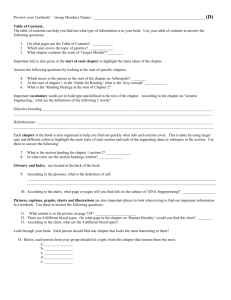
DHS
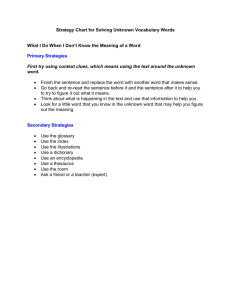
advertisement

***This version of the Health Care Programs Manual has been replaced and is no longer in effect. This includes all PDF versions below. Please see the current Health Care Programs Manual for policy in effect as of December 1, 2006.*** The terminology used to describe people with disabilities has changed over time. The Minnesota Department of Human Services ("Department") supports the use of "People First" language. Although outmoded and offensive terms might be found within documents on the Department's website, the Department does not endorse these terms. MDHS Health Care Programs Manual (Eligibility Policy through 11/30/06) Chapter 0902 - Glossary 0902.01 0902.03 0902.05 0902.07 0902.09 0902.11 0902.13 0902.15 0902.17 0902.19 0902.21 0902.23 0902.25 0902.27 0902.29 0902.31 0902.33 0902.35 0902.37 0902.39 0902.39.01 0902.41 GLOSSARY: 10-DAY GLOSSARY: ASSIGNMENT GLOSSARY: CAPITAL... GLOSSARY: CLIENT... GLOSSARY: DENIAL... GLOSSARY: EFFECTIVE... GLOSSARY: FAMILY... GLOSSARY: FPG... GLOSSARY: HEALTH CARE... GLOSSARY: IN-KIND... GLOSSARY: INSURANCE... GLOSSARY: MANAGED CARE... GLOSSARY: MFIP... GLOSSARY: NON-CITIZEN... GLOSSARY: PENSION... GLOSSARY: PROCEDURAL... GLOSSARY: QUALITY... GLOSSARY: RENEWAL... GLOSSARY: SOLE... GLOSSARY: TENNESSEN... GLOSSARY: TRUST DEFINITIONS... GLOSSARY: UNDERINSURED... PDF(s): Feb 1999 PDF(s) Feb 99 PDF(s): May 01 PDF(s): Jan 06 | Oct 03 | Oct 02 | Aug 00 PDF(s): May 05 |Oct 03 | Apr 00 PDF(s): Jan 05 | Oct 03 | Oct 02 | Apr 00 PDF(s): Mar 03 | Dec 99 PDF(s): Oct 02 | Feb 99 PDF(s): May 05 | Oct 00 PDF(s): Feb 01 PDF(s): Jan 02 PDF(s): Oct 02 | Jul 01 PDF(s): Oct 02 | Apr 00 PDF(s): May 05 | Apr 05 | Mar 03 | Jul 99 PDF(s): Jul 02 | Jan 02 PDF(s): Feb 99 PDF(s): Mar 03 | May 01 PDF(s): Apr 02 PDF(s): Oct 02 | Aug 99 PDF(s): Aug 04 | May 01 PDF(s): Feb 99 PDF(s): May 05 | May 01 GLOSSARY: 10-DAY... 0902.01 10-DAY NOTICE: Notices mailed or given to clients at least 10 days before the date of action. 1619a AND 1619b: Provisions of the Social Security Act which allow certain employed people who would otherwise be ineligible to retain SSI status. The SOCIAL SECURITY ADMINISTRATION certifies people for 1619a and 1619b eligibility. People with1619a or b status retain their MA eligibility under the SSI related category if they received MA the month before certification for 1619a or 1619b. See §0907.13.05.07 (MA Basis: 1619A and B). 1619a SOCIAL SECURITY ACT: A provision allowing continued SSI and MEDICAL ASSISTANCE eligibility for people who would otherwise lose SSI because of a demonstrated ability to work. 1619b SOCIAL SECURITY ACT: A provision allowing continued MEDICAL ASSISTANCE eligibility for people who become ineligible for SSI benefits under 1619a due to excess income. 18-MONTH RULE: MINNESOTACARE: One of the INSURANCE BARRIERS. The 18-month rule requires that some people not have current coverage or access to employer subsidized insurance. It also restricts eligibility for some people who have had access to ESI in the past 18 months if the employer chose to drop coverage. See §0910.11.03 (18-Month Rule). 4-MONTH RULE: MINNESOTACARE: One of the INSURANCE BARRIERS. The 4-month rule requires some people to have been uninsured for 4 months before they can enroll in MinnesotaCare. See §0910.07 (4-Month Rule). ACKNOWLEDGMENT OF PATERNITY: A legal DECLARATION OF PARENTAGE (DOP) or RECOGNITION OF PARENTAGE (ROP) signed by both the mother and father of a CHILD born to a woman who was not married to the child's father when the child was conceived nor when the child was born, declaring that they are the biological PARENTS of the child. The DOP may be signed before or after the child's birth and is valid only if it was executed before 8-1-95. For documents executed on or after 8-1-95, only the ROP is valid. The ROP cannot be signed until AFTER the child's birth. The ROP (DHS 3159) form is available from DHS Forms Supply. See RECOGNITION OF PARENTAGE (ROP) in §0902.33 (Glossary: Quality...). ADDENDUM: MA and GAMC: The Combined Application - Addendum form (DHS 2853a) used to add people to an existing household. ADEQUATE COMPENSATION: FAIR MARKET VALUE, or other compensation equal to the fair market value, received in exchange for the TRANSFER or sale of REAL or PERSONAL PROPERTY. ADEQUATE NOTICE: A notice sent no later than the date of action. ADJUDICATION OF PATERNITY: Determination of the identity of a CHILD's father by a court. ADOPTION ASSISTANCE: An adoption assistance grant from state or IV-E funds to adoptive PARENTS under Minnesota Statutes, section 259.67. AGED: MA: Age 65 or older. Used interchangeably with ELDERLY. AID TO FAMILIES WITH DEPENDENT CHILDREN (AFDC): The program formerly authorized under Title IV-A of the Social Security Act to provide financial assistance and social services to needy families with dependent children. AFDC was replaced by the Temporary Assistance to Needy Families (TANF) block grant in 1996. Minnesota’s TANF program is MFIP. See MINNESOTA FAMILY INVESTMENT PLAN (MFIP) in §0902.25 (Glossary: MFIP...). ALIMONY: An allowance for support that a court orders a person to pay to his or her current or former SPOUSE. ALLOCATION: MA: A DEDUCTION from the income of a LONG TERM CARE FACILITY RESIDENT or a person receiving ELDERLY WAIVER services for the maintenance needs of certain relatives. See §0912.05.25 (Allocations). ALTERNATIVE CARE (AC): Payments made by Social Services for home care services for a person age 65 and over who would otherwise require care in a nursing facility. To qualify for AC services, the cost of community care must be less than care in a nursing facility and the person must appear to be MA-eligible within 180 days of beginning to receive AC services based on income and ASSETS. APPEAL: A CLIENT's or AUTHORIZED REPRESENTATIVE's request to the State of Minnesota appeals section for review of the state or a county agency’s action or inaction. See §0917 (Appeals). Appeals may also be related to the delivery of health services under MANAGED CARE programs or to denial of specific health services. APPLICANT: A person who has submitted a request for coverage for whom no decision has been made regarding eligibility. APPLICATION: A request for coverage under the HEALTH CARE PROGRAMS. MINNESOTACARE: An application is a signed and dated Health Care Application (HCAPP, DHS 3239). MA/GAMC: For purposes of setting the application date, an application is a signed and dated Part I of the Combined Application Form (CAF); a signed and dated page 1 of the Health Care Application (HCAPP); or any other signed and dated request containing the applicant’s name and address. The applicant must submit a completed CAF Part II or HCAPP to complete the application process. See §0904 (Applications). ASSET LIMIT: The amount of net countable ASSETS clients may own or have available and remain eligible for MA or GAMC. Not all CLIENTS have an asset limit. See §0909.05 (Asset Limits). ASSETS: REAL PROPERTY and PERSONAL PROPERTY owned wholly or in part by the CLIENT. Return to top GLOSSARY: ASSIGNMENT... 0902.03 ASSIGNMENT: To transfer legal claim, such as assignment of benefits available through other health coverage or MEDICAL SUPPORT. AUTHORIZED REPRESENTATIVE: A person authorized by the APPLICANT or ENROLLEE to act on his or her behalf as an applicant or enrollee in any of the HEALTH CARE PROGRAMS. An authorized representative may exercise all the rights and responsibilities of a CLIENT. See §0904.11 (Authorized Representatives). The SOCIAL SECURITY ADMINISTRATION may designate authorized representatives to assist people in applying for and managing their RSDI or SSI benefits. MA may allow a DEDUCTION for costs of serving as an authorized representative under the guardianship provisions. See §0913.13 (Long Term Care Spenddown Calculation). AVAILABILITY: CLIENTS’ ability to gain access to income or to use, sell, or liquidate ASSETS they own. See §0909.09 (Availability of Assets) and §0911.03 (Availability of Income). BASIS OF ELIGIBILITY: MA: An identifying characteristic of a category of people specified as potentially eligible for MA. People without one of the specified characteristics are ineligible for MA but may be eligible for GAMC or MINNESOTACARE. BATTERED NON-CITIZEN: A NON-CITIZEN who is the SPOUSE or CHILD of a U.S. citizen or LAWFUL PERMANENT RESIDENT (LPR) and who has been battered or subject to extreme cruelty in the U.S. by a family member residing in the same household. A battered non-citizen may petition for adjustment of status to LPR on his or her own behalf. A person with an approved or pending petition on that basis would be considered a QUALIFIED NON-CITIZEN, but only if the U.S. Attorney General determines that there is a substantial connection between such battery or cruelty and the need for benefits to be provided. The battered noncitizen must no longer reside in the same household with the person who committed the battery. BEER: MA: Beneficiary Earnings and Exchange Record. A monthly IEVS tape exchange between the SOCIAL SECURITY ADMINISTRATION and DHS reporting wages, SELF-EMPLOYMENT, and federal PENSION earnings from federal tax returns. The original source is the Internal Revenue Service. BENEFICIARY: The person named to receive benefits or payments (for example, SOCIAL SECURITY payments or payments from a life insurance policy or TRUST). BENEFIT RECOVERY SECTION (BRS): A section of DHS which pursues collection of 3rd party payments and determines if health insurance is cost effective. BLIND: MA: An SSI definition used to determine the MA blindness BASIS OF ELIGIBILITY. The condition of a person without vision. Or, a person with vision of 20/200 or less in the better eye using a standard Snellen chart. If the vision in one eye is better than 20/200 but the person's visual field is 20 degrees or less, consider the person blind. Blind also includes people with aphakic eye with vision of 20/70 or worse in the better eye. BNDX: MA: BENEFICIARY Data Exchange. A monthly IEVS tape exchange between the SOCIAL SECURITY ADMINISTRATION and DHS. The report provides information on Title II benefits (RSDI) and MEDICARE Parts A and B. BURIAL AGREEMENT: An arrangement in which funds are deposited with a funeral director to be used for funeral expenses. The agreement may cover funeral and professional services, BURIAL SPACE ITEMS, or both. The money is usually held in trust by a bank or other financial institution unless the agreement is funded by an insurance policy or annuity. Burial agreements may be revocable or irrevocable. BURIAL FUNDS: Funds paid or designated in advance for funeral expenses, including but not limited to BURIAL AGREEMENTS. Burial funds provide for preparation of the body, cremation, or burial services. BURIAL SPACE: Any repository for the remains of the deceased such as cemetery plots, urns, niches, crypts, and caskets. BURIAL SPACE ITEMS: Items which add to or improve BURIAL SPACES such as markers, engraving, vaults, opening and closing of the grave, and 1-time charges for preservation/care of the space (perpetual care). C-CORPORATION: A corporation in which shareholders receive profits in the form of DIVIDENDS. Shareholders who perform work for the corporation also receive wages. The corporation must file a corporate tax return. CAF: See COMBINED APPLICATION FORM (CAF) in §0902.07 (Glossary: Client...). CANCELLATION: MINNESOTACARE: Termination of MINNESOTACARE coverage for 1 or more members of a HOUSEHOLD. Return to top GLOSSARY: CAPITAL... 