A. electrolyte disturbances (hypernatremia, hypokalemia) B. dehydration C. spastic colitis with stimulant laxatives D. gastrointestinal obstruction with bulk forming agents E. * All of the above 423. In esophagitis, elevation of the head of the bed, abstinence from ethanol and tobacco, and small frequent meals are all useful adjunctive therapeutic measures. Other useful therapy may include all of the following EXCEPT: A. omeprazole B. metoclopramide C. bethanechol D. cimetidine E. * amitriptyline 424. Drug which exerts anti-peptic ulcer effects through histamine-2 receptor antagonism: A. sucralfate B. ranitidine C. metoclopramide D. * omeprazole E. misoprostol 425. The substance which is principally an emollient laxative is: A. bran B. methylcellulose C. magnesium hydroxide D. phenolphthalein E. * mineral oil 426. Laxatives may aid in the treatment of portal systemic encephalopathy by: A. increasing stool pH B. increasing coliform bacteria C. * decreasing protein contact time with GI mucosa D. All of the above E. None of the above 427. Agents of potential use in peptic ulcer disease include: A. muscarinic antagonists B. proton pump inhibitors C. antacids D. prostaglandins E. * All of the above 428. Possible drug interactions: Aluminium hydroxide antacids tend to interfere with the gastrointestinal absorption of: A. cephalexin B. penicillin G C. erythromycin D. chloramphenicol E. * tetracycline 429. Prostaglandins E2 inhibit the secretion of gastric acid and stimulate the secretion of mucus. One adverse effect limiting the wide use of prostaglandins for gastric disease is: A. headache B. thrombocytopenia C. gynecomastia D. * diarrhea E. seizures 430. An agent which promotes defecation without increasing peristalsis is: A. castor oil B. phenolphthalein C. * docusate sodium D. cascara E. milk of magnesia 431. Cimetidine reduces the clearance of all of the following EXCEPT: A. theophylline B. phenytoin C. warfarin D. * digoxin 432. Antacids having a relatively non-systemic effect include: A. aluminum hydroxide B. sodium bicarbonate C. calcium carbonate D. all of the above E. * aluminum hydroxide and calcium carbonate 433. Which of the following substances has its major activity as an stimulant cathartic? A. sodium bicarbonate B. methylcellulose C. sodium citrate D. * castor oil E. mineral oil 434. One mechanism to reduce gastric acid secretion is by blocking the K+-Na+ATPase pump in the parietal cell. One drug that has this pharmacologic action is: A. misoprostol B. pirenzepine C. * omeprazole D. serotonin E. isoniazid 435. The amount of sodium, phosphate or magnesium contained in an antacid should be assessed when selecting an antacid for patients with: A. renal insufficiency B. congestive heart failure C. ascites D. * All of the above E. None of the above 436. The concomitant administration of calcium and/or magnesium antacids to patients receiving one of the tetracycline drugs may have which of the following effects upon the action of the tetracycline: A. enhances the action B. causes no significant change C. * decreases the action D. increases toxicity E. suppresses hypersensitivity reactions 437. Which of the following substances has its major activity as a saline cathartic? A. Sodium bicarbonate B. Aluminium hydroxide C. * Magnesium sulfate D. Calcium carbonate E. All of the above 438. In general, mechanisms of laxation include A. adding bulk to the stool B. increasing peristaltic activity C. emulsifuing aqenons and fatty substances with stool D. lubricating the passage of stool E. * all of the above 439. Drug which exerts anti-peptic effects through histamine-2 receptor antagonism: A. Denol B. * Ranitidine C. Omeprasole D. Aluminium hydroxide E. All of above 440. For treatment of heartburn patient regularly used some powder. After a week of drug using vomiting, nausea, abdomen pain, fibrillation, shallow and slow breathing, alkalosis. What drug used patient? A. * Natrii hydrocarbonas B. Aluminium hydroxide C. Magnesium sulfate D. Omeprasole E. Calcium carbonate 441. All these Drugs are cause obstipation Except: A. Anticholinergic agents B. Ca channel antagonists C. Opioids D. Tricyclic antidepressants E. * Muscarinic agonists 442. Plant fiber (a laxative, purgative) A. Decrease the bulk of the stools B. increases the bowel transit time C. * slowly distends the wall of the colon D. increases the effective caloric content of the diet E. takes down water and swells 443. Lactulose A. is a monosaccharide B. is broken down in the small intestine by bacteria C. is build to unabsorbed organic anions which retain fluid D. produces laxative effects after 2-3 hours E. * is of particular value in the treatment of hepatic encephalopathy 444. Lactulose is of particular value in the treatment of encephalopathy: A. B. C. D. E. 445. A. B. C. D. E. 446. A. B. C. D. E. 447. A. B. C. D. E. 448. A. B. C. D. E. 449. A. B. C. D. E. 450. A. B. C. D. E. 451. A. B. C. D. E. 452. A. B. C. D. * as it discourages the proliferation of ammonia producing organisms as it increases the absorption of ammonia as it decreases chronic portal hypertension as it treatment fever as it improves functions of CNS