Biology 2402 A&P II - Lymphatic System and Immunity Ch. 14
advertisement

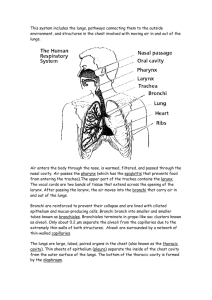
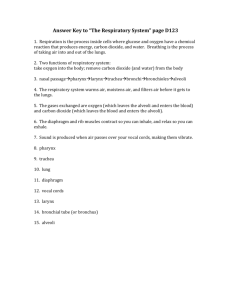
Biology 2402 A&P II - Lymphatic System and Immunity Ch. 14 Functions: Fluid balance by returning excess tissue fluid to the blood; returning solutes (especially plasma proteins) to the blood; filter body fluids to remove tissue debris, foreign material; defend body by production of lymphocytes and immunity; movement of larger substances into blood (lipids from intestine, etc.) Review terms for fluids in the body: intracellular intercellular (interstitial, tissue fluid) blood plasma lymph & plasma proteins Structure of the lymphatic system: Lymph Vessels Fig. 14.1-14.4 - begin as lymph capillaries, in almost all tissues close to blood capillary - very thin wall, single layer of epithelial cells, large lumen (central opening) - ends of capillaries closed, blind tubes - edges of epithelial cells not attached in places and work as inward “trap doors” - anchoring filaments assist - therefore, large particles can enter, but not leave - lymph capillaries merge to form larger and larger vessels, ending in the right and left (thoracic) lymphatic ducts that empty into the left and right subclavian veins. - thin wall, low pressure flow, have one-way valves similar to veins - lymph movement is caused by same forces as blood in veins. *Explain how lymph capillaries can take in larger particles than can enter blood capillaries. *The pressure of tissue fluid is very low (2 mm Hg). What forces move lymph through lymph vessels? (Hint: lymph vessels are built similar to, and parallel, veins) *Why are malignant (cancer) cells able to spread through the lymphatic system so easily? Lymphoid tissue (lymphatic tissue) Fig. 14.6 - 14.10 Composed of a network of loose and reticular connective tissue fiber framework with lymphocytes and macrophages. Fluid “trickles” through, macrophages destroy foreign cells and lymphocytes exposed to antigens. Lymph nodules (diffuse lymphatic tissue) not enclosed in fibrous capsule - located beneath epithelial tissue of respiratory, digestive, urinary systems - tonsils are examples, filter tissue fluid Lymph nodes enclosed in fibrous capsule, connected to several afferent lymph vessels and one efferent lymph vessel - filter lymph Spleen is encapsulated lymphatic tissue that filters blood, composed of white pulp (typical lymphatic) and red pulp (sinuses filled with blood). - filters blood of foreign cells and material and damaged red blood cells - serves as a blood reservoir (about 5% of blood volume into circulation) Thymus is organ where T cells mature and develop ability for immune response *Describe the structure of lymphoid tissue as a filter. Why as part of lymph vessels but not blood vessels? Body Defenses Innate (nonspecific) defenses or resistance - general and wide range, prevent entry or destroy foreign material in the body. - physical and chemical barriers (skin and epithelial linings and their secretions) - phagocytes (from white blood cells - neutrophils, eosinophils, macrophages) - immunological surveillance by natural killer cells, destroy abnormal cells - inflammation is swelling to isolate damaged tissue (fibers and connective tissue) - fever, body temperature above normal, disrupts bacterial growth Adaptive (specific) defenses (= immunity) - specific response to specific antigen Fig.14.12 - antigens are foreign substance that will trigger an immune response, usually protein molecules that have definite shape - antibodies are proteins produced by lymphocytes that specifically match the shape of an antigen; when they combine they form antigen-antibody complex - innate immunity is based on genetically determined antibodies without exposure to an antigen - acquired immunity is based on exposure to a specific antigen before antibodies can be produced - immunity has several properties due to complimentary shapes binding - specificity (one specific antibody to one specific antigen) - versatility (a very large number of antibodies can be produced - 1 b +) - tolerance (proteins in the body, “self”, are ignored) - memory (memory B and T cells can quickly produce antibodies of previously encountered antigens) T cells (from thymus) attack cells with antigens displayed - cellular immunity Fig 14.13 - macrophages engulf bacteria, or cell with viral infection; attach bacterial or viral proteins to special receptors (major histocompatibility complex proteins)on cell surface; present antigen to T cell - T cells are activated (learn to make specific shape receptor), and develop into - cytotoxic “killer” T cells that attack cells with target antigen - memory T cells that are inactive until later exposure - helper T cells that present antigen to B cells and trigger nonspecific defenses B cells (from bone marrow) produce antibodies that are released into body fluids - humoral (antibody-mediated) immunity Fig14.14 - activated by helper T cells, produce two type B cells - plasma cells divide repeatedly and produce large quantity of antibodies - memory B cells that are inactive until later exposure - antibodies destroy antigen in variety of ways - neutralization, agglutination, triggering inflammation, chemotaxis