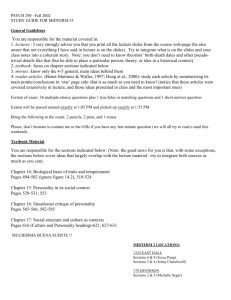
Personality Disorders
advertisement

Davis 1 Personality Disorders Peter Davis Abnormal Psychology Instructor: Dr. John Gibralter May 22, 2011 Davis 2 Abstract Personality disorders comprise a complex set of disorders encompassing emotional, interpersonal, cognitive, and behavioral patterns. The DSM-IV-TR organizes ten of these personality disorders into three groups, known as clusters, which share several traits and characteristics. Two other provisional personality disorders are listed in the DSM-IV-TR appendix. These deep-rooted, long-lasting disorders can cause a wide range of problems, with mild to severe consequences for the afflicted individual and the greater society. Some disorders primarily affect only the disordered person, while others, such as anti-social personality disorder, can have far-reaching implications for society as well as the disordered individual. Moreover, a personality disorder can cause self-limiting and self-defeating behavior in an individual who might otherwise lead a fulfilling, productive life. Difficult to diagnose and treat, personality disorders present a formidable challenge to those who are so diagnosed. Consequently, the mental health professionals tasked with understanding and treating these individuals face a set of challenges all their own. Davis 3 Personality Disorders: Definitions and Distinctions The DSM-IV-TR lists ten distinct personality disorders as well as two “provisional” disorders; passive-aggressive disorder and depressive personality disorder (Butcher et al., p. 362). Unlike certain stress-related or mood disorders, personality disorders might be considered to be chronic, rather than acute, as they have deep, long-lasting roots in the psyche of the afflicted individual. Organized by the DSM-IV-TR into three clusters, each cluster sharing similar traits, personality disorders represent long-term cognitive distortions and maladaptive behaviors, often stemming from traumas and stress-producing events that occurred early in life. According to Butcher et al. (2010), DSM-IV-TR criteria for personality disorders includes “an enduring pattern of behavior [that is] pervasive and inflexible, as well as stable and of long duration” (p. 341). In addition, the person’s “behavior must…cause either clinically significant distress or impairment in functioning” (p. 341). Thus, for someone diagnosed with a personality disorder, these long-term, familiar behaviors and impairments often seem normal. However, to a neutral observer, the person’s behaviors will seem odd, eccentric, and often unacceptable (Butcher et al., 2010, p. 342). The three personality disorder clusters, A, B, and C, represent different behavior patterns and tendencies. Within the individual clusters, the disorders display common traits, yet each disorder has its own distinguishing factors and criteria. The personality disorders also share traits between the clusters; this high comorbidity rate often makes it difficult to make an accurate diagnosis (Butcher et al., 2010, pp. 343-344). The personality disorders in cluster A are: paranoid, schizoid, and schizotypal. A person with one of these disorders “might seem odd or eccentric,” as well as displaying “distrust…suspiciousness [and] social detachment” (Butcher et al., 2010, p. 342). Cluster B includes: histrionic, narcissistic, antisocial, and borderline Davis 4 personality disorders. Butcher et al. (2010) portrays those with a cluster B diagnosis as “dramatic, emotional, and erratic” (p. 342). Finally, the personality disorders in cluster C are: avoidant, dependent, and obsessive-compulsive. People diagnosed with a cluster C disorder “show anxiety and fearfulness” (Butcher et al., 2010, p. 342). These are categorical summaries; the individual disorders require a deeper understanding and analysis. Cluster A: Paranoid, Schizoid, and Schizotypal Personality Disorders A person diagnosed with paranoid personality disorder might appear to be angry at the world for any number of reasons. Suspicion, distrust, anger, a tendency to bear a grudge, as well as to be unforgiving, are some of the symptoms that define a person with paranoid personality disorder. As in all cluster A disorders, an individual with paranoid personality disorder might seem introverted, detached, and a loner. Their inherent anger and suspicion for others creates distance between themselves and the rest of the world. In addition, a person with paranoid personality disorder feels that others are to blame for their perceived ills, so, why interact with those who mean you harm? Thus, the person diagnosed with paranoid personality disorder pushes the world away for self-defensive reasons that are largely self-invented. Those diagnosed with schizoid personality disorder disengage, not out of anger, but out of a lack of concern for most others. Their inability to experience pleasure from many common activities is attenuated, making them seem almost anhedonic. Butcher et al. (2010) used the term “introvert” to describe those who have this diagnosis when they wrote: “They tend not to take pleasure in…sexual activity, and rarely marry. More generally, they are not very emotionally reactive…[and] show a generally apathetic mood” (M.B. Miller et al., 2001; Mittal et al., 2007, as cited in Butcher et al., 2010, p. 346). Put simply, in layperson’s terms, an individual with schizoid personality disorder is not interested in others; they just do not seem to care. Davis 