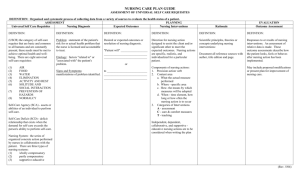
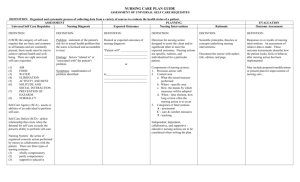
Refer to Nursing Diagnosis : Applicatio
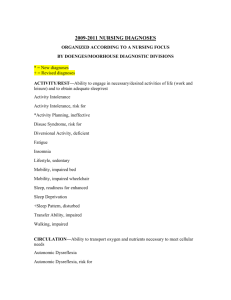
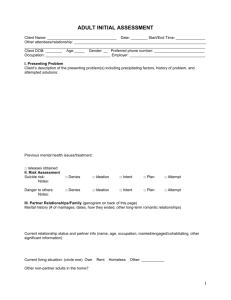
advertisement

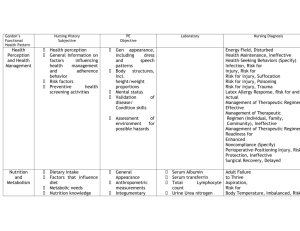
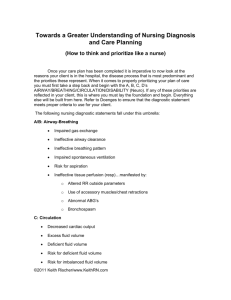
Worksheet NURSING PROCESS Gordon’s Functional Health Pattern Health Perception and Health Management Guide 1. Review the patient’s vital signs. Is the temperature within normal limits a. YES b. NO ( Risk for Infection;Ineffective Protection ) 2. Review the results of the complete blood cell count ( CBC) count. Are the cell counts within normal limits a. YES b. NO ( Risk for Infection;Ineffective Protection ) 3. Review the sensory status ( sight, hearing, touch, smell and taste ). Is the patient’s sensory status within normal limits ? a. YES b. NO ( Risk for Injury ) 4. Was the patient and family satisfied with the usual health status ? a. YES b. NO ( Health Seeking Behavior; Ineffective Health Maintenance ) 5. Did the patient, family, community describe the usual health status as good ? a. YES b. NO ( Health Seeking Behavior; Ineffective Health Maintenance ) 6. Had the patient , family, or community sought any health care assistance in the past year ? a. YES ( Health Seeking Behavior ) b. NO ( Ineffective Health Maintenace 7. Did the patient or family follow the routine the ( doctor , Nursing Diagnosis ( Refer to Nursing Diagnosis : Application to Clinical Practice By Lynda Juall Carpenito Moyet ( 2008 ) Energy Field, Disturbed Health Maintenance, Ineffective Health-Seeking Behaviors (Specify) Infection, Risk for Injury, Risk for Risk for injury, Suffocation Risk for injury, Poisoning Risk for injury, Trauma Latex Allergy Response, Risk for and Actual Management of Therapeutic Regimen, Effective Management of Therapeutic Regimen (Individual, Family, Community), Ineffective Management of Therapeutic Regimen, Readiness for Enhanced Noncompliance (Specify) Perioperative-Positioning Injury, Risk for Protection, Ineffective Surgical Recovery, Delayed nurse, dentist, etc ) prescribed ? a. YES ( Effective Management of Therapeutic Regimen. b. NO ( Non compliance , Ineffective Management of Therapeutic Regimen ) 8. Did the patient or family have any accidents or injuries in the past year ? a. YES ( Risk for Injury ) b. NO 9. Is there a disruption ( change in temperature , color , field, movement or sound )of the flow of energy surrounding the person ? a. YES ( Disturbed Energy Field ) b. NO 10. Was the patient, family, or community able to meet therapeutic needs of all members ? a. YES ( Effective Management of Therapeutic Regimen /Individual, Family, Community ) b. NO ( Ineffective Management of Therapeutic Regimen /Individual, Family, Community ) 11. Is the patient scheduled for surgery or has he or she recently undergone surgery ? a. YES (Risk for Perioperative Positioning Injury ) b. NO 12. Does the patient exhibit eczema ? a. YES ( Latex Allergy Response ) b. NO 13. Does the patient have a history of multiple surgeries or of reaction to latex ? a. YES ( Risk for Latex Allergy Response ) b. NO 14. Is the patient’s surgical incision healing properly? a. YES Nutrition and Metabolism b. NO ( Delayed Surgical Recovery) 1. Weigh the patient. Does the patient weigh more than the recommended range for his or her height , age and sex? a. YES ( Imbalanced Nutrition, More Than Body Requirements, Risk for or Actual : Fluid Volume Excess, Imbalanced Temperature, Risk for ; Imbalanced Fluid Volume , Risk for ) b. NO 2. Does the patient weigh less than the recommended range for his or her height, age and sex ? a. YES ( Imbalanced Nutrition, Less than Body Requirements, Deficient Fluid Volume, Risk for or Actual;Imbalanced Body Temperature, Risk for : Adult Failure to Thrive; Impaired Dentition. b. NO 3. Have the patient describe a typical day’s intake of both food and fluid, including snacks and the