ADULT INITIAL ASSESSMENT
advertisement

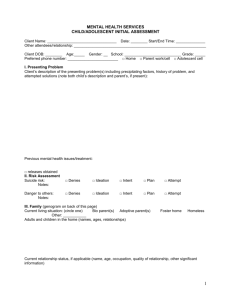
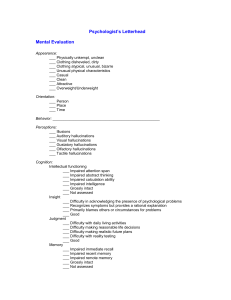
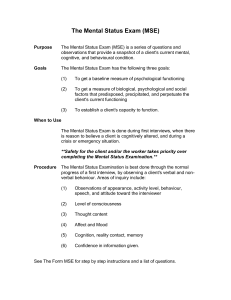
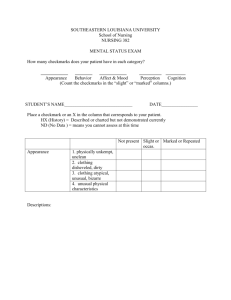
ADULT INITIAL ASSESSMENT Client Name: _________________________________ Date: ________ Start/End Time: ______________ Other attendees/relationship: _______________________________________________________________ ______________________________________________________________________________________ Client DOB: ________ Age:_____ Gender: __ Preferred phone number: ________________________ Occupation: _______________________________ Employer: ____________________________________ I. Presenting Problem Client’s description of the presenting problem(s) including precipitating factors, history of problem, and attempted solutions: Previous mental health issues/treatment: □ releases obtained II. Risk Assessment Suicide risk: Notes: Danger to others: Notes: □ Denies □ Ideation □ Intent □ Plan □ Attempt □ Denies □ Ideation □ Intent □ Plan □ Attempt III. Partner Relationships/Family (genogram on back of this page) Marital history (# of marriages, dates, how they ended, other long-term romantic relationships) Current relationship status and partner info (name, age, occupation, married/engaged/cohabitating, other significant information) Current living situation: (circle one) Own Rent Homeless Other: ___________ Other non-partner adults in the home? 1 Children in the home (names, ages, relationships) Other biological children not living with client (names, ages, reason for other placement) Family of origin (relationship with parents in childhood, current relationship with parents, parents’ occupations and personalities, relationship past and present with siblings, birth order, dates and age of any deceased family members- cont. on back if necessary) Cont. on back? YES NO IV. Health Last physical exam ______ Doctor’s name ______________ Medical history (illnesses, accidents, medications, current health status) Currently compliant in taking medications as prescribed? If not, why? Substance abuse: (alcohol, drugs, age of first use, frequency, family history, symptoms, consequences, tx) What is the client’s caffeine intake? Does client smoke cigarettes? (If yes, specify history and current use.) Family health history Family mental health history (including institutionalizations, ADHD-type problems, anyone “not quite right”) V. Personal Recent major changes/losses ( divorce, death, job, relocation, etc.) Employment (past, present, disruptions, aspirations) 2 Education (trouble with learning, attention, behavior, learning disabilities, truancy as child/adolescent, highest grade completed, adult educational history, future plans) Military service (branch, length and location of service, active duty, time at war, type of discharge) Legal problems (past or pending, criminal, nature, attitude toward authority) Abuse (physical/sexual/verbal/emotional, perpetrator or victim, if victim: by whom, age(s), duration, frequency, reactions, current attitude about the abuse) or other trauma VI. Resources Current support system (friends, family, pets, social groups, religion, hobbies, etc.) Strengths and skills Client self-ratings: On a scale of 1 to 10, client rates his/her current functioning at _____. Areas the client feels are impaired/impacted by the concern/problem(s): What stage of change does client appear to be at? □ Pre-contemplation □ Contemplation □ Planning □ Action □ Maintenance What does the client think would help move him/her towards the next level? Are there any barriers to change/reasons for maintaining the problem(s)? How will he/she know that things are getting better? Initial goals and plan: 3 VII. Behavioral Observations (check boxes and note any specific observations below each) Appearance: □ Normal Eye contact: □ Good □ Tidy □ Disheveled □ Culturally appropriate □ Immature □ Unclean □ Adequate □ Unusual □ Inconsistent □ Overly intense □ Poor Gait/Gross Motor Movement: □ Normal □ Accelerated □ Slowed/retarded □ Clumsy/lacking coordination □ Exaggerated □ Peculiar Posture: □ Normal Mannerisms: □ None noted □ Tics □ Rocking □ Grimacing □ Flapping □ Tremors □ Other Energy Level: □ Normal Speech: □ Normal □ Quiet □ Slowed □ Slumped □ Rigid □ Stiff/Rigid □ Atypical □ Fidgety □ Lethargic □ Nonverbal □ Monotone □ Halting/difficulty finding words □ Rapid □ Loud □ Impoverished □ Peculiar topics/other □ Stuttering □ Tearful/sad □ Anxious □ Fluctuating □ Tugging □ Hyperactive Patterns of Behavior: □ Unremarkable □ Rituals Affect: □ Composed □ Apathetic □ Dramatic □ Dysmorphic □ Agitated/restless □ Stereotypy (unvarying repetition) □ Compulsions □ Distressed □ Blunt/flat □ Euphoric □ Suspicious □ Labile □ Angry □ Shallow □ Inconsistent with thought/speech VIII. Cognitive Observations (check boxes and note any specific observations below each) Consciousness: □ Alert □ Drowsy/dazed □ Easily startled □ Unresponsive □ Under-responsive Attention: □ Good □ Distractible Orientation: □ Normal Impaired orientation to: □ Person Memory: □ Intact □ Impaired STM □ Selective □ Impaired LTM □ Obsessions □ Inadequate □ Place □ Confused □ Pre-occupied □ Time □ Situation □ Impaired immed. Recall □ Adeq. recall w/effort Intellectual Functioning: □ Average □ Below Average Any known deficits: □ Verbal □ Non-verbal Thought Content: □ Unremarkable □ Fluctuating □ Above Average □ Pre-occupation □ Delusions Thought Process: □ Unremarkable □ Non-linear □ Delusions □ Loose associations □ Paranoia □ Rapid shifts of focus □ Narcissism □ Somatic pre-occupations □ Obsession □ Grandiosity □ Other (specify) Perceptual Disturbance: □ None □ Flashbacks □ Dissociation Hallucinations: □ Visual □ Auditory □ Tactile □ Olfactory Insight: □ Developmentally appropriate □ Denies Problem Judgment: □ Dev. appropriate □ Unsafe behavior □ Poor decision-making □ Projects blame □ Inflexible □ Poor □ Easily overwhelmed 4 IX. Diagnostic Impressions Preliminary diagnosis: Therapist signature: _________________________________________________ Date: _____________ 5