5 The schizotypal personality disorder presents different symptoms. Like the schizoid personality, the schizotypal personality is introverted, aloof, and has “pervasive social and interpersonal deficits” (Butcher et al., 2010, p. 347). Added to these traits are “cognitive and perceptual distortions, as well as oddities and eccentricities in their communication and behavior” (Butcher et al., 2010, p. 347). Language, communication, and perceptual distortions can be presented as “odd speech, and paranoid beliefs” (McGlashan et al., 2005, as cited in Butcher et al., 2010, p. 348). Importantly, Butcher et al. (2010) wrote, “[these characteristics] are similar to those often seen in schizophrenic patients” (p. 348). They add, “many researchers conceptualize schizotypal personality disorder as an attenuated form of schizophrenia” (Raine, 2006, as cited in Butcher et al., 2010, p. 348). Thus, we see an example of comorbidity between the personality clusters, as well as between personality disorders and psychotic disorders. Cluster B: Histrionic, Narcissistic, Borderline, and Antisocial Personality Disorders While those diagnosed with a cluster A disorder can be described as introverted, a primary trait of the cluster B personality is extraversion. Those with histrionic personality disorder seek to be the center of attention, the focus of conversation, and have a tendency to display exaggerated emotionality in communication and behavior. When denied this attention, the histrionic personality can become emotionally frustrated and act out. Charming and seductive behavior can suddenly shift to aggression and verbal attack, causing discomfort for others. In contrast to the schizoid personality, where approval from others is rarely, if ever, sought, those with histrionic personality disorder actively seek the approval of others. Butcher et al. (2010) described those with histrionic personality disorder as “craving stimulation and attention….selfcentered, vain, and excessively concerned about the approval of others” (p. 349). Davis 6 Similar to the histrionic personality, those with narcissistic personality disorder also seek attention, although for very different reasons. While the histrionic personality seeks attention as a form of self-validation, (i.e., if you don’t love me I am worthless), the narcissistic personality seeks attention because they deserve it (i.e., if you don’t love me, you are worthless). For instance, the histrionic personality might think, “unless I captivate people, I am nothing” (Beck et al., 1990, p. 50; Beck et al., 2003, as cited in Butcher et al., 2010, p. 351). In contrast, the narcissistic personality “seeks admiration” (Butcher et al., 2010, p. 353). The DSM-IV-TR lists “excessive need for admiration” and a “grandiose sense of self-importance” as two of the nine criteria for narcissistic personality disorder (APA, 2000). In addition, the narcissistic personality tends to “overestimate their abilities and accomplishments while underestimating the abilities and accomplishments of others” (Butcher et al., 2010, p. 352). In this way, the narcissistic personality places themselves above others, looking down on all those who are deemed less worthy. Similar to the paranoid personality, the narcissistic personality has an “unwillingness to forgive…and they easily take offense” (Butcher et al., 2010, p. 352). A person with borderline personality disorder presents erratic, impulsive, and unstable behaviors. Lacking stable interpersonal relationships and a strong sense of self, those with borderline personality disorder have “chronic feelings of emptiness” and are quick to react with “inappropriate, intense anger” (APA, 2000). Moreover, these individuals can experience severe dysphoria, which can cause extreme reactions such as self-mutilation, known as “cutting.” In Alvin H. Perlmutter’s 1992 video series, “Kelly,” who was being treated for borderline personality disorder, describes her experience with dysphoria and cutting: “I needed a release from [the] pain…I just couldn’t touch reality…my one way of touching reality was to cut myself Davis 7 and to see the blood and that always made me feel better…to see the scars.” Accompanying this self-mutilating behavior is an increased rate of suicide attempts. Some theorize that this extreme behavior “serves to communicate the person’s level of distress to others” (Paris, 2007, as cited in Butcher et al., 2010, p. 355). Those with borderline personality disorder experience a high degree of comorbidity with other Axis I disorders including “unipolar…bipolar and anxiety disorders…[as well as] substance-use and eating disorders” (Hooley, 2008; Skodol, Gunderson, et al., 2002a, as cited in Butcher et al., 2010, p. 356). Although several causal factors are associated with borderline personality disorder, early childhood trauma seems to play a significant role with “about 90 percent of patients with borderline personality disorder [having reported] some type of childhood abuse or neglect” (Butcher et al., 2010, p. 357). However, this remains in dispute, for Butcher et al. (2010) adds, “most such studies…cannot tell us that such early childhood trauma plays a causal role” (p. 357). Last in cluster B is antisocial personality disorder, indicated by the “[violation] and… disregard for the rights of others through deceitful, aggressive, or antisocial behavior, typically without remorse or loyalty to anyone” (Butcher et al., 2010, p. 354). Those with this disorder often