pattern of eating. Is the patient’s food intake above the average for his or her age, sex, height, weight and activity level ? YES ( Imbalanced Nutrition, Less Than Body Requirements ;Adult Failure To Thrive; Impaired Dentition ) NO 5. Is the patient’s fluid intake sufficient for his or her age, sex, height, weight, activity level and fluid output ? a. YES b. NO ( Deficient Fluid Volume , Risk for or Actual;Imbalanced Body Temperature, Risk for;Imbalanced Fluid Volume, Risk for ) 6. Does the patient show evidence of edema ? a. YES ( Fluid Volume Excess;Imbalanced Fluid Volume, Risk for ) b. NO 7. Is the patient’s gag reflex present ? a. YES b. NO ( Impaired Swallowing; Risk for Aspiration ) Adult Failure to Thrive Aspiration, Risk for Body Temperature, Imbalanced, Risk for Breastfeeding, Effective Breastfeeding, Ineffective Breastfeeding, Interrupted Dentition, Impaired Fluid Balance, Readiness for Enhanced Fluid Volume, Deficient, Risk for and Actual Fluid Volume, Excess Fluid Volume, Imbalanced, Risk for Hyperthermia Hypothermia Infant Feeding Pattern, Ineffective Nausea Nutrition, Imbalanced, Less Than Body Requirements Nutrition, Imbalanced, More Than Body Requirements, Risk for and Actual Nutrition, Readiness for Enhanced Swallowing, Impaired Thermoregulation, Ineffective Tissue Integrity, Impaired Skin Integrity, Impaired, Risk for and Actual Oral Mucous Membrane, Impaired 8. Does the patient cough or choke during eating ? a. YES ( Impaired Swallowing; Risk for Aspiration) b. NO 9. Assess the patient’s mouth, eyes and skin. Are these assessments within normal limits ( e.g. no lesions, soreness, or inflamed areas ) a. YES b. NO ( Impaired Tissue Integrity , Impaired Mucous Membrane ) 10. Assess the patient’s teeth. Are teeth within normal limits ? a. YES b. NO ( Impaired Dentition ) 11. Are intake and output, skin turgor and weight vacillating ? a. YES ( Imbalanced Fluid Volume , Risk for ) b. NO 12. Is the patient able to move freely in bed ? a. YES b. NO ( Impaired Tissue Integrity, Risk for or Actual ) 13. Review the patient’s temperature measurement. Is the temperature within normal limits ? a. YES b. NO ( Ineffective Thermoregulation: Hyperthermia; Hypothermia ) 14. Is the patient’s temperature above normal ? a. YES ( Ineffective Thermoregulation; Hypothermia ) b. NO 15. Is the temperature below normal ? a. YES ( Ineffective Thermoregulation; Hypothermia ) b. NO 16.Is the patient exhibiting signs or symptoms of infection? Vasoconstriction? Vasodilatation ? Dehydration ? c. YES ( Ineffective Thermoregulation; Hypothermia d. NO 17. Ask the patient “ Do you have any problems swallowing food ?Fluids ? a. YES ( Impaired Swallowing; Risk for Aspiratio ) b. NO 18. Does the patient report chronic health problems ? a. YES ( Adult Failure to Thrive ) b. NO 19. Is the patient complaining of being nauseated ? a. YES ( Nausea ) b. NO The next questions pertain to a mother who is breastfeeding. 20 Weight the infant. Is her or his height within normal limits for his or her age. A. YES ( Effective Breastfeeding ) b. NO ( Ineffective Breastfeeding. 21. Ask the patient : “ Do you have any problems or concerns about breastfeeding ? a. YES ( Ineffective Breastfeeding ) b. No ( Effective Breastfeeding ) Elimination Is there stool leakage when the patient coughs, sneezes, or laughs ? YES ( Bowel Incontinence ) NO Is there involuntary passage of stool ? a. YES ( Bowel Incontinence ) b. NO Bowel Incontinence Constipation, Risk for, Actual, and Perceived Diarrhea Urinary Elimination, Readiness for Enhanced Urinary Incontinence Functional Urinary Incontinence Reflex Urinary Incontinence Stress Urinary Incontinence Total Does the patient take laxatives on a routine basis ? a. YES ( Constipation , Perceived Constipation ) b. NO Urinary Incontinence Urge Urinary Incontinence, Risk for and Actual Urinary Retention Has a number of bowel movements decreased ? a. YES ( Constipation ) b. NO Are stools hard