after absorption from the GIT Magnesium sulfate is a laxative which acts within 1-2 days dilates the gallbladder and relaxes the sphincter of Oddi decreases the secretion of cholecystokinin decreases gastric, intestinal and pancreatic secretion * should be given in dilute solution to a fasting individual Senna alcaloids (anthraquinones, the sennosides A and B) * act directly on the intramucosal plexus of the gut wall take about 8 minutes to produce an effect should be given to pregnant women should be given to nursing mothers can not induce diarrhea with excessive loss of water and electrolytes Glycerol (in the form of rectal suppositories) is useless if a rapid effect is required * acts as a rectal stimulant due to local irritant action cannot be used in children rectal suppositories promote colonic evacuation in 30 hours exerts severe diarrhea with loss of water and electrolytes All these drugs are increasing intestinal transit time Except: codeine (an opioid) morphine (an opioid) loperamide diphenoxylate * fysostigmin Peptic ulcer disease is an acute disorder * characterized by frequent recurrences comprises bones the incidence of duodenal ulcers is four to five times lower than that of gastric ulcer affects approximately 50% of the population All these are major factors of known importance for the etiology of ulceration Except acid-pepsin secretion mucosal resistance to attack by acid and pepsin * the age effects of non-steroidal anti-inflammatory drugs the presence of Helicobacter pylori Acid secretion is produced by endocrine cells in the gastric antrum cells * is stimulated by gastrin is inhibited by acetylcholine is inhibited by histamine is stimulated by prostaglandin E Antacids: * react with gastric acid to form a neutral salt produce sweating are Ineffective at healing duodenal ulcer are very effective at healing gastric ulcers E. 453. A. B. C. D. E. 454. A. B. C. D. E. 455. A. B. C. D. E. 456. A. B. C. D. E. 457. A. B. C. D. E. 458. A. B. C. D. E. 459. A. B. C. D. E. 460. A. B. C. D. E. 461. A. B. its effect on acid secretion lasts for long (5 hours) Antacids include: balsalazide orlistat cimetidine sucralfate * aluminium salts (hydroxide, phosphate, glycinate) Sodium bicarbonate (an antacid) acts only locally * excessive doses produce systemic alcalosis produces carbon monoxide by reacting with hydrochloric acid causes belching and distension of the large intestine sodium intake need not to be considered in patients with hypertension or heart failure Magnesium and aluminium salts do undergo absorption so are effective locally magnesium salts are constipating, aluminium salts may produce diarrhea can not reduce the rate and extent of absorption of other drugs aluminium salts should not be used with caution with any renal compromise * magnesium and aluminium salts are taken 1-3 hours after meals and at bedtime H2 lytics: at least 4 days treatment is required to achieve healing pain is relieved within 4 weeks treatment include morphine , tramadol * include nizatidine, ranitidine, famotidine include pirenzepine Ranitidine (ZANTAC) has higher affinity for cytochrome P 450 than cimetidine is less expensive than cimetidine * is preferable to cimetidine in the elderly has a similar profile of action to paracetamol increases the plasma levels of theophylline Pirenzepine * is an M1 muscarinic receptor antagonist can not cause mild difficulty with accomodation and dry mouth can not alter the rate of absorption of other drugs if given concurrently can be used in patients with concomitant glaucoma can be used in patients with pyloric stenosis and prostatic enlargement Omeprazol is an irreversible stimulator of the proton pump can be used only for healing gastric ulcer Is for women only is taken once weekly * degrades in the presence of moisture. Capsules are supplied in special containers Misoprostol * is a synthetic analog of prostaglandin E1 produces gastric acid secretion causes Stricture in the submucosa decreases production of protective mucus is indicated especially in pregnancy Sucralfate is less effective than cimetidine is not so effective in symptom relief C. antacids are contraindicated D. contains aliminium, diarrhea can not be induced E. * in severe renal failure accumulation is a potential hazard. 462. Cisapride A. inhibits motility of the GIT B. decreases rate of gastric emptying C. is not used in gastroesophageal reflux D. * is used in dyspepsia and delayed gastric emptying E. is used in diarrhea 463. Metoclopramide is effective for: A. preoperative vomiting B. vestibular disturbances C. motion sickness D. headache E. * facilitation of duodenal intubation and endoscopy 464. Drugs with a bacteriostatic effect in regular doses include: A. tetracyclines B. None of the above C. sulfamethoxazole and trimethoprim (Sumetrolim) D. erythromycin E. * All of the above 465. The use of which of the following should be avoided in patients receiving monoamino-oxidase inhibitor therapy: A. cheese B. imipramine (Melipramin) C. None of the above D. pethidine (Dolargan) E. * All of the above 466. Penicillin administration is the appropriate therapy in which of the following