present aggressive, destructive, and violent behaviors, showing little, if any, regard for those on the receiving end of these actions. Taken to its extreme, the antisocial personality will severely violate the norms of society and engage in criminal behavior such as property crimes, physical assaults, and murder. Before the DSM-III (1980) defined these behaviors as antisocial personality disorder, other terms were used. In the nineteenth century, “moral insanity” held sway (Pritchard, 1835, as cited in Butcher et al., 2010, p. 365). In the twentieth century, Davis 8 sociopathy and psychopathy (sociopath and psychopath) were used to describe many of the behaviors now referred to as antisocial personality disorder (Butcher et al., 2010, p. 365). While an individual with borderline personality disorder can display violent tendencies, they can also display a sense of remorse and conscience. The antisocial personality, however, shows no such thought or consideration for others. Two of the DSM-IV-TR criteria for antisocial personality disorder are, “reckless disregard for safety of self or others” and “lack of remorse” (APA, 2000). An important offshoot of the antisocial personality is the “successful” psychopath, meaning those who stay below society’s radar, avoiding arrest and incarceration, while actively engaging in antisocial or psychopathic behavior. Butcher et al. (2010) refers to the successful psychopath and the “criminal psychopath,” referring to those psychopaths who are institutionalized (Table 10.1, p. 372). If one were to look around their neighborhood, would they be able to point out those individuals who fit the definition of successful psychopath? Cluster C: Avoidant, Dependent, and Obsessive-Compulsive Personality Disorders Those with avoidant personality disorder suffer from an inability to comfortably interact and exchange with others. Deep-seated insecurities and maladaptive schemas cause the avoidant personality to avoid what they actually want: friends, confidants, and emotional intimacy. Timidity and a poor self image cause the avoidant personality to feel unworthy and incapable. The DSM-IV-TR criteria for avoidant personality disorder includes, “unwillingness to get involved with people unless certain of being liked,” “preoccupation with being criticized or rejected,” and “views self as socially inept or inferior to others” (APA, 2000). Unlike those with schizoid personality disorder who prefer their solitude, those with avoidant personality disorder “desire affection and are often lonely and bored” (Butcher et al., 2010, p. 358). As a result, their Davis 9 self-denying, self-limiting behavior causes them pain and isolation. Similar to the schizoid personality, an individual with avoidant personality disorder will “show deficits in their ability to experience pleasure” (Taylor et al., 2004, as cited in Butcher et al., 2010, p. 358). Those with dependent personality disorder show cognitive, behavioral, and perceptual distortions that result in pronounced dependency and submissiveness to others, as well as an inordinate fear of being left alone. Criteria in the DSM-IV-TR for dependent personality disorder includes, “needs others to take responsibility for most major areas of life,” “feels uncomfortable or helpless when alone because of fears of being unable to care for self,” and “urgently seeks another relationship for care and support when a close relationship ends” (APA, 2000). Those with dependent personality disorder will avoid expressing their true feelings, fearing reprisal or even abandonment by those they cling to. For example, people in “psychologically or physically abusive relationships,” rather than leave and be on their own, will stay in the damaging relationship (Butcher et al., 2010, p. 359). In addition, should the dependent personality actually leave, their “indiscriminate…selection of mates” might cause them to begin a new relationship with similar or identical negative parameters as the previous relationship. (Butcher et al., 2010, p. 359). Similar to the histrionic personality, the dependent personality achieves self-validation from the approval of others. In addition, the dependent personality shares traits with the borderline personality as “both…personalities fear abandonment” (Butcher et al., 2010, p. 359). Last in the cluster C disorders is obsessive-compulsive personality disorder. Those who have this disorder are overly concerned with “mental and interpersonal control…[as well as] attention to rules, orders, and schedules” (Butcher et al., 2010, p. 360). They are rigid, stubborn, and unwilling to delegate tasks, fearing that others might not accomplish the task in an identical Davis 10 manner to themselves. Unlike those diagnosed with Axis I obsessive-compulsive disorder, people with obsessive-compulsive personality disorder do not focus on specific rituals such as hand washing. Instead, the obsessive-compulsive personality takes a broader approach, insisting (through their behaviors), that everything be perfect, orderly, and in its proper place. DSM-IV-TR criteria for this personality disorder includes: “preoccupation with details, rules, order, or schedules, to the extent that the major point of an activity is lost,” “extreme perfectionism that interferes with task completion,” and “reluctance to delegate tasks or work with others unless others do exactly the same thing” (APA, 2000). Interestingly, the additional DSM-IV-TR criteria, “inability to discard worn-out