formed ? a. YES ( Constipation ) b. NO Does the patient have to strain to bowel movement ? a. YES ( Constipation ) b. NO Does the patient believe he or she is frequently constipated ) a. b. YES Constipation ) NO ( Perceived Does the patient expect to have a bowel movement at the same time each day ? A. YES ( Perceived Constipation ) B. NO Are bowel sounds increased ? a. YES ( Diarrhea ) b. NO Has a number of bowel movements increased ? a. YES ( Diarrhea ) b. NO Does the patient complain of loose, liquid stools ? a. YES ( Diarrhea ) b. NO Is there increased frequency of voiding ? a. YES ( Urinary Incontinence;Stress Incontinence; Urge Incontinence ) b. NO Is there dribbling of urine when the patient laughs, coughs or sneezes ? a. YES ( Stress Incontinence ) b. NO Once need to void is felt, is the patient able to reach toilet in time ? a. YES b. NO ( Urge Incontinence , Funcitonal Incontinence ) Does the patient complain of bladder spasms ? a. b. YES ( Reflex Incontinence ) NO Is there awareness of the need to void ? a. YES ( Reflex Incontinence ) b. NO Is there a decreased urge to void ? a. YES ( Reflex Incontinence ) b. NO Does the patient void in small amounts ? a. YES ( Urge Incontinence ;Urinary Retention) b. NO Is there urine flow without bladder distention? a. YES ( Total Incontinence ) b. NO Is the bladder distended ? a. YES ( Urinary Retention) b. NO Activity and Exercise Is there decreased urine output ? a. YES ( Urinary Retention ) b. NO 3. Does the patient’s heart rate or blood pressure increase abnormally in response to activity ? a. YES ( Activity Intolerance ) b. NO 1. Does the patient have dyspnea after activity ? a. YES ( Activity Intolerance ) b. NO 2. Does the patient have a medical diagnosis related to the cardiovascular or respiratory system ? a. YES ( Risk for Activity Intolerance ) b. NO 3. Does the patient have a history of Activity Intolerance ? a. YES ( Risk for Activity Intolerance ) b. NO 4. Does the patient complain of fatigue, weakness, or lack of energy ? a. YES ( Activity Intolerance or Fatigue ) b. NO 5. Is the patient unable to maintain usual routines ? a. YES ( Fatigue or Self Care Deficit ) b. NO 6. Does the patient report difficulty in concentrating ? a. YES ( Fatigue ) Activity Intolerance, Risk for and Actual Airway Clearance, Ineffective Autonomic Dysreflexia, Risk for and Actual Bed Mobility, Impaired Breathing Pattern, Ineffective Cardiac Output, Decreased Disuse Syndrome, Risk for Diversional Activity, Deficient Dysfunctional Ventilatory Weaning Response Falls, Risk for Fatigue Gas Exchange, Impaired Growth and Development, Delayed Development, Risk for Delayed Growth, Risk for Disproportionate Home Maintenance, Impaired Infant Behavior, Disorganized, Risk for and Actual, and Readiness for Enhanced Organized Peripheral Neurovascular Dysfunction, Risk for Physical Mobility, Impaired Sedentary Lifestyle Self-Care Deficit Feeding Bathing-Hygiene Dressing-Grooming Toileting Spontaneous Ventilation, Impaired Tissue Perfusion, Ineffective (Specify Type: Renal, Cerebral, Cardiopulmonary, b. NO 7. Review self-care chart. Does the patient have any self care deficits ? a. YES ( Self Care Deficit_ Specify which area ) b. NO 8. Can the patient engage in usual hobby while in hospital ? a. YES b. NO ( Deficient Diversional Activity ) 9. Does the family need help with home maintenance after the patient goes home ? a. YES ( Impaired Home Maintenance ) b. NO 10. Does the patient have insurance ? a. YES b. NO ( Impaired Home Maintenance ) 11. Is the patient within height and weight norm for age ? a. YES b. NO ( Delayed Growth and Development ) 12. Can the patient perform developmental skills appropriate for age level? a. YES b. NO ( Delayed Growth and Development ) 13. Are there any abnormal movements ? a. YES ( Disorganized Infant Behavior ) b. NO 14. Does the infant respond appropriately to stimuli ? a. YES b. NO ( Disorganized Infant Behavior ) 15. Does