Question - LCCC-LPN
advertisement

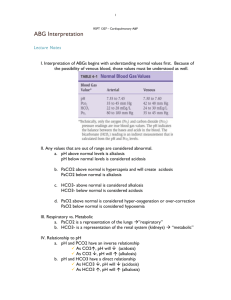
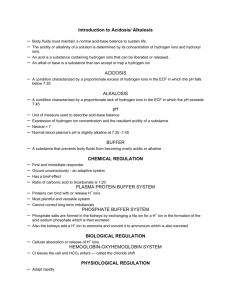
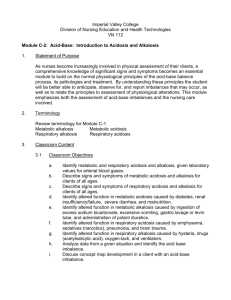
Electrolytes and Acid-Base Balance Question Answer ANSWER Note/Hint 1. Clinical manifestations of respiratory alkalosis 1. N/V, tingling of fingers, excitatory symptoms. 1. Patients likely to get metabolic acidosis. 2. Reasons for metabolic acidosis 1. Kidney patients, C. Diff patients lose too much bicarb from diarrhea. 2. Kidneys are not escreting enough hydrogen produced by anaerobic metabolism; losing too much HCO3 by GI tract; drug overdose. 1. Physiologic buffers(4) 1. Lungs 2. second line of defense 3. twice as effective as chemical buffers because can handle twice the amount of acid and bases. 4. responds quickly but can restore only temporarily. 1. Respiratory acidosis means the patient is 2. Some of the common causes of the retention of carbon dioxide (respiratory acidosis) are 1. retaining CO2 2. Pneumonia, drug overdose, pulmonary edema, pneumothorax. (Less surface area, decreased respiratory rate, fluid in lungs) 1. CO2 1. respiratory alkalosis is not enough 2. Pain, fever, asthma, congestive heart 2. Some of the common causes of respiratory failure, anxiety/fear, pulmonary alkalosis (6) embolus. 3. first sign of pulmonary embolus is 3. tachypnea 1. Respiratory control center is in the__. 2. Long term adjustments of pH are accomplished by the __. Takes how long to work? 3. Bicarb can be excreted in 1. medulla 2. kidneys up to 4 days 3.urine 1. The major diagnostic tool for evaluating acid-base balance and oxygenation. 2. the purpose of ABG is to show how 1. ABG's 2. effectively the lungs are delivering oxygen to the blood, how efficiently they are eliminating carbon dioxide, and how well the lungs and kidneys are interacting to maintain normal blood pH (acid base balance). 1st step to blood gas interpretation look at pH and determin a/b status 60% of the body's weight is made up of what? water Water A client has been taking extra lasix for “bloating”. The acid base imbalance is? Metabolic alkalosis A pt. is in pain and is anxious from an accident. The acid base imbalance is? Respiratory alkalosis ABG Normal Values: 1. pH 2. PaO2 3. PaCO2 4. HCO35. SaO2 6. critical range of pH 1. 2. 3. 4. 5. 6. Acid A substance that can donate H+ Acidosis •< 7.35 •H+ Excess •HCO3 Deficit Alkalosis •> 7.45 •H+ Deficit •HCO3 Excess At an age, a PaO2 lower than 40 is ? life-threatening and requires immediate action. Base A substance that can accept H+ Bicarb is a product of what body system? The kidneys Bicarbonate-Carbonic Acid Buffering system •Most important ECF buffering system •HCO3 + H+ => H2CO3 => H20 + CO2 breathe out Buffering anions HCO3 major also hemoglobin, phosphate, and proteins Carbonic Acid (H2CO3) Unable to measure directly Dissolves in plasma to form CO2 +H20 eliminated by lungs Use co2 to measure acid component Causes of Metabolic Acidosis Cardiac Arrest, Shock, Diabetic Ketoacidosis, Fasting/starvation/malnutrition, Ketogenic diet, Aspirin Toxicity, Renal Failure, Severe Diarrhea, Hyperchloremia Causes of Metabolic Alkalosis Excess NaHCO3 intake, prolonged vomiting/bingeing/purging, GI suction, Diuretics, Hyperaldosteronism, Renal Failure Causes of Metabolic Alkalosis have what in common? they increase the bicarb or volume concentration of bicarb is high (too much bicarb), it causes pH level to rise making it alkalotic/losis Causes of Respiratory Acidosis HYPOVENTILATION: COPD, Drug overdose, Head injury, respiratory muscle disorders Causes of Respiratory Acidosis (3) 1. CNS depression from drugs, injury, or disease 2. Asphyxia (airway obstruction) 3. Hypoventilation related to a disease 7.35-7.45 80-100 mmHg 35-45 mmHg 22-26 mEq/L 97-100% (also known as