0902.05 CAPITAL ASSET: REAL or PERSONAL PROPERTY used in a trade or business with a useful life of 1 year or more. CAPITAL GAIN: Profit from the sale of a CAPITAL ASSET. CAPITATION: A method of payment for health services. DHS pays a monthly per-person rate in advance to a HEALTH PLAN in return for comprehensive medical and dental services. CAPITATION DATE: The monthly date on which DHS sends CAPITATION payments to HEALTH PLANS. CARETAKER: A person who provides care and support to a MINOR CHILD. The person may or may not be covered and may or may not be considered part of the child’s household. See RELATIVE CARETAKER in §0902.33 (Glossary: Quality...) and §0908 (Household Composition). CASE MANAGEMENT: For MANAGED CARE: A method of providing health care in which the HEALTH PLAN coordinates the provision of health services to a MANAGED CARE ENROLLEE. See §0914 (Service Delivery). MA: Services not normally covered by MA that may be covered under a waiver for people with severe and persistent mental illness. CASE MANAGEMENT SERVICE COVERAGE: MA: For severely and persistently mentally ill people. GAMC: For people with serious and persistent mental illness who would be eligible for MA except that they reside in an INSTITUTION FOR MENTAL DISEASES (IMD). CASH PROGRAMS: GENERAL ASSISTANCE (GA), MINNESOTA FAMILY INVESTMENT PLAN (MFIP), MINNESOTA SUPPLEMENTAL AID (MSA), REFUGEE CASH ASSISTANCE (RCA), and emergency cash programs. CERTIFICATION PERIOD: MA and GAMC: The time period for which income is considered and the SPENDDOWN, if any, is determined. For people requesting RETROACTIVE ELIGIBILITY, the initial certification period may include months in which there is no eligibility but for which income and bills were considered. MA and GAMC certification periods are set up for 6 months at a time but may be ended sooner in some circumstances. See §0913.19 (Shortened Spenddown). CHAMPUS: The Civilian Health and Medical Program of Uniformed Service. CHAMPUS provides health coverage to current civilian employees of the armed services, dependents of active duty service people, and retired civilian and active duty employees of the armed services. The cost of CHAMPUS coverage is paid by the U.S. government, but there is usually an annual DEDUCTIBLE and CO-PAYMENTS for some services. CHAMPUS is also known as TRICARE. CHAMPVA: The Department of Veterans’ Affairs’ Civilian Health and Medical Program. The Veterans’ Administration shares the cost of covered health services and supplies with eligible BENEFICIARIES. CHILD: A person under age 21. CHILD & TEEN CHECKUPS: A component of MA and MinnesotaCare that promotes preventive health care for children from birth to age 21. Formerly named the Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) Program. CHILD SUPPORT: A voluntary or court-ordered payment by NON-CUSTODIAL PARENTS for the support of their children. CHILDREN'S HEALTH PLAN: The forerunner of the MINNESOTACARE program. CHILDREN'S HOME CARE OPTION (CHCO): See definition of TEFRA §0902.37 (Glossary: Sole...). CIVIL RECOVERY: Recovery of an OVERPAYMENT through the civil judicial process rather than the criminal process. Return to top GLOSSARY: CLIENT... 0902.07 CLIENT: A person who is an APPLICANT or ENROLLEE. CLOTHING AND PERSONAL NEEDS ALLOWANCE: MA: The amount of monthly income institutionalized clients may retain or receive for their day to day expenses. CO-INSURANCE: An insured person’s share of the cost of treatment. For example, if an insurance policy covers 80% of the cost, the co-insurance amount is 20%. CO-PAYMENT: A fixed amount that an insured person is required to pay for each episode of a particular treatment, medical supply, or equipment. For example, a policy might require a $5 co-payment for each prescription while the insurance pays the remainder. COBRA COVERAGE: A provision of the Consolidated Omnibus Budget Reconciliation Act (COBRA) which requires employers to allow former employees to continue coverage through the employer’s group plan for 18 months after the employment has ended (29 months if the employee is disabled). In most cases, the former employee must pay the full cost of COBRA coverage. COLA: Cost of Living Adjustment. An increase in income to compensate for inflation. COLAs are usually made annually. COMBINED APPLICATION FORM (CAF): A form on which people can apply for multiple programs administered by DHS, including GENERAL ASSISTANCE (GA), GENERAL ASSISTANCE MEDICAL CARE (GAMC), FOOD SUPPORT, MINNESOTA FAMILY INVESTMENT PLAN (MFIP), MEDICAL ASSISTANCE (MA), MINNESOTA SUPPLEMENTAL AID (MSA), Emergency Assistance (EA), EMERGENCY MEDICAL ASSISTANCE (EMA), and EMERGENCY GENERAL ASSISTANCE MEDICAL CARE (EGAMC). COMMUNITY ALTERNATIVE CARE (CAC): A federally approved home and community based services WAIVER program for chronically ill people under age 65. See §0907.23.07 (Community Alternative Care (CAC). COMMUNITY SPOUSE: A person who does NOT reside in a medical institution, LTCF, or receive EW services whose spouse DOES reside in a medical institution, LTCF, or receives EW services and meets the definition of a LONG TERM CARE SPOUSE. A community spouse may or may not receive MA. COMPREHENSIVE COVERAGE: MINNESOTACARE: A term used by insurance companies to describe a broad range of covered services including the diagnosis and treatment of most illnesses and injuries. Coverage may vary under individual policies. CONSERVATOR: A person, official, or institution designated to protect the interests of an incompetent person. A conservator has some, but not all, of the duties and powers of a legal guardian and is not counted in the person’s household for any of the HEALTH CARE PROGRAMS. CONTINUED ABSENCE: MA: A BASIS OF ELIGIBILITY for PARENTS and RELATIVE CARETAKERS of a DEPENDENT CHILD. See §0907.19.07 (MA Families and Children Basis: AFDC-Related Adults). CONTINUOUS ENROLLMENT: MINNESOTACARE: Enrollment in MINNESOTACARE, MA, or GAMC with a break in coverage of less than 1 calendar month. CONTINUOUS PERIOD OF INSTITUTIONALIZATION: MA: A stay in a medical or LONG TERM CARE FACILITY which is expected to last at least 30 consecutive days from the date of entry. Count the date of entry and the date of discharge to determine whether a stay has lasted at least 30 consecutive days. A new continuous period of institutionalization begins after a client re-enters an institution after having been discharged for at least 30 consecutive days. CONTRACT FOR DEED: A conditional sales contract for purchase of real estate. The contract is held by a private party as opposed to a lending institution. Consider contracts for deed to be PERSONAL PROPERTY. See §0909.13.05 (Contracts for Deed). COUNTY AGENCY: The local human services office responsible for determining eligibility for MA and GAMC. Some county agencies also determine eligibility for MinnesotaCare. COUNTY OF FINANCIAL RESPONSIBILITY: The county responsible for the county costs of an ENROLLEE’s MA or GAMC. CUSTODIAL PARENT: A PARENT who has physical custody of his or her CHILD. CUTOFF DATE: The date by which information must be entered in MAXIS or MMIS to effect a change for the following month. DECLARATION OF PARENTAGE (DOP): A form printed by the Minnesota Department of Health, Vital Records Section, that serves as an ACKNOWLEDGMENT OF PATERNITY. This form may be signed before or after the child's birth. However, to be valid, it must be executed before 8-1-95. Effective 8-1-95, clients must use the RECOGNITION OF PARENTAGE (DHS 3159). Notarized signatures of both parents must be on the form. DEDUCTIBLE: The amount of health care expenses an insured person is required to incur before benefits are payable under a health insurance policy. For example, if an insured person has a $1,000 deductible, he or she must incur $1,000 in medical costs before the policy begins paying benefits. DEDUCTION: MA and GAMC: An amount of income not counted in the computation of a person's income because its use or intended use is for certain specific expenses. For example, employed people are allowed a deduction for DEPENDENT CARE. DEED: Legal document which conveys ownership of property between parties. DEEM: To count the income or ASSETS of 1 person when determining the eligibility of another. See §0908.07 (Household Composition: Deeming). DEEMED SSI RECIPIENT: MA: An individual who for Medicaid purposes is considered to be receiving SSI. This includes people eligible under 1619(a) and (b); children eligible under the TEFRA waiver; people eligible for the Pickle disregard; Disabled Adult Children; Disabled Widows and Widowers; and people not receiving SSI payment because of recoupment or 1-month suspension due to excess income. See the following sections: §0907.21.07.03 (MA Basis: 1619 A and B) §0907.23.09 (MA Waiver Programs: TEFRA) §0911.09.15.01 (Income from RSDI and SSI--MA/GAMC) §0912.05.17 (Widow and Widower’s Disregard) §0912.05.19 (Disabled Adult Children Disregard) §0912.05.21 (Disabled Widow/Widower’s Deduction) §0912.05.23 (Pickle Disregard) DELAYED VERIFICATION: A process for granting eligibility to applicants before verifying all mandatory eligibility factors. This process was formerly known as presumed eligibility for MinnesotaCare. See §0904.07.05 (Application Follow Up) for procedures for delayed verification for MinnesotaCare. See §0904.13.05 (Delayed Verification) for procedures for MA and GAMC. Return to top GLOSSARY: DENIAL... 