the patient’s cardiogram indicate arrhythmias ? Gastrointestinal, Peripheral) Transfer Ability, Impaired Walking, Impaired Wandering Wheelchair Mobility, Impaired a. YES ( Decreased Cardiac Output ) b. NO 16. Is the patient’s jugular vein distended ? a. YES ( Decreased Cardiac Output ) b. NO 17. Are the patient’s peripheral pulses within normal limits ? a. YES b. NO ( Decreased Cardiac Output , Ineffective Tissue Perfusion,or Risk for Peripheral Neurovascular Dysfunction ) 18. Are the patient’s extremities cold ? a. YES ( Ineffective Tissue Perfusion or Risk for Peripheral Neurovascular Dysfunction) b. NO 19. Does the patient have claudification ? a. YES ( Ineffective Tissue Perfusion or Risk for Peripheral Neurovascular Dysfunction ) b. NO 20. Does the patient have full range of motion ? a. YES b. NO 21. Does the patient have problems moving self in bed ? a. YES ( Impaired Mobility ) b. NO 22. Does the patient have problems ambulating ? a. YES ( Impaired Physical Mobility or Impaired Walking ) b. NO 24. Is the patient paralyzed? a. YES ( Risk for Disuse Syndrome ) b. NO 23. Is the patient mobilized by casts or traction ? a. YES ( Risk for Autonomic Dysreflexia ) b. NO 24. Does the patient have a spinal cord injury at T7 or above and paroxysmal hypertension ? a. YES ( Autonomic Dysreflexia ) b. NO 25. Does the patient have a spinal cord injury at T7 or above and bradycardia or tachycardia? a. YES ( Autonomic Dysreflexia ) b. NO 26. Review mental status examination. Is the patient exhibiting confusion or drowsiness? a. YES ( Impaired Gas Exchange ) b. NO 27. Review blood gases. Does the patient demonstrate hypercapnia ? a. YES ( Impaired Gas Exchange or Impaired Spontaneous Ventilation ) b. NO 28. Were rales ( crackles ) or rhonchi ( wheezes ) present on chest auscultation ? a. YES ( Ineffective Airway Clearance ) b. NO 29. Is Respiratory rate increased above normal range ? a. YES ( Ineffective Airway Clearance or Ineffective Breathing Pattern ) b. NO 30. Is the patient on a ventilator ? If Yes, does the patient have restlessness or an increase from baseline of blood pressure , pulse, or respiration when attempts at weaning are tried ? a. YES ( Dysfunctional Ventilatory Weaning Response ) b. NO 31. Does the patient have dyspnea and shortness of breath ? a. YES ( Ineffective Breathing Pattern, Impaired Spontaneous Ventilation , or Activity Intolerance ) b. NO 32. Is the patient exhibiting pursed lip breathing ? a. YES ( Ineffective breathing Pattern ) b. NO 33. Does the patient have history of falling ? a. YES ( Risk for Falls ) b. NO 34. Does the patient have diminished mental status ? a. YES ( Risk for Falls ) b. NO 35. Does the patient have difficulty in manipulating his or her wheelchair ? a. YES ( Impaired Wheelchair Mobility ) b. NO 36. Can the patient independently transfer himself or herself from site to site ? a. YES b. NO ( Impaired Transfer Ability ) Cognition and Perception c. 1. Does the inctracranial pressure fluctuate following a single activity ? a. YES ( Decreased Intracranial Adaptive Capacity ) 2. Does the patient have a problem with appropriate response to Adaptive Capacity, Intracranial, Decreased Confusion, Acute and Chronic Decisional Conflict (Specify) stimuli ? a. YES ( Confusion) b. NO 3. Does the patient have a problem with fluctuating levels of consciousness ( in presence of inappropriate response to stimuli ) a. YES ( Acute Confusion) b. NO ( Chronic Confusion) 4. Does the patient indicate difficulty in making choices between options for care ? a. YES ( Decisional Conflict –specify ) b. NO 5. Is the patient delaying decision making regarding care options ? a. YES ( Decisional Conflict –Specify ) b. NO 6. Has the patient been disoriented to person, place, and time for more than 3 months ? a. YES ( Impaired Environmental Interpretation Syndrome ) b. NO 7. Can the patient respond to simple directions or instructions ? a. YES b. NO ( Impaired Environmental