SAT) below 7.20 or above 7.55 Causes of Respiratory Alkalosis HYPERVENTILATION: Panic attacks, hypoxia, Fever, Saliclate Toxicity, Mechanical Ventilation Clinical Manifestations of metabolic acidosis (5) 1. hyperkalemia; shift of acid to ICF and K+ to the ECF 2. anorexia, n/v 3. warm, flushed skin 4. cardiac dysrhythmias & CNS dysfunction (somnolence, decreased LOC) 5. h/a, diarrhea, tremors Clinical manifestations of metabolic alkalosis (5) cardia dysrhythmias seizures confusion muscle twitching agitation Clinical manifestations of respiratory acidosis (6) vasodilation cardiac dysrhythmias, tachycardia, somnolence decreased ventilation, decreased level of consciousness. Clinical manifestations or signs of respiratory acidosis Drowsiness, unconsciousness, disorientation, rapid, shallow respirations, tachycardia, dizziness, decreased BP, headache, Tachycardia, seizures clinical manisfestations of Metabolic acidosis drowsiness, coma, dehydration, n/v, diarrhea, headache,MOST COMMON is muscular twitching and deep rapid respirations (Kussmaul's breathing) clinical manisfestations of metabolic alkalosis belligerence, irritable, disorientated, lethargy, shallow slow respirations, periods of apnea, tachycardia, dysrhythmias, n/v, hypertonic muscles, tingling of fingers and toes, seizures Clinical manisfestations or signs of respiratory acidosis Drowsiness, unconsciousness, disorientation, rapid, shallow respirations, tachycardia, dizziness, decreased BP, headache, Tachycardia, seizures increased neuromuscular irritability, hyperreflexia, muscular twitching, clinical manisfestations or signs of respiratory seizures, lightheadedness,numbness and alkalosis are tingling in toes and fingers, tachycardia, dysrhythmias. CO2 used to express Carbonic acid Although CO2 is not an acid (has no H+ to donate), but because of its relationship with H2CO3, it is referred to as an acid common cause of Respiratory acidosis *abnormalities in pulmonary ventilation leading to CO2 retention. *Halted or hindered gas exchange *Obstructions preventing exhalation of CO2 *Impaired neuromuscular function or integerity of chest wall *Depressed Respiratory center in medullat common cause of Respiratory acidosis *abnormalities in pulmonary ventilation leading to CO2 retention. *Halted or hindered gas exchange *Obsructions preventing exhalation of CO2 *Impaired neuromuscular function or integerity of chest wall *Depressed Respiratory center in medullat Common Causes Increased acid loss or excretion vomiting, gastric suction, hypokalemia Common Causes Increased acid production - lactic acidosis, ketoacidosis Common causes of metabolic alkalosis excessive loss of hydrogen ions from body through vomiting and gastric suction w/o replacement of alkali Compensatory mechanisms of metabolic alkalosis hypoventilation (to keep some of the CO2), hydrogen ions are conserved and large amounts of sodium and potassium are excreted by the kidneys Compensatory Mechanisms of Respiratory alkalosis *Respirations decrease or even cease until CO2 levels rise enough to stimulate increase in respirations. *Kidneys slow absorption of HCO3 and increase release of hydrogen ions causing alkaline urine Compensatory mechanisms that take place within 24 hours of Respiratory Acidosis Kidneys conserve HCO3 and excrete more hydrogen ions into urine Urine becomes more acidotic Compensatory mechanisms that take place within 24 hours of Respiratory Acidosis Kidneys conserve HCO3 and excrete more hydrogen ions into urine Urine becomes more acidotic condition in which acid accumulates in the body Acidosis condition in which base substances accumulate in the body Alkalosis Definitions: 1. Acidosis (or acidemia) 2. Alkalosis (or alkalemia) 3. A primary RESPIRATORY problem is determined if 4. A primary metabolic problem is when 1. occurs when pH drops below 7.35 (causing CNS depression) 2. occurs when the pH rises above 7.45 (causing CNS excitation). 