dyspepsia - Webstercare
advertisement
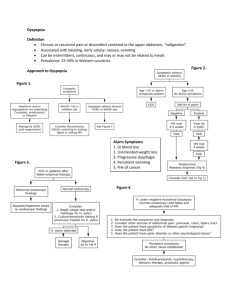
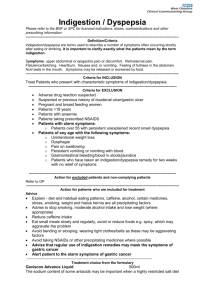
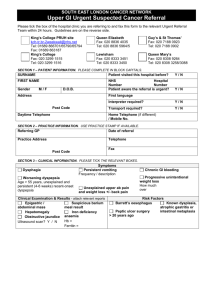
JANUARY 2014 DYSPEPSIA D yspepsia is pain or discomfort, including fullness, early satiety, bloating or nausea, centred in the upper abdomen. The most common cause is functional dyspepsia. Functional or non-ulcer dyspepsia is defined as dyspepsia without evidence of an organic disease that is likely to explain the symptoms. It is estimated that up to 20% of the population complains of functional dyspepsia at some time in their lives. Functional dyspepsia is divided into two separate syndromes – epigastric pain syndrome and postprandial distress syndrome. Functional dyspepsia can impact considerably on quality of life. Symptoms Epigastric pain or discomfort is the most common symptom in people with functional dyspepsia. However, some people will not complain of pain, but will experience burning, pressure or fullness after ordinary sized meals and often cannot finish a normal sized meal (early satiety). People with epigastric pain syndrome report intermittent pain or burning in the upper middle region of the abdomen or epigastric region at least once a week. It is not relieved by defaecation or passing of wind. Postprandial distress syndrome presents as bothersome postprandial fullness after an ordinary sized meal, at least several times a week. Early satiation that prevents a meal being finished occurs at least several times a week. Upper abdominal bloating or postprandial nausea or excessive belching can be present. In summary, symptoms of dyspepsia include: ■■ Postprandial fullness ■■ Early satiety ■■ Epigastric burning ■■ Postprandial nausea ■■ Belching ■■ Abdominal bloating ■■ Weight loss ■■ Nausea and vomiting Symptoms often worsen with eating, and can wax and wane over time. ‘Alarm symptoms’ require immediate assessment by a medical practitioner. These include age >55 years with new onset dyspepsia, chronic gastrointestinal bleeding, dysphagia (difficulty swallowing), progressive unintentional weight loss, persistent vomiting, iron deficiency anaemia, and epigastric mass. Gastro-oesophageal reflux disease (GORD) should be considered if predominant heartburn or regurgitation exists. Comorbid conditions Comorbid conditions are major determinants of the quality of life impact of functional dyspepsia. Dyspepsia may coexist with reflux disease, irritable bowel syndrome (IBS), or gastroparesis. Causes Dyspepsia may develop due to genetic predisposition, a viral infection, anxiety and stress, inflammation, surgery, trauma or Helicobacter pylori infection. Hormonal influences may play a role in some people. Medication causes Medicines known to cause or exacerbate dyspepsia include NSAIDs, aspirin, bisphosphonates (alendronate, risedronate), tetracycline and erythromycin antibiotics, theophylline, nitrates and calcium channel blockers. Diet Dietary modifications include eating smaller meals with reduced fat intake. Fullness and bloating are directly related to the amount of fat ingested. Foods that precipitate symptoms should be avoided, and the time of the main meal of the day can be changed. Stopping smoking and reduction in alcohol intake may have some benefit. Treatment Treatment options for dyspepsia are limited, but should be based on the predominant symptom. The following medications are used for treatment of dyspepsia; however evidence of efficacy is limited: ■■ Proton pump inhibitors (PPIs) ■■ Histamine2 antagonists ■■ Prokinetic agents DYSPEPSIA ■■ ■■ Tricyclic antidepressants (TCAs) Serotonin reuptake inhibitors (SSRIs) Eradication of Helicobacter pylori improves symptoms of dyspepsia in only 7% of people treated. Treatment