complications of syphilis? A. * meningitis B. aneurysm of the aorta C. interstitial keratitisD. none of the above E. the generalized paralysis of psychotic patients 467. Which of the following conditions is associated with true hematuria? A. urinary tract tuberculosis B. acute cystitis C. renal infarction D. none of the above E. * all of the above 468. Which of the following signs can be attributed to an iron deficiency anemia? A. a pale color of the sclera B. hepatosplenomegaly C. glossodynia (pain in the tongue) D. * all of the above E. none of the above 469. Haloperidol: A. has marked extrapyramidal side effects B. has a marked antiemetic effect C. can be used to substitute for phenothiazine derivatives in patients who become jaundiced following phenothiazine administration D. E. 470. A. B. C. D. E. 471. A. B. C. D. E. 472. A. B. C. D. E. 473. A. B. C. D. E. 474. A. B. C. D. E. 475. A. B. C. D. E. 476. A. B. C. D. E. 477. A. B. C. D. E. 478. A. * all of the above none of the above Indications of penicillamine therapy include: systemic sclerosis primary biliary cirrhosis hemosiderosis * all of the above none of the above The side effects of corticosteroids include: a loss of collagen decreased leukocyte migration avascular bone necrosis * all of the above none of the above Digitalis therapy: is contraindicated in atrial tachycardia * elongates the effective refractory period of the AV node is likely to cause intoxication with a concomitant hyperkalemia is contraindicated in cor pulmonale is effective in hypertrophic obstructive cardiomyopathy Possible therapeutic interventions in thyrotoxic crisis include: the administration of beta-blockers immediate propylthiouracil treatment the administration of iodine * all of the above none of the above Osteoporosis: causes an elevation of the serum calcium concentration typically causes elevation of the alkaline phosphatase activity * causes pain in the bones improves during bed rest the response to calcium substitution therapy is usually positive Barbiturates, if continuously administered can: induce physical dependence cause relaxation of skeletal muscles cause ataxia * all of the above none of the above Megaloblastic anemia is a possible side-effect of: carbamazepine therapy primidone (Sertan) therapy methotrexate therapy sulfamethoxazole and trimethoprim (Sumetrolim) therapy * all of the above Possible initial symptoms of diabetes mellitus include: polydipsia polyuria severe pruritus * all of the above none of the above In the nephrotic syndrome: A generalized edema is present B. the administration of steroids is always ineffective C. favourable treatment includes the management of any underlying disease D. * a generalized edema is present + favourable treatment includes the management of any underlying disease E. none of the above 479. In acute pyelonephritis: A. * a common symptom is shaking chills B. the absence of any lumbar pain excludes the diagnosis C. an intravenous pyelogram is necessary for the diagnosis D. to confirm the diagnosis, a hemoculture should routinely be made E. all of the above 480. Immunosuppressive therapy is suitable in which of the following conditions? A. psoriatic arthritis B. * psoriatic arthritis + rheumatoid arthritis C. persistent viremia D. rheumatoid arthritis E. all of the above 481. Which of the following statements about nitroglycerin are correct? A. only topical application is effective in Raynaud's disease B. it causes paroxysmal nocturnal dyspnea as a side-effect C. it relieves the pain caused by diffuse esophageal spasms D. * it might relieve pain in biliary colic E. it alleviates the symptoms of bronchial asthma 482. Laboratory findings characteristic for early nephrotic syndrome include: A. a serum albumin level which is lower than 25 g/1 B. a decreased fibrinogen level C. an elevated serum cholesterol level D. * a serum albumin level which is lower than 25 g/1 + an elevated serum cholesterol level E. all of the above 483. A widely used drug that supresses cellular immunity, inhibits prostaglandin and leukotriene synthesis, and increases the catabolism of IgG antibodies is A. Cyclophosphamide B. Cyclosporine C. Infliximab D. Mercaptopurine E. * Prednisone 484. What drug is mostly used for the treatment of chronic lymphatic leukemia? A. * Chlorambucil B. Prednisone C. Cyclophosphamide D. Myleran E. Penicillin 485. Which of these groups is the most likely to experience anemia? A. Men B. * Women C. Teenagers D. Older adults E. None of the above 486. How does anemia affect the body? A. * The body is less able to absorb oxygen from the lungs B. Blood becomes thin C. Tissues retain fluids D. None of the above E. All of the above 487. The body needs an adequate supply of which of these in order for red blood cells to mature normally? A. Oxygen B. vitamin C C. * vitamin B-12 and folic acid D. Carbon dioxide E. None of the above 488. All of the following may cause microcytic hypochromic anaemia, except: A. * Vitamin B12 deficiency B. Thalassemia C. Iron deficiency D. Gastrointestinal bleeding E. Lactation 489. The sign of iron deficiency anaemia are all of the following except: A. Increase in