0902.09 DENIAL: The act of disapproving an APPLICATION, a request to add a person to coverage, or a request for specific medical services. DEPENDENT CARE DEDUCTION: An income DEDUCTION based on the cost of caring for a CHILD or adult. See §0912.05.07 (Dependent Care Deduction). DEPENDENT CHILD: MINNESOTACARE: A person less than 21 years old who lives with a PARENT, LEGAL GUARDIAN, RELATIVE CARETAKER, or foster parent. MA: A person who lives with a parent, legal guardian, relative caretaker or foster parent and is less than 18 years old, or an 18-year-old FULL-TIME STUDENT expected to graduate by age 19. DEPENDENT HEALTH INSURANCE: Health insurance coverage offered or provided to the insured’s specified dependents. EMPLOYER SUBSIDIZED INSURANCE may be available only to the employee or to the employee and dependents. DHS: The Minnesota Department of Human Services. DISABILITY: MA: A BASIS OF ELIGIBILITY based on the disability standards of the SOCIAL SECURITY ADMINISTRATION (SSA). Disability may be determined by the SSA or the STATE MEDICAL REVIEW TEAM (SMRT). See §0906.15 (Disability Determinations). DISABILITY INSURANCE: A policy which pays a fixed amount of income to a person who becomes disabled under the terms of the policy. DISABILITY insurance is intended as an income replacement and is not health insurance. DISREGARD: An amount of income which is excluded in determining NET INCOME. DIVIDEND: The amount of the profit distribution a shareholder receives or the amount of the surplus distribution a policyholder of a participating insurance policy receives. DOMESTIC VOLUNTEER SERVICE ACT: Federal law authorizing the Foster Grandparents Program, Retired Senior Volunteer Program, Service Corps of Retired Executives, Active Corps of Executives, Action Cooperative Volunteer Program, Senior Companion Program, VISTA, and University Year for Action. EARNED INCOME: Money received from employment or SELF-EMPLOYMENT. This includes but is not limited to salaries, wages, tips, commissions, vacation, and sick pay. See §0911.07 (Determining if Income Is Earned or Unearned) and §0911.07.03 (Earned Income). EARNED INCOME CREDIT (EIC): A federal tax credit given to low income people. Household members may receive an EIC once a year as a refund or as an advance payment or tax reduction with each paycheck. EARNED INCOME DISREGARD: MA: An amount deducted from earned income as an employment incentive. See §0912.05.09 (Earned Income Disregards--Method A) and §0912.05.09.05 (Earned Income Disregards--Method B). EARNED INCOME DISREGARD CYCLE: MA: The time period in which you apply the EARNED INCOME DISREGARD for Method A. See §0912.05.09.03 (Earned Income Disregard Cycle--Method A). Return to top GLOSSARY: EFFECTIVE... 0902.11 EFFECTIVE DATE: The date a specific action such as an approval, DENIAL, TERMINATION, or other change in eligibility or coverage begins. EIGHTEEN-MONTH RULE: MINNESOTACARE: One of the INSURANCE BARRIERS. The 18-month rule requires that some people not have current coverage or access to ESI. It also restricts eligibility for some people who have had access to ESI in the past 18 months if the employer chose to drop coverage. See §0910.11.03 (18-Month Rule). ELDERLY: MA: Age 65 or older. Used interchangeably with AGED. ELDERLY WAIVER (EW): MA waivered services for a person over age 65 who would otherwise need care in a LONG TERM CARE FACILITY. See §0907.23.11 (MA Waiver Programs: EW). ELIGIBILITY BEGIN DATE: The date an ENROLLEE is eligible for coverage under 1 of the HEALTH CARE PROGRAMS. ELIGIBILITY GROUP: MINNESOTACARE: One of 3 groups to which MINNESOTACARE ENROLLEES are assigned based on certain characteristics. See §0907 (Eligibility Groups and Bases of Eligibility). ELIGIBILITY VERIFICATION SYSTEM (EVS): DHS’s system to verify ENROLLEES’ coverage and eligibility dates under the HEALTH CARE PROGRAMS. Providers contact EVS by phone to confirm eligibility. EMANCIPATED MINOR: A person under the age of 18 who is or was married, is on active duty in the uniformed services, or has been declared emancipated by a court. EMERGENCY: MA: A sudden onset of a physical or mental condition OR a chronic medical condition which, if left untreated, could reasonably be expected to place the person’s health in serious jeopardy, cause serious impairment to bodily functions, or cause serious dysfunction of any bodily organ or part. This includes prenatal care, labor, and delivery. See §0907.29.03 (Emergency Medical Assistance - EMA). EMPLOYER SUBSIDIZED INSURANCE (ESI): Insurance coverage offered to employees for which the employer pays at least 50% of the cost of coverage. See §0910.11 (Employer Subsidized Insurance). ENCUMBRANCE: A legal claim against REAL PROPERTY or PERSONAL PROPERTY payable when the property is sold. ENROLLEE: 1. A person receiving coverage through MA, GAMC, or MINNESOTACARE. 2. A person enrolled in a HEALTH PLAN. ENROLLMENT REPRESENTATIVE: Term used by MINNESOTACARE OPERATIONS at DHS and on MINNESOTACARE notices to refer to an employee who determines initial and continued eligibility for MINNESOTACARE. Also see WORKER in §0902.41 (Glossary: Underinsured...) EQUITY: The FAIR MARKET VALUE of property minus any ENCUMBRANCE. ESCROW: A DEED, bond, money, or piece of property held in TRUST by a 3rd party to be turned over to the grantee only on fulfillment of a condition. ESTATE CLAIMS: A method of recovering MEDICAL ASSISTANCE from the estate of a deceased person. ESTIMATED MARKET VALUE (EMV): The value assigned to real estate by the county assessor for the purpose of levying property taxes. EMV is found on the annual property tax assessment statement. EW: See ELDERLY WAIVER above. EXCESS ASSETS: The amount of ASSETS which exceeds the client's ASSET LIMIT. EXCLUDED INCOME: Income not used to determine eligibility or MINNESOTACARE premium amount. EXCLUDED TIME: Any time a person spends in any of the following places or situations: hospitals, sanitariums, nursing homes, shelters (other than emergency shelters), HALFWAY HOUSES, FOSTER HOMES, board and care homes, maternity homes, battered women's shelters, correctional facilities, supervised board and lodging facilities, REGIONAL TREATMENT CENTERS, facilities based on an emergency hold, placements in training and habilitation programs (including a rehabilitation facility or work or employment program), day training and habilitation programs, assisted living services, placements with an indeterminate commitment, including independent living. EXCLUDED TIME RESIDENCE/FACILITY: A type of living arrangement which affects determining financial responsibility. See §0906.07.05 (Excluded Time). EXCLUDED TIME SERVICES: 1. Participation in a rehabilitation facility which meets the definition of a long term sheltered workshop. 2. Receiving Personal Care Assistant (PCA) services. 3. Services from a SEMI-INDEPENDENT LIVING SERVICES (SILS) PROGRAM. EXPENSES COVERED BY GAMC OR MA: See the Minnesota Health Care Programs Provider Manual for detailed information on services covered by GAMC or MA. EXTENDED MEDICAL ASSISTANCE: See TRANSITIONAL MEDICAL ASSISTANCE (TMA) and TRANSITION YEAR MEDICAL ASSISTANCE (TYMA) in §0902.39 (Glossary: Tennessen...) FACE-TO-FACE INTERVIEW: A face-to-face meeting arranged to determine initial or ongoing eligibility for MA, GAMC or MINNESOTACARE. Face-to-face interviews are at the option of the CLIENT for people who are requesting only health care coverage. FAIR MARKET VALUE: The price an item would sell for on the open market in a local geographic area. See individual property sections in §0909 (Assets) for exceptions and provisions. Return to top GLOSSARY: FAMILY... 0902.13 FAMILY: MINNESOTACARE: A family with children means a biological or adoptive PARENT or parents, a STEPPARENT living with a biological or adoptive parent, or a LEGAL GUARDIAN, together with the parent’s, stepparent’s, or legal guardian’s CHILDREN or wards, and DEPENDENT SIBLINGS living in the same household. A family with children means a biological or adoptive PARENT(s) or STEPPARENT(s), together with the parent’s or stepparent’s CHILDREN or stepchildren and DEPENDENT SIBLINGS living in the same household. A family with children may also include foster parents, grandparents, or other RELATIVE CARETAKERS or a LEGAL GUARDIAN living in the same home as the children for whom they have primary responsibility. A person may not be considered a relative caretaker if the children’s biological or adoptive parent also resides in the home and has primary responsibility for the children. In households without children, family means a single individual in a 1-person household or SPOUSES living in the same household. See §0908 (Household Composition). FAMILY SUPPORT GRANT PROGRAM: A state-funded program that provides funds to help families provide home care for dependents with mental retardation or related conditions. FEDERAL BENEFIT RATE (FBR): MA: The maximum federal benefit rate for the SUPPLEMENTAL SECURITY INCOME (SSI) program. This amount is updated each January and is used to determine the PICKLE DISREGARD and the SPECIAL INCOME STANDARD (SIS) for the ELDERLY WAIVER (EW) program. See §0907.23.11 (MA Waiver Programs: EW) and §0912.05.23 (Pickle Disregard). FEDERAL FINANCIAL PARTICIPATION (FFP): Reimbursement to DHS for some of the cost of an ENROLLEE’s medical services from the federal government. People must meet certain criteria to be eligible for FFP. FEDERAL INCOME TAX FORMS: The Internal Revenue Service forms that people who are not exempt must file annually to establish their federal income tax liability. Federal tax forms usually consist of Form 1040 and various supplemental schedules depending on the taxpayer’s circumstances. FEDERAL POVERTY GUIDELINES (FPG): The amount of income below which a household of a given size is considered to be impoverished. The federal government updates the FPG annually. All MINNESOTACARE and some MA income standards are based on the FPG. FEE-FOR-SERVICE: A method of payment for health services. The medical provider bills and is paid for specific individual services. FFP: See Federal Financial Participation above. FICA: Social Security withholding tax. FIRST-YEAR CHANGE OPTION: A managed care ENROLLEE’s opportunity to change HEALTH PLANs once during the 1st year of enrollment in a health plan. FOOD STAMPS/FOOD SUPPORT: A program authorized by the U.S. Department of Agriculture to provide food assistance to low-income individuals or families. Benefits may be issued in the form of coupons, electronic benefits, or in cash to certain people who receive MFIP or MSA. The Food Stamp program is known as Food Support in Minnesota. FOSTER CARE: Care given to a DEPENDENT CHILD or adult including emergency, interim, or permanent care. FOSTER CHILD: A DEPENDENT CHILD who has been placed in a FOSTER CARE home or facility by a social services agency. FOSTER HOME: A home licensed to provided care to dependent children and/or adults. FOUR-MONTH RULE: MINNESOTACARE: One of the INSURANCE BARRIERS. The 4-month rule requires some people to have been uninsured for 4 months before they can enroll in MINNESOTACARE. See §0910.07 (4-Month Rule). Return to top GLOSSARY: FPG... 0902.15 FPG: The amount of income below which a household of a given size is considered to be impoverished. The federal government updates the FPG annually. All MINNESOTACARE and some MA income standards are based on the FPG. FULL-TIME STUDENT: A person who is enrolled in a graded or ungraded primary, intermediate, secondary, GED preparatory, trade, technical, vocational, or POST-SECONDARY SCHOOL and who meets the school's standard for full-time attendance. Summer vacations and school holidays do not affect the student's full-time status. Consider people who are enrolled and attending but do not meet the school’s standard for full-time attendance to be part-time students. GENERAL ASSISTANCE (GA): A program authorized under Minnesota Statutes 256D to provide cash assistance to needy individuals and couples without children. GENERAL ASSISTANCE MEDICAL CARE (GAMC): A