Interpretation Syndrome ) 8. Does the patient indicate lack of information regarding his or her problem ? a. YES ( Deficient Knowledge – Specify ) b. NO 9. Can the patient restate the regimen he or she needs to follow for improved health ? a. YES b. NO ( Deficient Knowledge – Specify ) 10. Can the patient remember events occurring within the past 4 hours ? a. YES Environmental Interpretation Syndrome, Impaired Knowledge, Deficient (Specify) Knowledge, Readiness for Enhanced (Specify) Memory, Impaired Pain, Acute and Chronic Sensory Perception, Disturbed (Specify: Visual, Auditory, Kinesthetic, Gustatory, Tactile, Olfactory) Thought Processes, Disturbed Unilateral Neglect b. NO Sleep and Rest a. b. Self Concept 1. Does the patient report a problem falling asleep ? YES ( Disturbed Sleep Pattern ) NO 1. Does the patient report interrupted sleep ? a. YES ( Sleep Deprivation ) b. NO 1. Does the patient express concern regarding current situation ? a. YES ( Anxiety or Fear ) b. NO 2. Can the patient identify source of concern ? a. YES ( Fear ) b. NO ( Anxiety ) 3. Is the patient going to have, as a result of this admission, a change in body structure or function? a. YES ( Disturbed Body Image ) b. NO 4. Does the patient verbalize a change in lifestyle as a result of this admission ? a. YES ( Disturbed Body Image ) b. NO 5. Does the patient express fear about dying ? a. YES ( Death Anxiety ) b. NO 6. Is the patient expressing worries about the impact of his of her death on his or her family and /or friends ? a. YES ( Death/Anxiety ) b. NO 7. Does the patient verbalize a negative view of self ? Sleep, Readiness for Enhanced Sleep Deprivation Sleep Pattern, Disturbed a. YES ( Situational Low Self Esteem ) b. NO 8. Does the patient believe he or she can deal with the current problem that led to this admission ? a. YES b. NO ( Situational Low Self Esteem ) 9. Does the patient of his or her family indicate the self negating impression is a long standing ( several years ) problem ? YES ( Chronic Low Self Esteem ) NO ( Situational Low Self Esteem ) 10. Does the patient question who he or she is or verbalize lack of an understanding regarding his or her role in life ? a. YES ( Disturbed Personal Identity ) b. NO 11. Does the patient appear passive or verbalize passivisity ? a. YES ( Hopelessness ) b. NO 12. Does the patient demonstrate decreased verbalization and /or flat affect ? a. YES ( Hopelessness ) b. NO 13. Does the patient have a problem with physical or social isolation ? a. YES ( Risk for Loneliness ) b. NO 14.Has the patient recently suffered the loss of significant other ? a. YES ( Risk for Loneliness ) b. NO 15. Does the patient verbalize lack of control ? a. YES ( Powerlessness ) b. NO 16. Is the patient participating in care and decision making regarding care ? a. YES b. NO ( Powerlessness ) Roles and Relationship 1. Is the client exhibiting distress over a potential loss ? a. YES ( Anticipatory Grieving ) b. NO 2. Is the client denying a potential loss ? a. YES ( Anticipatory Grieving ) b. NO 3. Is the client exhibiting distress over an actual loss ? a. YES ( Dysfunctional Grieving ) b. NO 4. Is the client denying an actual loss ? a. YES ( Dysfunctional Grieving ) b. NO 5. Is the client making verbal threats against others ? a. YES ( Risk for Violence ) b. NO 6. Is the client exhibiting increased motor activity ? a. YES ( Risk for Violence ) b. NO 7. Can the patient speak English ? Anxiety Body Image, Disturbed Death Anxiety Fear Helplessness Loneliness, Risk for Personal Identity, Disturbed Powerlessness, Risk for and Actual Self-Concept, Readiness for Enhanced Self-Esteem, Chronic Low, Situational Low, and Risk for Situational Low Self-Mutilation, Risk for and Actual a. YES b. NO ( Impaired Verbal communication) 8. Does the patient demonstrate any difficulty in talking ? a. b. YES ( Impaired Verbal Communication ) NO 9. Does the patient verbalize difficulty with social situations? a. b. YES ( Impaired Social Interaction) NO 10. Does the client indicate strained relationships with his family or others ? a. b. YES ( Impaired Social Interaction ) NO 11. Does the patient have family or significant others visiting or calling ? a. YES b. NO ( Social Isolation ) 12. Is the patient uncommunicative, withdrawn or not making eye contact ? a. YES ( Social Isolation) b. NO 13. Does the client indicate the admission might impact role ?