iron binding capacity B. Decrease in serum ferritin level C. Decrease in serum iron level D. Decreased MCV E. * Hyper-segmented neutrophils 490. The sign of megaloblastic anaemia is: A. Increase in iron binding capacity B. Decrease in serum ferritin level C. Decrease in serum iron level D. Decreased MCV E. * Hyper-segmented neutrophils 491. The earliest sign of iron deficiency anaemia: A. Increase in iron binding capacity B. * Decrease in serum ferritin level C. Decrease in serum iron level D. Decreased MCV E. Transferrin saturation 492. All of the following statements are true about sickle cell disease except A. Vaso-occlusive crisis B. Aplastic Crisis C. * Hypertensive crisis D. Sequestration Crisis E. Hyperhemolytic crisis 493. Which is not seen in a chronic case of Sickle cell anemia: A. Hepatomegaly B. Pulmonaryhypertension C. Cardiomegaly D. Splenomegaly E. * Peripheral neuropathy 494. Commonest acute presentation of sickle cell anaemia is: A. Priapism B. * Bone pain C. Fever D. Splenomegaly E. Pulmonary hypertension 495. All of the following are the signs of anemia EXCEPT A. B. C. D. E. 496. A. B. C. D. E. 497. A. B. C. D. E. 498. A. B. C. D. E. 499. A. B. C. D. E. 500. A. B. C. D. E. 501. A. B. C. D. E. 502. A. B. C. D. E. 503. A. B. C. D. Malaise Dyspnea on exertion Increasing cardiac output Palpitations * Dyspepsia All of the following are the signs of anemia except Malaise Pallor Increasing cardiac output Palpitations * Dysphagia For diagnosis of anemia clinicians request all of the following except Complete blood counts Red blood cells * Leukocyturea Hemoglobin level MCV When the cause of anemia is not obvious, clinicians use all of the following tests except Ferritin Serum iron * Fibrinogen Serum vitamin B12 RBC folate level Normocytic anemia are all of the following except Acute blood loss Anemia of chronic disease Aplastic anemia (bone marrow failure) Hemolytic anemia * Vitamin B12 deficiency The average blood volume for an adult is about 45 liters 450 ml 5 gallons * 5 liters 3 liters Which statement concerning blood viscosity is CORRECT? The viscosity of blood is 4.5 to 5.5 higher than the viscosity of water. * Blood viscosity is due to the presence of the plasma proteins and erythrocytes. The higher the blood viscosity the harder the heart has to work to move blood through the vessels Anemia increases blood viscosity. Hypocoaculation increases blood viscosity. Other than water, the most common component of plasma is Chloride Urea * Protein Sodium Calcium Decrease in numbers of red blood cells or hemoglobin within red blood cells: * Anemia Erythrocytosis Thrombocytosis Leukemia E. Leukocytosis 504. Which type of anemia has a 54-year-old man with artificial aortic value and fatigue, palpitations, tachypnea on exertion, jaundice? A. Iron deficiency anemia, B. Megaloblastic anemia, C. * Hemolytic anemia D. Folic acid deficiency anemia, E. B12 vitamin deficiency anemia 505. Which of signs is characteristic for hemolytic anemia? A. * Jaundice B. Pale lips C. Sore mouth D. Weakness E. Fatigue Situational tasks: 1. The patient suffers from hypertensive disease with bradiarrhythmia. What drug is necessary to 2. 3. 4. 5. prescribe? A. * Platyphyllini hydrotartras B. Ceftriaxone C. Papaverinum D. Paracetamol E. Methyldopa The 45 years old patient has diagnosis Angina pectoris. Cardiosclerosis. Arrhythmia. Hypertensive disease. Choose the drug for treatment? A. * Nebivolol B. Suprastine C. Potassium chloride D. Strophantine E. Lidocaine At the patient after injecting drug for the medical treatment of hypertensive crisis tachycardia, and orthosthatic hypotension in the vertical position has developed. What drug was injected? A. Reserpine B. * Clophelinum C. Magnesium sulfate D. Dibazolum E. Verapamilum To the patient with hypertensive disease was prescribed a drug from the adrenotropic group. After some time the pressure normalized, but developed bradycardia (50 beats on minute) and the atrioventricular block. What drug was prescribed? A. * Propranolol B. Papaverinum C. Clophelinum D. Mesatonum E. Verapamilum The 45 years old patient with the hypertensive disease has been taking antihypertensive drug during 4 days. The blood pressure normalized but somnolence and dry cough developed. What drug has been taking the patient? A. Clophelinum B. Prazosinum C. * Enalapril D. Aspirine E. Adrenaline 6. The 56 years old woman with hypertensive disease appealed to the doctor. Methyldopa was 7. 8. 9. 10. 11. 