or worthless objects,” can also be applied to those who hoard. Moreover, does the obsessive-compulsive personality’s unwillingness to delegate to others signify a lack of trust in the abilities of others to meet their (obsessivecompulsive) standards? Alternatively, because “excessive devotion to work to the exclusion of leisure and friendships” is another DSM-IV-TR criteria for obsessive-compulsive personality disorder, is the devotion to perfection a way to keep others at a distance and avoid close relationships? (APA, 2000). Passive-Aggressive and Depressive Personality Disorders Listed in the DSM-IV-TR appendix are two provision diagnoses, passive-aggressive and depressive personality disorders. The passive-aggressive personality will display a low-level resistance to demands from others in “social or work situations,” going so far as to show hostility for, and criticism of, authority (Butcher et al., 2010, p. 362). The passive-aggressive personality will often portray himself or herself as a victim of circumstance, complaining “about their personal misfortunes or of being misunderstood and underappreciated,” while cycling between “defiance and submission” (Butcher et al., 2010, p. 362). Similar to the borderline personality, Davis 11 the passive-aggressive personality presents “inappropriate” anger, although to a lesser degree (APA, 2000). In addition, again to a lesser degree, there are shared criteria with the paranoid personality such as “pervasive suspiciousness of being…exploited,” and “bears grudges, does not forgive” (APA, 2000). In nonprofessionals’ terms, the passive-aggressive personality might be referred to as difficult, unpleasant, and antisocial (not antisocial personality disorder). To different degrees, those diagnosed with depressive personality disorder share several symptoms with the other personality disorders, as well as mood and anxiety disorders. Like those with dysthymic disorder, the depressive personality generally experiences a low, unhappy mood. The tendency to feel “inadequate [and] worthless,” can also be ascribed (to varying degrees) to the dependent, avoidant, borderline, narcissistic, and histrionic personalities. In addition, the depressive personality is “prone to worry,” reminiscent of those diagnosed with an anxiety disorder (Butcher et al., 2010, p. 362). Diagnostic Accuracy The DSM-IV-TR uses a strict categorical approach to determine each diagnosis. However, because personality disorders show a great deal of shared traits and behaviors, it can be difficult to provide an accurate diagnosis. Butcher et al. (2010) wrote, “regarding the diagnoses of personality disorders…more misdiagnoses probably occur here than in any other category of disorder” (p. 343). A simple example might include an individual who meets all the criteria for antisocial personality disorder except “the pervasive pattern of disregard for and violation of the rights of others since age 15…” (APA, 2000). Because this individual’s behaviors began when he or she was 16 years old, the antisocial personality diagnosis is disqualified. (An additional example of this shortcoming in the DSM-IV-TR is the fact that a Davis 12 male cannot be diagnosed with anorexia nervosa because he does not menstruate). Taken a step further, Butcher et al. (2010) adds: You may have had some difficulty in developing a clear…picture of…the personality disorders….the characteristics and attributes of some of them seemed to blend….people frequently do not fit these prototypes neatly and instead qualify for a diagnosis of more than one personality disorder (e.g., Clark, 2007; Grant et al., 2005b; Widiger et al., 1991, as cited in Butcher et al., 2010, Unresolved Issues, p. 378). One alternative to the DSM-IV-TR is the five-factor, six-facet model, which examines the various dimensions of a person. This offers the diagnostician increased flexibility in understanding and diagnosing a particular individual (Butcher et al., 2010, table 10.2, pp. 351-352). However, Butcher et al. (2010) add this caveat: “18 different dimensional systems have been proposed, and there is still no clear evidence as to which one is best” (e.g., Clark, 2007; Livesley, 2001, 2005; Widiger, 2001; Widiger & Trull, 2007, as cited in Butcher et al., 2010, Unresolved Issues, p. 379). Conclusion J. M. Grohol (2003) noted, “Personality disorders tend to be an integral part of a person, [therefore, they are] difficult to treat or cure.” Fortunately, many people have been helped through the use of various methodologies and therapeutic approaches. However, shortcomings in the present system can prevent identification and classification of those whose personality disorder presents a cause for greater concern. For those individuals who need extensive help, society must, whenever possible, take steps to assist and treat them. By doing so, not only can lives be changed for the better, lives can also be saved. Davis 13 References American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC, American Psychiatric Association, 2000. Butcher, J. N., S Mineka, & J. M. Hooley. (2010). Abnormal Psychology. 14th edition. Boston, MA: Allyn & Bacon. Grohol, J.M. (2003, July). Personality Disorders. Retrieved from the PsychCentral Website: http://psychcentral.com/personality/ Perlmutter, Alvin H. (Producer). (1992). Personality Disorders [Educational series episode]. The World of Abnormal Psychology. Retrieved from: http://www.learner.org/resources/series60.html?pop=yes&pid=780#