Health&Illness
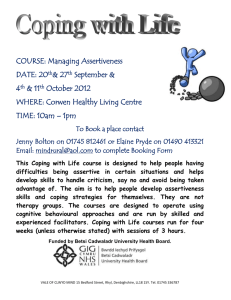
advertisement

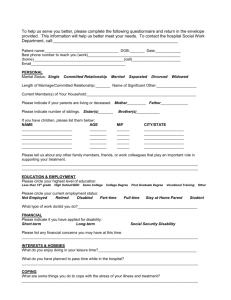
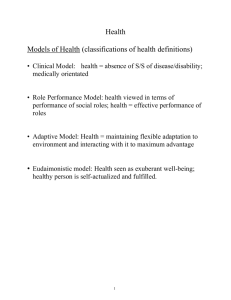
Health, Illness, & Nursing 1 Health What does health mean to be healthy? Has your perception of the meaning of health changed since you began nursing? Can health and illness co-exist? 2 Health Model • Clinical Model: – Health = absence of S/S of disease/disability – Medically orientated • Role Performance Model: – Health viewed in terms of performance of social roles – Health = effective performance of roles • Adaptive Model: – Health = maintaining flexible adaptation to environment and interacting with it to maximum advantage • Eudaimonistic model: – Health seen as exuberant well-being – Healthy person is self-actualized and fulfilled. 3 Health defined • WHO – Complete physical, mental, social well-being; not merely absence of disease/infirmity • Pender – The actualization of inherent and acquired human potential through goal-directed behavior, competent self-care, and satisfying relationships with others, while adjustments are made as needed to maintain structural integrity and harmony with relevant environments • Bevis – The ability to set goals and to mobilize the energy and resources needed to meet these goals while feeling good and caring about self and others and helping others feel good about themselves 4 Health defined • U of W – A dynamic process whereby client is able to realize aspirations, satisfy needs, and change/cope with environment – A resource for everyday life – A positive concept emphasizing social and personal resources as well as physical capacity – The goal of all nursing behaviors 5 Alterations in Health • Acute/Episodic Illness – Rapid onset, short duration – Self-limiting or responds to Rx • Long term/Chronic Illness – Permanent – Irreversible pathologic conditions – Residual disability 6 Disease versus Illness • Disease: – Objective state of ill health manifested by pathology detectable by medicine • Illness: – subjective experience of loss of health 7 Impact of Long Term Illness • Physiologic/Somatic • Psychologic • Sexual • Social • Occupational • Financial 8 Coping with Chronic Illness • Nursing role: Facilitate achievement of coping tasks • Coping Tasks: – Maintaining sense of normalcy – Modifying daily routine, adjusting lifestyle – Obtaining knowledge and skill for self care – Maintaining positive self-concept – Adjusting to altered social relationships 9 Coping with Chronic Illness • Coping Tasks (cont) – – – – – – – Grieving over losses associated with chronic illness Dealing with role change Handling physical discomfort Confronting inevitability of death (make most of life) Dealing with social stigma of illness/disability Maintaining sense of being in control Maintaining hope despite uncertain or downward course of health 10 Family Caregivers • Family Caregivers – 21% of caregivers are > 75 yrs – Caregivers of elderly with long-term illness usually: • • • • Spouses Children (usually daughters, daughters-in-law) Other family members Outside sources (when needs exceed family resources) 11 Types of Caregivers • Care Providers – perform direct care • Care Managers – manage/arrange services to provided by others – Often have own careers – Often provide psychosocial support, transportation, visiting, etc. 12 Impact of Long Term Illness on Families • Burden – Decreased social, recreational involvement, financial difficulties, depression, declining personal health – May lead to nursing home placement • Problems related to home care – Financial – Competing demands 13 Impact of Long Term Illness on Families • Physical Strain – Lifting, 24/7 physical care, sleep deprivation, chronic fatigue • Emotional Strain – High incidence of stress-related disorders (HTN, heart disease) – Manifested as anxiety, anger, guilt, loss of self – Could lead to elder abuse 14 Impact of Long Term Illness on Families • Role Changes Associated with Caregiving – Pre-existing relationships change – Take on new duties – Role Ambiguity • Taking on of new roles (e;g. roles traditionally fulfilled by spouse) – Role Reversal • Children caring for parents 15 Nursing Interventions for Family Caregivers • Encourage verbalization and acceptance of negative emotions • Facilitate Realistic expectations re – client’s illness and expected course – Own limitations – Common feelings • Encourage to accept assistance from others • Info about resources (support groups, respite services) 16 Lazarus’ Theory of Stress and Coping Pschological Stress Cognitive Appraisal Coping Health Outcome 17 Lazarus’ Theory of Stress and Coping • Stress – Relationship b/w person and environment that is appraised by the person as • Taxing or exceeding his/her resources • Endangering his/her well-being 18 Lazarus’ Theory of Stress and Coping • Cognitive Appraisal – Process through which person evaluates whether a particular encounter with the environment is relevant to his/her well-being and if so, in what way(s) – i.e., evaluation of the significance or meaning of an event to the individual 19 Lazarus’ Theory of Stress and Coping • Two Types of Cognitive Appraisal – Primary Appraisal • Person evaluates whether he/she has anything at stake (i.e., is there potential harm or benefit?). • Evaluates significance of the “event” with respect to well-being • Types of appraisal: – Stressful – harm, loss, threat – Challenge – opportunity for growth, gain or mastery 20 Lazarus’ Theory of Stress and Coping – Secondary Appraisal • Evaluates what if anything can be done to overcome or prevent harm or to improve the prospects of benefit (ie., evaluates coping resources and options) • Various coping options (e.g., altering the situation, accepting it, seeking information) are evaluated 21 Lazarus’ Theory of Stress and Coping • Coping – Person’s constantly changing cognitive and behavioral efforts to manage specific external and/or internal demand that are appraised as taxing or exceeding the person’s resources – i.e., efforts to master the demands 22 Lazarus’ Theory of Stress and Coping • Two major types of coping strategies – Emotion-focused coping • Used to control distressing emotions, sometimes by altering the meaning of an outcome • Likely to be used in situations that are perceived not be not amenable to change – Problem-focused coping • Used to control the troubles person-environment relationship through problem-solving, decision-making and/or direct action • More likely to be used in situations perceived as changeable 23 Alterations in Health: Role of the Nurse (Bevis) • Nursing – A process – Purpose - promote optimal health; facilitate maturation and adaptation in clients (individuals [intrapersonal], groups [interpersonal] & community) 24 Nursing System (Bevis) • Input – Needs, goals problems & desires of clients – Includes assessment data 25 Nursing System (Bevis) • Throughput – Theories, concepts, processes used – Tools used • Problems-solving/decision-making (critical thinking) • Caring • Teaching/Learning (Educator) • Communication • Management/change (change agent) 26 Nursing System (Bevis) • Output – Behaviors, services, roles, functions of nurses 27 Life Tasks (Bevis) • Stress – Forces that press in upon or noxiously stimulate the individual. e.g. health problems, medical diagnoses, social problems • Strain – Expresses itself in symptoms, signs or behaviors that signal response to stress. E.g., S/S of an illness; physical assessment findings, behaviors (crying) • Maturation – Process of human development • Adaptation/Maladaptation – Coping patterns or ways of behaving that can head to an interruption or maintenance of health 28 Review of Nursing Process Assessment – Data collection • Sources – Client – Family/significant others – Records – Collaboration (other health professionals) – Formulate nursing judgements Data clustering: organize into meaningful clusters (e.g., physiological systems, Gordon’s functional health patterns) • 29 Review of Nursing Process • Analysis – Analyze and interpret data: draw conclusions re health risks/problems – Nursing Diagnosis • A clinical judgement about a response to actual potential health problems/life processes • Nurse is accountable/responsible for developing and treating – Collaborative Problem – potential problem for which nurse monitors; requires collaboration with MDs 30 Review of Nursing Process • Planning – Sets priorities – Establishes outcomes/goals (collaborate with client) • client-centered • Realistic • specific and measurable – Select nursing interventions - individualized for the client • Implementation – Carry out the plan of care • Evaluation – Determine the degree to which expected outcomes were met – Essentially a re-assessment of the client in relation to the goals 31