12. prescribed to her. Indicate a mechanism of action of this drug. A. * Violation of noradrenalin synthesis B. Increasing of acetylcholine synthesis C. Block of beta-adrenoreceptors D. Block of alpha-adrenoreceptors E. Depression of angiotensin converting enzyme activity Patient with diagnosis of pheochromocytoma suffers from the high blood pressure which outgrows in hypertensive crisis. What group of drugs will help in this situation? A. Beta- adrenoblockers B. Ganglionblockers C. Sympatolitics D. * Alpha-adrenoblockers E. Calcium channels blockers During assessment of a patient diagnosed with pheochromocytoma, the doctor reveales a blood pressure of 210/110 mm Hg. The nurse would expect to administer which of the following medications? A. nadolol B. * phentolamine C. dobutamine D. verapamil E. validolum In the patient with the considerable peripheral edema the by turns using of dihlothiazid, ethacrynic acid and Furosemide did not result in the considerable diuretic effect. The analysis of blood indicated the considerable increasing of aldosteron level. Prescribe drug for treatment. A. Mannitol B. * Spironolactone C. Clopamid D. Triamterene E. Amiloride To the 55 years old man for the medical treatment of gout was prescribed etamid. What is the mechanism of uric actions of the drug? A. * Depression of reabsorbing of urinary acid B. Increasing of secretion of urinary acid C. Decreasing of production of urinary acid D. Depression of activity of ksantinoxydase E. Production of easy soluble salts At the 46 years old patient with blink arrhythmia the edema of lungs began. What drug is necessary to inject in the first turn? A. * Furosemide B. Triamterene C. Verospirone D. Amiloride E. Euphylline To the patient with edema of cardiac origin the doctor must prescribe diuretics. What drugs are contraindicated in this situation? A. Hypothiazid B. Spironolactone C. Furosemide D. * Mannitol E. Diacarb 13. In the patient with the considerable peripheral edema using of dihlothiazid did not result in the 14. 15. 16. 17. 18. 19. considerable diuretic effect. The analysis of blood indicated the considerable increasing of aldosteron level. Prescribe drug for treatment in this situation. A. Mannitol B. * Spironolactone C. Ethacrynic acid D. Furosemide E. Diacarb In the complex medical treatment of hypertensive disease a diuretic was prescribed to the patient. In a few days the BP went down, but the signs of hypokaliaemia arose up. What drug could cause such complication? A. Triamterene B. Clofeline C. Enalapril D. Spironolactone E. * Furosemide A patient with Type I diabetes presents with significant water retention and pulmonary congestion. Serum creatinine and potassium were significantly elevated. The diagnosis was advanced renal failure. A diuretic was given to treat water retention, but shortly thereafter the patient exhibited cardiac conduction changes which progressed to heart block and cardiac arrest. The diuretic which was determined to cause this event was probably: A. furosemide (Lasix) B. * triamterene (Dyrenium) C. chlorothiazide (Diuril) D. bumetanide (Bumex) E. None of the above The patient, who used prescribed preparation for a long time to treat acute respiratory diseases, suffered from headache, vertigo, and noise in his ears, nausea, pain in epigastria region. What preparation can cause such effects? A. Midantan. B. Vitamin C. C. Naphthysini. D. Bromhexini. E. * Acetylsalicylic acid. The patient, who suffered from irritability, sleeplessness, rapid fatigability and pain in the heart, consulted a doctor. What preparation must be prescribed? A. * Tincture Valerianae. B. Sodium bromide. C. Aminasin. D. Droperidol. E. Phenazepam. A 46-year-old patient has ischemic heart disease, angina on exertion, II functional class. What is the drug of choice in treatment of acute attack? A. * Nitroglycerin sublingually B. Platelet inhibiting agents (aspirin) C. Spasmolitics (No-spa) IV D. Digitalis IV E. Sedative agents (Seduxenum) orally A 52-year-old patient complains of intensive and prolonged retrosternal pains, decreased exercise tolerance for 5 days. Which of the following groups is the most useful? A. * nitrates dyslipidemic drugs diuretics digitalis ACE inhibitors A 50-year-old patient was admitted to resusitation department with aqute myocardial infarction . Which one of the following drugs is uneffective in this case? A. Proranolol B. Nitroglycerin C. * Nifedipine D. Phentanyl E. Morfin A 55-year-old men has stenocardia on exertion II. Taking of nitroglycerin potentiate a sever headache. Which of the following drugs is the most useful in this case? A. * Molsidomin B. Amiodaron C. Nifedipine D. Propranolol E. Verapamil A 49-year-old patient has ischemic heart disease, angina on exertion, II functional class. What is the drug of choice in treatment of acute attack? A. No-spa IV B. Aspirin C. * Nitroglycerin sublingually D. Digitalis IV E. Seduxenum orally A patient of 42 year has arterial hypertension with bradyarrhythmia. Which of the following drugs is necessary to administer? A. Klonidine B. * Nifedipine C. Diltiazem D. Bisoprolol E. Methyldopa A 45-year-old women with diagnosis: Paroxysmal arrhythmia. Arterial hypertension II. Drug of choice for stopping attack: A. * Metoprolol B. Nitroglycerin C. Potassium chloride D. Digoxin E. Lidocain A woman 56 years old with hypertension edema develops on lower extremities, moist wheezes in the lower parts of lungs. What must be administered in the complex therapy of the patient? A. Betaadrenomimetics, B. * Diuretics, C. Glucocorticoids, D. Preparations of calcium, E. M-cholinolitics. A woman 51 years old has arterial hypertension. Which group of drugs may be used for her treatment? A. Betaadrenomimetics, B. * Angiotensin-converting enzyme inhibitors, C. Glucocorticoids, D. Preparations of calcium, B. C. D. E. 20. 