should not be prolonged as functional dyspepsia is generally a relapsing and remitting condition. Proton pump inhibitors Proton pump inhibitors are one of the most popularly prescribed drugs in Australia for functional dyspepsia as well as GORD and peptic ulcer disease. PPIs are more effective than antacids and H2 antagonists at reducing symptoms of dyspepsia. For functional dyspepsia, PPIs have limited effectiveness and there is no evidence of a difference in outcomes between H2 antagonists and PPIs. Benefits of PPIs may be confined to those people who have co-existing reflux symptoms, but are ineffective with dysmotility-like symptoms such as fullness or bloating. A trial of PPIs for four to eight weeks is worthwhile, but treatment should be ceased if symptoms are not controlled. If effective, the dose of the PPI should be reduced or ‘stepped down’ to find the lowest effective dose. Intermittent or on demand use is reasonable to manage symptoms. (Motilium) and metoclopramide (Maxolon) can be trialled. These agents are dopamine antagonists with antiemetic properties, usually used for diabetic gastroparesis. They may improve gastric emptying by stimulating gastric smooth muscle contractions. ■■ domperidone 10 to 20 mg orally, 3 to 4 times daily before meals ■■ metoclopramide 5mg orally, 4 times daily Domperidone should be started at the low dose due to concerns of an increased risk of serious ventricular arrhythmias or sudden cardiac death, particularly in patients taking daily doses greater than 30 mg, and in patients older than 60 years of age. If dizziness, palpitations, syncope or seizures occur, the medication should be stopped immediately. Domperidone also can cause a number of serious drug interactions. Risk of extrapyramidal side effects limits the use of metoclopramide in older people. Other medications If the predominant symptom is epigastric pain, tricyclic antidepressants, tramadol, gabapentin and duloxetine are suggested. There is no evidence for SSRI antidepressants in treating functional dyspepsia. There is some evidence that the herbal preparation (STW5 [Iberogast]) may be of value in treating functional dyspepsia. Long-term use of higher dose PPIs are associated with an increased risk of hip fracture, community acquired pneumonia, and Clostridium difficile infections. Other approaches include referral to a clinical psychologist for assessment and cognitive behavioural therapy or hypnotherapy. Proton pump inhibitors include: ■■ Esomeprazole (Nexium) ■■ Omeprazole (Losec) ■■ Pantoprazole (Somac) ■■ Lansoprazole (Zoton) ■■ Rabeprazole (Pariet) Summary Histamine H2-receptor antagonists References Aliment Pharmacol Ther 2012;36:3-15. Am J Gastroenterol 2012;107:1615-20. BMJ 2013;347:f5059. Aust Prescr 2012;35(6):199. AMH Drug Choice Companion: Aged Care, 2010. Histamine H2-receptor antagonists reduce acid production and may be effective in relieving symptoms of dyspepsia. Cimetidine is rarely used as it has many drug interactions and needs to be taken up to 4 times daily. Famotidine, nizatidine and ranitidine are all prescribed once or twice daily. Dose reductions are needed in people with poor renal function. ■■ Cimetidine (Magicul) ■■ Famotidine (Ausfam, Pamacid, Pepzan) ■■ Nizatidine (Tazac, Tacidine) ■■ Ranitidine (Zantac, Rani2, Ranoxyl, Ulcaid) Prokinetic agents If the patient’s main symptom is a feeling of discomfort, fullness and bloating, prokinetic agents such as domperidone Functional dyspepsia is associated with a major impact on quality of life and treatment options are limited. Therapy should initially be based on the predominant symptom. Pharmacist-conducted medication reviews (RMMRs) can identify medications that can cause or exacerbate dyspepsia.