Glycogen Storage Disease – A Professional Refresher
advertisement

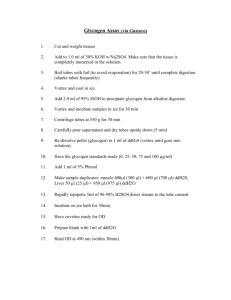
Glycogen Storage Disease Glycogen storage disease is a genetically inherited disease caused by an absence or deficiency of one of the enzymes responsible for making or breaking down glycogen in the body. This may affect the liver, muscles, heart, kidneys, and/or the blood cells. Many different forms of glycogen storage disease exist. Signs and symptoms of glycogen storage disease Type I glycogen storage disease This is the most common form of glycogen storage disease. Von Gierke disease often presents with: – Sweating – Irritability – Mouth ulcers – Infection – Muscle weakness – Hypoglycemia – Enlarged liver – Stunted growth Patients with type Ib can suffer from: – Platelet dysfunction – Inflammatory bowel disease – Hyperlipidemia – Renal insufficiency – Gout – Severe neutropenia Hypoglycemic complications, sometimes severe or lethal, can occur Type II glycogen storage disease (Pompe’s disease) The following are signs and symptoms of type II glycogen storage disease: Usually causes muscle weakness and respiratory issues (patients often need a ventilator) Heart failure may result Scoliosis is common An enlarged tongue is common Weak throat muscles are common Type III glycogen storage disease (Cori disease) The following are signs and symptoms of type III glycogen storage disease: Swollen stomach from an enlarged liver Low fasting blood sugars Growth delay Muscle weakness Type IV glycogen storage disease (Anderson’s disease) The following occur with type IV glycogen storage disease: Most children die before 2 years of age from: – Cirrhosis of the liver – Cardiac failure Type V glycogen storage disease (McArdle’s disease) Causes: – Muscle pain with normal activity – Muscle weakness – Fatigue Type VI glycogen storage disease (Hers’ Disease) The following are signs and symptoms of type VI glycogen storage disease: A very mild form causes liver enlargement in childhood Decreased alanine levels and ketosis can occur Type VII glycogen storage disease (Tarui disease) The following are signs and symptoms of type VII glycogen storage disease: Muscle pain and weakness Kidney damage possible with strenuous activity Nutrition therapy for glycogen storage disease Type I glycogen storage disease Limit foods containing sucrose, fructose, lactose, or galactose Recommend frequent, high-starch feedings Night tube feedings often are necessary to prevent hypoglycemia Watch energy intake to prevent obesity and/or hypertriacylglycerolemia 10% to 15% of total calories should come from protein 25% to 35% of total calories should come from fat (less if obesity becomes an issue) Recommend that patients consume complex carbohydrates and avoid refined carbohydrates Children older than 2 to 3 years of age should receive 1.25 to 2.5 grams/kilogram body weight of raw cornstarch between meals to prevent hypoglycemia (mix in water or soy formula/milk) Increase amount of carbohydrate by 10% to 15% and decrease fat by equal amount during times of hypoglycemia Iron supplementation often is necessary Restrict the following foods for people with glycogen storage disease: – All fruits except avocados, lemons, rhubarb, gooseberries, loganberries, blackberries, cranberries, currants, pomegranates, or limes – Beer – Brandy – Carob powder – Chile sauces – Fructose – Fruit juice – High-fructose corn syrup – Honey – Jams, jellies, and preserves – Ketchup – Liquor – Maple syrup – Milk – Milk products – Molasses – Rum – Sherry – Sorbitol – Sugar – Vermouth – Vodka Type II glycogen storage disease People with type II glycogen storage disease often have trouble with the mechanics of eating and may require tube feeding Sometimes a high-protein, low-carbohydrate diet is recommended Sometimes alanine supplementation is recommended Type III glycogen storage disease Some research shows that cornstarch therapy also is effective in Type III glycogen storage disease Sometimes a high-protein, low-carbohydrate diet is recommended (generally 45% carbohydrate, 25% protein, and 30% fat) Recommend low-fat milk with whey protein powder Discourage sweets Type V glycogen storage disease Sometimes a diet that is moderately high in protein is helpful Some patients benefit from B6 supplements Types VI and VII glycogen storage disease Sometimes a high-protein, low-carbohydrate diet is recommended (generally 45% carbohydrate, 25% protein, and 30% fat) Recommend low-fat milk with whey protein powder Discourage sweets References and recommended resources Anderson WE. Type IV glycogen storage disease. Medscape Reference Web site. http://www.emedicine.com/med/topic910.htm. Accessed April 16, 2013. PompeConnections: Common Health Concerns. Baarn, Netherlands: International Pompe Association; 2005. http://www.worldpompe.org/pompe-disease/publications/category/2english. Accessed April 16, 2013. PompeConnections: Nutrition and Dietary Therapy. Baarn, Netherlands: International Pompe Association; 2005. http://www.worldpompe.org/pompedisease/publications/category/2-english. Accessed April 16, 2013. Roth KR. Genetics of glycogen-storage disease type I. Medscape Reference Web site. http://www.emedicine.com/PED/topic2416.htm. Accessed April 16, 2013. Review Date 4/13 K-0589