21. 22. 23. 24. 25. 26. E. M-cholinolitics. 27. A man 36, years old, has arterial hypertension. Which group of drugs may be used for treatment? A. Betaadrenomimetics B. Preparations of calcium, C. Glucocorticoids, D. * Calcium_channel inhibitors, E. M-cholinolitics. 28. Patients suffering from congestive heart failure will show signs and symptoms of peripheral 29. 30. 31. 32. 33. 34. vasoconstriction, moist skin, pale complextion because of: A. Na and water retention B. decreased renin release C. * increased sympathetic tone D. decreased vagal tone E. decreased aldosterone levels The 56 years old woman with hypertensive disease appealed to the doctor. Methyldopa was prescribed to her. Indicate a mechanism of action of this drug. A. Violation of noradrenalin synthesis B. * alpha-adrenoreceptors blockers C. Block of beta-adrenoreceptors D. Depression of angiotensin converting enzyme activity E. Increasing of acetylcholine synthesis In the complex medical treatment of hypertensive disease a diuretic was prescribed to the patient. In a few days the blood pressure went down, but the signs of hypokaliaemia arose up. What drug could cause such complication? A. Triamterene B. Clofeline C. Enalapril D. Spironolactone E. * Furosemide The patient has cranial trauma. The brain edema threat developed in the postoperative period. To prescribe drug for the removal of this complication. A. Spironolactone B. Papaverini hydrochloride C. * Furosemide D. Dihlothiazid E. Diacarb In the patient with the considerable peripheral edema the by turns using of dihlothiazid, ethacrynic acid and furosemide did not result in the considerable diuretic effect. The analysis of blood indicated the considerable increasing of aldosteron level. Prescribe drug for treatment. A. Mannitol B. * Spironolactone C. Clopamid D. Triamterene E. Amiloride At the 46 years old patient with blink arrhythmia the edema of lungs began. What drug is necessary to inject in the first turn? A. * Furosemide B. Triamterene C. Verospirone D. Amiloride E. Euphylline An elderly male patient has essential hypertension, congestive heart failure, and type I insulin- 35. 36. 37. 38. 39. dependent diabetes. His congestive failure developed secondary to coronary vascular disease associated with hyperlipidemia. What antihypertensive drug(s) may be most appropriate for this patient? A. Chlorothiazide (Diuril) B. * captopril (Capoten) C. propranolol (Inderal) D. metoprolol (Lopressor) E. none of the above An elderly female patient has essential hypertension, congestive heart failure, and type I insulindependent diabetes. His congestive failure developed secondary to coronary vascular disease associated with hyperlipidemia. What antihypertensive drug(s) may be most appropriate for this patient? A. chlorothiazide B. * lisinopril C. propranolol D. metoprolol E. all of the above A patient presents with a blood pressure of 160/110 mm Hg. The patient has a history of coronary vascular disease, resulting in angina, but has no evidence of congestive heart failure. The patient also has asthma and has been treated mainly using terbutaline, by aerosol inhalation Propranolol (Inderal) was prescribed to manage essential hypertension. Was this action appropriate? A. Propranolol (Inderal) is appropriate because it will reduce heart rate and cardiac output. Negative inotropism will help reduce the incidence of angina. It is an effective antihypertensive agent B. Propranolol (Inderal) is inappropriate because it is only useful in mild hypertension; a better drug would be minoxidil or hydralazine because they are more effective in lowering blood pressure C. Propranolol (Inderal) is appropriate because it is an effective, low-cost antihypertensive. It will augment the effects of terbutaline, an additional benefit D. * Propranolol (Inderal) is inappropriate because its use is contraindicated in a patient with asthma. E. All of the above The patient with severe allergic bronchial asthma has been treated by oral drug during 7 months. Hypertension, “moon face”, obese trunk, oedema, insomnia occur. What drugs does he used? A. * Patient used one of orally used glucocorticoids, e.g. prednisolonum. B. Patient used one of beta-agonists. C. Patient used cromolynum. D. Patient used euphyllinum E. Patient used all above. Patient 65 years old suffers from bronchial asthma. Adrenergic receptor activator is used for treatment, After two weeks of management a pain near heart, palpitation. How can these side effects be prevent? It is necessary to prescribe A. * selective beta2-adrenergic receptor stimulator, for example salbutamolum. B. glucocorticoids. C. theophylline. D. anticholinergics E. cromolyn sodium. An 81-year-old female with arteriosclerotic heart disease and pulmonary emphysema was found to have significant bronchospasm. Her physician prescribed theophylline 400 mg every 12 hours. All of the following toxicities may be observed EXCEPT: A. cardiac arrhythmias B. nausea and vomiting C. agitation D. * sodium and water retention E. tremulousness 40. During auscultation of patient P., 60 years old, with chronic non-obstructive bronchitis, dry buzzling 41. 42. 43. 44. 