3. the PaCO2 is less than 35 mmHg (alkalosis) or greater than 45 mmHg (acidosis) 4. the HCO3 is less than 22mEq/L (acidosis) or greater than 26mEq/L (alkalosis) Diabetic/starvation/alcoholicKetoacidosis, Poisoning, lactic acidosis, renal failure, and diarrhea are causes of? Metabolic Acidosis Drainage of pancreatic juice, ureterosigmoidoscopy, obstructed ileal loop, acetazolamide(diamox), ammonium chloride, renal tubular acidosis are causes of? Metabolic Acidosis Edema Excess fluid in the interstitial space and/or body cavities Elevated osmolarity is indicative of what? Increased solute (sodium) and decreased fluid (water) Etiology of Respiratory acidosis ARDS, Pneumonia, Atelectasis, COPD, emphysema, asthma, bronchial burns, chest trauma, GuillainBarre, MS, Mysathenia gravi, Drug overdoses, anesthesia, acute alcoholism. Etiology of Respiratory acidosis ARDS, Pneumonia, Atelectasis, COPD, emphysema, asthma, bronchial burns, chest trauma, GuillainBarre, MS, Mysathenia gravi, Drug overdoses, anesthesia, acute alcoholism. Exchange between H+ & K+ Buffering System •Acidosis => H+ moves into ICF K+ moves into ECF •Alkalosis => H+ moves into ECF K+ moves into ICF HCO3- Bicarbonate (4) 1. normal is 22-26 mEq/L 2. Major Base 3. Reflects the activity of the kidneys in retaining or excreting bicarb. 4. Accomplished by kidneys conserving or excreting Hydrogen and hydrogen bicarbonate. How can we improve respiratory function? antibiotics for infection, postural drainage, bronchodilators, inhalation therapy, breathing exercises, mechanical ventilation, oxygen therapy. How can we improve respiratory function? antibiotics for infection, postural drainage, bronchodilators, inhalation therapy, breathing exercises, mechanical ventilation, oxygen therapy. How is fluid balance regulated? By regulating intake (thirst) and output (kidneys) How is PaO2 for an elderly person calculated? Starting at 60 years, begin at 80mmHg, then for each year over 60, add 1mmHg Hyperventilation can be caused by 1._____________ anxiety, aftermath of severe exercise and hypoxia at 2.____________ high altitudes 3.____________ Imbalances are classified as being respiratory or metabolic ____________ or ____________. Imbalances are classified as being respiratory or metabolic ____________ or ____________. Increased osmolarity of the plasma activates what? Neural pathways that result in the conscious perception of thirst. Interpret the ABG: ph 7.25, pCo2 54, HCO3 24, pO2 84 Respiratory acidosis Interpret the ABG: ph 7.50, pCo2 28, HCO3 24, pO2 70 Respiratory Alkalosis Interventions for Respiratory acidosis Improve respiratory function, correct acidosis, assess for iatrogenic complications of interventions Kidney Regulation of pH Retain or excrete HCO3 or H+ as needed Kidneys compensate slowly but provide complete compensation Acidosis (↓ pH) •Retain HCO3 or Excrete H+ Alkalosis (↑ pH) •Excrete HCO3 or Retain H+ Metabolic Acidosis pH &lt; 7.35 Metabolic Acidosis ↓Bicarbonate (HCO3) <21 mEq/L ↓pH Resp. Comp: Hyperventalation to ↓ PCO2 Renal Comp: if no renal disease, ↑ H+ excretion and ↑ HCO3 Reabsorption -BE Metabolic Acidosis pH < 7.35 HCO3 <22 mEq/L Metabolic Acidosis Bicarbonate or HCO3 loss with acid retention Metabolic Acidosis Common Causes Increased acid production - lactic acidosis, ketoacidosis Decreased acid excretion - renal failure Increased Bicarb loss - Diarrhea, ileosomy drainage, intestinal biliary or pancreatic fistulas Increased Chloride - sodium chloride IV solutions, renal tubular acidosis, carbonic anhydrase inhibitors Metabolic acidosis cause excess acids Metabolic acidosis cause excess acids