program authorized under Minnesota Statutes 256D.03 to provide medical care to people receiving GA, or ineligible for medical coverage through MSA or MEDICAL ASSISTANCE as long as ineligibility for MA is not due to program non-compliance. People on GAMC may be eligible for MINNESOTACARE but may not be covered on both programs at the same time. GOOD CAUSE: The circumstances beyond a person's control which keep the person from following program requirements or specific eligibility conditions, such as premium payment or cooperation with MEDICAL SUPPORT. See §0915.11 (Fail to Pay Premium/Voluntary Cancellation) and §0906.13.05 (Good Cause Exemptions--Medical Support). GRACE MONTH: MINNESOTACARE: The final month in which an ENROLLEE may pay a premium without losing coverage. If the premium is not paid by the last working day of the grace month, coverage is terminated. The grace month is also known as the coverage month. See §0913 (Premiums and Spenddowns). GROSS INCOME: Total non-excluded income (minus expenses for SELF-EMPLOYMENT and certain student income) before any DEDUCTION or DISREGARD. GROSS RSDI: The RSDI benefit amount before deducting the MEDICARE premium. GROUP HOME: A specialized facility providing 24-hour care for no more than 10 children, including the group home PARENTS' own children under age 21. GROUP LIVING ARRANGEMENT: A public or private non-profit facility certified under Section 1616(e) of the Social Security Act or a comparable state law or rule which serves no more than 16 people. This may include ICF-MRs. GROUP RESIDENTIAL HOUSING: A group living situation which has a fixed rate contract with a county to provide room and board for MSA or GA clients. This includes FOSTER CARE settings for a single adult. It does not include battered women's shelters or medical care (TITLE XIX) facilities. GROUP STATUS: MINNESOTACARE: The ELIGIBILITY GROUP to which an individual is assigned. See §0907 (Eligibility Groups and Bases of Eligibility). HALFWAY HOUSE: 1. A place that provides a temporary residence for people waiting for institutional placement. 2. A place that provides a temporary residence for people who have left an INSTITUTION and who are preparing to re-enter the community. Return to top GLOSSARY: HEALTH CARE... 0902.17 HEALTH CARE APPLICATION (HCAPP): A form which people can use to apply for GAMC, MA, or MINNESOTACARE. HEALTH CARE PROGRAMS: MINNESOTACARE, MEDICAL ASSISTANCE (MA), and GENERAL ASSISTANCE MEDICAL CARE (GAMC). MA includes QMB, SLMB, QWD, QI, MA-EPD and the federally funded waivers. The MA references in this manual apply to these programs unless otherwise stated. References to the statefunded PRESCRIPTION PROGRAM are included under MA and identified as applying to Prescription Drug. HEALTH INSURANCE INFORMATION FORM (HIIF): A form (DHS 1922 or 1922b) used to supply information on ENROLLEES’ other health coverage to the BENEFIT RECOVERY SECTION. See §0910 (Other Health Coverage). HEALTH MAINTENANCE ORGANIZATION: An organization licensed by the Department of Health to provide all defined health care benefits to people in return for a capitated payment. HEALTH PLAN: An organization contracting with the State to provide health services to ENROLLEES covered by MA, GAMC, or MINNESOTACARE in exchange for a monthly CAPITATION payment. A health plan may be a HEALTH MAINTENANCE ORGANIZATION or other defined group of medical providers. See MANAGED CARE in §0902.23 (Glossary: Managed Care...). HILL-BURTON ACT: A federal act that gives hospitals and other health facilities money to build and remodel in return for providing a limited volume of services to people living in their area who cannot pay for health care. HOME AND COMMUNITY BASED SERVICES: Services not normally covered by MA which are covered under a WAIVER, including CASE MANAGEMENT, homemaker services, home health aide, personal care, adult day health treatment, habilitation, respite care, and day treatment for individuals with chronic mental illness. See §0907.23 (MA Waiver Programs) for detailed information on the services covered under each waiver. Also see EXCLUDED TIME SERVICES in §0902.11 (Glossary: Effective...). Except for personal care attendant services, home and community based services are not considered excluded time services. HOSPITAL LEAVE DAY: MA: Each day an LTCF is eligible for MA payment even though the client has been transferred to an INPATIENT hospital for medically necessary health care. See §0908.15 (Nursing Facilities and ICF-MR Leave Days). HOUSEHOLD REPORT FORM (HRF): MA and GAMC: A form (DHS-2120) used by ENROLLEES to report income and circumstance changes. HOUSEHOLD SIZE: MINNESOTACARE: The number of people used to determine the premium amount for the number of individuals covered. The household size is also used to determine income eligibility. MA/GAMC: The number of people used to determine each person’s income standard. See §0908.05 (Determining MA/GAMC Household Size). IEVS (INCOME AND ELIGIBILITY VERIFICATION SYSTEM): A set of data exchanges with other state and federal sources that is used to verify income and assets of MA APPLICANTS and ENROLLEES. IMD (INSTITUTION FOR MENTAL DISEASES): An INSTITUTION for the treatment of mental diseases. See §0907.27 (MA/GAMC Basis: IMD Residents) for information on eligibility for IMD residents. IMMIGRANT: A person who leaves another country to settle permanently in the U.S. IMMIGRANT SPONSOR: 1. A person, church, organization, or group agreeing to help receive and place refugees in the U.S. 2. A person who agrees to provide financial support to an IMMIGRANT as a condition of entry into the U.S. See SPONSOR in §0902.37 (Glossary: Sole...). IMMIGRATION AND NATURALIZATION SERVICE (INS): The former name of the federal agency responsible for immigration and citizenship. See U.S. CITIZENSHIP and IMMIGRATION SERVICES (USCIS) in §0902.41 (Glossary: UNDERINSURED). IMPROPER TRANSFER: When an ASSET is sold, given away, or otherwise disposed of for less than FAIR MARKET VALUE for the purpose of obtaining or maintaining MA or GAMC eligibility. Return to top GLOSSARY: IN-KIND... 0902.19 IN-KIND INCOME: Payment for a service in a form other than money, or receipt of non-cash gifts or non-cash contributions such as food or clothing. See §0911.09.17 (In-Kind Income). INCAPACITATED PARENT (IP): MA: A CARETAKER PARENT who is physically or mentally disabled for a period of at least 30 days. INCOME CERTIFICATION PERIOD or CERTIFICATION PERIOD: MA and GAMC: A 6-month period for determining income eligibility for clients. INCOME REVIEW: MA: A process for verifying income monthly or semi-annually. INDEMNITY POLICY: An insurance policy that pays benefits directly to people for each day of hospitalization or for a specified injury. Indemnity payments may cover certain costs not covered by other insurance but do not always limit benefits to paying for medical expenses. Consider indemnity payments as THIRD PARTY LIABILITY unless they are specifically designated as income replacement. Do not consider indemnity policies as other insurance for purposes of the INSURANCE BARRIERS. See §0910 (Other Health Coverage). INDIVIDUAL DEVELOPMENT ACCOUNT (IDA): An account funded under the Assets for Independence Act, Public Law 105-285. Federal funds are available to match funds that low-income working families put into savings for a 1st home, post-secondary education or to start a new business. Families who are eligible for MFIP, or who have income no greater than the maximum allowed to qualify for the EARNED INCOME CREDIT (EIC) and assets no greater than $10,000, excluding a home and 1 vehicle, are eligible for matching funds. The Minnesota Department of Children, Families and Learning (DCFL) operates Minnesota’s demonstration IDAs. INITIAL APPLICATION: MINNESOTACARE: An application received from a household who has had a break of at least 1 full calendar month in MinnesotaCare enrollment. INITIAL ENROLLMENT: MINNESOTACARE: The first month in which an individual or household has MINNESOTACARE coverage. The initial enrollment month does not change unless there is a break in coverage of more than 1 full calendar month. See CONTINUOUS ENROLLMENT in §0902.07 (Glossary: Client...). INITIAL PREMIUM PAYMENT: MINNESOTACARE: The 1st monthly premium payment which an APPLICANT must make before MINNESOTACARE coverage begins. See PEND AWAITING PAYMENT in §0902.27 (Glossary: Non-Citizen...). INPATIENT: A person admitted to a hospital. Inpatient applies to a person temporarily absent from the hospital with the approval of a physician. Inpatient does not apply to a person absent from the hospital against medical advice. INSTITUTION: An establishment that furnishes food, shelter, and some treatment or services to 4 or more people unrelated to the proprietor. An institution may be a single facility or multiple facilities owned by the same entity. INSTITUTION FOR MENTAL DISEASES (IMD): An INSTITUTION for the treatment of mental diseases. See §0907.27 (MA/GAMC Basis: IMD Residents) for information on eligibility for IMD residents. Return to top GLOSSARY: INSURANCE... 0902.21 INSURANCE BARRIERS: MINNESOTACARE: Eligibility criteria which govern when an ENROLLEE may have other health coverage or access to other health coverage currently or during a specified period. See §0910 (Other Health Coverage). INTEREST: 1. Money earned and paid to the holder of a bank account, loan, or other investment. Earned interest may be credited to the account or paid directly to the owner. See DIVIDEND in §0902.09 (Glossary: Denial...). 