45. 46. rales above all parts of the lungs were heard as well as weakened vesicular breathing. What medical preparation is it necessary to prescribe to the patient? A. Diuretics; B. Antitussive agents; C. * Expectorants; D. Broncholitics; E. beta-blockers. A 56-yr-old man wheezes and coughs. He has tried to give up smoking, but he finds it very difficult. He is thin and healthy looking with a rounded chest. His breathing is noisy. His cough is unproductive. What treatment has to be prescribed? A. Amoxycillin B. Prednisolone C. * Ipratropium D. Salbutamol E. Bronchial lavage A 20-yr-old woman presents with a week's history of fever, rigors arid productive rusty cough. CXR shows right lower lobe consolidation. Prescribe treatment A. Erythromycin B. Co-trimoxazole C. Prednisolone D. * Amoxicillin E. Salbutamol inhaler Patients having a history of a severe, immediate reaction to penicillin: A. may be given a cephalosporin without concern; B. have a definite risk of reaction to any cephalosporin; C. have a low risk of having a reaction to a broad spectrum antipseudomonal penicillin; D. have a high risk of hypersensitivity to a broad spectrum anti-pseudomonal penicillin E. * have a definite risk of reaction to any cephalosporin & have a high risk of hypersensitivity to a broad spectrum anti-pseudomonal penicillin A 23 years old patient is pregnant with a history of severe (anaphylactic) penicillin allergy. To prepare her for an upcoming tooth extraction a doctor prescribes an antimicrobial medication that can be taken prophylaxis 2 hrs prior to the procedure. This medication is A. Cefaclor B. Doxycycline C. Erythromycin base D. * Erythromycin stearate E. Gentamycin Circumstances associated with allergy to penicillins may include: A. maculopapular or urticarial rash; B. anaphylaxis; C. anaphylactic reaction to penicillin skin-tests; D. exposure to penicillins in food E. * All of the above A week after initiating clindamycin therapy a patient develops signs of a potentially fatal infection of the colon. His tests reveal that his infection is due to clostridium difficile, to treat this new condition you should initiate drug therapy with A. a higher dose of clindamycin B. gentamicin i.v C. linezolid D. * metronidazole E. rifampin 47. Imipenem is a beta-lactam antibiotic which is neither a penicillin nor a cephalosporin. Correct 48. 49. 50. 51. 52. 53. statements regarding imipenem include: A. it covers an extremely broad spectrum of microorganisms; B. it is very active against many gram negative rods; C. resistant pseudomonas may emerge during treatment; D. it should not be given to patients having a history of allergic reactions to penicillin E. * All of the above A patient with pulmonary disease is taking prednisone. A doctor begins her on phenytoin therapy for a newly diagnosed seizure disorder. Two weeks later the patient returns to the clinic to see the doctor and complains that her pulmonary disease has worsened since she began the phenytoin therapy. A likely reason for this new change is that phenytoin: A. interferes with absorption of the prednisone B. stabilizes cell membranes, preventing the prednisone from diffusing to the site of action C. * accelerates hepatic degradation of the prednisone D. induce renal excretory pathways, accelerating urinary excretion of the prednisone E. activates the asthma directly A 21-year-old male has been brought to the emergency room unconscious three hours after ingestion of a large dose of barbiturate. The immediate method of management would be: A. administer concentrated dextrose intravenously B. perform hemodialysis immediately with an artificial kidney C. administer an analeptic drug such as pentylenetetrazol D. * maintain a clear airway and artificially assist ventilation of air E. exchange is unsatisfactory Which of the following are true regarding cephalosporins? A. "third generation" cephalosporins are generally more active against gram-negative organisms; B. cephalosporins may depress beta-lactamase in certain organisms (Enterobacter, pseudomonas, serratia) causing production of the enzyme to increase markedly; C. the enzyme in part B above binds to the cephalosporin; D. enterococcus is never reliably sensitive to any available cephalosporin E. * All of the above The administration of one drug may stimulate the metabolism of another drug (enzyme induction). Phenobarbital is an example of such an enzyme inducer. The metabolism of which of the following drugs may be affected by phenobarbital administration? A. warfarin B. phenytoin C. digitoxin D. * All of the above E. None of the above In the differential diagnosis of hirsutism, drug-induced hirsutism must be considered. A drug which is known to include hirsutism as a side- effect is: A. thallium B. heparin C. cephalosporins D. * phenytoin E. diazepam A patient comes to the office complaining of sore, enlarged gums. She is currently taking medication for hypertension and phenobarbital and phenytoin for seizures. The fibrous hyperplasia is most probably due to: A. * phenytoin B. excessive brushing of teeth C. propranolol D. staphylococci infection of gums E. phenobarbital 54. Appropriate indications for and/or uses of laxatives include: A. * All are correct B. prevent straining at the stool in patients with cardiovascular disease; C. bulk forming agents for diverticular disease; D. treatment of drug overdose; E. None of the above 55. In esophagitis, elevation of the head of the bed, abstinence from ethanol and tobacco, and small 56. 