bicarb deficiency Metabolic acidosis compensation rate and depth of respirations increase, eliminating additional CO2 Metabolic acidosis compensation rate and depth of respirations increase, eliminating additional CO2 Metabolic acidosis effect on ABGs decrease pH decrease HCO3 decrease PaCO2 Metabolic Alkalosis pH > 7.45 HCO3 > 26 mEq/L Metabolic Alkalosis ↑HCO3 >28 mEq/L ↑pH Resp. Comp: Hypoventalation to ↑PCO2 Renal Comp: If no renal disease ↓H+ excretion and ↓ HCO3 reabsorption + BE Metabolic Alkalosis HCO3 retention and acid loss Metabolic Alkalosis Common Causes Increased acid loss or excretion - vomiting, gastric suction, hypokalemia Increased Bicarb - Alkali ingestion (bicarbonate of soda), excess bicarb administration Metabolic alkalosis cause bicarb excess Metabolic Alkalosis common causes (2) 1. Gain of base: increased ingestion of antacids or an excessive administration of sodium bicarb 2. Loss of metabolic acids: vomiting, nasogastric suctioning diuretics (loss of hydrogen) Metabolic alkalosis compensation rate and depth of respirations decrease, retaining CO2 Metabolic alkalosis effect on ABGs increase pH increase HCO3 increase PaCO2 Metabolic imbalances affet the base ____________. bicarbonate Metabolic imbalances affet the base ____________. bicarbonate mild hypoxemia 60-80 mm Hg PO2 Mod. Hypoxemia PO2: 45-60 mm Hg Most common cause of metabolic acidosis? overproduction of metabolically produced acids found in diabetes mellitus, Infections with high fever, trauma, and major surgery. Noncompensation pH is abnormal PCO2 or HCO3 OR Abnormal Normal Acid-base balance is 1:20 Normal Acid-base balance is 1:20 Normal adult PaO2 is? and for an infant? 80-100; 40-70 Normal range for pH 7.35 - 7.45 Normal valuses for HCO3 20-30mmHg Normal valuses for HCO3 20-30mmHg Normal valuses for O2 saturation is 96-100% Normal valuses for O2 saturation is 96-100% Normal valuses for pCO2 35-45 mmHg Normal valuses for pCO2 35-45 mmHg Normal valuses for pH 7.35-7.45 Normal valuses for pH 7.35-7.45 Normal valuses for pO2 80-100 mmHg Normal valuses for pO2 80-100 mmHg Nursing intervention for metabolic alkalosis treat primary condition, correct alkalosis, correct water sodium, chloride and potassium deficits. Nursing interventions for metabolic acidosis restore blood volume and osmolarity Correct HCO3 deficit assess for and prevent electrolyte imbalances (Hyperkalemia) and protect from injury. Osmolarity Total solute concentration in a solution- osmoles/liter Osmosis Net movement of water through a selectively permeable membrane that seperates two solutions with different solute concentrations. other causes of Metabolic acidosis excessive ingestion of acid (aspirin, ferrous sulfate), Renal diseases( kidneys lose ability to secrete acids), abnormal loses of alkali (acute vomiting, loss of pancreatic, biliary and lower intestinal fluids PaCo2 (3) 4. Normal CO2 is 1. refers to the partial pressure of CO2 in arterial blood. 2.Indicates the effectiveness of ventilation (how well the lungs are blowing off caronic acid) 3. Provides the info about the respiratory component of acid-base balance 4. 35-45mmHG PaO2 (Anearobic Metabolism)(4) 1. Gives information about patient's oxygenation level. 2. Used to identify hypoxemia. 