2. Money charged as a borrower’s fee on a loan. INTERSTATE AGREEMENT: The agreement between Minnesota and North Dakota to help resolve residence disputes for MA eligibility for long-term care. See §0906.05 (State Residence). IRREVOCABLE TRUST: A TRUST which allows neither the person originating the trust nor the BENEFICIARY to change the provisions of the trust. IV-D AGENCY: An agency responsible for CHILD and MEDICAL SUPPORT enforcement. IV-D UNIT: A unit within a county agency that is responsible for establishing PATERNITY and collecting CHILD SUPPORT and MEDICAL SUPPORT according to TITLE IV-D of the Social Security Act. IV-E ADOPTION AND FOSTER CARE: ADOPTION ASSISTANCE or FOSTER CARE placements that are funded under Title IV-E of the Social Security Act. JOINT OWNERSHIP: An ownership agreement in which two or more people own the same piece of property. Joint tenants have equal shares and rights to the property. Tenants-in-common prorate equity according to shares of ownership. LAWFUL PERMANENT RESIDENT (LPR): An IMMIGRANT legally admitted to the U.S. under the U.S. Immigration and Nationality Act on a permanent basis. See QUALIFIED NON-CITIZEN in §0902.31 (Glossary: Procedural...) and §0906.03.03 (Qualified Non-Citizens) for information on immigration status and eligibility for the HEALTH CARE PROGRAMS. LAWFUL TEMPORARY RESIDENT (LTR): A NON-IMMIGRANT legally admitted to the U.S. under the U.S. Immigration and Nationality Act on a temporary basis. LEAVE DAYS: MA: Any calendar day and all subsequent consecutive calendar days a client residing in a LONG TERM CARE FACILITY is absent overnight. A calendar day is a 24-hour period ending at midnight. An overnight absence from the facility of less than 23 hours does not constitute a leave day. When the client is absent from the facility to participate in active programming of the facility under the personal direction and observation of facility staff, do not consider the day a leave day. See §0908.15 (Nursing Facilities and ICF-MR Leave Days) for information on when leave days are eligible for MA payment. LEGAL GUARDIAN OF A MINOR: A person who has been appointed or accepted as a guardian pursuant to Minnesota Statutes, sections 260.242, 525.615, 525.617, or 525.6165, and related laws. MINNESOTACARE: A person designated by a court to assume responsibility to care for a CHILD. The guardian has all the powers and responsibilities that would otherwise be held by the PARENT of the child or the adult ward. The guardian may choose to be considered part of the child’s FAMILY and be included in the HOUSEHOLD SIZE. LIEN: A legal claim against property for the satisfaction of a debt. The lien is paid off at the time the property is sold. LIFE ESTATE: A legal procedure to limit the ownership of an ASSET to a person's lifetime according to Minnesota Statutes, Sections 500.01 to 500.24. Life estates are REAL PROPERTY. Establishing a life estate is a TRANSFER. See §0909.13.07 (Life Estates). LIFE ESTATE MORTALITY TABLE: Chart issued in the SOCIAL SECURITY ADMINISTRATION’s Program Operations Manual (POMS) as specified by the Commissioner of Revenue in the Code of Federal Regulations (CFR). This table is used to compute the value of a life estate based on a person’s age. See §0909.13.07.03 (Life Estate Mortality Table). LIFE EXPECTANCY TABLE: Chart issued in the SOCIAL SECURITY ADMINISTRATION’s Program Operations Manual (POMS). This chart is used to determine whether annuitizing an annuity is a transfer for less than FAIR MARKET VALUE. See §0909.23.03 (Life Expectancy Table - Annuities). LIQUID ASSETS: Cash or property (such as stocks or bonds) easily converted to cash. LONG TERM CARE CONSULTATION (LTCC): A screening program that prevents inappropriate nursing home or boarding care placement. Formerly known as PRE-ADMISSION SCREENING (PAS) PROGRAM. LONG TERM CARE FACILITY (LTCF): A place such as a nursing facility, intermediate care facility for the mentally retarded (ICF-MR), medical hospital, or an MA-covered bed in the REGIONAL TREATMENT CENTER (RTC). LONG TERM CARE FACILITY RESIDENT: A person living in a LONG TERM CARE FACILITY. LONG TERM CARE SPOUSE: A married person living in a medical or nursing facility who is expected to remain there for at least 30 consecutive days; or a person who is expected to receive or to continue to receive waivered services through the ELDERLY WAIVER (EW) for 30 consecutive days beginning on the date the LONG TERM CARE CONSULTATION determines the person needs a long term care level of care. LUMP SUM: Cash received on a non-recurring or irregular basis that cannot reasonably be anticipated. Examples of lump sums include winnings, insurance settlements, inheritances, and retroactive payments of RSDI, VA, and REEMPLOYMENT INSURANCE. See §0911.05 (Excluded Income). MAINTENANCE NEEDS ALLOWANCE: The amount of monthly income protected for people eligible under the SIS EW program. People with incomes less than the maintenance need allowance are eligible without a SPENDDOWN or WAIVER OBLIGATION. The maintenance needs allowance is determined by adding the MSA equivalent rate and the clothing and personal needs allowance. It is updated annually. The amount of the maintenance needs allowance changes annually. See §0913.13.05 (Waiver Obligation--SIS EW). Return to top GLOSSARY: MANAGED CARE... 0902.23 MANAGED CARE: A method of payment under which enrollees receive most medical services through a HEALTH PLAN or network of providers which coordinates the services provided. DHS pays the HEALTH PLANs a fixed rate in advance for each ENROLLEE. Medical bills for non-MANAGED CARE clients are paid through FEEFOR-SERVICE. See CAPITATION in §0902.05 (Glossary: Capital...) and §0914 (Service Delivery). MARITAL RELATIONSHIP: MINNESOTACARE: A spousal relationship. See SPOUSE in §0902.37 (Glossary: Sole...). MASS CHANGE: A change brought about by a shift in federal or state policy which affects many or all households. MAXIS: Minnesota's statewide automated eligibility system for county-administered programs, including the former AFDC program, Emergency Assistance, FOOD STAMPS, GENERAL ASSISTANCE, GENERAL ASSISTANCE MEDICAL CARE, MEDICAL ASSISTANCE, MFIP, and MINNESOTA SUPPLEMENTAL AID. MEDICAID MANAGEMENT INFORMATION SYSTEM (MMIS): Minnesota’s statewide automated system for MinnesotaCare eligibility and payment of medical claims and CAPITATION payments for MINNESOTACARE, MA, and GAMC. MEDICAL ASSISTANCE (MA): The program established under Title XIX of the Social Security Act and Minnesota Statutes 256B providing for health care to needy people. People may receive MA in conjunction with an MSA grant or as a separate program. MEDICAL CLAIM HISTORY: A listing of a CLIENT's medical expenses paid by the HEALTH CARE PROGRAMS. MEDICAL SUPPORT: Cash payments or health insurance coverage that a NON-CUSTODIAL PARENT provides or is courtordered to provide to meet the medical needs of the non-custodial PARENT’s child(ren). Court orders generally require medical support payments until the CHILD is 18 but may require payments beyond age 18 in some cases. MEDICALLY NECESSARY: A health service rendered in response to a life-threatening condition or pain; to treat an injury, illness, or infection; to achieve a level of physical or mental function consistent with prevailing community standards for the diagnosis or condition; to care for a mother and child through the maternity period; is a preventative health service; or to treat a condition that could result in physical or mental DISABILITY. The provider's professional peer group must recognize the service as the prevailing standard or current practice and as consistent with the recipient's diagnosis or condition. MEDICARE: A federal health insurance program for people who are over 65, disabled, BLIND, or have permanent kidney failure. Part A covers hospital care, hospice care, and home health care. Part B covers doctor's services, x-rays, laboratory services, and medical supplies. Return to top GLOSSARY: MFIP... 0902.25 MFIP: See MINNESOTA FAMILY INVESTMENT PLAN (MFIP). MINNESOTA COMPREHENSIVE HEALTH ASSOCIATION (MCHA): A plan which provides health insurance to people who are otherwise uninsurable due to health conditions or other circumstances specified in statute. To qualify for MCHA, people must provide a denial of private coverage. MCHA coverage often has high premiums and may require DEDUCTIBLES, co-insurance, or co-payments. MINNESOTA FAMILY INVESTMENT PLAN (MFIP): A program authorized under the federal Temporary Assistance to Needy Families (TANF) block grant and Minnesota Statutes 256J to provide cash assistance and employment support to needy families. MFIP replaced the AFDC program. See AID TO FAMILIES WITH DEPENDENT CHILDREN (AFDC) in §0902.01 (Glossary: 10-Day...) MINNESOTA SUPPLEMENTAL AID (MSA): A state-funded program that provides cash assistance to SSI recipients, BLIND people, people age 65 or older, and disabled people who are age 18 and older. MINNESOTACARE: A subsidized premium-based HEALTH CARE PROGRAM for some families with children and some adults without children. It is administered by DHS and by COUNTY AGENCIES that elect to be MinnesotaCare enrollment sites. DHS receives FFP for some ENROLLEEs. Others are funded through the health care access fund. MINNESOTACARE OPERATIONS: The organizational unit at DHS responsible for determining MINNESOTACARE eligibility and providing case maintenance to ENROLLEEs. MINOR CHILD: A CHILD under age 18. See DEPENDENT CHILD in §0902.09 (Glossary: Denial...). MINOR PARENT: MINNESOTACARE AND MA: For purposes of determining household composition and counting parental income in a 3generation household, consider a person who is under the age of 21 years, has never been married or otherwise legally EMANCIPATED, and is the birth parent of a DEPENDENT CHILD living in the same household to be a MINOR PARENT. For all other purposes, such as medical support and social services referrals, a MINOR PARENT is a person under the age of 18 years who has never been married or otherwise legally EMANCIPATED who is a birth parent of a minor child. MMIS: MEDICAID MANAGEMENT INFORMATION SYSTEM. Minnesota’s statewide automated system for MINNESOTACARE eligibility and payment of medical claims and CAPITATION payments for MINNESOTACARE, MA, and GAMC. MONTH OF APPLICATION: The month in which MINNESOTACARE or a county agency receives a client's APPLICATION for coverage under the HEALTH CARE PROGRAMS. MONTHLY MEDICAL SPENDDOWN CALCULATION: MA and GAMC: One type of medical SPENDDOWN calculation for people who do not qualify for MA or GAMC due to excess income. See §0913.09 (Automated Monthly Spenddown) and §0913.11 (Manual Monthly Spenddown). MONTHLY REPORTING: MA and GAMC: The requirement to complete a HOUSEHOLD REPORT FORM every month. See §0905.07 (Monthly Reporting). MORTALITY TABLES: See LIFE ESTATE MORTALITY TABLE and LIFE EXPECTANCY TABLE in §0902.21 (Glossary: Insurance). MULTIPLE HEALTH PLAN MODEL: A health service delivery system that allows MANAGED CARE recipients to enroll in 1 of 2 or more HEALTH PLANs. NET INCOME: MA and GAMC: Income remaining after each program's DEDUCTIONS and DISREGARDS are subtracted from GROSS INCOME. NETHERLANDS' ACT (WUV): WUV is a Dutch acronym for payments the Dutch government makes under the Netherlands' Act on Benefits for Victims of Persecution 1940-1945. These payments are for both Dutch and non-Dutch people who, during the German and Japanese occupation of the Netherlands and Netherlands East Indies (now the Republic of Indonesia) in World War II, were victims of persecution because of their race, religion, beliefs, or homosexuality and, as a result of that persecution, suffer from illness or DISABILITY. Payments under this Act began January 1, 1973, and include 4 categories of benefits: periodic income payments; compensation for non-definable disability expenses (Dutch acronym, NMIK); reimbursement of persecution-related disability expenses; and partial compensation for persecution-related disability expenses. See §0911.05 (Excluded Income). Return to top GLOSSARY: NON-CITIZEN... 