57. 58. 59. 60. frequent meals are all useful adjunctive therapeutic measures. Other useful therapy may include all of the following EXCEPT: A. omeprazole B. metoclopramide C. bethanechol D. cimetidine E. * amitriptyline What drug used patient? For treatment of heartburn patient regularly used some powder. After a week of drug using vomiting, nausea, abdomen pain, fibrillation, shallow and slow breathing. Biochemical examination show alkalosis. A. * Natrii hydrocarbonas B. Aluminium hydroxide C. Magnesium sulfate D. Omeprasole E. Calcium carbonate A doctor is caring for a client with a diagnosis of rheumatoid arthritis who is receiving sulindac (Clinoril) 150 mg po twice daily. Which finding would indicate to the doctor that the client is experiencing a side effect related to the medication? A. * nausea B. photophobia C. fever D. tingling in the extremities E. All of the above To the patient with gout the doctor prescribed allopurinol. What pharmacological property of allopurinol is important in this situation? A. * Competitive inhibition of xantinoxydase. B. Increasing of evacuation of nitrogen substances. C. Acceleration of catabolism of pirimidinic nucleotides D. Decreasing of reutilization of pirimidinic nucleotides E. Increasing of synthesis of nucleic acids At the 42 years old man with gout the concentration of urinary acid in the blood increased. For the decline of level of urinary acid allopurinol was prescribed to him. What enzyme is allopurinol competitive inhibitor of? A. * Xantinoxydase B. Adeninphosphoriboziltransferase C. Hypoksantinphosphoriboziltransferase D. Guanindesaminase E. Adenosindesaminase The patient, who suffered from irritability, sleeplessness, rapid fatigability and neurosis has been diagnosed. What agents can be prescribed? A. Anapriline. B. Sodium chloride C. Aminasine. D. Atropine. E. * Sibasone. 61. The patient, who suffered from anxiety, fear, hesitancy Sibasone has been prescribed. What is the 62. 63. 64. 65. 66. 67. 68. mechanism of its tranquilizing activity? A. * Interaction with benzodiazepine receptors. B. Interaction with adrenergic receptors. C. Interaction with cholinergic receptors. D. Interaction with serotonin receptors. E. Interaction with dophaminergic. The patient, who suffered from hyper excitability, irritability, sleeplessness was prescribed phenazepam. What is the mechanism of its action? A. * Stimulation of benzodiazepine receptors. B. Stimulation of GABA (gamma amino butyric acid) receptors. C. Stimulation of beta-adrenergic receptors. D. Stimulation of M-cholinergic receptors. E. Stimulation of H-cholinergic receptors. The patient, suffered from schizophrenia, was prescribed aminazine for delusion and hallucinations reducing. What is the mechanism of its antipsychotic action? A. * Block adrenergic dophaminergic receptors in CNS. B. Stimulate adrenergic dophaminergic receptors in CNS. C. Stimulate cholinergic receptors in CNS. D. Block cholinergic receptors in CNS. E. Inhibition of re-uptaking of MAO. The patient instead aminasine was prescribed another neuroleptic. What drug belongs to this group? A. * Haloperidole. B. Phentanile. C. Paracetamol D. Sibasone. E. Morphine. The physician monitors a patient taking an antipsychotic medication for side effects, including: A. Hyper salivation B. Hypetension C. Diarrhea D. * Extrapyramidal syndrome E. Cramps At the hands of nurse, working at the psychiatric unit during two years symptoms of neurodermatitis appears. What drug can cause such adverse effect? A. * Aminazine B. Morphine. C. Paracetamol. D. Atropine. E. Diasepam For the patient with depression was prescribed Nialamide. The physician informed patient about necessity to remove from the diet during of medical treatment: A. Apples B. * Cheese C. Potatoes D. Cabbages E. Pears To the patient for the removal of depressed syndrome was prescribed inhibitor of monooxygenase (MAO). What food products are necessary to remove from the patient’s diet? A. * Hard sorts of cheese, bananas, peanut, B. Cabbages, cucumbers, tomatoes, C. Millet, buckwheat, D. milk porridges, E. Honey, fruits 69. The old patient complains to headache, dizziness, rapid fatigue, worsening a memory. In anamnesis is cranial-cerebral trauma. What pharmacological group is necessary to prescribe? A. Hypnotics, B. Neuroleptics, C. Tranquilizers, D. * Nootrops, E. Analgetics 70. The physician notes lithium on a patient's drug history upon admission. The physician would suspect that this patient suffers from: A. Obesity B. Abstinent syndrome C. Renal disorder D. * Manic episodes E. All of the above 71. The problem of skeletal muscle contraction exist at child after poliomyelitis. What medicine is possible to prescribe? A. * Galantamine hydrobromide B. Platyphylline C. Methacine D. Atropine sulfate E. Tubacurarine