health
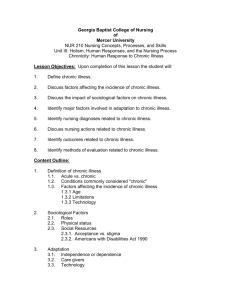
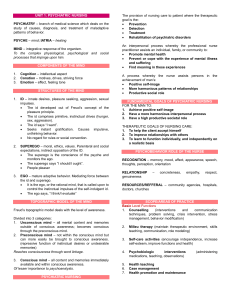
advertisement

Health Models of Health (classifications of health definitions) • Clinical Model: health = absence of S/S of disease/disability; medically orientated • Role Performance Model: health viewed in terms of performance of social roles; health = effective performance of roles • Adaptive Model: Health = maintaining flexible adaptation to environment and interacting with it to maximum advantage • Eudaimonistic model: Health seen as exuberant well-being; healthy person is self-actualized and fulfilled. 1 Definitions of Health WHO • Complete physical, mental, social well-being; not merely absence of disease/infirmity Pender • The actualization of inherent and acquired human potential through goal-directed behavior, competent self-care, and satisfying relationships with others, while adjustments are made as needed to maintain structural integrity and harmony with relevant environments Bevis • The ability to set goals and to mobilize the energy and resources needed to meet these goals while feeling good and caring about self and others and helping others feel good about themselves U of W • A dynamic process whereby client is able to realize aspirations, satisfy needs, and change/cope with environment • A resource for everyday life • A positive concept emphasizing social and personal resources as well as physical capacity • The goal of all nursing behaviors 2 Alterations in Health Acute/Episodic Illness • Rapid onset, short duration • Self-limiting or responds to Rx Long term/Chronic Illness • Permanent • Irreversible pathologic conditions • Residual disability Disease versus Illness • Disease: objective state of ill health; manifested by pathology detectable by medicine • Illness: subjective experience of loss of health 3 Impact of Long term Illness of the Individual and Family Physiologic/Somatic Psychologic Sexual Social Occupational Financial 4 Alterations in Health: Role of the Nurse (Bevis) Nursing • A process • Purpose - promote optimal health; facilitate maturation and adaptation in clients (individuals [intrapersonal], groups [interpersonal] & community) Input • Needs, goals, problems, desires of clients • Includes assessment data Throughput • Act/practice of nursing • Theories, concepts, processes used • Tools used: • Problem-solving/decision-making (critical thinking) • Caring • Teaching Learning (educator) • Communication • Management/change (change agent) Output 5 • The behaviors, services, functions, skills of nursing 6 Life Task Concepts (Bevis) Stress - forces that press in upon or noxiously stimulate the individual. e.g. health problems, medical diagnoses, social problems Strain - expresses itself in symptoms, signs or behaviors that signal response to stress. E.g., S/S of an illness; physical assessment findings, behaviors (crying) Maturation - process of human development Adaptation/Maladaptation - coping patterns or ways of behaving that can head to an interruption or maintenance of health 7 Review of Nursing Process Assessment • Data collection. Sources: - client - family/significant others - records - collaboration - other health care professionals. • Formulate nursing judgements - data clustering: organize into meaningful clusters (e.g., physiological systems, Gordon’s functional health patterns) Analysis Analyze & interpret data, draw conclusions re health risks/problems; requires critical thinking • Nursing Diagnosis • a clinical judgement about a response to actual/potential health problems/life processes • Nurse is accountable/responsible • Collaborative problems - potential health problems for which the nurse monitors; requires collaboration with physicians. 8 Planning • Set priorities • Establish outcomes (collaborate with client) • client-centered • realistic • specific and measurable • Select nursing interventions - individualized for the client Implementation • Carry out the plan of care Evaluation • Determine the degree to which expected outcomes were met • Essentially a re-assessment of the client in relation to the goals 9