Disturbances of the Parathyroid
advertisement

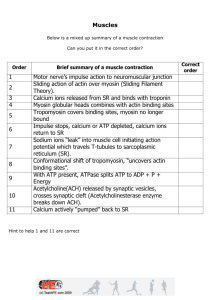
Disturbances of the Parathyroid Ann MacLeod, RN, BScN, MPH Objectives Review anatomy and physiology of Parathyroid gland Understand Hyper and Hypoparathyroid • assessment findings • nursing diagnoses • management Physiology Parathyroid Glands Hyperparathyroidism Overactivity of one of the parathyroid gland classified as primary or secondary 90% caused by adenoma 8% by hyperplasia or hypertrophy 2% by carcinoma Physiology Normal function of PTH is to control and increase bone resorption of calcium, therefor maintain ca+ and phos. Ions within the bloodstream Assessment: excessive blood calcium causes: Hyperparathyroidism Bone damage muscles become hypotonic fatigue, muscle weakness cardiac muscle may be affected with arrhythmias Back ache, joint pain fractures, deformities n/v, constipation large amts. Of calcium passing through the kidneys may cause kidney stones Collaborative Treatment Primary: always treated surgically (1/2 of one gland is sufficient to sustain the body secondary: managed by correcting the cause Para-thyroidectomy Pre-op: while ct. awaits surgery: push fluids to > 3000mls/day, cranberry and prune juice prevents stone formation and decreases infection low Ca+ diet; no milk or milk products prevent constipation; increase activity, stool softeners, laxatives Parathyroidectomy Pre-op care cont’d Strain all urine; observe for hematuria and renal colic protect from injury d/t path. #s Phosphate or Sodium Phytate(Rencal) this drug decreases absorption of calcium in the gut calcitonin: decreases serum calcium Post-operative Care: Immed. Post.op observe for hemorrhage and airway obstruction watch for serious decrease in blood calcium which will produce tetany Tetany could be so severe and lead to muscle twitching and seizures Rx. IV calcium gluconate Hungry Bone Syndrome: Post-op Parathyroidectomy cont’d May need to increase calcium in the diet post. Op calcium gluconate injections Oral calcium preparations Hypoparathyroidism Hyposecretion of PTH causes decreased blood calcium, and increased serum phosphorus leads to pronounced neuromuscular irritability Causes Accidental removal of parathyroid gland auto immune destruction congenital absence of the glands Assessment: caused by low serum calcium levels Tetany numbness and tingling of fingers painful muscle spasms chvostek’s sign: hyperirrritability of facial nerve Trousseau’s sign: carpal spasm of fingers and hand after pressure cuff deflated laryngeal spasm may also occur>>dyspnea severe : can affect cardiac muscle>heart failure Hypoparathyroidism - Assessment Cont’d Chronic: lethargy, brittle nails, constipation, loss of tooth enamel, muscle pains diagnosis is made based on the presence of Chvostek’s and Trousseau’s sign and also decreased calcium Collaborative Management Acute: can be life threatening; goals: increase calcium rapidly, prevent and or treat possible convulsions, and control laryngeal spasms and possible resp. obstruction Management 10% calcium gluconate by IV Trach set and ET tube while emergency in progress oral Calcium and Vit. D Diet: Increase ca+, calcium supplements Lifelong medication and follow-up blood work full recovery if diagnosed early