for macrophages, compliment protein binding which ruptures cell membranes Allergies, tissue rejection and autoimmunity are miss-directed immune responses. *What is the primary function of memory T cells? *What is the role of macrophages (involved in nonspecific phagocytosis) in immunity? Biology 2402 A&P II - Respiratory System Ch 16 Respiration - exchange of gasses between atmosphere and body cells - occurs in stages: - pulmonary ventilation - movement of air into and out of lungs (breathing -inspiration or inhalation and expiration or exhalation) - gas exchange at respiratory membrane (lungs to blood) - transport of gasses by blood - gas exchange between blood and cells - cellular respiration - use of oxygen in energy production, carbon dioxide produced Structure of respiratory system - tube (respiratory tract), with specialized regions (conducting portion), that brings air to respiratory exchange surface (a very delicate layer of cells, respiratory portion); and warms, cleans and humidifies air so that the exchange surface is not damaged. nasal cavity - cavity behind nostrils Fig 16.1-.2 - divided by nasal septum into right and left chambers - connected to four pair of paranasal sinuses which are located in bones bordering the nasal cavity (frontal, ethmoid, sphenoid and maxillary). These sinuses secrete mucus that flows into the nasal cavity adding extra moisture. - three pairs of nasal conchae, also called scroll bones, project into nasal cavity. (these bones form a baffle that increases surfaces area and causes air turbulence) - coarse hairs around nostrils filter larger particles - tears from eyes drain into nasal cavity, adding extra moisture - nasal cavity lined with pseudostratified columnar epithelium. This is an epithelial tissue that produces mucus and sweeps the mucus across the surface by cilia. Mucus is very sticky and traps small particles, swept into pharynx. Fig.16.3 - numerous well developed capillary beds are beneath epithelium, brings warm blood close to the surface to warm the air. - the nasal cavity also serves as a resonating chamber in sound production (speech) and the location of the olfactory epithelial for the sense of smell. *What is the primary function of the nasal cavity? Describe 5 ways that it does this. *What is the primary function of the nasal conchae - how do they work? pharynx - tube that is part of respiratory and digestive tracts, three sections: Fig. 16.2 - nasopharynx - from nasal cavity to posterior edge of soft palate and uvula - lined with pseudostratified columnar epithelium - openings of auditory tube to middle ear and pharyngeal tonsil - normally does not contain food - oropharynx - soft palate to base and tongue, part of digestive tract - lined with stratified squamous epithelium for abrasion resistance - laryngopharynx - base of tongue to larynx, part of digestive tract - lined with stratified squamous epithelium *Incoming air is cleaned in the nasal cavity then enters the pharynx where it mixes with dirty air from the mouth. What is the value of having this? larynx - movable box that forms a protective cap for the trachea, composed of cartilage plates, ligaments and skeletal muscle. Fig. 16.4 - .5 - glottis is opening into trachea, formed by false vocal cords that close glottis and true vocal cords that vibrate to produce sounds. - epiglottis is elastic and cartilage plate that covers glottis to prevent food entering - lined with stratified squamous epithelium above vocal cords and pseudostratified columnar epithelium below cords. - muscles change shape of larynx - to close glottis to protect trachea, - to form “pneumatic skeleton” to stiffen body and - to change tension of true vocal cords to produce different sounds. trachea - flexible tube from larynx to primary bronchi in thoracic cavity Fig. 16.7 - cartilage rings (about 20) support trachea, prevent collapse - smooth muscle in walls allow change in diameter, waves of contractions in cough and sneeze reflex - lined with pseudostratified columnar epithelium (mucus swept into pharynx) bronchi and bronchioles - the “bronchial tree”, from trachea to the respiratory membrane - right and left primary bronchi into right and left lung, respectively - branch into secondary, tertiary and smaller bronchi - bronchi lined with pseudostratified columnar epithelium and have cartilage rings - branch into smaller bronchioles, which lack cartilage rings and mucus cells - smooth muscle in bronchial walls allow constriction or dilation to regulate flow of air into different sections of lung - terminal and respiratory bronchioles end in alveolar duct and alveoli alveoli - thin walled air sacs that form respiratory membrane Fig. 16.7 - .10 - 150 million alveoli per lung, total of 140 m2 surface area (both lungs) - lined (actually formed of) simple squamous epithelium to make thin layer - each alveolus surrounded by capillary bed - alveoli contain macrophages to engulf and remove foreign material - walls contain surfactant cells that secrete surfactant (more on this later) respiratory membrane - separates air and blood, gas exchange surface - composed of simple squamous epithelium of alveoli and endothelial cell of capillary (two layers of thin cells) and “glue” that hold them together ( 0.1 um) *Follow a molecule of air from the outside to the respiratory membrane. List in order all of the structures that the air would pass through, or past. *List the different types of epithelial tissue lining the respiratory tract. For each type epithelium tell where it is located and the job that it does. *How do bronchi differ from bronchioles? *Describe how pseudostratified columnar epithelium works as a cleaning surface. *Why is it better to have 150 million very tiny alveoli per lung that 150 very large alveoli per lung. (Larger alveoli would contain more air) *What mechanism allows air to be directed to different areas of the lung? Lungs - left and right, within left and right pleural cavities (l. and r. pleural cavities, mediastinum, pericardial cavity are all part of thoracic cavity) - thoracic cavity is formed by rib cage on top and sides and the diaphragm on the bottom (diaphragm separates the thoracic and abdominal cavities) - pleural cavities lined by parietal pleura and lungs covered by visceral pleura; the pleura are serous membranes that produce a slick fluid, pleural fluid. - “potential space” between parietal and visceral pleura, usually in close contact * How can the lungs move within the pleural cavities during pulmonary ventilation and not be damaged by friction? *What does the term “potential space” mean? Respiratory physiology Fig. 16.12 -.14 pulmonary ventilation - breathing mechanism - movement of air into and out of the lungs - air, like other fluids, moves from high to low pressure - air pressure inside the lungs compared to atmospheric pressure causes movement - normally the lungs fill the pleural cavities, pleura adhered; therefore the volume of the pleural cavities is the volume of the lungs - inspiration involves two muscles, or muscle groups: - the diaphragm accounts for about 75% of change in size of thorax. when relaxed it domes up due to pressure from abdominal organs. when it contracts it flattens, lowering the floor of the thorax thus increasing the volume of the thoracic cavity. - the external intercostal muscles elevate the anterior ends of the ribs and sternum. This increases the volume of the thoracic cavity. - this causes slightly lower pressure in alveoli - surface tension of water between parietal and visceral pleura adhere two surfaces so expanding thorax pulls lungs open. . - quiet expiration is caused by elastic recoil. Elastic fibers of the lungs, ligaments and muscles of the chest return to their position before stretching and compressed abdominal organs expand pushing diaphragm up - causes slightly higher pressure in alveoli - forced expiration involves two muscle groups: - abdominal muscles contract, pushing abdominal organs up against the diaphragm (the diaphragm is relaxed) which domes the diaphragm upward. This decreases the volume of the thoracic cavity. - the internal intercostal muscles pull the anterior end of the ribs and the sternum downward. This decreases the volume of the thoracic cavity. *Explain what we mean when we say that inspiration and forced expiration are active, but quiet expiration is passive. *List the muscles involved in inspiration and tell what they do to cause inspiration. *List the muscles involved in forced expiration and tell what they do to cause this. *What is a pneumothorax and how does it disrupt pulmonary ventilation? *How does pleural fluid aid in pulmonary ventilation? Compliance is the “stretchability” of the lungs. Several factors can alter compliance, such as loss of elastic fibers in lungs, scar tissue and surface tension of water. - surfactant is wetting agent in alveoli that reduces surface tension of water - reduces force required to stretch water layer in alveoli - prevents alveoli from collapsing and having their sides stick - prevents larger alveoli from expanding and collapsing smaller ones *Respiratory distress syndrome is a common problem in babies born prematurely because their surfactant cells have not yet become active. Explain the problem. Respiratory air volumes: respiratory cycles Fig 16.15 - total lung capacity about 6000 ml for males, 4200 ml for females - tidal volume is normal volume of air exchanged during quiet breathing (500 ml) - expiratory reserve volume is air that can be forced out after a normal quiet exhalation (about 1000 ml) - inspiratory reserve volume is air that can be inhaled after a normal quiet inhalation ( about 3000 ml ) - vital capacity is the total volume of air that can be exchanged during a respiratory cycle; equals tidal volume, inspiratory and expiratory reserves. - residual volume is the air that cannot normally be forced from the lungs, fills anatomic dead space (about 1200 ml) *Draw a graph clearly showing the volumes of air involved in the respiratory cycle (or rip page 455 out of your text and glue it to your study sheets). *Describe the mechanism (muscles, bones, etc,) that causes the movement of air called the tidal volume. Do the same for the expiratory reserve volume. *The anatomical dead space is filled with air that cannot reach the alveoli and cannot be forced out - fresh air and stale air are always mixing. Why do we have the anatomic dead space? Diffusion across the respiratory membrane: Fig. 16.19-.20 - partial