Wildwood Case Management Unit Intake Assessment (Social
advertisement

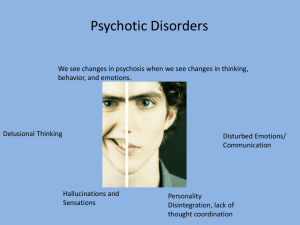
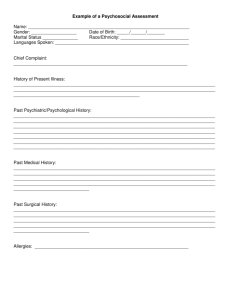
Wildwood Case Management Unit Intake Assessment (Social History) Form Client Name: Date of Birth: Date of Assessment: Presenting Problem (functional impairment, symptoms, background) Current Client Involvement with Other Agencies Agency/Person Phone Service Date Assessment of Life Circumstances or Changes in the Following Areas Family: Social: Support: Current Medications Name/Dosage: Side effects: Medication allergies: Prescribed by: Relationship Risk Factors Is client safe at home? Yes No Does client feel threatened in any way? Yes No If Yes, describe: Has client been abused in any way? Yes No If Yes, complete the following: Check all that apply: Physical Emotional Sexual Relationship of perpetrator to client: Legal action taken: Does client have a safety plan? Yes No Needs shelter? Yes No Needs protection from abuse order? Yes No 1 Client’s Legal History Suicide/Homicide Evaluation Client’s self-rating of suicide risk: 1-none 2-slight 3-moderate 4extreme/immediate Client’s self-rating of becoming violent: 1-none 2-slight 3-moderate 4extreme/immediate Client’s self-rating of homicide risk: 1-none 2-slight 3-moderate 4extreme/immediate Mental Status Exam Appearance age appropriate well groomed Orientation person place time disheveled/unkempt other situation Behavior/Eye Contact good limited avoidant none relaxed/calm slumped posture tense tics tremors Motor Activity mannerisms bizarre motor retardation restless rigid agitated catatonic behavior Manner appropriate trusting cooperative inappropriate withdrawn seductive playful evasive guarded sullen passive defensive hostile manic demanding inappropriate boundaries Speech normal incoherent pressured too detailed slurred slowed impoverished halting neologisms neurological language disturbances Mood appropriate expansive Affect broad depressed tearful irritable blunted anxious constricted 2 euphoric flat labile fatigued excited angry anhedonic Sleep good fair poor terminal insomnia Appetite good fair poor increased decreased initial insomnia increased decreased weight gain middle insomnia weight loss Thought Process logical and well organized illogical flight of ideas circumstantial loose associations rambling obsessive blocking tangential spontaneous perseverative distractible Thought Content delusions paranoid delusions distortions thought withdrawal thought insertion thought broadcast magical thinking somatic delusions ideas of reference delusional guilt grandiose delusions nihilistic delusions ideas of inference Perceptions/Hallucinations illusions hallucinations depersonalization derealization Suicide Risk none slight plan (describe: moderate ) significant extreme no plan Violence risk none slight plan (describe: moderate ) significant extreme no plan Judgment intact age appropriate severe impulsive Insight intact limited very limited fair understands personal role in problems Sensorium alert drowsy stupor above average none obtundation Memory intact impaired immediate recall amnesia (type of amnesia: ) Intelligence average immature impaired remote 3 moderate aware of current disorder coma below average mild unable to establish Interviewer Summary of Findings (add details where appropriate) Substance Use/Abuse Type Amount Used How Taken Duration Frequency Tobacco Alcohol Illicit Drugs Prescription Drugs OTC Drugs Other Experiencing Withdrawal Blackouts Hallucinations Vomiting Severe Depression DTs and Shaking Seizures Other Yes Yes Yes Yes Yes Yes Yes Yes No No No No No No No No If yes, describe: Patterns of Use Uses more under stress Continues use when others have stopped Has lied about consumption Has tried to avoid others while using Has been drunk/high for several days at a time Neglects obligations when using Usually uses more than intended Needs to increase use to become intoxicated Has tried to hide consumption Sometimes uses before noon Cannot limit use once begun Failed to keep promises to reduce use Yes Yes Yes Yes Yes Yes Describe attempts to stop: 4 Yes No No No Yes Yes Yes No Yes No No Yes No No No No No No Date of last use Describe circumstances that usually lead to relapse: Is client involved in AA/NA? Yes No Client Requests, Goals, Expectations Clinical Summary (Pull together information you have collected and summarize, identifying possible relationships, conditions, and causes that may have lead to current situation.) Impressions Recommendations Diagnostic Impression Axis I: Axis II: Axis III: Axis IV: Axis V: Case Manager Signature: Date: 5