3. Anaerobic Metabolism 4. Normal PaO2 is 80-100 mmHg PaO2 measures? the partial pressure of oxygen dissolved in arterial plasma. Partial Compensation pH is abnormal both PCO2 AND HCO3 are abnormal PCO2 In acid-base terminology, CO2 is expressed as PCO2 P = Partial Pressure Refers to the pressure / tension exerted by this gas in blood Partial Pressure = because CO2 is only one of several gases contributing to the total pressure (Oxygen, Nitrogen & Other Gases pH down acidosis pH indicates the number of Hydrogen Ions H+ pH ratio and what is it determined by? •Determined by ratio of bicarb & carbonic acid •pH maintained by a ratio of 20:1 (bicarb:CA) pH Up Alkalosis Possible causes of Metabolic Acidosis (3) 1. Bicarbonate depletion from diarrhea 2. Excess production of organic acids from hepatic disease, endocrine disorders, shock, or drug intoxication 3. Inadequate excretion of acids from renal disease Possible causes of Metabolic Alkalosis (3) 1. Loss of hydrochloric acid from prolonged vomiting or gastric suctioning 2. Loss of potassium from increased renal excretion (as in diuretic therapy) or steroids 3. Excessive alkali ingestion Possible causes of Respiratory Alkalosis (3) 1. Hyperventilation from anxiety, pain, or improper ventilator settings 2. Respiratory stimulation due to drugs, disease, hypoxia, or fever 3. Gram negative bacteremia Primary Disturbance match between pH and PCO2 Respiratory system causing primary disturbance Primary Disturbance: Match between pH and HCO3 Metabolic system causing primary disturbance Respiratory Acidosis * Excess carbon dioxide retention * patient is <7.35pH * increase in carbonic acid Respiratory Acidosis pH &lt; 7.35 Respiratory Acidosis ↑ PCO2 (>45mm Hg) ↓pH Renal Comp:↑H+ excretion and ↑HCO3 reabsorption Respiratory Acidosis pH < 7.35 PaCO2 > 45 mmHg Respiratory Acidosis Common Causes Acute respiratory conditions (pulmonary edema, pneumonia, acute asthma), opiate OD, foreign body aspiratio0n, chest trauma Chronic respiratory acidosis, COPD, cystic fibrosis, MS, Stroke Respiratory acidosis cause retained CO2 excess carbonic acid Respiratory acidosis compensation Kidneys conserve bicarb to resore carbonic acid:bicarb ration of 1:20 Respiratory acidosis effect on ABGs decrease pH Increase PaCO2 Increase HCO3 Respiratory Alkalosis pH 7.45 PaCO2 < 35 mmHg Respiratory Alkalosis ↓PCO2 (<35mm Hg) ↑pH Renal Comp: ↓H+ excretion and ↓ HCO3 reabsorption Respiratory Alkalosis excess CO2 excretion Respiratory Alkalosis Common Causes Anxiety induced hyperventilation, fever, early salicylate intoxication, hperventilation with mechanical ventilator Respiratory alkalosis cause loss of CO2 deficient carbonic acid Respiratory alkalosis compensation Kidneys excrete bicarb and conserve H+ to restore carbonic acid: bicarb ratio Respiratory alkalosis effect on ABGs increase pH decrease PaCO2 decrease HCO3 Respiratory alkalosis is almost always a result of _________? hyperventilation Respiratory imbalances affect _________ _________ concentrations. carbonic acid Respiratory imbalances affect _________ _________ concentrations. carbonic acid Respiratory Regulation of pH Lungs regulate carbonic acid (H2CO3) by ↑ ↓ Respirations Lungs compensate quickly but incompletely Acidosis (↓ pH) •↑ RR => Blow off CO2 + H20 Alkalosis (↑ pH) •↓ RR => Retain CO2 + H2O Salicylates, fever, gram neg septicemia, hepatic insufficiency, chf, asthma, severe anemia- all causes of? Respiratory Alkalosis SaO2 values give a measurement the amount of oxygen bound to hgb compared to the of ? total hgb. Severe Hypoxemia PO2: < 45 mm Hg Symptoms of Metabolic Acidosis (9) 1. 2. 3. 4. Headache and lethargy Kussmaul's respirations Hypotension Stupor, possibly leading to coma and death 5. 6. 7. 8. 9. Anorexia N/V/D Dehydration Warm, flushed skin Fruity-smelling breath Symptoms of Metabolic Alkalosis (6) 1. Picking at bedclothes 2. Twitching 3. Confusion 4. N/V/D 5.Trousseau's sign 6. Slow, shallow respirations Symptoms of Respiratory Acidosis (8) 1. 2. 3. 4. 5. 6. 7. 