( family, work or leisure ) ? a. b. YES ( Ineffective Role Performance ) NO 14. Does the family or do significant others verbalize that admission might impact the patient’s role ( family, work of leisure ) a. YES ( Ineffective Role Performance ) b. NO 15. Does the child show signs or symptoms of physical or emotional abuse ? a. YES ( Impaired Parenting ) b. NO 15. Do the parents indicate difficulty controlling the child ? a. YES ( Impaired parenting ) b. NO 16. Do the parents indicate difficulty in controlling the child ? a. YES ( Impaired Parenting ) b. NO 17. Do the parents demonstrate attachment behavior ? a. YES b. NO ( Risk of Impaired Parenting , Risk for Impaired Parent, Infant and Child Attachment ) 18. Do the parents make negative comments about the child ? a. YES ( Risk for Impaired Parenting ) b. NO 19. Does the family demonstrate capability to meet the child’s physical needs ? a. YES b. NO ( Interrupted Family Processes ) 20. Does the family demonstrate capability to meet the child’s physical needs ? a. YES b. NO ( Interrupted Family Processes ) 21. Does a family member exhibit signs and symptoms of alcoholism ? a. YES ( Dysfunctional Family Processes : Alcoholism ) b. NO 22. Do the parents express concern about ability to meet the child’s physical or emotional needs ? a. YES ( Parental Role Conflict ) b. NO 23. Are the parents frequently questioning decisions about the child’s care ? a. YES ( Parental Role Conflict ) b. NO 24. Was the infant premature ? a. YES ( Risk for Impaired Parent, Infant and Child Attachment ) b. NO 25. Do the parents express anxiety regarding the parental role ? a. YES ( Risk for Impaired Parent, Infant and Child Attachment ) b. NO 26. Has the patient recently received a diagnosis related to a chronic physical or mental condition? a. YES ( Chronic Sorrow ) b. NO 27. Is the patient verbally expressing sadness ? a. YES ( Chronic Sorrow ) b. NO 28. Is the patient role of primary caregiver for another person a. YES ( Risk for Caregiver Role Strain, Caregiver Role Strain ) b. NNNO 29. Does the patient verbally express difficulty in our caregiver role ? a. YES ( Caregiver Role Stress ) b. NO 30. Has the patient recently moved from one living site to another ? a. YES ( Risk for Relocation Stress Syndrome ) b. NO 31. Does the patient appear depressed following a change in living environments ? a. YES ( Risk for Relocation Stress Syndrome ) b. NO 32. Does the patient facing a change in a living environment have a good support system ? a. YES b. NO ( Risk for Relocation Stress Syndrome ) 33. Does the patient express concern over his or her recent move ? a. YES ( Risk for Relocation Stress Syndrome ) b. NO Sexuality and Reproductive Function 1. Following a rape, is the patient experiencing multiple physical symptoms ? a. YES ( Rape Trauma Syndrome;Compound Reaction ) b. NO 2. Following a rape , is the patient indicating severe emotional reactions ? a. YES ( Rape Trauma Syndrome ; Compound Reaction ) Rape-Trauma Syndrome: Compound Reaction And Silent Reaction Sexual Dysfunction Sexuality Patterns, Ineffective b. NO 3. Is the client using alcohol or drugs to cope following a rape ? a. YES ( Rape Trauma Syndrome :Compound Reaction) b. NO 4. Has the client changed her relationship with males ? a. YES ( Rape Trauma Syndrome; Silent Reaction) 5. Does the client indicate increased anxiety in follow up counseling ? a. b. YES ( Rape Trauma Syndrome ; Silent Reaction ) NO 6. Does the client verbalize any problems