0902.27 NON-CITIZEN: A person who is not a U.S. citizen. NON-CUSTODIAL PARENT: A PARENT who does not have physical custody of a CHILD. NON-IMMIGRANT: A person from another country who is admitted to the U.S. on a temporary basis and does not have USCIS permission to settle permanently. See UNDOCUMENTED PEOPLE in §0902.41 (Glossary: Underinsured...). NON-REIMBURSABLE MEDICAL EXPENSE: MA and GAMC: An expense that is not eligible for payment under MA or GAMC but that is Prescribed or recommended in writing by the enrollee’s physician or dentist AND Of direct benefit to the enrollee AND Available but not necessarily obtained through a licensed medical provider. MEDICALLY NECESSARY non-reimbursable expenses may be allowed as spenddown deductibles. See MEDICALLY NECESSARY in §0902.23 (Glossary: Managed Care...) and §0913.21 (Allowable Medical Bills to Meet Spenddown). EXAMPLE: Jim’s dentist, a licensed provider, refers him to a specialist who is not a licensed provider. Although the expense is not reimbursable through MA, it can be allowed as a non-reimbursable spenddown deductible. EXAMPLE: Glenda purchased vitamins through a mail-order company. Her physician advised her to take the vitamins for a 12-month period. Although the mail order company is not a licensed provider and cannot be reimbursed, the vitamins could have been obtained through a licensed pharmacy and can be allowed as a non-reimbursable spenddown deductible. EXAMPLE: Matt purchased a prescription drug while enrolled in MA, and incurred a $3 co-payment. The copayment amount can be allowed as a non-reimbursable spenddown expense. Do not allow expenses for food or utilities as a spenddown deductible, even if the cost is related to a special diet or medical equipment recommended by a physician. Do not allow items that do not directly benefit the enrollee, such as special equipment requested by the enrollee’s personal care attendant or other caretaker. OPEN ENROLLMENT: The annual period during which MANAGED CARE ENROLLEES may change HEALTH PLANs. OVERPAYMENT: MA and GAMC: Benefits households receive that exceed the amount for which they are eligible. PARENT: MINNESOTACARE: A CHILD's biological or adoptive mother or father whose parental rights have not been terminated or STEPPARENT. MA: A CHILD's legal biological or adoptive mother or father whose parental rights have not been terminated. PARENTAL FEE: MA: An amount assessed to the PARENTs of a MINOR CHILD as reimbursement for the cost of care of a CHILD under 18 who receives MA without consideration of parental income and ASSETS. See §0906.13.09 (Parental Fees). PARENTAL RELATIONSHIP: MINNESOTACARE: The relationship that exists between a PARENT and his or her biological or adoptive CHILD. PARTNERSHIP: A SELF-EMPLOYMENT enterprise in which 2 or more people share in the profits and losses of the business according to their individual shares of ownership. PATERNITY: Legal fatherhood, either adjudicated or acknowledged by the father. PEND: 1. To enter an APPLICATION that has not yet been approved or denied on MAXIS or MMIS. 2. To delay approving or denying an application until more information is received. PEND AWAITING PAYMENT: MINNESOTACARE: To approve an APPLICATION conditioned on the receipt of the INITIAL PREMIUM PAYMENT. When an application is pending awaiting payment, the household has been found eligible for MINNESOTACARE but will not have coverage until the month after DHS receives the initial payment. Return to top GLOSSARY: PENSION... 0902.29 PENSION: A fixed sum paid regularly to retired people or their dependents. PERSON Chapter INDEX (PMI) NUMBER: A unique identification number that MAXIS assigns to each person. The PMI number is used to verify the person’s eligibility under the HEALTH CARE PROGRAMS. PERSONAL PROPERTY: Property that is not considered REAL PROPERTY. See §0909 (Assets) for treatment of specific types of property. PERSONAL RESPONSIBILITY AND WORK OPPORTUNITY RECONCILIATION ACT (PRWORA): Federal law signed on 8-22-96 which eliminated the federal entitlement program AID TO FAMILIES WITH DEPENDENT CHILDREN (AFDC) and created a new program called Temporary Assistance for Needy Families (TANF). PRWORA provides block grants to states to offer time-limited cash assistance. It also made major changes in the FOOD STAMP Program and delinked eligibility for Medicaid from receipt of cash assistance. PICKLE DISREGARD: MA: An UNEARNED INCOME DISREGARD for some MA clients who lost eligibility for 1619(a), 1619(b), SSI or MSA and would remain eligible if RSDI cost of living increases are disregarded. See §0912.05.23 (Pickle Disregard). PIGGYBACK GAMC or PIGGYBACK MA: Term formerly used to describe GAMC or MA that is automatically set up when a cash program is approved, currently known as automatic MA. People approved for MSA in the community get piggyback MA. Most people approved for GA who do not meet a BASIS OF ELIGIBILITY for MA get piggyback GAMC. People approved for MFIP must have a separate MA or MinnesotaCare determination. PLAN TO ACHIEVE SELF SUPPORT (PASS): A plan approved by the COUNTY AGENCY for MA or MSA recipients or the SOCIAL SECURITY ADMINISTRATION for SSI recipients which allows certain client ASSETS or income to be excluded in determining benefits for some assistance programs. See §0912.05.11 (Plan to Achieve Self-Support). POST-SECONDARY SCHOOL: A school serving students beyond the 12th grade, such as a community college, university, or technical college. PRE-ADMISSION SCREENING (PAS) PROGRAM: A screening program that prevents inappropriate nursing home or boarding care placement. PRE-EXISTING CONDITION: A medical condition existing before an insurance policy took effect. Some health insurance policies limit or exclude coverage for pre-existing conditions. PREPAID GENERAL ASSISTANCE MEDICAL CARE PROGRAM: The program through which GAMC MANAGED CARE ENROLLEES receive medical services. PREPAID MEDICAL ASSISTANCE PROGRAM: The program through which MA MANAGED CARE ENROLLEES receive medical services. PRESCRIPTION DRUG PROGRAM (PDP): A state-funded program to help pay the prescription drug costs of eligible people who receive QMB or SLMB. See §0907.21.09.11 (Medicare Supplement Programs: PDP). PREVENTIVE COVERAGE: MINNESOTACARE: A term used by insurance companies to describe services provided to keep enrollees healthy and promote continuous health care. Preventive care includes services such as routine physical exams, immunizations, and prenatal care. PRESUMED ELIGIBILITY: MINNESOTACARE: See DELAYED VERIFICATION in §0902.07 (Glossary: Client...). PRINCIPAL WAGE EARNER (PWE): MA: The PARENT in a 2-parent household who earned the most income in the 24 months before the APPLICATION. See §0907.19.07 (MA Families and Children: AFDC-Related Adults). PRISM: Minnesota’s automated system for the establishment and enforcement of CHILD SUPPORT and MEDICAL SUPPORT. PRIVATE DATA: Data not available to the public under state law. It is available to the subject of the data and that person's AUTHORIZED REPRESENTATIVE. See §0903.03.05 (Client Rights--Privacy Rights). Return to top GLOSSARY: PROCEDURAL ELIGIBILITY... 0902.31 PROCEDURAL ELIGIBILITY: Things people have to do to be eligible for coverage under the HEALTH CARE PROGRAMS, such as requirements regarding social security numbers, cooperating with obtaining MEDICAL SUPPORT, and assigning rights to other health coverage. See §0906 (Technical/Procedural Eligibility). PROCESSING PERIOD: The time program rules allow for processing an APPLICATION. Also called PROCESSING STANDARDS. PROCESSING STANDARDS: The period of time allowed to determine eligibility. PROGRAM L: MINNESOTACARE: The MMIS designation for the range of medical services available to pregnant women and children on MINNESOTACARE. PROGRAM X: MINNESOTACARE: The MMIS designation for the range of medical services available to non-pregnant PARENTS with income over 175% FPG and adults without children on MINNESOTACARE. PROPORTIONATE SHARE: MINNESOTACARE: The amount of a household’s income attributed to each individual member of the household in determining whether the household contains a DEPENDENT SIBLING. See §0908 (Household Composition). QUALIFIED INDIVIDUAL (QI): A person eligible for payment of all or part of the MEDICARE Part B payment by the MA program. The person does not have to be eligible for MA. See §0907.21.09.09 (Medicare Supplement Programs: QI). QUALIFIED MEDICARE BENEFICIARY (QMB): A person eligible for payment of some MEDICARE expenses (premiums, CO-PAYMENTS and DEDUCTIBLES) by the MA program. The person does not have to be eligible for MA. See §907.21.09.03 (Medicare Supplement Programs--QMB) for eligibility requirements. QUALIFIED NON-CITIZEN: A legal IMMIGRANT who: OR OR OR OR Is lawfully admitted for permanent residence under the Immigration and Nationality Act (INA) and was living in the U.S. before 8-22-96. Was admitted to the U.S. as a refugee under section 207 of the INA. Was granted asylum under section 208 of the INA. Whose deportation is being withheld under section 243(h) of the INA. Was paroled under section 212(d)(5) of the INA for a period of at least 1 year and was living in the U.S. before 8-22-96. OR Was granted conditional entry pursuant to section 203(A)(7) of the INA as in effect prior to 4-1-80, and was living in the U.S. before 8-22-96. OR Is a BATTERED NON-CITIZEN or CHILD of a battered NON-CITIZEN. See battered non-citizen in §0902.03 (Glossary: Assignment...). OR Is a Cuban or Haitian entrant. OR Is an honorably discharged U.S. veteran or the SPOUSE or unmarried dependent child of such veteran. OR Is an immigrant on active duty with the U.S. armed forces or the SPOUSE or DEPENDENT CHILD of an immigrant on active duty. For information on how qualified status affects eligibility for the HEALTH CARE PROGRAMS, see §0906.03 (Citizenship and Immigration Status). QUALIFIED WORKING DISABLED ADULT (QWD): A person eligible for payment of the MEDICARE Part A premium by the MA program. The person cannot receive MA or QMB benefits. See §0907.21.09.07 (Medicare Supplement Programs--QWD) for eligibility requirements. Return to top GLOSSARY: QUALITY... 