8. Restlessness Confusion Coma Headaches SOB and tachypnea Decreased reflexes Hypoxemia Tachycardia and arrhythmias Symptoms of Respiratory Alkalosis (5) 1. Deep and rapid respirations 2. Dizziness 3. Agitation 4. Circumoral and peripheral paresthesia 5. Carpopedal spasms, twitching, and muscle weakness The acid base imbalance of a client with diabetic ketoacidosis is called? Metabolic acidosis The causes of Metabolic Acidosis have what in common? Volume concentration of bicarb is too low (not enough), it causes the pH level to fall making it acidosis/dotic The goal of the body is to maintain what kind of osmolarity? Neutral Treatment of Metabolic Acidosis (4) 1. Mechanical ventilation is usually first line of therapy 2. Treat DKA 3. Administer sodium bicarbonate 4. Dialysis Treatment of Metabolic Alkalosis (3) 1. D/C thiazide diuretics and NG suctioning 2. Give an antimetic for N/V 3. Meds to excrete bicarb Treatment of Respiratory Acidosis (6) 1. 2. 3. 4. 5. 6. Treatment of Respiratory Alkalosis 1. Treat underlying cause: sepsis, salicylate overdos 2. Hypoxia: give O2 Bronchodilator Oxygen Treat hyperkalemia Treat infection Treat underlying causes Chest CPT 3. Anxiety: gove a sedative 4. Hyperventilation: breathe into a paper bag 5. Adjust ventilator settings Ventilatory failure occurs when the PaCO2 level reaches? Acute ventilatory failure is indicated by? >50; PaCO2 >50 AND pH <7.30 What are the three compartments The intracellular, the extracellular and as a that water is stored in in the body? component of blood What are the two components of extracelluar fluid? Plasma and interstitial fluid What are the two most important extracellular solutes? Sodium and protein What are the two most important intracellular solutes? Potassium and protein What cells monitor the osmolarity of the plasma? Osmoreceptors What does isosmotic mean? Equal osmolarity What is interstitial fluid responsible A medium for exchange between the cell and the for? outside, how things enter and exit cells What is the 2nd intervention in correcting respiratory acidosis? and how do we correct that? Correct Acidosis through treating hyperkalemia if present and IV sodium bicarbonate What is the 2nd intervention in correcting respiratory acidosis? and how do we correct that? Correct Acidosis through treating hyperkalemia if present and IV sodium bicarbonate What is the 3rd intervention in correcting respiratory acidosis? and what are some of them? assess for iatrogenic complications of interventions--tetany, CO2 narcosis, rebound respiratory alkalosis, metabolic acidosis. What is the principal regulator of water intake? Thirst What is thirst regulated by? The osmolarity of the plasma What is water directly regulated by? Antidiuretic hormone (ADH) What is water indirectly regulated by and how is it regulated? Aldosterone- because it regulates sodium and wherever sodium goes water follows What organs regulate water balance? Kidneys, GI tract, lungs, and to a lesser extent skin What results from excreting too much CO2? respiratory alkalosis What should the nurse do for a respiratory alkalosis pt.? Eliminate cause of hyperventilation, help person breathe more slowly and deeply (paper bag), if neurological problems is the cause, treat the primary problem. What type of conditions can cause Respiratory Acidosis? any condition that would keep Co2(an acid) in the lungs; hypoventilation, obstructive lung disease, oversedation Whay type of condition can cause Respiratory alkalosis? Conditions due to LACK of Co2 (either by loss or inability to intake);hypoxia, anxiety, pulm embolus, hyperventilation Where does all the exchange between plasma and interstitial space occur? The capillary level Which is more dilute a solution with an osmolarity of 100 or a 100 solution with an osmolarity of 200? Why are diabetics always thirsty? Because there is an increased plasma osmolarity because of the increased glucose so the regulators are always being stimulated Your COPD patient has an acute exacerbation of the disease-- the acid base imbalance is? Respiratory acidosis