pressure is a measure of gas concentration, describes gasses in a mixture - a gas in a mixture, like air, behaves independently of other gasses - oxygen is about 21% of air; at an atmospheric pressure of 760 mmHg of air oxygen would have a partial pressure of 160 mmHg (760 x .21 = 160) Po2 = 160 mm Hg Pco2 = 0.3 mmHg (760 x 0.04) - passive diffusion of gasses occurs from high partial pressure to low p.p. - in the alveoli Po2 = 104 mmHg and Pco2 = 40 mmHg; in the arteriole end of the pulmonary capillaries Po2 = 40 mmHg and Pco2 = 45 mmHg. Therefore O2 diffuses from the alveoli to the blood and CO2 diffuses from the blood to the alveoli. - external respiration is the movement of gasses across the respiratory membrane - three factors determine the volume of gasses that diffuse across the membrane: - the total surface area (condition of resp. membrane, scar tissue, mucus) - the distance across the resp. mem. (very thin, 0.5um - pulmonary edema) - the difference of gas concentration across the resp. mem. (breathing rate to replace air in alveoli, rate of blood flow in pulmonary capillaries, pressure of atmospheric air and % gas in inhaled air). *Why can the Po2 in the alveoli never be as high as the Po2 of air outside the body? *Describe the three factors that determine how much oxygen will enter the blood across the respiratory membrane. *Explain how we change these factors to regulate the oxygen level in the blood short term *Explain how breathing coal dust or cigarette smoke decreases the ability to absorb O2. *Define the terms anoxia, hypoxia, hypercapnia and hypocapnia. *Describe the respiratory membrane (cells involved, structure, etc.). Transport of gasses in the blood Fig. 16.20 - .23 - 2% of oxygen dissolved in blood plasma, 98% bound to hemoglobin in rbc O2 in tissues or alveoli <----> plasma <----> hemoglobin - hemoglobin-oxygen dissociation curve shows how much of the hemoglobin will be carrying oxygen (% saturation) under different levels of available oxygen - high levels of H+ (low pH) will shift dissociation curve (Bohr effect) *Describe the hemoglobin-oxygen dissociation curve and explain why hemoglobin is a very good carrier molecule. *Describe how the Bohr effect is important in maintaining homeostasis. *The affinity (ability to bind with) of hemoglobin for carbon monoxide is about 200 times greater than its affinity for oxygen. Why is this a problem? - 7% of CO2 dissolved in plasma, 23% bound to hemoglobin, 70% in HCO3-- the bicarbonate buffering system allows the blood to absorb a large quantity of carbon dioxide, in rbc CO2 + H2O <----> H2CO3 <----> H+ + HCO3-HbH NaHCO3 *How does an increase in carbon dioxide affect the pH of the blood? *How does the bicarbonate buffering system allow the blood to carry more carbon dioxide without changing pH very much? In the systemic capillaries oxygen diffuses from the blood to the intercellular fluid and carbon dioxide diffuses into the blood - blood Po2 = 104 mmHg and Pco2 = 40 mmHg (at arteriole end of capillaries) - intercellular fluid Po2 = 40 mm hg and Pco2 = 45 mm Control of breathing - cells use oxygen and produce carbon dioxide in cellular respiration to produce energy. This increases with activity level and supply must meet demand to maintain __________. Fig. 16.16 - .18 The nervous system feedback involves: Receptors ------------- control centers ------------- effectors receptors: two types of receptors: - chemoreceptors in carotid bodies, aortic body sense the levels of CO2, pH and O2 in the blood. Normally CO2 is more sensitive. - baroreceptors in the carotid and aortic bodies sense blood pressure, effect cardiovascular system and respiratory cycle. - baroreceptors (stretch receptors) in the bronchiole and alveoli sense air pressure in the lungs, stimulate the inflation reflex. control centers in the medulla oblongata of the brain - the respiratory rhythmicity center is divided into two control centers: - the inspiratory center (dorsal respiratory group) stimulates the muscles of inhalation, and is involved in each respiratory cycle - stimulated for 2 seconds, inhibited 3 seconds; this sets normal 12 breaths per minute pattern. - can be slowed or increased by several mechanisms. - the expiratory center (ventral respiratory group) is only active during forced breathing, stimulates the muscles of forced breathing - pneumotaxic area stimulates inspiratory center to regulate the breathing rate. - higher centers in the brain can alter the respiratory cycle (nonrespiratory movements) - cerebral cortex (voluntary movements like in speaking, laughing, crying, coughing, whistling, humming, blowing up balloons, etc.) - limbic system (emotional changes), hypothalamus (maintaining homeostasis like temperature adjustments) effectors are the muscles of inspiration and expiration *Describe the inflation reflex and tell why it is important. What receptors are involved? *Why is there not a center that stimulates exhalation in quiet breathing? *Describe the mechanism that controls and regulates pulmonary ventilation. Include all of the control centers, receptors and muscles involved. *If carbon dioxide is filtered from the air a person is breathing they will almost faint before they start breathing. Explain why this happens.