0902.33 QUALITY ASSURANCE: MINNESOTACARE: A performance evaluation system established by the Minnesota Legislature to review the accuracy of MINNESOTACARE determinations. QUALITY CONTROL: A performance evaluation and reporting system established by Congress to review federal assistance programs including MA. QUALITY CONTROL REVIEWER: The person designated by the state or federal government to conduct the QUALITY CONTROL or QUALITY ASSURANCE review according to federal and state standards. REAL PROPERTY: Land, all buildings, structures, improvements, or other fixtures on it belonging or pertaining to the land and all mines, minerals, fossils, and trees on or under it. LIFE ESTATES are real property. A mobile home is real property if it is attached to a foundation on land owned by the unit. REASONABLE COMPENSATION: Value received in exchange for transferred property which equals or exceeds the property’s FAIR MARKET VALUE, less any ENCUMBRANCES and sale costs. RECERTIFICATION: A term formerly used for the annual RENEWAL of eligibility for MA and GAMC. See RENEWAL in §0902.35 (Glossary: Renewal...). RECOGNITION OF PARENTAGE (ROP): A form (DHS 3159) printed by the Minnesota Department of Human Services (DHS) that serves as an ACKNOWLEDGMENT OF PATERNITY. This form can only be signed after the CHILD's birth. Notarized signatures of both PARENTS must be on the form. REEMPLOYMENT INSURANCE: See UNEMPLOYMENT INSURANCE in §0902.41 (Glossary: Underinsured...) REFEREE: A person who presides over APPEAL hearings and issues a recommendation on the appealed matter to the Commissioner of DHS. REFUGEE CASH ASSISTANCE (RCA): A program that provides financial help to refugees ineligible for both MFIP and SSI. REFUGEE MEDICAL ASSISTANCE (RMA): A federally authorized program providing MEDICAL ASSISTANCE to refugees. See §0907.21.13 (MA Basis: Refugee Medical Assistance - RMA). REGIONAL TREATMENT CENTER (RTC): State hospital for the treatment of mental diseases. REINSTATEMENT MONTH: MINNESOTACARE: The month following the month in which a household is canceled for non-payment. The enrollee must pay all billed premiums by the reinstatement month due date to receive coverage back to the date of cancellation. See §0915.11.05 (Fail to Pay Premium/Reinstatement). RELATIVE CARETAKER: MINNESOTACARE: A CARETAKER related to a DEPENDENT CHILD as a natural or adoptive PARENT, STEPPARENT, grandparent, great-grandparent, great-great-grandparent, sister, step-sister, brother, stepbrother, aunt, great or great-great-aunt, uncle, great or great-great-uncle, nephew, niece, 1st cousin, 1st cousin once removed, or SPOUSE to any person listed above even if the marriage terminated by death or divorce. PARENTs and STEPPARENTs are always considered in the household size of children with whom they live and their income is counted for the child’s eligibility. Non-parent caretakers may choose to include the child in their household or apply separately for the child. If coverage is not requested for the children in a non-parent caretaker’s household, do not include the children in the household size. See §0908 (Household Composition). MA: Follow MinnesotaCare, EXCEPT that STEPPARENTs are not defined as PARENTs. STEPPARENTs may qualify as relative caretakers if the biological or adoptive parent is not in the home. PARENTs are always counted in the household size of the child(ren) with whom they live and their income is counted for the child’s eligibility unless the child receives MA with a deeming waiver. See §0908.05 (Determining MA/GAMC Household Size). Return to top GLOSSARY: RENEWAL... 0902.35 RENEWAL: The annual process which a WORKER uses to determine a household’s continued eligibility and premium or SPENDDOWN amount for MINNESOTACARE, MA or GAMC. REPRESENTATIVE PAYEE: A person or organization, selected by the SOCIAL SECURITY ADMINISTRATION, who is designated to receive benefits on behalf of an RSDI or SSI recipient and is obligated to use those benefits for the RSDI or SSI recipient's personal care and well being. RETIREMENT, SURVIVORS, AND DISABILITY INSURANCE (RSDI): A program operated by the SOCIAL SECURITY ADMINISTRATION that provides a monthly income to retired people, survivors or dependents of insured people, and people with disabilities. See §0911.09.15 (Income From RSDI and SSI) and §0911.09.15.01 (Income From RSDI and SSI--MA/GAMC). RETROACTIVE ELIGIBILITY: MA: Eligibility for MA up to 3 months before the month of APPLICATION. GAMC: Eligibility for GAMC up to 1 month before the month of application. RULE 24: Minnesota's Consolidated Treatment Fund. RULE 35 FACILITIES: Facilities offering a rehabilitation program to 5 or more chemically dependent people at one time. RULE 36 FACILITIES: Facilities offering residential care and program services to 5 or more adult mentally ill people at one time. RULE 78: A funding mechanism for community mental health grants. Rule 78 may fund placements in RULE 36 FACILITIES or other living arrangements in the community. S-CORPORATION: A small business corporation of 35 or fewer shareholders. Each shareholder reports his or her share of income or loss separately. SAPSNF: MA and GAMC: The monthly Statewide Average Payment for a Skilled Nursing Facility. The SAPSNF is used to determine the period of ineligibility for long term care services or GAMC resulting from an IMPROPER TRANSFER of ASSETS. SAVE: Acronym for Systematic Alien Verification for Entitlements. SAVE is a process which allows access to INS data to validate the immigration status of NON-CITIZEN APPLICANTS, or for ENROLLEES who report a change in immigration status, for MA, RMA, MINNESOTACARE for Families with Children, and GAMC. Workers access the INS data through the Alien Status Verification System (ASVS). See §0906.03.11.01 (Systematic Alien Verification for Entitlements--SAVE). See the Combined Manual for information on using SAVE for the cash and food stamp programs. SDXS/SDXI: The State Data Exchange reports. A monthly IEVS tape exchange between the SOCIAL SECURITY ADMINISTRATION (SSA) and DHS. It includes information on the SSI grant and income and asset information SSA uses to compute the grant. SEASONAL INCOME: Income that is regularly received for only part of the year. See §0911.09.09 (Seasonal Income). SELF-EMPLOYMENT: Employment where people generally work for themselves rather than an employer and are responsible for their own work schedule. Self-employed people must file specific schedules as part of their federal tax returns. See §0911.09.03 (Self-Employment Income). SELF-INSURED: An employee health insurance plan that an employer administers itself or through an insurer, TRUST, or agent. Under a self-insured plan, the employer provides coverage to employees directly or indirectly rather than purchasing coverage from an insurance company. Self-insured plans are regulated under the Employer Retirement Income Security Act (ERISA) and are not subject to state insurance regulations. SEMI-INDEPENDENT LIVING SERVICES (SILS) PROGRAM: Training, counseling, and supervision services for people who need less than 24-hour care. SENIOR DRUG PROGRAM (SDP): The former name of the PRESCRIPTION DRUG PROGRAM. See §0902.29 (Glossary: Pension. . .). SERVICE LIMITED MEDICARE BENEFICIARY (SLMB): A person eligible for payment of the MEDICARE Part B premium by the MA program. The person does not have to be eligible for MA. See §0907.21.09.05 (Medicare Supplement Programs: SLMB) for eligibility requirements. SIBLINGS: Brothers and sisters related through 1 or both PARENTS. SOCIAL SECURITY: See RETIREMENT, SURVIVORS, AND DISABILITY INSURANCE above. SOCIAL SECURITY ADMINISTRATION (SSA): A federal agency which administers the SSI and RSDI programs. SOCIAL SECURITY DISABILITY INSURANCE: The term sometimes used for the disability insurance part of the RETIREMENT, SURVIVORS, AND DISABILITY INSURANCE (RSDI) program. Return to top GLOSSARY: SOLE... 0902.37 SOLE PROPRIETOR: A person who is the sole owner of an unincorporated SELF-EMPLOYMENT business. SPECIAL INCOME STANDARD (SIS): MA: An income standard equal to 3 times the FEDERAL BENEFIT RATE (FBR). The SIS is used to determine eligibility for the ELDERLY WAIVER (EW). See §0907.23.11 (MA Waiver Programs: EW). SPECIAL PERSONAL ALLOWANCE: An income DISREGARD for certain MA clients with mental retardation. See §0912.05.09.07 (Special Personal Allowance Disregard). SPENDDOWN: MA and GAMC: A method available to people who do not qualify for MA or GAMC due to excess income. People may become eligible by incurring medical expenses equal to or greater than the excess income for a 1-month or 6-month period. See §0913.03 (Spenddowns--MA and GAMC). SPENDDOWN SATISFACTION DATE: The date when medical expenses exceed the CLIENT's excess income to satisfy the SPENDDOWN. See §0913.21 (Allowable Medical Expenses to Meet Spenddowns). SPONSOR: Any person, or public or private agency or organization, who signed an affidavit agreeing to support an IMMIGRANT (who is not the DEPENDENT CHILD or SPOUSE of the sponsor) as a condition of the immigrant's entry into the U.S. SPOUSE: A person who is legally married to another person; a husband or wife. SSN: Social security number. STANDARD DEDUCTION: MA: An income DEDUCTION applied to the income of CLIENTs using Method B. See §0912.05.13 (Standard Deduction). STATE MEDICAL REVIEW TEAM (SMRT): A unit at DHS that determines DISABILITY in consultation with medical professionals appointed by the commissioner. STEPPARENT: A person who is not a CHILD’s biological or adoptive PARENT but is the spouse of a child's biological or adoptive parent. STEPSIBLING: The biological or adoptive CHILD of a child’s STEPPARENT. STUDENT: A person enrolled in and attending an educational institution. See FULL-TIME STUDENT in §0902.15 (Glossary: FPG...). STUDENT FINANCIAL AID: Loans, grants, scholarships, and work study funds to be used for educational and living expenses while attending school. SUBSTANTIAL CHANGE: MINNESOTACARE: A change in income from what a household reported on the previous year’s tax forms. See §0911.11 (Computing Countable Income--MinnesotaCare). SUPPLEMENTAL SECURITY INCOME (SSI): A program operated by the SOCIAL SECURITY ADMINISTRATION that provides monthly income to low income AGED, BLIND, and people with a DISABILITY. See §0911.09.15 (Income From RSDI and SSI) and §0911.09.15.01 (Income From RSDI and SSI--MA/GAMC). TECHNICAL ELIGIBILITY: Non-financial eligibility requirements such as citizenship and residence. See §0906 (Technical/Procedural Eligibility). TEFRA: MA: A WAIVER that provides MA eligibility to some disabled children who live with their families. See §0907.23.09 (MA Waiver Programs: TEFRA). TEMPORARY ABSENCE: A period of time a person may be physically absent from a residence but still considered to be in the household. See §0908.13 (Temporary Absence--MinnesotaCare - Part 1), §0908.13.01 (Temporary Absence--MinnesotaCare - Part 2), and §0908.13.03 (Temporary Absence--MA/GAMC). TEN-DAY NOTICE: Notices mailed or given to clients at least 10 days before the date of action. Return to top GLOSSARY: TENNESSEN... 