related to sexual functioning ? a. YES ( Sexual Dysfunction) b. NO 7. Does the client exhibit any indications of physical or psychosocial abuse ? a. YES ( Sexual Dysfunction) b. NO 8. Does the client relate any changes in sexual behavior ? a. YES ( Ineffective Sexuality Pattern ) b. NO 9. Does the client report any difficulties or limitations in sexual behavior ? a. b. Stress and Stress Response YES ( Ineffective Sexuality Patterns ) NO 1. Does the client verbalize inability to cope? a. YES ( Ineffective Individual Coping ) Adjustment, Impaired b. NO Coping – Stress Tolerance Test 2. Does the client demonstrate inability to problem solve ? a. YES ( Ineffective Individual Coping ) b. NO 3. Does the client deny problems or weaknesses in spite of evidence to the contrary? a. YES ( Defensive Coping ) b. NO 4. Is the client projecting blame for the current situation on other persons or events ) a. YES ( Defensive Coping ) b. NO 5. Did the patient delay seeking health care assistance to the detriment of his or her health ? a. YES ( Ineffective Denial ) b. NO 6. Does the patient downplay condition? a. YES ( Ineffective Denial ) b. NO 7. Does the patient verbalize nonacceptance of health status change ? a. YES ( Impaired Adjustment) b. NO 8. Is the patient moving toward independence ? a. YES b. NO ( Impaired Adjustment ) 9. Is the client’s primary caregiver denying the severity of the client’s problem? a. YES ( Disabled Family Coping ) b. NO Community Coping, Ineffective and Readiness for Enhanced Coping, Readiness for Enhanced Family Coping, Compromised and Disabled Family Coping, Readiness for Enhanced Individual Coping, Ineffective Coping, Defensive Denial, Ineffective Post-Trauma Syndrome, Risk for and Actual Suicide, Risk for 10. Does the client demonstrate indications of neglect ? a. YES ( Disabled Family Coping ) b. NO 11. Does the client state concerns about care being received from primary caregiver ? a. YES ( Compromised Family Coping ) b. NO 12. Can the primary caregiver verbalize understanding of care requirements? a. YES b. NO ( Compromised Family Coping ) 13. Does the family indicate physical and emotional support for the client ? a. b. YES ( Readiness for Enhanced Family Coping ) No a. Does the family or primary caregiver indicate interest in a support group? a. b. YES ( Readiness for Enhanced Family Coping ) NO 15. Does the patient exhibit re reexperience of traumatic events ( flashbacks or nightmares ) a. YES ( Post Trauma Syndrome ) b. NO 16. Does the patient exhibit vagueness about traumatic event ? a. YES ( Post Trauma Syndrome ) b. NO 17. Is there evidence of positive communication and community participation in planning for predicted community stressors ? a. YES ( Readiness for Enhanced Community Coping ) b. NO 18. Is there evidence of community conflict and deficits in community participation ? a. b. YES ( Ineffective Community Coping ) NO 19. Has the patient threatened to kill himself or herself ? a. YES ( Risk for Suicide ) b. NO 20. Has the patient demonstrated marked changes in behavior , attitude or school performance ? a. YES ( Risk for Suicide ) b. NO Values and Beliefs 1. Does the patient express anger toward a supreme being regarding his or her current condition ? a. YES ( Spiritual Distress ) b. NO ( Spiritual Well Being ) 2. Does the patient verbalize conflict about personal spiritual beliefs ? a. YES ( Spiritual Distress ) b. NO ( Spiritual Well Being ) 3. Does the patient indicate positive thoughts about spirituality ? a. YES ( Readiness for Enchanced Spiritual Well Being ) b. NO Impaired Religiosity, Risk for and Actual Spiritual Distress, Risk for and Actual Spiritual Well-Being, Readiness for Enhanced References : Carpenito – Moyest , L.J. Nursing Diagnosis :Application to Clinical Practice 12th edition( 2008 ). Lippincott Williams and Wilkins, PA Cox, H.C Clinical Application of Nursing Diagnosis 4th edition ( 2002 ). FA Davis Company. PA RCR 071209