0902.39 TENNESSEN WARNING: A statement of rights given to people who are asked to provide private or confidential data about themselves. See §0903.03.05 (Client Rights--Privacy Rights). TERMINATION: A discontinuation of program participation and benefits. See CANCELLATION in §0902.03 (Glossary: Assignment...). THERAPEUTIC LEAVE DAY: MA: Each day an NF I, NF II, or ICF-MR is eligible for MA payment even though the CLIENT is in a residential setting other than an LTCF, a hospital, or another entity eligible to receive federal, state, or county funds for the client's maintenance. See LEAVE DAYS. THIRD PARTY LIABILITY (TPL): The obligation of a person or organization other than MA, GAMC, or MINNESOTACARE to pay for a person’s medical expenses. Examples of TPL include group or private health insurance, auto insurance, WORKER’S COMPENSATION, and personal liability insurance. See §0910 (Other Health Coverage) and §0910.13 (Third Party Liability). TIMELY NOTICE: A notice sent at least as far ahead of the proposed action as program rules require. TITLE IV-D: The part of the Social Security Act that authorizes establishing PATERNITY and collecting CHILD and MEDICAL SUPPORT by the IV-D UNIT. See IV-D AGENCY and IV-D UNIT in §0902.21 (Glossary: Insurance...). TITLE IV-E ADOPTION ASSISTANCE: A federally funded program providing financial assistance to adoptive PARENTS. See ADOPTION ASSISTANCE in §0902.01 (Glossary: 10-Day...) and IV-E ADOPTION AND FOSTER CARE in §0902.21 (Glossary: Insurance...). TITLE IV-E FOSTER CARE: FOSTER CARE payments authorized under Title IV-E of the Social Security Act. See IV-E ADOPTION AND FOSTER CARE in §0902.21 (Glossary: Insurance...). TITLE XIX: The section of the Social Security Act authorizing the MEDICAL ASSISTANCE Program. TORT LIABILITY: The legal obligation of a party responsible for an accident or injury to pay for the resulting costs. TORT SETTLEMENT: Compensation awarded as a result of a lawsuit filed to recover costs related to an accident or injury. TRANSFER: To cause right, title, or interest in REAL PROPERTY or PERSONAL PROPERTY to pass from 1 person to another. TRANSITIONAL MEDICAL ASSISTANCE (TMA): Up to 4 months of additional medical coverage provided to some people terminated from regular MA because of increased child or spousal support. See §0907.19.11 (Transitional/Transition Year MA). TRANSITION YEAR MEDICAL ASSISTANCE (TYMA): Up to 12 months of additional medical coverage provided to some people terminated from regular MA due to increased earnings, loss of earned income disregards, or a combination of loss of child/spousal support and increased earnings/loss of earned income disregards. See §0907.19.11 (Transitional/Transition Year MA) and §0907.19.11.05 (TMA/TYMA Changes and Reporting Requirements). TRICARE: Insurance coverage provided through the Civilian Health and Medical Program of Uniformed service. See CHAMPUS in §0902.05 (Glossary: Capital...) TRUST: Any arrangement in which a grantor transfers money or property to a trustee(s) with the intention that it be held, managed or administered by the TRUSTEE for the benefit of certain designated persons (BENEFICIARIES). See §0902.39.01 (GLOSSARY: Trust Definitions) for additional definitions related to trusts. TRUST AGREEMENT: The legal documentation establishing a TRUST. TRUST FOR BURIAL: Funds paid or designated in advance for funeral expenses and held in a TRUST. TRUST FOR CREMATION: Funds paid in advance for funeral expenses and held in a TRUST. TRUST PRINCIPAL: Property or funds used by a TRUSTOR to set up a TRUST, also called the trust CORPUS. TRUSTEE: A person or entity which holds the legal title to money or property for the benefit of another person or persons for certain specified purposes. A trustee may also be a BENEFICIARY if specified in the TRUST. A trustee has the responsibility to manage the trust's resources and income for the benefit of the beneficiaries according to the terms of the trust and requirements of state law. TRUSTOR: The person who created a TRUST; also called a settlor or GRANTOR. UBEN: REEMPLOYMENT INSURANCE data. An IEVS tape exchange with the Minnesota Department of Economic Security completed monthly for enrollees and semi-monthly for applicants for federal programs. Return to top GLOSSARY: TRUST DEFINITIONS... 0902.39.01 TRUST DEFINITIONS BENEFICIARY: The person(s) designated in the TRUST as benefitting in some way from the trust, except for the TRUSTEE or other individual whose benefit consists only of reasonable fees or payments for managing or administering the trust. The beneficiary can be the GRANTOR, another person or persons, or a combination. CORPUS: Also called the TRUST PRINCIPAL, it is the income and/or resources that form the main body of the TRUST. Resources or income in the trust corpus may be available to a person but the person no longer owns them. All MA exclusions that could be applied if the resource or income were owned by the person apply when the item is owned by the trust, EXCEPT for the MA homestead exclusion. When homestead property is made a part of the trust corpus, the MA homestead property exclusion does NOT apply. GRANTOR: Also called the TRUSTOR or settlor, is the person or entity which creates or establishes the TRUST. IRREVOCABLE TRUST: One which cannot be revoked in any way after it is established by the GRANTOR or his or her representative. LEGAL INSTRUMENT OR DEVICE SIMILAR TO A TRUST: Any instrument that exhibits the general characteristics of a TRUST, but is not called a trust, is treated in the same way for MA purposes as a trust. This can include, but is not limited to, ESCROW accounts, investment accounts, PENSION funds and other similar devices managed by an individual or entity with fiduciary obligations. MEDICAID QUALIFYING TRUST (MQT): A TRUST or similar legal device established before August 11, 1993, by a person or person's spouse or legal representative under which the person is the beneficiary of all or part of the payments from the trust, and amount of the distribution is determined by a TRUSTEE who is permitted to exercise any discretion with regard to the amount to be distributed to the person. Although referred to as a Medicaid Qualifying Trust, this type of trust may cause a person to be ineligible for MA. This trust is described as a "Client-Created Trust" in §0909.21 (Trusts). PAYMENT FROM A TRUST: A payment from a TRUST includes any disbursement from the TRUST CORPUS or from income generated by the trust, including but not limited to cash and other liquid items that are easily convertible to cash, PERSONAL PROPERTY, REAL PROPERTY, or the right to use and occupy real property. PAYMENTS TO OR FOR THE BENEFIT OF A PERSON: Any payments made from the TRUST to the person of any amount, including an amount from the trust corpus or income produced by the CORPUS, that are paid directly to the person or to someone acting on the person's behalf, such as a guardian or legal representative. It also includes payments of any sort, whether from trust corpus or trust income, paid to another person or entity so that the person gets some benefit from the payment. This includes, but is not limited to: Payments for clothing or other items for the person. Payments for services the person receives. Payments for care such as medical or personal that the person receives. Payments to maintain a home. REVOCABLE TRUST: One which can be revoked, or dissolved, by the GRANTOR. A TRUST which provides that the trust can be modified or terminated by a court is considered to be a revocable trust since the grantor or his/her representative, can petition the court to terminate the trust. A trust which is called irrevocable but which terminates if some action is taken by the grantor is considered to be a revocable trust. For example, a trust may require a TRUSTEE to terminate a trust and disburse the funds to the grantor if the grantor leaves a nursing home and returns home. TRUST INSTRUMENT: A formal written document which creates a trust and contains the powers of the TRUSTEE(s) and the rights of the beneficiaries, also called a TRUST AGREEMENT. Return to top GLOSSARY: UNDERINSURED... 0902.41 UNDERINSURED: MINNESOTACARE: A person whose health insurance lacks coverage in 2 or more of the following areas: Basic hospital insurance, medical-surgical insurance, prescription drug coverage, PREVENTIVE and COMPREHENSIVE dental, coverage (with or without co-pays), or PREVENTIVE and COMPREHENSIVE vision coverage (with or without co-pays). OR Has an annual DEDUCTIBLE of $100 or more per person. OR Excludes coverage for some diagnoses. Children under 21 are also considered underinsured if their only coverage is through MEDICARE. See §0910.09 (Determining if Someone Is Underinsured). UNDOCUMENTED PEOPLE: People living in the U.S. without the knowledge or approval of the U.S. CITIZENSHIP and IMMIGRATION SERVICES (USCIS). See §0906.03.09 (Undocumented and Non-Immigrant People). UNEARNED INCOME: Income a person receives without being required to perform any labor or service. See §0911.07 (Determining if Income Is Earned or Unearned) and §0911.07.05 (Unearned Income). UNEMPLOYMENT INSURANCE: A state cash payment made to some people who have lost their jobs. This program was formerly known as REEMPLOYMENT INSURANCE in Minnesota. UNSALABLE REAL PROPERTY: Property which 2 sources who are knowledgeable about the value of the property and the local area agree cannot be sold due to a specified condition, or property which has been for sale at least 90 days at a price no more than the highest current FAIR MARKET VALUE without an offer received. Current market value means a value established within 6 months of application or since the last RECERTIFICATION. UNVI: Unverified Unearned Income. An IEVS tape exchange completed annually for recipients and monthly for applicants of federal programs. The source is the Internal Revenue Service (IRS). It reports information such as DIVIDENDS, INTEREST, and lottery winnings. VARYING INCOME: MA: For purposes of determining whether a CLIENT will use an automated or a manual monthly SPENDDOWN, varying income is any income that cannot reasonably be anticipated to be the same amount every month. For example, most earned income for non-salaried employees is varying income. Most monthly benefit payments such as Social Security are non-varying income. VERIFICATION: The process and evidence used to establish accuracy or completeness of information from an APPLICANT, ENROLLEE, third party, or AUTHORIZED REPRESENTATIVE. Require the CLIENT’s written consent to obtain verification from a third party. VETERANS' BENEFITS: Benefits and services provided by the U.S. Veterans Administration (VA) to people who have served in the U.S. armed forces and their dependents. WAGE MATCH: MA: An IEVS tape exchange with the Minnesota Department of Economic Security completed quarterly for recipients and monthly for applicants of federal programs. It provides information on wages earned in Minnesota. WAIVER: A suspension or change of a federal regulation, service limitation, or eligibility requirement. WAIVER OBLIGATION: The amount of income in excess of the MAINTENANCE NEEDS ALLOWANCE that people eligible for SIS EW must contribute toward the monthly cost of waivered services. See §0913.13.05 (Waiver Obligation--SIS EW). WIC: See WOMEN, INFANTS, AND CHILDREN NUTRITION PROGRAM (WIC). WIDOW'S AND WIDOWER'S DISREGARD: MA: A DISREGARD of UNEARNED INCOME available to some MA clients who are widows or widowers with a DISABILITY. See §0912.05.17 (Widows and Widowers Disregard). WOMEN, INFANTS, AND CHILDREN NUTRITION PROGRAM (WIC): A federal program authorized by the Child Nutrition Act of 1966 to provide nutritious food and nutrition education to low-income pregnant and postpartum women and their children. (In this instance, postpartum means up to 6 months after termination of pregnancy.) WORKER: An employee of a COUNTY AGENCY or MINNESOTACARE OPERATIONS who determines initial and continued eligibility for the HEALTH CARE PROGRAMS. WORKERS’ COMPENSATION: A state program providing payments and reimbursement of medical expenses for people injured on the job. Return to top